18
Ashley Jacoby
Employee Health
Employee health is the foundation for success in many businesses. Employers want to provide healthy strategies to their employees to have a more productive workforce. It is centered on the physical and mental health status of employees, which varies between professions. Many employers focus on the wellness and prevention areas of employee health in order to promote a healthy lifestyle for each individual. Since the 1980s, the rates of obesity have risen to 39.6% between 2015 and 2016 (Ramasamy et al., 2020). This increase has influenced companies to take action within their organization to lower the rates of smoking, promote exercise, and enhance healthy eating habits. As a whole, this will lead to a more useful workforce. Obesity in the workplace is occupation specific with a focus on the differences in the risks associated with employment and lifestyle factors.
According to the World Health Organization (WHO), obesity in the workplace is one of the most overlooked health problems in the world (Johnson & Schminkey, 2019). The Behavioral Risk Factor Surveillance Survey (BRFSS) for Washington State showed that the current rate of obesity in the workforce is 24.6% (Bonauto et al., 2014). This is about one-fourth of all employees! The rate of obesity in health care occupations, such as physicians, dentists, and nurses, is 11.6% (Bonauto et al., 2014). Obesity in these professions is dangerous to their level of production while working. There is an increased risk of musculoskeletal and mental health conditions among health care workers that are obese, which has the potential to interfere with their treatment of patients. The occupations with the highest rates of obesity, at 38.6%, are transportation, security, and cleaning services (Bonauto et al., 2014). Employees in transportation and security services are more likely to be obese because of their decreased level of physical activity during their daily tasks and other lifestyle factors, such as smoking. Cleaning services have higher rates of obesity because they are more likely to be less educated.

Obesity has caused negative health consequences in the workplace, which affects the physical and mental well-being of the employee. Many employees are at a higher risk of developing metabolic syndrome from constant exposure to high stress and job strain (Syed, 2020). Metabolic syndrome is directly linked to an increased risk of developing type 2 diabetes, cardiovascular disease, high blood pressure, and stoke. Also, technological improvements in many occupations have led to an increase in sedentary lifestyle, which contributes to the development of metabolic syndrome and its related conditions (Bailey et al., 2018). In addition, employees are at a risk of developing osteoarthritis, cancer, and gout. All of the medical conditions related to obesity in the workforce have a negative effect on the success of the business.
Many additional factors, including demographics, personality, and socioeconomic status, contribute to the increasing rates of worksite obesity. Obesity rates in employees were higher in older individuals, males, workers with a lower income, and people with a lower level of education (Banauto). It was shown that race and ethnicity were not related to the rates of obesity in the workplace. One factor that influenced obesity in employees was health behaviors. Employees who exercised daily and consumed fruits and vegetables with every meal had lower rates of obesity compared to those who do not exercise and consume less healthy foods (Banauto). Each lifestyle factor, in combination with occupational tasks, plays an important role in the development of obesity on the jobsite.
In addition, the company experiences negative outcomes from employing an obese workforce. Employees that are classified as obese contribute to the high cost of healthcare and the work-loss related expenses for the organization. These expenses include disability among employees, absence from work, and being unproductive on the job (Ramasamy et al., 2020). Obesity adds to a variety of jobsite health issues including joint pain, high blood pressure, respiratory problems, and additional medical concerns, which prevent employees from completing their daily tasks (Johnson & Schminkey, 2019). Based on loss of productivity alone, employers pay an average of $277,000 per year in medical expenses (Logsdon, 2019). The negative consequences related to having an obese workforce has led to the addition of a variety of worksite wellness programs that are specific to the organization of employment.
Here is a video describing the benefits of employee action in the workforce (Baldwin, 2012): https://vimeo.com/51029898
Worksite Wellness Programs
Worksite wellness is a key factor contributing to the functioning of organizations. It is any health promotion activity or workplace policy that is used to encourage healthy behavior and improve the health of employees. These programs educate employees towards making lifestyle choices that lead toward a balanced and healthy life.
The key to the successful addition of a worksite wellness program is focusing on the values of the employees, the occupation of employment, and the cultural characteristics of the job. Large companies offer wellness programs that include a broad range of screening activities, interventions for healthy lifestyles, and support systems for their employees (Mattke, 2015). Each company develops a different set of factors to improve their program based on the goals of the organization. The RAND Employer Survey is used as the foundation for an effective program by analyzing the employee characteristics, promoting features, and wellness offerings. Incentives are a key component to the success of worksite wellness programs, which are based on participation in the program, progress towards goals, and positive health outcomes. Some examples of incentives are paid time off, gift cards, home exercise equipment, and pedometers. Every program is specific to the organization of interest.
There are barriers to the addition of worksite wellness programs in a business. One of the biggest limitations is the cost to develop a program. This explains why 90% of employers with more than 50,000 employees have a worksite wellness program, but only 50% of employers with at least 50 employees have one (Mattke, 2015). Larger employers have more funding to use towards making programs available to improve the health of their employees. In addition, employees face limitations to their participation in the worksite wellness programs offered at their job. These barriers include inconvenient locations, limited incentives, scheduling conflicts, health beliefs, and lack of interest in participation (Person, 2010). Employers can address these barriers directly to increase their employee’s use of the program.
One of the most common occupations of interest for the development of a worksite wellness program is manufacturing. This is due to 8.8% of the total U.S. population being employed in this area, which provides a large group for disease prevention and health promotion (Logsdon, 2019). Individuals in the manufacturing workforce are more obese because of their lifestyle factors outside of their daily job. These health behaviors consist of smoking, increased alcohol consumption, and limited physical activity, which leads to higher rates of obesity. Also, individuals in this occupational cohort are exposed to a variety of mechanical, physical, and chemical elements adding to the need for intervention (Logsdon, 2019). In general, worksite wellness programs should focus on the health behaviors of the individual and the characteristics of their job. The worksite wellness programs in the manufacturing occupation are centered on the lifestyle factors practiced by these employees in order to show the greatest improvement in health behaviors. Many individuals in the manufacturing occupation are involved in worksite wellness programs through their company.
Successful Worksite Wellness Programs
The first step in developing a successful worksite wellness program is to form a plan focusing on the goals of the organization and the values of the employees. The program should encourage healthy behaviors to promote a more productive workforce. It is key to consider time conflicts, access to areas and equipment to exercise, and the use of incentives to motivate the participation of employees. Employees should be driven to continue using the program to meet their individual goals. Each employer should address the needs of the employees in order to have a positive outcome.
One example of the successful addition of a worksite wellness program is the Healthiest Maryland Businesses (HMB) Program, which was created to fill in the gaps of promoting physical activity in the workplace (Bailey et al., 2018). The goal of the program was to reduce heart disease, stroke, and cardiovascular disease by requiring a set number of hours of exercise each day. The HMB focused on the factors related to adding a physical activity program. The employees participating in the program were more motivated to act because of the incentives provided for walking, bicycling, or joining support groups. As a result of the program, the number of days absent from work and the healthcare cost to the company were reduced (Bailey et al., 2018, p. 1145). The Healthiest Maryland Businesses Program was beneficial because it focused on the needs of the company and motivated individuals to live a healthy lifestyle.
Here is a video explaining the benefits an employee received from joining a worksite wellness program (Eat Smart Move More Weigh Less, 2015): https://vimeo.com/139960746
Summary
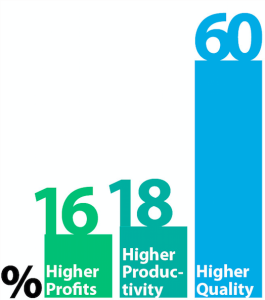
Employee health is a key component to the functioning of many businesses (see infographic below). This is crucial because employees are the core of production in organizations. Employers can develop worksite wellness programs to improve employee health behaviors by promoting healthier lifestyles. This can increase production on the job, reduce the risk of obesity-related diseases, and increase the success of the organization. Employees should find a program that matches their values to have the highest rates of success.

Review Questions
1. What disease are obese employees at a higher risk of developing?
a. Metabolic Syndrome
b. Cardiovascular Disease
c. Cancer
d. High Blood Pressure
2. What is the most common occupation of interest for worksite wellness programs?
a. Office Jobs
b. Construction
c. Manufacturing
d. Health Care Services
3. What survey is used as the foundation for creating an effective worksite wellness program?
a. Wellness Survey
b. RAND Employer Survey
c. National Healthy Worker Survey
d. Behavioral Risk Factor Surveillance System (BRFSS)
References
Bailey, M., Coller, R., & Pollack Porter, K. (2018). A qualitative study of facilitators and barriers to implementing worksite policies that support physical activity. BMC Public Health, 18(1), 1145. https://doi-org.libproxy.clemson.edu/10.1186/s12889-018-06045-x
Baldwin, Montgomeri. (2012). Wellness in the Workplace Series: Employee Engagement. Vimeo. https://vimeo.com/51029898
Bonauto, D., Lu, D., & Fan, J. (2014). Obesity prevalence by occupation in Washington state behavioral risk factor surveillance system. Prevention Chronic Disease: Public Health Research, Practice, and Policy. https://dx.doi.org/10.5888/pcd11.130219
Eat Smart Move More Weight Less. (2015). Erin’s Testimonial. Vimeo. https://vimeo.com/139960746
Johnson, M. & Schminkey, M. (2019). Thinking big: An integrative conceptual review of the workplace consequences of obesity and a theoretical review of the workplace consequences of obesity and a theoretical extension of the processes that create them. The Journal of Applied Psychology. https://doi-org.libproxy.clemson.edu/10.1037/apI10000459
Logsdon, S., Branstetter, M., & Main, E. (2019). Perceived health status in rural manufacturing workers. Workplace Health & Safety, 67(2), 78-86. https://doi-org.libproxy.clemson.edu/10.1177/2165079918794206
Mattke, S., Kapinos, K., Caloyeras, J., Taylor, E., Batorsky, B., Liu, H., Van Basum, K., & Newberry, S. (2015). Workplace wellness programs: Services offered, participation, and incentives. Rand Health Quarterly, 5(2). 7. https://doi-libproxy.clemson.edu/101622976
Person, A., Colby, S., Bulova, J., & Eubanks, J. (2010). Barriers to participation in a worksite wellness program. Nutrition Research and Practice, 4(2), 149-154. https://doi.org/10.41262/nrp.2010.4.2.149
Ramasamy, A., Laliberte, F., Aktavoukian, S., Lejeune, D., DerSarkissian, M., Cavanaugh, C., Smolarz, B. G., Ganuly, R., & Duh, M. (2020). Direct, absenteeism, and disability cost burden of obesity among privately insured employees: A comparison of healthcare industry versus other major industries in the United States. Journal of Occupational and Environmental Medicine, 62(2), 98-107. https://doi-org.libproxy.clemson.edu/10.1097/JOM.0000000000001761
Syed, I. (2020) Diet, physical activity, and emotional health: what works, what doesn’t, and why we need integrated solutions for total worker health. BMC Public Health, 20(1), 152. https://doi-org.libproxy.clemson.edu/10.1186/s12889-020-8288-6
a syndrome marked by the presence of usually three or more of a group of factors (such as high blood pressure, abdominal obesity, high triglyceride levels, low HDL levels, and high fasting levels of blood sugar) that are linked to increased risk of cardiovascular disease and type 2 diabetes
doing or requiring much sitting
a common form of arthritis typically with onset during middle or old age that is characterized by progressive degenerative changes in the cartilage of one or more joints (as of the knees, hips, and hands) accompanied by thickening and overgrowth of adjacent bone and that is marked symptomatically chiefly by stiffness, swelling, pain, deformation of joints, and loss of range of motion —abbreviation OA
a metabolic disease marked by a painful inflammation of the joints, deposits of urates in and around the joints, and usually an excessive amount of uric acid in the blood
the statistical characteristics of human populations (such as age or income) used especially to identify markets
An individual's or group's position within a hierarchical social structure. Socioeconomic status depends on a combination of variables, including occupation, education, income, wealth, and place of residence. Sociologists often use socioeconomic status as a means of predicting behavior.
https://www.dictionary.com/browse/socioeconomic-status?s=t
something that incites or has a tendency to incite to determination or action
an instrument usually in watch form that records the distance a person covers on foot by responding to the body motion at each step
a group of individuals having a statistical factor (such as age or class membership) in common in a demographic study
