4 Disorders of the Lesser Toes
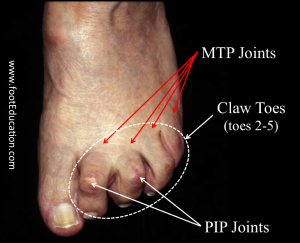
An imbalance between the extrinsic and intrinsic muscles of the foot can produce deformities of the lesser toes. These deformities are classified by how the separate toe joints are affected. Hammertoe deformities are characterized by flexion of the proximal interphalangeal (PIP) joint and extension of the metatarsal-phalangeal (MTP) joint resulting in a prominent bump at the PIP joint. Claw toe deformities also have PIP flexion and MTP extension but additionally have flexion of the distal interphalangeal (DIP) joint which produces “clawing.” Only the DIP joint is affected in mallet toe deformities, so the MTP and PIP joints are naturally extended but the DIP joint is flexed.
Structure and function
The lesser toes have three phalanges. The proximal phalanx articulates proximally with the metatarsal (at the MTP joint) and distally with the middle phalanx (at the PIP) joint; the middle phalanx’s articulation with the distal phalanx is called the DIP joint.
The extensor digitorum longus (EDL), an extrinsic muscle, is the primarily extender of the MTP joint. The extensor digitorum brevis (EDB), an intrinsic muscle, extends the PIP and DIP joints.
The flexor digitorum longus (FDL), another extrinsic muscle, flexes all three joints of the lesser toes, but the DIP joint especially. The flexor digitorum brevis (FDB) tendon (intrinsic) primarily flexes the PIP joint. The lumbricals originate from the metatarsals and flex the MTP joint and extend the PIP and DIP joints.
All of the toe joints have a fibrocartilaginous plantar plate, which passively resist extension as well.
Claw toes are caused by an imbalance between the extrinsic and the intrinsic muscles in the foot, causing flexion at the PIP (proximal interphalangeal) joint and extension at the MTP (metatarsal phalangeal) joint. The PIP joints become prominent and can be irritated by shoes, leading to painful calluses on the dorsal aspect of the toes (Figure 1).
Typically, when only a single toe is clawed, trauma or arthritis in the cause. More commonly all four lesser toes are involved and hereditary muscle imbalance (extrinsics > instrinsics) or nerve damage (neuropathy) is the cause.
Hammer toes are usually caused by shoes that force the toe to bend; they are also seen in patients with bunions.
A mallet toe, (i.e. isolated flexion of the DIP joint), may be caused by shoe pressure (causing, eventually, attenuation of the extensor tendon); a tight flexor digitorum longus can also be the cause.
Patient presentation
A patient with a deformity of the lesser toes is very likely an older female presenting with pain on the top of the toes (as they rub against the shoes). There also can be pain on the tip of the toes as they jam into the soles of the shoes. With a long-standing deformity, there can be pain at the base of the toes along with corns or calluses of the skin from repeated friction.
Objective evidence
The deformity is usually obvious, and x-rays confirm what is seen clinically. On physical exam, each joint should be assessed as to whether it can be passively corrected; that is whether the deformities are flexible or rigid (as this guides treatment). It is also important to assess the toes in various positions of ankle flexion/extension, so the effect of any extrinsic muscle tightness can be demonstrated (i.e., tightness of the extrinsic flexors would be worsened with ankle dorsiflexion). Also, because toe deformities are seen as a manifestation of neurological disease, a detailed assessment of strength and sensation is needed.
Epidemiology
Claw toes can be congenital or acquired, and so are seen throughout all ages, though more common with increasing age (the 7th and 8th decades). Women are affected four to five times more than men.
Differential diagnosis
Underlying associated conditions include:
- diabetes, with peripheral neuropathy
- rheumatoid arthritis
- primary neuromuscular disease (poliomyelitis, Freidrich’s ataxia, myelopathy, multiple sclerosis or Charcot Marie Tooth Disease
- other foot deformities such as bunions, flat feet, or pes cavus deformity (highly arched feet)
Red flags
All lesser toe deformities are red flag findings, suggesting the presence of a complication of diabetes or a neurological disorder. Close evaluation of the whole patient is essential.
Treatment options and outcomes
Non-operative
Most deformities can be treated by applying pads to the areas of prominence or using a shoe with a wide-toe box to accommodate the deformity and alleviate pain. Some patients may need an orthotic to create cushioning over the toe region. Trimming painful calluses can relieve symptoms, but without addressing the deformity, they may recur.
Operative
Surgery is considered only in deformities that cannot be corrected non-operatively.
Claw and hammer toes with a flexible deformity may be treated with a flexor and/or extensor tenotomy or a flexor to extensor tendon transfer with a capsular and extensor tendon release. If there is a fixed deformity at the MTP joint, a capsular release and extensor tendon lengthening may suffice. In some patients a metatarsal shortening osteotomy may be needed, especially if the patient has metatarsalgia or tenderness. A fixed PIP deformity is treated with resection arthroplasty or Interphalangeal fusion.
A mallet toe with a flexible deformity can be treated with a percutaneous flexor tenotomy; a rigid deformity requires either a resection arthroplasty of the distal aspect of the middle phalanx or DIP fusion.
Note that the recovery period for any toe surgery is prolonged. It is not uncommon to note swelling and stiffness in the toes even 6 months post-surgery.
Foot surgery, in general, is more susceptible to wound complications and infection; toe deformity surgery, in particular, can be complicated by recurrence of the deformity.
Skills
Claw/hammer/mallet toes are typically present in older age or as an indication of an underlying neurological disorder – asking the right questions to the patient and ordering the necessary exams to identify the cause is important.
Key terms
claw toe, hammer toe, mallet toe, lesser toe deformity, metatarsalgia, corns, muscular imbalance
