8 Achilles Tendon Disorders
The Achilles tendon is subject to high forces with each step and therefore subject to wear-and-tear damage. There are many pathological conditions that affect the Achilles tendon, but the most common chronic conditions are tendonitis and bursitis. The most common acute condition is an Achilles rupture (often super-imposed on wear-and-tear).
Structure and function
The Achilles tendon is the largest and strongest tendon in the human body. It attaches the posterior calf muscles (the gastrocnemius and soleus) to the calcaneus.
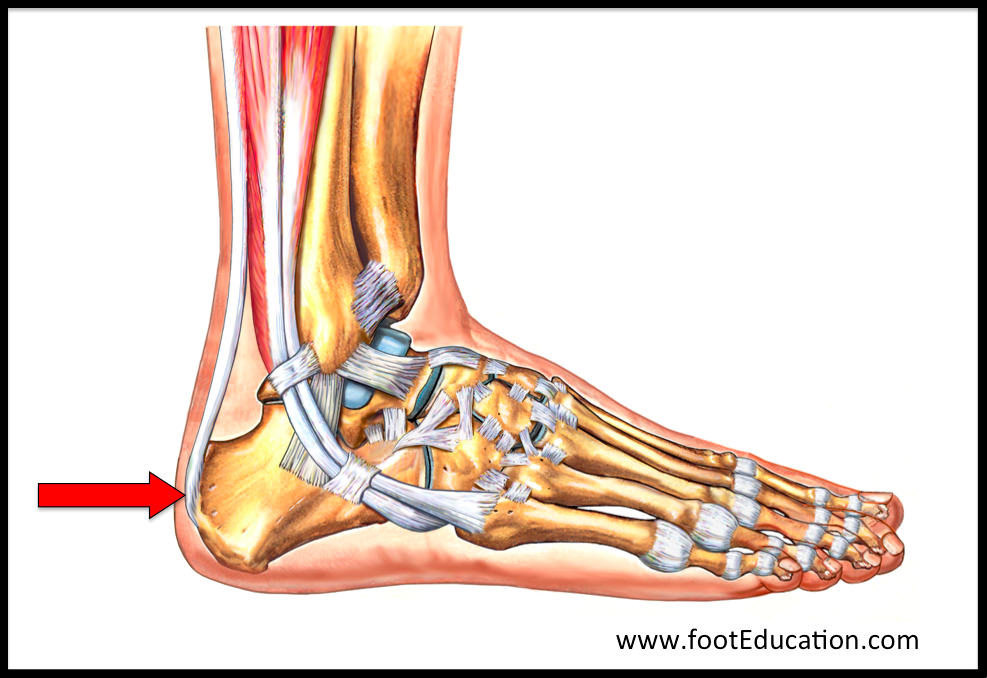
The posterior calf muscles both actively plantar flex the ankle and resist passive dorsiflexion during walking, jumping, and running. Note that when the person places the ball of his or her foot on the ground during gait, body weight and momentum will force the ankle into dorsiflexion. Resisting this motion, and in turn decelerating the landing of the heel, is powered by the posterior calf muscles. Forces up to 3 times body weight may be applied to the tendon when this happens while walking; even greater forces are applied while jumping and running. The Achilles tendon inserts into the posterior surface of the calcaneus. The insertion begins about halfway between the plantar and superior surface of the calcaneus (Figure 1).
A bursa lies between the tendon and calcaneus above the insertion point: the so-called retrocalcaneal bursa. Another bursa lies posterior to the tendon between the tendon and skin, namely, the subcutaneous calcaneal bursa. A bursa is a fluid-filled sac (the word shares its origin with the English word “purse”) that normally exists between tendons and bone in places where the bone surface may be prominent; this allows the tendon to glide more easily. In the healthy state, the bursa is only a few cells thick, and the bursa is filled with only a small amount of lubricating fluid. However, when irritated, a bursa can become markedly thickened and filled with larger amounts of fluid. This condition is known as bursitis.
Patient presentation
Achilles tendonitis is a chronic condition characterized by pain and swelling in the Achilles tendon.
Symptoms of tendonitis are produced by swelling and inflammation of the tissue that surrounds the Achilles tendon – the paratendon. As such, the condition may be more appropriately described as an Achilles tenosynovitis (inflammation of the lining surrounding the Achilles tendon). Inflammation of the tendon can be caused either by direct pressure from shoewear or more commonly, as part of the healing response to over-use and micro-trauma.
There are two types of Achilles tendonitis: non-insertional tendonitis and insertional tendonitis.
Achilles Tendonitis (Non-Insertional):
In classic non-insertional (or mid-substance) Achilles tendonitis, the pathology is typically located 2 to 6 cm proximal to the insertion of the Achilles tendon to the calcaneus.
Non-insertional Achilles tendonitis is often associated with a history of increased activity level (e.g., starting a new training regimen or attempting to resume a normal activity level after an injury and enforced immobilization).

A patient presenting with non-insertional Achilles tendonitis (Figure 2 left) will often describe pain and tenderness 2-6 cm from the insertion of the tendon into the calcaneus. The patient will often describe an increase in activity, such as starting a new training regimen or attempting to resume a normal activity level after an injury to another part of the foot or ankle.
Physical Examination will usually reveal swelling and tenderness around the Achilles tendon. There is often an associated tight calf muscle (equinus contracture). The location of the pain can help differentiate this from insertional tendinitis (Figure 2 right) which presents with pain more distally.
Insertional Achilles Tendonitis:
In so-called “insertional” Achilles tendonitis, the pathology is located at the insertion of the Achilles tendon to the calcaneus (Figure 2, right). Insertional Achilles tendonitis is a product of wear and tear at the attachment (“insertion”) of the tendon onto the calcaneus. This degeneration incites an inflammatory response and produces pain at the back of the heel. Eventually, the inflamed Achilles tendon may become calcified, forming bone-like fragments in the tendon.
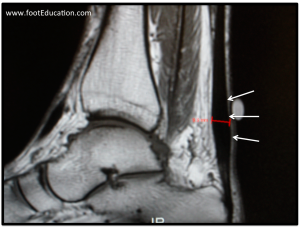
The pathology associated with insertional Achilles tendonitis includes the “terrible triad” (Figure 3):
- Degeneration of the Achilles tendon near the insertion site,
- An inflamed retrocalcaneal bursitis, and
- A Haglund’s deformity (a prominent bony lump on the heel)

A Haglund’s deformity is a bony prominence associated with the upper part of the calcaneus (Figure 4). This is sometimes called a “pump bump.” This prominent bone tends to form gradually over many years, and can eventually cause irritation by disrupting nearby structures, including the retrocalcaneal bursa and the Achilles tendon. The bony prominence also creates discomfort by rubbing up against the back of footwear, the so-called “heel counter” of the shoe.

When a Haglund’s deformity is present, the retrocalcaneal bursa can become inflamed. This inflammation can result in exquisite tenderness along the posterior aspect of the heel.
Objective Evidence
X-rays will usually be negative in cases of non-insertional Achilles tendonitis, unless there is calcification of the Achilles tendon. (Calcification is relatively rare except in older patients.) Cases of insertional Achilles tendonitis may reveal a calcaneal spur on x-ray.
An MRI can give a detailed view of the soft tissue (Figure 5). However, this test is not routinely indicated in the initial assessment of Achilles tendonitis.
Ultrasound is usually less expensive than an MRI, but may not be available in all settings. Further, use of ultrasound may be limited by the examiner’s lack of skill or experience.
Epidemiology
Insertional Achilles tendonitis with its associated “terrible triad” of heel pain typically occurs in middle-aged individuals who are overweight, though a variant of this condition is also seen in young, active runners. The exact incidence of this bimodal distribution has not been recorded.
Non-Insertional Achilles tendonitis is often associated with an increase in activity level/overuse and tends to occur in patients in their 30s and 40s. According to Jarvinen et al., the reported annual incidence of Achilles tendonitis is between 7-9% in top-level runners (PMID: 15922917).
Differential diagnosis
There are four common causes for pain near the back of the heel:
- non-insertional Achilles tendonitis,
- insertional Achilles tendonitis (with or without bursitis)
- paratendonitis (inflammation of the sheath surrounding the Achilles tendon, rather than of the tendon itself), and
- Achilles tendon rupture.
The Thompson test will identify an Achilles tendon rupture. The precise location of the pain should distinguish non-insertional Achilles tendonitis vs insertional Achilles tendonitis.
Red flags
Although corticosteroid injections in and around the Achilles can be helpful in the short-term managing symptoms they weaken the tendon and predispose to tearing. Be alert for patients that have had corticosteroid injections in this area.
Patients with inflammatory arthropathies may also get inflammation in the lining around their Achilles. If a patient has other joints that are painful or swollen, especially if they are of recent onset, an inflammatory etiology should be ruled out.
Treatment Options and Outcomes
Non-operative Treatment of Achilles Tendonitis
Most patients with Achilles tendonitis can have their symptoms treated effectively without surgery. Insertional Achilles tendonitis can be more recalcitrant to treatment than non-insertional Achilles tendonitis. An initial period of relative rest to allow the symptoms to settle is often beneficial. This is followed by a gradual return to normal activities incorporating the following non-operative treatment elements:
- Activity modification,
- Shoewear modification (a heel lift will unload the tendon),
- Weight Loss (if applicable)
- Anti-inflammatory medication (if not contra-indicated) and;
- A rehabilitation program including specific stretching and strengthening exercises.
Stretching the gastrocnemius (outer calf muscle) with the knee straight (Figure 6) is an important component of non-operative treatment. A tight calf muscle will increase the force going through the Achilles tendon and predispose the tendon to micro-tearing.
A graduated eccentric loading program (strengthening the calf muscle while it is lengthening) is an important component of non-operative treatment for non-insertional Achilles tendonitis (Figure 7). However, it may be too aggressive for patients with insertional Achilles tendonitis.
Using a heel lift reduces the “stretch” on the Achilles during walking and thereby reduces the stress on the tendon.
The forces applied to the Achilles tendon during activities are proportional to body weight. Therefore losing weight (even a small amount) can be very helpful.
Surgical Treatment of Achilles Tendonitis
Surgical debridement, that is, the removal of the damaged tissue with meticulous repair of the remaining tendon, may be chosen if non-operative treatment fails. One setting where surgery may be considered more readily is that of a high-level athlete with insertional Achilles tendonitis and a Haglund’s deformity. This surgery usually involves removing the prominent excess bone and the thickened inflamed retrocalcaneal bursa and debriding the Achilles tendon. In older, heavy-set middle-aged patients with insertional Achilles tendonitis that have truly failed a focused non-operative treatment regiment it may be necessary to transfer the Flexor Hallucis Longus (FHL) tendon into the calcaneus to help offload the Achilles.
Recovery from surgery can be prolonged. Initially, the leg is immobilized to allow the wound to heal. Once the wound is healed, gentle range of motion exercises can be started. Some patients are limited in weight-bearing for the first six weeks during the healing process. Gradually, activity can be increased. Improvement in strength continues for several months and may take over one year.
Stiffness of the ankle, rupture of the tendon, and deep vein thrombosis are known potential complications of surgery. Wound healing issues and infection can occur and when they do it is a very serious problem because loss of skin and soft-tissue in this area is very hard to treat.
Risk factors and prevention
Regular calf stretching (Figures 6 & 7), can help improve the Achilles tendon’s mechanical compliance (“stretchability” in layman’s terms) and makes it more resilient.

A consistent calf-stretching program is an important part of treatment and prevention of Achilles injuries (Figure 6). Leaning against the wall with one foot forward and the back heel kept on the ground will stretch the Achilles and posterior calf muscles. As it is the outer calf muscle (gastrocnemius) that is usually tight this stretch should be performed with the knee straight as the gastrocnemius originates from the posterior aspect of the distal femur. Bending the knee will take the tension off the gastrocnemius and place it on the soleus.
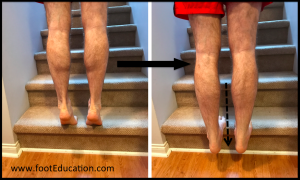
Controlled “eccentric” exercises where the Achilles tendon is being lengthened while the calf muscle contracts, may help prevent (or treat) Achilles tendonitis (Figure 7). This includes exercises such as the “Heel drop” shown here. In this exercise, patients stand on their toes while positioned on the edge of a ledge such as a stair. They then slowly lower their heels down below the ledge simultaneously stretching and strengthening the Achilles tendon. This can be done with both legs at a time (bilaterally) or for a more concentrated effort, one leg at a time. It can also be done with the knees straight (putting force on the gastrocnemius) or the knees bent (putting force on the soleus). Patients should gradually work up to performing 5 sets of 10 repetitions. These exercises should be performed 5-6 days per week during the active treatment phase and then 3 times per week to minimize the chance of developing recurrent symptoms. It is critical that this exercise is approached cautiously, as it has the potential to put excessive pressure on the Achilles. Patients should always warm up first (ex. get their blood flowing on an exercise bike for 5-10 minutes) before performing these exercises.
Using a heel lift or a shoe with a moderate heel can help reduce the stress on the tendon.
Miscellany
In Greek mythology Achilles was dipped into the River Styx by his mother Thetis to coat his body with a shield of protection. Thetis grasped Achilles by the heel (on the eponymous tendon) when she dipped him, leaving that one area not washed by the river, and in turn unprotected. From that comes the term “Achilles heel,” connoting a person’s area of vulnerability.
Key terms
Achilles tendonitis; insertional Achilles tendonitis; non-insertional Achilles tendonitis; Haglund’s deformity; retrocalcaneal bursitis;
Skills
Bedside skills for the diagnosis of disorders of the Achilles include the ability to take a detailed but focused history and perform a thorough musculoskeletal examination.
