7
By Gabriel Espinosa, Frank Ford, and Alex Wadsworth
Climate Change and Human Health
With the widespread use of modern medicine, many health concerns of the past have become obsolete, drawing human attention to more serious complications such as cancers and genetic disorders. However, climate change will reintroduce medical relics of the past while introducing a host of new health problems in its wake. Most literally, human health encompasses physical, social, and mental well-being and can be affected by every aspect of day-to-day life. Ideally, everyone on Earth would be physically healthy with regular exercise and access to clean food and water. Mental and social fitness is often more challenging to define but can be generalized by the ability to manage positive and negative emotions while maintaining honest relationships with others (CDC, 2020a). While all aspects of health are critical to one’s survival, for the sake of brevity, the following will focus on physical consequences of climate change on one’s well-being.
The stratosphere is the region above the troposphere and contains ozone which is vital to human health. Ozone acts as a barrier, protecting the surface of the earth from ultraviolet radiation by absorbing its energy and dissipating it into heat (Earth Observatory, 2009). Ultraviolet radiation is a high energy light wavelength that is emitted from the Sun, composing 10% of the total light emitted each day. However, man-made chemicals, like chlorofluorocarbons (CFC’s) that contribute to climate change also react with the ozone layer and destroy ozone molecules (NOAA Research, n.d.). The depletion of the ozone layer results in a higher concentration of ultraviolet radiation reaching the surface, which can be seen in Figure 1, creating dangerous conditions for humans.
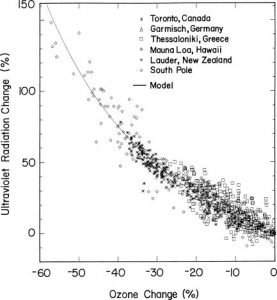
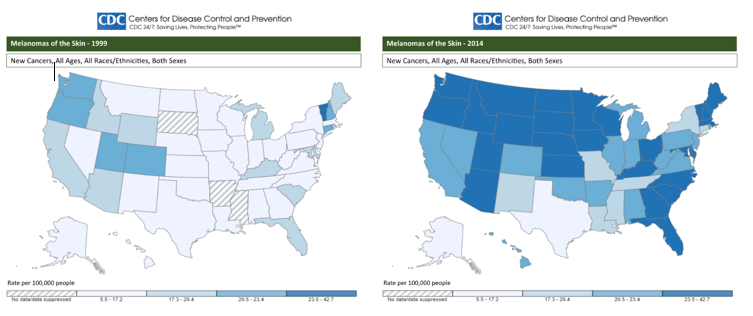
Long term exposure to UV radiation, particularly UVB radiation, can lead to the development of cancer and an assortment of eye diseases given the skin penetrating characteristics of the wavelength (Norval et al., 2007). Given that UVB radiation can only penetrate the surface of the skin it most commonly is the cause of melanoma, a form of skin cancer affecting the pigment producing cells below the surface. While melanoma only makes up 1% of current skin cancer cases, it is by far the deadliest, estimated to kill over 6800 people in the US by the end of 2020 (CDC, 2020b). Although the death rate of skin cancers is expected to decline as medicine improves, Figure 2 visualizes the rapidly increasing rate of melanoma diagnoses over the past 15 years with an increase of 44,877 over the recorded period from 1999 to 2014 (CDC, 2020b). Comprehensive data on the issue hasn’t fully been studied, however, scientists believe UV radiation will also have negative effects on human eyes. Ultraviolet wavelengths can cause the eyes to sunburn (photokeratitis) along with corneal swelling which can lead to severe conditions such as glaucoma and cataracts both of which can cause blindness (Norval et al., 2007).
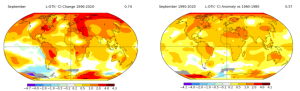
The troposphere, which contains atmosphere near the Earth’s surface, is responsible for surface temperature, a characteristic essential to human life. In the past 50 years, average temperatures in the US have risen by 2 degrees Fahrenheit and are continuing to rise. According to the CDC, as regional and global temperatures rise, so will the severity and frequency of extreme heat events (CDC, n.d.). Extreme heat events are detrimental to human life, shown by the 2003 heatwave in Europe which left 14,802 people dead in France alone and thousands of others in surrounding countries (Haines et al., 2006). The occurrence and concentration of heat related weather anomalies shows significant warming around the middle east and the poles which can be seen in Figure 3 below.
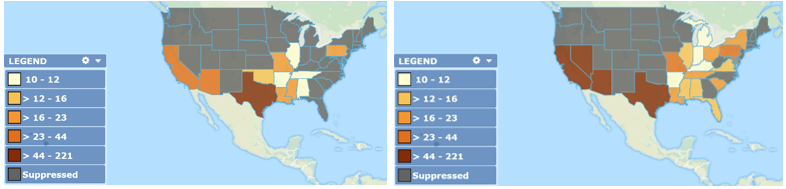
The described increase in global temperature will lead to a far greater rate of heat mortality around the world. Between 1998 and 2017 roughly 166,000 people died worldwide as a result of heatstroke which occurs if one’s core temperature exceeds 40°C (WHO, 2020). With warmer weather, cold related deaths during winter months will decrease over time, however, deaths attributed to high temperatures will far exceed these losses, resulting in a net mortality increase due to global heat (Huang et al., 2011). Figure 4 below pictures the slow, yet constant trend towards higher heat mortality rates in the United States which could cost the country $141 billion in the next 80 years (Aronoff, 2018).
The biosphere of Earth also plays a role on health through vector-borne diseases. Epidemiology defines a vector as any living organism capable of carrying and transmitting infections to another living creature. Disease vectors are most well known to be rodents, arachnids, insects, and parasites and their presence on this planet is increasing alongside the average global temperature (Semenza & Menne, 2009). The hosts of these diseases rely on a very warm or humid environments to survive, with an increase in rainfall promoting transmission and breeding sites (Reiter, 2001). An example of these environments is the tropics where, according to several studies which used independent data sets, they will expand up to 2 degrees in latitude (approximately 138 miles) during the 21st century due to changes in air currents above the equator (Seidel et al., 2008). This increase of the tropical boundaries will broaden the habitats of vectors and increase the human population susceptible to the viruses they transmit. Figure 3 shows the global temperature change over the past 30 years, illustrating that regions in North American and Europe have seen a mean rise of 0.5-4 degrees Celsius. In Italy, local transmission of Plasmodium vivax malaria has occurred recently, 40 years after its eradication, because of higher temperatures allowing different parasites to survive in Italy’s new climate (Githeko et al., 2000). As higher temperature and humidity ranges around the equator increase, the footprint of vector-borne diseases will spread within those larger regions.
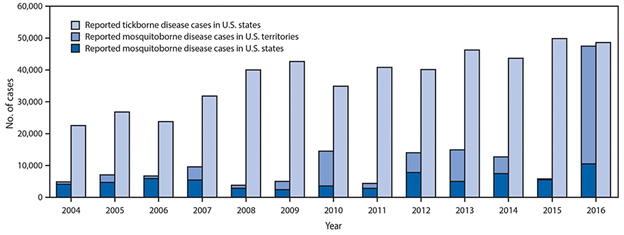
As seen in Figure 5, over the past 12 years the United States has seen a steady increase in insect-borne disease cases resulting from ticks and mosquitos. North American ticks are most known to transmit Lyme Disease, which, if untreated can lead to severe nerve and joint damage. From 2004 to 2016 the number of Lyme Disease cases in the US has increased by 16,625 (Rosenberg et al., 2018) making growing disease transmission a very real and current threat. Mosquito-borne illnesses have increased quite drastically in the US in recent years, from 2004 to 2015 cases peaked at 14,505 while 2016 saw a peak 47,461 cases alone (Rosenberg et al., 2018). While less common, mosquito-borne diseases such as dengue fever, when untreated, have a 20-50% mortality rate, far more lethal than tick-borne diseases (Brownstein et al., 2005).
It is important to note, the correlation between vector-borne infection rates and climate change was first characterized in the late 1990s and thus data on the matter is frequently lacking in great time scales. However, the limited data that does exist and future research prospects demonstrate convincing arguments in proving causation (Haines et al., 2006).
Previous public health research provides important insight to current public health professionals and governments so that the human population can reduce negative impacts of climate change on human health. Currently it is believed that the adaptiveness of the human population will allow for many communities to protect themselves from climate impacts, however, it must be noted that this would be a temporary buffer (McMichael et al., 2006). Additionally, human adaptiveness varies greatly depending on many factors such as geography, technological resources, wealth and governance. Research into this is being done to attempt to lessen health risks that will accompany the changing climate (McMichael et al., 2006). Furthermore, researchers are using satellite data, computer modeling, and geographic information system modelling of the effect that increased precipitation and changes in temperature will have on infectious disease (Ebi et al., 2005). This will allow for public health officials to better understand how future changes in the climate will allow for the increased spread of infectious diseases, UV concentration, and severe heat so that governments can better prepare. One final promising area that is being researched is improving case surveillance for infectious diseases (McMichael et al., 2006). By identifying highly infectious diseases faster, it will be much easier to contain them.
While currently there is highly encouraging research being done for the public health sector there is still much that needs to be done. One of the most challenging but rewarding work will be identifying how local communities will adapt to changes and what still needs to be done to allow these communities to adapt most successfully. Even though there is a good global sense of how the human population will adapt it is still mostly unknown at local levels how specific areas will or will not adapt to future climatic changes (Ebi et al., 2005). Mitigating potential future risks of these changes will need to be studied by individual communities, local governments, and nations. This challenge can be overcome, but urgency is required by lawmakers and governments so that proper preparations can take place. Without this sense of urgency there will come a time when we reach a threshold of what the human body can endure and there will be dire consequences on humanity.
References
Aronoff, K. (2018, December 5). With a Green New Deal, here’s what the world could look like for the next generation. The Intercept. https://theintercept.com/2018/12/05/green-new-deal-proposal-impacts/
Brownstein, J. S., Holford, T. R. & Fish, D. (2005). Effect of climate change on Lyme disease risk in North America. EcoHealth, 2, 38-46. https://doi.org/10.1007/s10393-004-0139-x
Department of Environment Food and Rural Affairs. (n.d.). Depletion of the ozone layer leading to an increase in ground-level ultraviolet radiation. UK AIR (Air Information Resource). https://uk-air.defra.gov.uk/research/ozone-uv/moreinfo?view=increase-uv-radiation
Earth Observatory. (2009, April 10). Ozone: What is it, and why do we are about it. NASA Education. https://www.nasa.gov/audience/foreducators/postsecondary/features/F_Ozone.html
Ebi, K. L., Smith, J. B., & Burton, I. (2005). Integration of public health with adaptation to climate change: Lessons learned and new directions. CRC Press.
Githeko, A. K., Lindsay, S. W., Confalonier, U. E., & Patz, J. A. (2000). Climate change and vector-borne diseases: A regional analysis. Bulletin of the World Health Organization, 78(9), 1136-1147. https://www.scielosp.org/article/bwho/2000.v78n9/1136-1147/en/
Haines, A., Kovats, R. S., Campbell-Lendrum, D., & Corvalan, C. (2006). Climate change and human health: Impacts, vulnerability and public health. Public Health, 120(7), 585-596. https://doi.org/10.1016/j.puhe.2006.01.002
Hajat, S., Vardoulakis, S., Heaviside, C., & Eggen, B. (2014). Climate change effects on human health: Projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. Journal of Epidemiology and Community Health, 68(7), 595-596. http://dx.doi.org/10.1136/jech-2013-202449
Huang, C., Barnett, A. G., Wang, X., Vaneckova, P., FitzGerald, G., & Tong, S. (2011). Projecting future heat-related mortality under climate change scenarios: A systematic review. Environmental Health Perspectives, 119(12), 1671-1690. https://doi.org/10.1289/ehp.1103456
McMichael, A., Woodruff, R. E., & Hales, S. (2006). Climate change and human health: Present and future risks. The Lancet, 367(9513), 859-869. https://doi.org/10.1016/S0140-6736(06)68079-3
NOAA Research. (n.d.). Frequently Asked Questions. Global Monitoring Laboratory. https://www.esrl.noaa.gov/gmd/education/faq_cat-2.html
Norval, M., Cullen, A. P., de Gruijl, F. R., Longstreth, J., Takizawa, Y., Lucas, R. M., Noonan, F. P., van der Leun, J. C. (2007). The effects on human health from stratospheric ozone depletion and its interactions with climate change. Photochemical and Phytobiological Sciences, 3, 232-251. https://doi.org/10.1039/B700018A
Reiter, P. (2001). Climate change and mosquito-borne disease. Environmental Health Perspectives, 109(1), 141-161. https://ehp.niehs.nih.gov/doi/pdf/10.1289/ehp.01109s1141
Rosenberg, R., Lindsey, N. P., Fischer, M., Gregory, C. J., Hinckley, A. F., Mead, P. S., Paz-Bailey, G., Waterman, S. H., Drexler, N. A., Kersh, G. J., Hooks, H., Partridge, S. K., Visser, S. N., Beard, C. B., & Peterson, L. R. (2018). Vital signs: Trends in reported vectorborne disease cases — United States and Territories, 2004–2016. Morbidity and Mortality Weekly Report (MMWR), 67(17), 496–501. http://dx.doi.org/10.15585/mmwr.mm6717e1
Schmunk, B. Robert. (2020, September 13). GISS Surface Temperature Analysis. National Aeronautics and Space Administration Goddard Institute for Space Studies. https://data.giss.nasa.gov/gistemp/maps/index.html
Seidel, D. J., Fu, Q., Randel, W. J., & Reichler, T. J. (2008). Widening of the tropical belt in a changing climate. Nature Geoscience, 1, 21-24. https://doi.org/10.1038/ngeo.2007.38
Semenza, J. C., & Menne, B. (2009). Climate change and infectious diseases in Europe. The Lancet Infectious Diseases, 9(6), 365-375. https://doi.org/10.1016/S1473-3099(09)70104-5
U.S. Center for Disease Control and Prevention [CDC], (2020a). Learn About Mental Health. U.S. Center for Disease Control and Prevention. https://www.cdc.gov/mentalhealth/learn/index.htm
U.S. Center for Disease Control and Prevention [CDC], (2020b). United States Cancer Statistics: Data Visualizations. U.S. Center for Disease Control and Prevention. https://gis.cdc.gov/Cancer/USCS/DataViz.html
U.S. Center for Disease Control and Prevention [CDC], (2020c). Vector-Borne Diseases in the United States, 2004-2018. U.S. Center for Disease Control and Prevention. https://www.cdc.gov/ncezid/dvbd/vital-signs/index.html
U.S. Center for Disease Control and Prevention [CDC]. (n.d.). Climate Change and Extreme Heat Events. National Center for Environmental Health. https://www.cdc.gov/climateandhealth/pubs/climatechangeandextremeheatevents.pdf
World Health Organization [WHO], (2020). Heatwaves. World Health Organization. https://www.who.int/health-topics/heatwaves#tab=tab_2
