18 Bursitis of the Knee
A bursa is a sac-like structure found near joints that allows soft tissues to glide across bony prominences. Bursitis is an inflammation of the bursa. Near the knee, there are three clinically important bursas: the prepatellar (in front of the patella itself), infrapatellar (just distal to the patella) and anserine (on the proximal – medial tibia). Bursitis may result from local injury, infection or systemic diseases such as rheumatoid arthritis or gout. Bursitis due to infection is known as septic bursitis.
Structure and Function
The word bursa (similar to the English word “purse”) means sack, though in the healthy state, the sack is mostly empty: that is, the bursa is a double layer of a synovial membrane with a very small amount of synovial fluid between the layers. This anatomical arrangement promotes low friction gliding, and indeed the function of a bursa is to facilitate the gliding of a tendon or ligament around a bony process.
In the knee, there are three bursas (the plural is also spelled “bursae”): the pre-patellar bursa, the infrapatellar bursa and the anserine bursa (Figure 1). As their name implies, the first two bursas are designated by their position relative to the patella. The anserine bursa got its name by its association with the so-called pes anserinus, meaning “foot of the goose”, namely, the three tendons that insert onto the anteromedial tibia. (The three tendons are the sartorius, gracilis and semitendinosus.) The pes bursa is typically about 5 cm below the joint line, and therefore symptoms there may be mistaken for articular pathology.

The prepatellar bursa is located superficial to the patella. It decreases friction as the soft tissues glide over the patella during knee flexion and extension. Because of the location of the prepatellar bursa, it is susceptible to repetitive microtrauma, especially when kneeling. Its location also makes it susceptible to blunt and penetrating trauma. Septic prepatellar bursitis can occur following local inoculation due to trauma. The prepatellar bursa has three layers. The subcutaneous layer is located just below the deep dermis and is the one most commonly implicated.
There are two infrapatellar bursae, superficial and deep. The superficial bursa is located between the tibial tubercle and the subcutaneous fascia, while the deep bursa is located between the patellar tendon and the upper tibia.
Infrapatellar bursitis develops in a similar fashion to prepatellar bursitis. Chronic microtrauma secondary to kneeling can lead to superficial bursa wall thickening and inflammation. Chronic overuse and irritation of the patellar tendon can lead to deep infrapatellar bursitis. Its location also makes it susceptible to traumatic causes of bursitis, and septic bursitis.
After injury, synovial cells in the bursa thicken and may undergo villous hyperplasia. Over time, granulation tissue and fibrous tissue may develop. If an inflammatory reaction occurs, the bursa becomes filled with fluid.
Patient Presentation
Patients with prepatellar or infrapatellar bursitis typically report a history of chronic kneeling, or a recent increase in time spent kneeling. They may also report difficulty walking and pain that is exacerbated by kneeling. Abrasion of the skin with marked swelling (Figure 2) suggests an infectious etiology.

Chronic prepatellar bursitis can present with a soft, non-tender boggy mass on the anterior aspect of the patella, while acute bursitis can present as an erythematous, warm and tender mass. Patients with infrapatellar bursitis exhibit tenderness and edema over the patella tendon. Strength and range of motion are often unaffected but may be limited secondary to pain.
Patients with pes anserine bursitis commonly report medial knee pain that is exacerbated by arising from a seated position or ascending stairs. Patients often do not localize the pes anserine as the source of pain. On exam, patients typically have tenderness near the pes anserine extending to the joint line. The pes anserine is typically 5-7 centimeters below the joint line and 3-4 centimeters medial to the tibial tubercle. Flexion of the knee with the patient supine can help identify the pes anserine. While in this position, if the patient pushes their heels into the table, the gracilis and semitendinosus tendon become more prominent. Resisted knee flexion with the patient lying prone can reproduce symptoms. Hamstring tightness should also be assessed to determine its potential contribution to bursa pain.
Objective Evidence
Patients presenting with anterior or medial knee pain should be evaluated with plain radiographs to assess for fractures and presence of osteoarthritis.
Given the soft tissue nature of knee bursitis, radiographs are not helpful in confirming the diagnosis but may reveal a bony prominence that irritates the bursa.
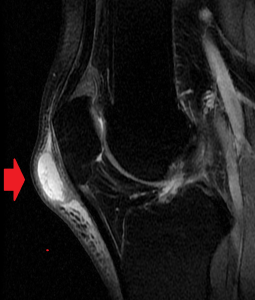
MRI and ultrasound can be useful in localizing soft tissue edema and ruling out other injuries such as MCL or meniscal tears; however, they are not typically required for diagnosis, but if bursitis is present, MRI will detect it (Figure 3).
Musculoskeletal ultrasound is emerging as a viable imaging modality to assess the knee joint. Advantages include its ease of availability, economic savings compared to MRI, ability to easily compare abnormalities to the contralateral side, demonstration of fibrillar microanatomy of tendons, ligaments, and muscles, and the ability to compress and dynamically assess structures. Musculoskeletal ultrasound can be utilized to distinguish difficult cases of joint effusion from that of bursal swelling.
Aspiration of an acutely inflamed bursa can help determine if the bursitis is septic in nature.
Non-infectious (aseptic) bursitis is characterized by cell counts lower than 2000/µL. The presence of a predominance of polymorphonuclear leukocytes or a count greater than 5000/µL should be considered indicative of infection.
The fluid should also be examined for monosodium urate crystals (as seen in gout) or calcium pyrophosphate crystals (as seen in pseudogout).
If infection is suspected, the fluid should be sent for Gram stain and culture. Staphylococcus aureus is responsible for about 80% of cases of septic bursitis of the knee.
Varying degrees of inflammation occur in bursitis. The fluid is usually rich in fibrin, but can be hemorrhagic.
A complete blood cell count and blood cultures should be collected if there is concern for systemic infection.
Epidemiology
Bursitis is common: this diagnosis accounts for 0.4% of primary care clinic visits.
The epidemiology of prepatellar bursitis and infrapatellar bursitis are similar. Males have a greater prevalence of prepatellar and infrapatellar bursitis and may be four times more likely to experience bursitis. There is increased prevalence among workers or clergy that spend a significant amount of time kneeling. The prevalence of prepatellar or infrapatellar bursitis is highest amongst construction workers and skilled blue collar workers (painters, plumbers, etc.), approximately 2%. Prepatellar bursitis is also common among wrestlers for the same reason.
Pes anserine bursitis accounts for approximately 2.5% of symptomatic knee evaluations. Pes anserine bursitis affects both young, athletic patients and older patients with knee osteoarthritis. There is also an increased incidence in obese patients, especially females. Interestingly, pes anserine bursitis occurs more frequently in the right knee than in the left knee. Bilateral bursitis occurs in approximately one third of patients.
Differential Diagnosis
Knee bursitis is one of the many causes of knee pain. Once it is established that there is apparent enlargement of the bursa, the differential diagnosis must separate septic bursitis from noninfectious conditions, and distinguish between bursal inflammation and other soft tissue masses. Septic prepatellar bursitis presents with an acute onset of pain, erythema and focal tenderness. This may follow a history of trauma or cellulitis. Notably, a long-standing bursa can be, acutely infected. A soft tissue mass, such as a lipoma, can present as a firm non-tender, non-erythematous mass on the anterior aspect of the knee. Cellulitis can present with erythema and pain. Often, there is a known history of trauma to the skin. This may be confused with acute septic bursitis. Cellulitis has limited edema and typically spreads, while bursitis remains limited to the bursa.
It is important to recall that many patients with pes bursitis will also have medial compartment arthritis, and therefore it becomes important to distinguish between bursal pain and true joint pain. Bursal pain may be most amenable to physical therapy and medication; detecting the bursa as a source of the pain may prevent overtreatment of the underlying arthritis.
Infrapatellar bursitis may present with symptoms that are indistinguishable from those caused by patellar tendinitis. Fortunately, the treatment of the two is roughly the same and therefore they may not need to be precisely differentiated.
Red Flags
Patients with fever, severe knee pain, inability to bear weight and significantly limited range of motion should be evaluated for a septic joint or septic prepatellar bursitis. Patients with systemic symptoms such as fevers, chills, night sweats, and tachycardia should be evaluated for a systemic infection (sepsis).
Treatment Options and Outcomes
Treatment options for knee bursitis include benign neglect (“observation”), weight loss, non-steroidal anti-inflammatory medication (NSAIDs), physical therapy, aspiration with or without corticosteroid injections, immobilization and in rare instances operative treatment.
Extracorporeal shock wave therapy and kinesio-taping have also been investigated as potential treatments but are not commonly utilized.
Generally, non-septic bursitis is a self-limited condition. Treatment is best focused on addressing the inciting condition to prevent recurrence.
In the case of pes anserine bursitis, observation alone is usually not an effective approach. That is because bursitis in this location is commonly due to an underlying condition such as obesity or muscular tightness. Until the underlying cause is addressed, the bursitis will persist. Weight loss can help alleviate the symptoms of pes anserine bursitis. NSAIDs are used when tolerated to decrease bursa inflammation and pain. Physical therapy can decrease pes anserine symptoms by stretching the hamstring muscles, thus relieving pressure on the bursa. Physical therapy also focuses on strengthening the quadriceps and other knee stabilizing muscles.
Corticosteroid injected directly into the bursa can relieve symptoms by decreasing the inflammatory response. Like NSAIDs, corticosteroids can be used in conjunction with other treatment to increase efficacy.
Unlike pes anserine bursitis, prepatellar and infrapatellar bursitis can be treated with lifestyle modification and the use of knee pads. NSAIDs can be used to decrease inflammation; however, corticosteroid injections are generally avoided due to the risk of infection in prepatellar and infrapatellar bursitis. In the case of chronic prepatellar bursitis, corticosteroid injection can be used if other treatment modalities have failed.
Patients with septic bursitis are treated with antibiotics, splint immobilization, and urgent bursal aspiration. Aspiration may be repeated if the fluid re-accumulates. These patients may require surgical debridement if antibiotic treatment and aspiration of the bursa is not successful.
Operative bursectomy may be utilized also for cases of intractable non-infectious bursitis.
There is limited published data about the outcomes of knee bursitis treatments. Most patients treated with oral or topical NSAID experience significant symptom relief. Both physical therapy and corticosteroid injection significantly improve pain and symptoms secondary to pes anserine bursitis. Approximately 70% of patients treated with steroid injections will experience significant improvement, and 30-91% will experience resolution of symptoms.
Extracorporeal shock wave therapy is more effective than placebo for pes anserine bursitis symptom relief. Kinesio-taping for pes anserine bursitis may be superior to naproxen combined with physical therapy for both pain and tissue swelling relief.
Surgical bursectomy is an effective treatment for persistent bursitis; up to 80% of patients will have complete resolution of symptoms and return to pre-injury work and activities. However, patients with jobs that require significant kneeling or with chronic prepatellar bursitis may continue to be symptomatic.
Risk Factors and Prevention
Valgus knee deformity, obesity, diabetes, and female sex are risk factors for pes anserine bursitis. The risk for pes anserine bursitis can be decreased by stretching the hamstring muscles as well as strengthening the quadriceps and secondary knee stabilizing muscles. Maintenance of a healthy weight can also decrease the risk of pes anserine bursitis.
Blue collar employment, significant kneeling, and male sex are risk factors for prepatellar and infrapatellar bursitis. The risk of prepatellar and infrapatellar bursitis can be reduced by the use of knee pads when kneeling for an extended period of time and activity modification when possible.
Miscellany
Prepatellar bursitis is commonly known as housemaid’s knee. Housemaids would injure this bursa due to frequent kneeling when cleaning.
Infrapatellar bursitis is commonly known as clergyman’s knee. Clergyman injured this bursa by commonly kneeling on hard surfaces while in prayer.
The university financial officer is called “bursar”, for in the old days, he (and it always was a “he”) carried the college’s sack of coins.
Key Terms
Knee bursitis, pes anserine, patella, inflammation
Skills
Identify bursas on exam by palpation of key lower extremity anatomical landmarks. Recognize septic bursitis.
