23 Cruciate Ligament Disorders
The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) connect the femur to the tibia and stabilize the knee joint, primarily in the sagittal plane (i.e., resisting anterior and posterior displacement, respectively). Of the two, it is the anterior cruciate ligament that is more frequently injured, either in isolation or with associated injuries to the meniscus, articular cartilage or collateral ligaments. Tears of the ACL typically occur when a person abruptly changes direction or decelerates with the foot planted. The less common PCL injury usually occurs when the tibia is forced poseriorly when the knee is flexed. The classic mechanism is an automobile accident in which the flexed knee strikes the dashboard after collision. The anterior cruciate ligament has very little healing potential, whereas the posterior cruciate ligament can occasionally repair itself.
Structure and Function
The cruciate ligaments are named according to their attachment on the tibia: the anterior cruciate ligament courses from the posterior aspect of the intercondylar notch on the femur and inserts on the anterior tibial plateau. Similarly, the posterior cruciate ligament courses from a more anterior position in the notch to the posterior aspect of the proximal tibia. The term “cruciate” refers to the fact that these ligaments cross each other (Figures 1, 2 and 3).


The ACL has been described having two bundles: the anteromedial bundle and the posterolateral bundle. This distinction is somewhat arbitrary as the boundary between bundles is not stark. A better way to think about it, perhaps, is that there are different regions of the ligament, with the anteromedial aspect more taut in flexion and the posterolateral aspect more taut during extension.
Injury to the ACL is usually caused by excessive force moving the tibia anterior relative to the femur, sometimes in combination with internal rotation of the tibia at the knee. This rotation increases the distance between the origin and insertion of the ligament, such that the ligament is under greater tension for a given degree of anterior displacement.
Varus or valgus (clipping) forces at the knee can also injure the ACL but only after the affected collateral ligament is injured first.
So-called cutting maneuvers (rapid changes in direction while running) are very common mechanisms for ACL injuries. When the foot is planted the tibia is anchored in space, whereas the body’s center of gravity may pull the femur in a different direction.
Mechanoreceptor nerve fibers are found within the ACL and provide proprioception. Thus, an injury can create a sense of instability not only because of the loss of passive restraint but because of the loss of proprioception.
The PCL also lies within the intercondylar notch. It originates from the inner aspect of the medial femoral condyle and attaches to the posterior aspect of the proximal tibia, slightly below the joint line.
Like the ACL, the PCL also has two bundles, called the anterolateral bundle and the posteromedial bundle. The anterolateral bundle is tightest in knee flexion and prevents posterior translation of the tibia relative to the femur. The posteromedial bundle is tightest in extension of the knee and prevents hyperextension of the knee.
A posterior-directed force that pushes the tibia backwards while the knee is flexed can tear the PCL. Alternatively, a force that causes sufficient hyperextension of the knee can also cause a PCL injury, but this is less commonly seen.
The PCL is at least 25% stronger than the ACL, being able to resist forces up to 3000 N.
Patient Presentation
Patients with a torn ACL will typically present with immediate swelling and pain.
Patients will commonly report hearing a popping sound or perceiving a popping sensation at the time of the injury.
The classic mechanism of injury for an ACL tear is a non-contact injury after a sudden pivot with the leg planted – think of a skier whose ski is fixed on the snow and twists his or her torso.
The knee may fill with blood (forming a so-called hemarthrosis). This fluid collection may make motion painful, but also may stabilize the knee. This false stability is enough to mask the tear on examination.
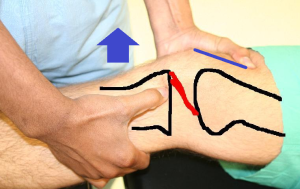
The most sensitive physical exam maneuver for detecting a torn ACL is the Lachman test, where the femur is stabilized while the tibia is pulled forward (Figure 4). A positive test is signified by excessive forward translation without a firm endpoint, indicating disruption to the ACL. Because the Lachman test is assessed by the perceived firmness of the endpoint – an intact ACL will stop anterior translation more suddenly – experienced examiners will perform the test more accurately.
The anterior drawer test (simply assessing whether there is an abnormal amount of anterior displacement when a force is applied to the flexed knee) is another physical exam maneuver that is similar to the Lachman test but is less accurate. That is because a varying degree of anterior translation is normal, and whether what the examiner is perceiving represents an abnormal amount may be difficult to tell.
Another specific test to assess for ACL instability is the pivot shift test. This test is a diagnostic maneuver that moves the tibia in and out of its normal anatomical position, if and only if the ACL is damaged. The test is performed with the examiner grasping the leg and holding the knee in extension (with a slight internal rotation torque to the tibia). In this position, the tibia will subluxate anteriorly relative to the femur if the ACL is torn. The knee is then flexed. In flexion, the knee is in its normal position, even if the ACL is torn. Thus, if the knee is noted to clunk back into position during flexion, the test is positive (for a torn ACL). This test may be difficult to perform in the apprehensive patient, but is a critical component of the physical examination when performed under anesthesia.
Tests for ACL tears can be falsely negative if there is a displaced fragment of either bone or cartilage in the knee or if the hamstrings are resisting the examiner. Also, as noted, the fluid in the knee may stabilize it somewhat and therefore if there is a tense effusion the Lachman test may be falsely negative as well.
It may be diagnostically and therapeutically helpful to aspirate the knee. Removing the volume of fluid will make the patient more comfortable. Also, merely assessing the color of the fluid helps with diagnosis (red, meaning blood, signifies a clinically important injury in approximately 90% of cases). In addition, by draining the knee, a more reliable physical examination can be performed.
Patients with chronic deficiency of the anterior cruciate ligament present with a “trick knee”, that is a sense of instability. They may also present with the stigmata of arthritis, as the loss of the ACL leads to abnormal biomechanics which in turn can cause articular damage.
The classic presentation of a patient with a PCL injury is generalized knee pain, a limp, and mild to moderate knee swelling.
Patients with injuries to the PCL do not typically describe a popping sensation, but they may report a direct blow to the knee.
The most accurate physical exam maneuver for PCL tears is the posterior drawer test, where the knee is flexed at 90 degrees and a posterior force is applied to the anterior proximal tibia, driving it backwards. A positive sign is excessive posterior translation of the tibia relative to the femur, as compared to the uninjured side and the lack of a firm endpoint.
Patients with chronic PCL deficiency do not complain of instability but rather anterior knee pain. That is because patients have learned to stabilize their knee by “holding on” to their tibia with active quadriceps force. This quadriceps force loads the patellofemoral joint causing articular degeneration.
Objective Evidence
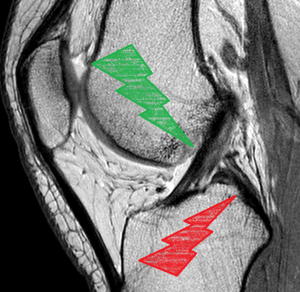
While x-rays can and should be obtained to rule out concomitant fracture or avulsion injury to the bones of the knee (i.e., Segond fracture – a fleck of bone off the anterolateral tibia that is pathognomonic for ACL injury), the gold standard imaging modality for definitive diagnosis of both ACL and PCL injuries is an MRI of the knee (Figure 5).

On sagittal view, absence or discontinuity of ACL fibers would indicate an ACL injury.
The classic finding for an ACL tear on MRI is a so-called kissing contusion on both the tibia and femur: this is a bone bruise caused by the impact of the lateral tibial plateau into the middle of the femoral condyle, a region known as the sulcus terminalis.
Epidemiology
ACL injury is common in athletes, especially in the high school age group. Female athletes are particularly prone to ACL injury. However, ACL injury is still common in college and professional athletes, as well as the general population. The estimated incidence of ACL injuries per year is about 200,000 in the United States. Approximately half of all ACL tears are isolated injuries; the other half are associated with either damage to the meniscus or collateral ligaments.
PCL injuries are less common, owing to the ligament’s greater strength but also because pivoting while running is not apt to tear it. The most common mechanism of PCL injury involves motor vehicle accidents, with contact from the dashboard against the flexed knee pushing the tibia in a posterior direction.
Differential Diagnosis
In the acute setting, the goal is to identify all of the injured structures. Concomitant injuries are common.
Assuming radiographs do not show a fracture, the other structures that might be injured include the collateral ligaments, the menisci and the articular surfaces.
Patella dislocations may occur with a history that suggest a cruciate ligament injury: namely, a twisting mechanism, a sense of a “pop” and bleeding into the knee.
The PCL in particular is usually associated with other ligamentous injury, especially injuries to the posterolateral corner of the knee, which tends to make it relatively more difficult to diagnose compared to ACL injury.
Bony contusions, fractures, and knee dislocation are also generally included in the differential diagnosis for PCL injuries.
Red Flags
A patient’s inability to fully extend the knee may be due to a displaced tear of the meniscus. This requires urgent arthroscopic surgery not only to remove the mechanical block and restore the range-of-motion of the knee but to possibly preserve the tissue for repair.
A young male patient may present with both an effusion and a history of knee pain after playing sports but the two may not be related. Rather, the joint fluid in this case may actually be caused by gonorrhea. This can be assessed by a short question about urethral symptoms.
Treatment Options and Outcomes
Patients with less severe ACL injury or willingness to modify their activities may be successfully treated with physical therapy and some degree of immobilization (e.g. use of a brace while playing sports).
There is a school of thought (more so in Europe than in the United States) that perhaps all patients should be treated non-operatively at first, as many will do fine with therapy alone. The downside to this approach is that those patients who are unstable enough to ultimately need surgery often inflict greater damage on the knee in the interval between the initial injury and the surgical treatment.
Younger patients, athletes, and those with severe instability of the knee are more likely to require operative reconstruction in order to return to their desired activity level. ACL tears should be evaluated by an orthopedic surgeon to determine if surgery is indicated.
The first consideration when contemplating surgical repair of PCL injuries is the degree of injury. If not torn completely, the PCL has particularly high potential to heal with immobilization and then therapy. These exercises can assist with stability of the knee, particularly by strengthening the quadriceps muscles (which have an anterior-directed vector in their normal action).
PCL surgery is most commonly indicated when there is another injury (e.g., the posterior-lateral corner ligaments) when patients continue to have persistent feelings of posterior tibial instability or, more commonly, they develop anterior knee pain. That pain reflects overuse of the quadriceps to stabilize the knee, which then produces overload to the patellofemoral joint.
In both ACL and PCL injury, surgical repair involves replacement of the injured ligament with a graft (Figure 6). This may be from the patient’s own patellar or hamstring tendons or from a cadaver. The damaged ligament itself is removed and discarded. The repair is typically done arthroscopically.

Autografts are generally favored over allografts in patients 25 years old or younger, given the lower rate of re-tears as compared to allografts in this population.
The surgery for ACL and PCL reconstruction typically involves creating tunnels in the bone of the tibia and femur through which the grafted tendon will be inserted and fixed. These are then fixed into the tunnels, typically with screws. Other techniques can be used as well, but they all generally involve fixation of the graft on either end onto the bone of the femur and tibia.
Both ACL and PCL surgical repairs require postoperative rehabilitation. Rehabilitation exercises focus on regaining normal range of motion and strengthening the quadriceps and hamstring muscles. Care must be taken not to overload or overstress the graft during the initial phases of healing.
The outcomes for ACL reconstruction are generally very good at least in the medium term. In the past, ACL tears in particular would end careers for professional athletes, but improvements in surgical reconstruction have allowed athletes to essentially regain full functional stability. It is common to see patients return to their high-level performance. The long term risk of arthritis does loom, as even the best surgical reconstruction is not as good the native ligament, and the articular surface may have been irreparably damaged by the impact at the time of injury.
The outcomes of PCL reconstruction are typically very good to excellent, but because the surgery is reserved for only severe injuries, usually, the knee is not perfect post-operatively.
With both ACL and PCL injuries, outcomes are worse if there is a concomitant articular or meniscal injury.
Risk Factors and Prevention
For ACL injury, risk factors include high school age, female gender, and playing soccer or basketball. For PCL injury, athletes such as American football linemen may be at increased risk.
Prevention of either injury relies upon strengthening of the muscles that stabilize the knee joint and promote endurance. It is not uncommon to see ACL tears later in the day on the ski slopes, which may reflect the loss of hamstring stabilization due to muscle fatigue. That is, if the hamstrings are tired and weak, they may not be able to hold on to the tibia, which then exposes the ACL to greater forces. Teaching proper landing technique may also reduce risk of ACL injury.
Key Terms
Arthroscopy, anterior cruciate ligament, posterior cruciate ligament, knee, tibial plateau
Skills
Examination of cruciate ligament injuries to the knee.
