21 Chondral Injuries of the Knee
Chondral injuries of the knee are lesions of the articular cartilage of the knee joint. (The colloquial expression “cartilage damage” might also include meniscal tears, which is an altogether separate category of disease.) Chondral injuries include both single focal defects and diffuse damage more characteristic of degenerative joint disease. Acute focal defects can accompany injuries such as an ACL tear and patellar dislocation. Articular cartilage damage can be seen with or without changes in the underlying bone. When bone pathology is absent, repair of the surface cartilage may be very helpful clinically, whereas when bone changes are present, the cartilage damage is merely the surface manifestation of the disease, and treating it alone is often futile.
Structure and Function
The knee is a hinged synovial joint and consists of two articulations– the tibiofemoral and patellofemoral. The medial and lateral condyles of the femur rest on the tibial plateau to form the tibiofemoral articulation. The anterior aspect of the distal femur (trochlea) meets the patella to form the patellofemoral articulation. These joints are covered by articular cartilage.
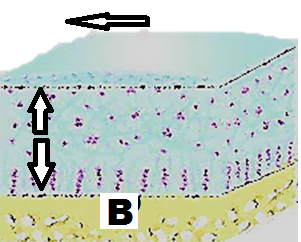
In brief, articular (hyaline) cartilage decreases friction and distributes loads. The key to both properties is water: articular cartilage contains chondrocytes, proteoglycan and collagen molecules (almost all Type II), but at least 2/3rd of its mass is water. Articular cartilage has characteristic zones, in which the more superficial zone aspects have the collagen oriented parallel to the joint (for gliding) and the deep layer has its collagen oriented perpendicular to the joint (for compressibility). The deepest layer, the tidemark, is calcified and attaches to the subchondral bone (Figure 1). This organization distinguishes articular cartilage from the fibrocartilage that appears in some healing response. Fibrocartilage lacks this organization and thus lacks the normal mechanical properties and the durability of articular cartilage.
Another important biological principle regarding articular cartilage is that mild repetitive loading stimulates proteoglycan production whereas both immobilization and excessive repetitive loading leads to proteoglycan loss. That is to say, the health of the joint demands that the cartilage must be loaded within its physiological envelope of function: too much loading will cause damage, but too little loading will cause wasting.
The tibiofemoral articulation carries most of the body’s weight across the knee (medial more than lateral). Because of leverage effects the patellofemoral joint is also exposed to high compressive forces. Both articulations are susceptible to articular cartilage injury.
Patient Presentation
It is important to recall that patients do not present complaining of chondral injuries, per se. Rather they present complaining of a recent injury or subacute pain, and it is the examiner’s task to determine whether a chondral lesion contributes to the presentation.
Chondral lesions commonly accompany injuries such as ACL tear and patellar dislocation. The cartilage is damaged by impact: in the case of an ACL tear, the tibia damages the lateral femoral condyle in a characteristic spot of contact (a so-called kissing lesion). Patellar dislocation can cause cartilage damage either as the bone goes out of place or when it is reduced (returns to the trochlea).
Defects can also be found incidentally on MRI or arthroscopy.
If there is no history of acute trauma, the pain usually is described as dull and aching. Patellofemoral lesions are usually associated with pain or discomfort after sitting for long periods of time. (This is known as the “theater sign”.) Activity-related pain involves weight-bearing activities and are more common with tibiofemoral lesions. Other symptoms include effusion, catching, locking, and instability.
Other contributing factors may be noted on either history or physical exam, including prior patellar subluxation or dislocation, malalignment, or joint laxity due to ligamentous insufficiency.
The physical exam should assess patellar position and varus/valgus alignment. While sitting, assess quadriceps angle, tibial torsion, quadriceps atrophy (especially of the vastus medialis) and knee range of motion.
The supine exam should focus on effusion, decreased quadriceps or gastrocnemius flexibility, and patellar abnormalities. Tenderness to palpation over the joint line or directly over the femoral condyle would be expected with femoral condyle lesions. Pain with patellar compression would be expected with patellofemoral lesions.
Objective Evidence
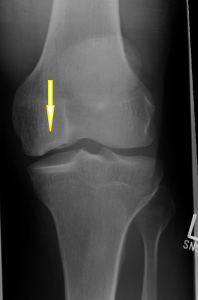
X-rays are mainly used to rule out arthritis and assess for malalignment. Large osteochondral lesions, if present, will be apparent (Figure 2).
CT scanning is helpful when assessing patellar lesions, as it can more precisely measure the distance between the tibial tuberosity and the trochlear groove. Greater distances signify worse tracking of the patella and may prompt a need for surgical realignment.
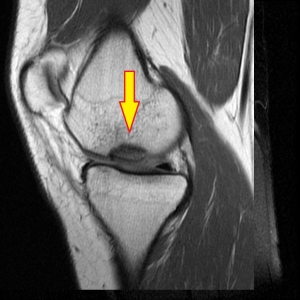
MRI is the imaging of choice and most sensitive available for evaluating focal lesions (Figure 3). It also is the most essential for determining surgical vs. non-surgical management as it has the highest sensitivity and specificity for detecting osteochondral fragmentation.
Lab findings are not usually helpful for evaluation of mechanical injuries such as chondral defects. However, inflammatory markers and disease-specific tests can be used to rule out inflammatory disease that may contribute to accelerated disease processes in the joints. Examples include systemic lupus erythematous and rheumatoid arthritis.
Epidemiology
Chondral injuries are more common in the adult and elderly population, likely a result of both degeneration and traumatic damage over time. About 10% of the population older than 40 years old have chondral defects. Traumatic knee injury can result in chondral defects in young patients.
Differential Diagnosis
Concomitant osteoarthritis and meniscus tears of the knee can present similarly to chondral lesions with pain, swelling, and mechanical issues such as catching.
An articular defect may also be due to osteochondritis dissecans. This is almost always present in the posterolateral aspect of the medial femoral condyle in skeletally immature patients. Recurrent effusions of the knee are commonly seen. This lesion is often amenable to treatment, and therefore it should not be missed. A child presenting with knee pain but without a significant history of trauma should raise appropriate clinical suspicion.
Red Flags
Chondral defects are usually associated with an effusion, and an effusion can of course suggest either septic or inflammatory arthritis. Aspiration and laboratory analysis of the fluid can be performed under the appropriate conditions to exclude these.
Treatment Options and Outcomes
Treatment of a chondral lesion in the context of diffuse degenerative joint disease is dictated by the treatment needed for the arthritis.
For focal lesions, non-surgical management is the preferred initial treatment modality for most presenting cases and is the best route for those without significant symptoms. Common non-operative orthopedic management methods are used here, including activity modification, physical therapy, weight loss, exercise, NSAIDs and possibly corticosteroid injection.
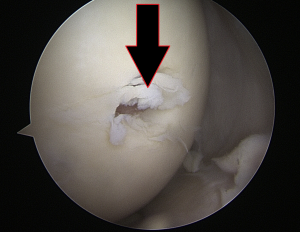
Surgical management is considered in the young patient (<50 years old) who has attempted non-operative treatment with continued long-standing and functionally limiting symptoms, especially those related to a loose chondral fragment. Factors such as lesion size, depth, location, and status of the underlying chondral bone are all considered. At times, arthroscopy is needed to characterize the size and depth of the lesion (Figure 4).
The classic surgical candidate is a young, active patient presenting with acute osteochondral fracture and full-thickness loss of cartilage. Strong contraindications to surgery include inflammatory disease and obesity. Relative contraindications include mechanical issues such as joint laxity, mal-alignment and ligamentous laxity.
The best form of surgical treatment leads to healing. Unfortunately, many articular lesions are not amenable to true healing. Fixation of a cartilage flap and drilling of the underlying bone is reliable only in patients with open growth plates, though this may be attempted in others.
Debridement, typically through arthroscopy, of course can clear debris and minimize mechanical symptoms, but given that the remaining articular cartilage is not normal, long-term positive results are hardly assured. Recall that the top layer is structurally and functionally different than the bottom layers, so damage to and loss of the superficial layer produces not only thinner articular cartilage but qualitatively worse articular cartilage: if there is surface abrasion, the top layer (the lamina splendans) is simply missing. This top layer helps protect the cartilage from damage, and its loss leaves it susceptible to further erosion.
There are a few techniques for filling defects: so-called marrow stimulation, in which fibrocartilage formation is induced; grafting; and chondrocyte implantation.
Marrow stimulation (also known as micro-fracture, abrasion chondroplasty and osteochondral drilling, depending on the specific method) aims to allow access of mesenchymal stem cells of the marrow into the articular defect to stimulate the formation of repair tissue, i.e. fibrocartilage. This technique is most effective in small lesions on the femur; it is less favored on the patella, in larger lesions, and in younger patients.
Grafting can be in the form of an autograft or an allograft. Osteochondral autografting fills a cartilage defect located in a critical area with plugs of normal autologous cartilage (with bone underneath) harvested from a less critical area. Ideally, the chondrocytes in the plug remain viable, and the bone heals into the subchondral bed in which it is placed (Figure 5).

The “plug” technique is limited by the fact that articular cartilage will appear during early growth and development only in response to loadbearing. It is accordingly impossible to harvest cartilage from a non-weight-bearing part of a joint; at best one can hope to harvest from an area that is used sparingly. Accordingly, there may be some donor site morbidity when plugs are harvested. Also, the radius of curvature of the cartilage defect unlikely matches the radius of curvature of the harvested plug precisely.
Larger defects can be filled with cadaveric donor cartilage and bone. This technique of course brings with it the risk of infection, and chondrocyte viability may be lower.
Autologous chondrocyte implantation (ACI) attempts to foster regeneration of cartilage. The technique begins by harvesting a piece of native cartilage from the edge of the weight-bearing surface, usually from the intercondylar notch or periphery of the trochlea. Then, this is sent to a commercial laboratory where chondrocytes are isolated and encouraged to proliferate. This larger volume of cartilage cells are then re-implanted under a soft-tissue flap during a second procedure. This is the most expensive approach but does offer potential benefits that other operations lack.
If a defect arises from malalignment and uneven loading, then a realignment procedure may be indicted. In the patellofemoral joint, a tibial tubercle osteotomy may improve patellar tracking. In the tibiofemoral joint, a high tibial osteotomy or distal femoral osteotomy can help.
To date, the literature analyzing the long-term surgical outcomes of osteochondral defects is limited. A randomized controlled trial of adequate numbers of patients for the various operations (including a placebo), assessing not only short term function but long term avoidance of arthritis–the true measures of success–is highly infeasible.
Risk Factors and Prevention
Risk factors include an unstable knee joint, malalignment and excessive repetitive activity. Addressing instability when it occurs should theoretically protect the joint surface, but it is unclear whether our methods of ligament reconstruction are sufficiently physiologic to truly protect the joint surface.
Miscellany
It is probably best to avoid the initials “OCD” to describe articular lesions, as these three letters may suggest both “osteochondral defect” as well as “osteochondritis dissecans”. There is some overlap between the two: however, there are important distinctions that should be preserved. Osteochondritis dissecans may be associated with a defect, but certainly not all defects represent osteochondritis dissecans. The treatment and prognosis of osteochondritis dissecans (especially in young patients) is altogether different than that of osteochondral defects in general.
Key Terms
Femoral condyle defect, patellofemoral defect, osteochondritis dissecans, microfracture, osteochondral autograft transfer, autologous chondrocyte implantation, transtibial-trochlear groove distance
Skills
Recognize and identify a chondral defect on imaging. Perform a physical exam to detect related instability or malalignment. Analyze imaging to characterize articular lesions.
