Support Systems of the Body
9 Skeletal System
Introduction
Learning Objectives
Describe the functions of the skeletal system.
How important are your bones and your skeletal system?

Try to imagine what you would look like without them. You would be a soft, wobbly pile of skin, muscles, and internal organs, so you might look something like a very large slug. Not that you would be able to see yourself—folds of skin would droop down over your eyes and block your vision because of your lack of skull bones. You could push the skin out of the way if you could only move your arms, but you need bones for that as well!
Humans are vertebrates, which are animals that have a vertebral column or backbone. Invertebrate animals, like the banana slug below, do not have a vertebral column, and they use a different mechanism than vertebrates to move about. The sturdy internal framework of bones and cartilage found inside vertebrates, including humans, is called an endoskeleton. The adult human skeleton consists of approximately 206 bones in adults. An endoskeleton develops within the body rather than outside like the exoskeleton of insects.
Are bones living?
It’s common to think of bones as not living. But bones are very much living. In fact, you are constantly making new bone tissue. That means that you are also constantly getting rid of bone. Bone is full of blood, nerves, and all sorts of cells and proteins, making it an extremely complex living tissue.
Many people think of bones as dry, dead, and brittle, which is what you might think if you saw a preserved skeleton in a museum. The association of bones with death is a common association because the calcium-rich bone tissue of a vertebrate is the last thing to decompose after the organism dies. However, the bones in your body are very much alive. They contain many tough protein fibers, are crisscrossed by blood vessels, and certain parts of your bones are metabolically active. Preserved laboratory skeletons are cleaned with chemicals that remove all organic matter from the bones, which leaves only the calcium-rich, mineralized (hardened) bone tissue behind.
Bone, or osseous tissue, is a hard, dense connective tissue that forms most of the adult skeleton, the support structure of the body. In the areas of the skeleton where bones move (for example, the rib cage and joints), cartilage, a semi-rigid form of connective tissue, provides flexibility and smooth surfaces for movement. Bones are the primary organs in the skeletal system. Their functions include:
- protection of vital structures, such as the spinal cord, brain, heart, and lungs
- support of body structures
- body movement through coordination with the muscular system
- hematopoiesis, or generation of blood cells, within the red marrow spaces of bones
- storage and release of the inorganic minerals calcium and phosphorous, which are needed for functions such as muscle contraction and neural signal conduction.
- Energy Storage: The yellow marrow in the bones stores fats, which can serve as an energy reserve.
The most apparent functions of the skeletal system are the gross functions—those visible by observation. Simply by looking at a person, you can see how the bones support, facilitate movement, and protect the human body. Just as the steel beams of a building provide a scaffold to support its weight, the bones and cartilage of your skeletal system compose the scaffold that supports the rest of your body. Without the skeletal system, you would be a limp mass of organs, muscles, and skin. Bones also facilitate movement by serving as points of attachment for your muscles. While some bones only serve as a support for the muscles, others also transmit the forces produced when your muscles contract. From a mechanical point of view, bones act as levers and joints serve as fulcrums. Unless a muscle spans a joint and contracts, a bone is not going to move. Bones also protect internal organs from injury by covering or surrounding them. For example, your ribs protect your lungs and heart, the bones of your vertebral column (spine) protect your spinal cord, and the bones of your cranium (skull) protect your brain.
On a metabolic level, bone tissue performs several critical functions. For one, the bone matrix acts as a reservoir for a number of minerals important to the functioning of the body, especially calcium and phosphorus. These minerals, incorporated into bone tissue, can be released back into the bloodstream to maintain levels needed to support physiological processes. Calcium ions, for example, are essential for muscle contractions and controlling the flow of other ions involved in the transmission of nerve impulses.
Bone also serves as a site for fat storage and blood cell production. The softer connective tissue that fills the interior of most bones is referred to as bone marrow. There are two types of bone marrow: yellow marrow and red marrow. Yellow marrow contains adipose tissue; the triglycerides stored in the adipocytes of the tissue can serve as a source of energy. Red marrow is where hematopoiesis—the production of blood cells—takes place. Red blood cells, white blood cells, and platelets are all produced in the red marrow.
Learn By Doing 10.1
Bone tissue can be described as ________.
- dead calcified tissue
- cartilage
- the skeletal system
- dense, hard connective tissue
Which function of the skeletal system would be especially important if you were in a car accident?
- storage of minerals
- protection of internal organs
- facilitation of movement
- fat storage
Without red marrow, bones would not be able to ________.
- store phosphate
- store calcium
- make blood cells
- move like levers
Yellow marrow has been identified as ________.
- an area of fat storage
- a point of attachment for muscles
- the hard portion of bone
- the cause of kyphosis
Which of the following can be found in areas of movement?
- hematopoiesis
- cartilage
- yellow marrow
- red marrow
The skeletal system is made of ________.
- muscles and tendons
- bones and cartilage
- vitreous humor
- minerals and fat
Skeletal Structures and Functions
Learning Objectives
- Identify and label the bones of the axial skeletal system.
- Identify and label the bones of the appendicular skeleton.
Bones and Their Articulations
It’s common to think of the skeletal system as being made up of only bones, but the skeletal system contains many types of structures. In addition to localizing blood cell formation and storing calcium, bones come together at locations called articulations (or joints) to allow for locomotion and work. In any complex system that moves (such as a bicycle or car), allowing functional, repetitive motion requires a lot of control and support.
Connective Tissues
In addition to bones, the skeletal system contains other important connective tissues including cartilage and ligaments. Tendons, technically a structure of the muscular system, are also important connective tissue for stabilizing joints and supporting structures.
Cartilage is a firm yet pliable substance that performs various functions: protection, shape maintenance and support, lubrication, and shock absorption. Its primary function is to coat the end of the bones where they articulate with one another, providing a smooth, cushioned surface. Furthermore, cartilage can serve as a template for bone formation during development and bone healing (this will be further discussed in the section about bone ossification).
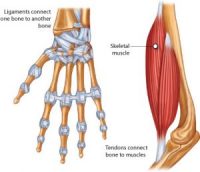
Ligaments and tendons support articulations and control the muscle attachment to the bones. Ligaments connect bones and stabilize articulations. Tendons connect bones to muscles.
The structures of ligaments and tendons are similar in that both tissues are made of fibrous proteins aligned in the direction of the force experienced. The types of proteins and differences in stretch and recoil distinguish the mechanical behavior of ligaments and tendons. Ligaments are stiffer but deform more since they stabilize articulations. Tendons are wrapped with a continuation of the connective tissue (fascia) surrounding muscle cells to help transmit and dissipate force.
Axial Skeleton Anatomy
The adult human skeletal system is composed of 206 bones. The skeleton is divided into two functional groupings—the axial and the appendicular skeleton.
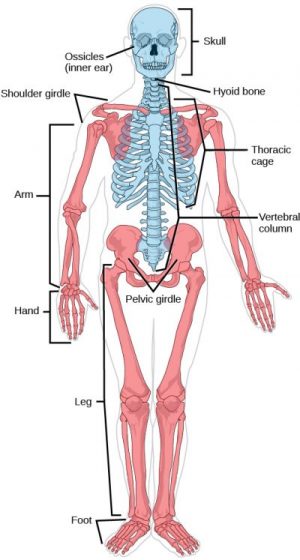
The axial skeleton comprises the skull, hyoid bone, vertebral column, and thorax (ribs and sternum). The axial skeleton protects and supports the head, neck, and trunk organs.
- The skull consists of 22 facial and cranial bones that interlock to form openings for the eyes and provide protection for the brain. The cranium, a collection of bones that protect the brain, and the mandible are the two major parts of the skull.
- The hyoid bone is not attached to any other bone, is located in the neck, and supports tongue movement.
- The vertebral column consists of individual vertebrae separated by cartilaginous disks. The vertebral column forms the middle axis of the skeleton.
- The thoracic cage protects the internal organs of the thorax and upper abdomen. The thoracic cage consists of the ribs and the sternum. The ribs articulate anteriorly with the sternum and posteriorly with the vertebrae of the thorax.
The table below lists the location and function of the major bones of the axial skeleton:
| Bone(s) | Location | Function | Major groups in the axial skeleton |
| Cranium | Head | Supports facial structures, encloses and protects the brain, provides muscle attachments for chewing and moving the head | Skull |
| Mandible | Lower jaw | Permits chewing | Skull |
| Vertebrae | Spine | Permit mechanical stability for the body and protect the spinal cord | Vertebral column |
| Ribs | Chest wall | Provide protection for the organs of the upper body | Thoracic cage |
| Sternum | Center of the chest | Provides attachment for many (not all) ribs | Thoracic cage |
Appendicular Skeleton Anatomy
The appendicular skeleton is composed of the upper limbs, lower limbs, pectoral girdle, and pelvic girdle. The appendicular skeleton functions to anchor the limbs to the axial skeleton.
The pectoral girdle consists of a scapula and clavicle on each side of the body. The pectoral (shoulder) girdle permits movement of the upper limbs by connecting the upper limbs to the axial skeleton.
The upper limbs of the appendicular skeleton are composed of the humerus, the radius, and the ulna, which complement each other to form the forearm, and the wrist. The hand subdivides into smaller bones of the palm and fingers.
The pelvic girdle of the appendicular skeleton is composed of two coxal bones (fused ilium, ischium, and pubis bones), which attach to the vertebral column and the lower limbs.
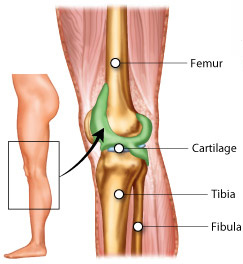
The lower limbs each consist of the femur or thigh bone; the tibia or shinbone, the fibula, or calf bone; and the foot. The patella is the bone located at the point where the femur and tibia articulate with each other. The foot subdivides into smaller bones of the ankle, instep, and toes.
The table below lists the location and function of the major bones of the appendicular skeleton:
| Bone(s) | Location | Function | Major groupings of appendicular bones |
| Scapula | Flat, triangular bone located on the posterior side of each shoulder | Articulates with the clavicle and humerus | Pectoral girdle |
| Clavicle | Located in each shoulder at the base of the neck | Helps to keep the shoulders in place as part of the pectoral girdle | Pectoral girdle |
| Humerus | Extends from the scapula to the elbow | Provides attachments for muscles that move the shoulder and upper arm at the proximal end; articulates with the radius and ulna at the distal end | Upper limbs |
| Radius | Located on the lateral side of the forearm between the elbow and wrist | Provides attachment for muscles that rotate and bend the arm at the elbow and muscles that allow movement of the wrist | Upper limbs |
| Ulna | Located on the medial side of the forearm between the elbow and wrist | Provides attachment for muscles that bend and straighten the arm at the elbow and muscles that allow movement of the wrist | Upper limbs |
| Ilium | Located on the superior portion of the coxal bone | Connects the bones of the lower limbs to the axial skeleton | Pelvic girdle |
| Femur | Extends from the hip to the knee | Provides attachment for muscles of the lower limbs and buttocks; distal end articulates with the tibia and patella | Lower limbs |
| Tibia | Located on the medial side of the leg between the knee and the ankle | Articulates with the femur, on its superior side, to form the knee joint; articulates with the fibula on the lateral side; articulates with the patella on the anterior side; and the tarsels to form the ankle joint | Lower limbs |
| Fibula | Located on the lateral side of the tibia between the knee and ankle | Forms the lateral part of the ankle joint | Lower limbs |
| Patella | Located on the anterior surface of the articulation between the femur and tibia | Supports movement of the knee joint | Lower limbs |
Learn By Doing 10.2
The appendicular skeleton is associated with which function?
- protection of the internal organs
- interaction with the environment
- organizing the structural center of the body
- all of the above are correct
Hint: The appendicular skeleton contains the bones of the arms and legs, and it does not contain major bones along the axis of the body.
Select the name of the bone that is being described from the following: ribs, mandible, sternum, cranium, vertebrae
- The ______________ supports facial structures and encloses and protects the brain.
- The ______________ provide protection for the organs of the upper body.
- The ______________ permits mechanical stability for the body and protects the spinal cord.
- The ______________ provides attachment for many (not all) ribs.
- The ______________ permits chewing.
Which of the following attaches to the vertebral column and the lower limbs?
- Sternal girdle
- Patella girdle
- Pectoral girdle
- Pelvic girdle
Indicate whether each of the following represents a bone in the axial or appendicular skeleton or indicate that it is not a bone at all.
- Mandible
- Tibula
- Hyoid
- Clavicle
- Sternum
- Radius
- Ulna
- Hydro
- Vertebrae
- Scapula
- Patella
- Fibia
Bones – Classification by Microscopic Structure
Learning Objectives
- Describe the classification of bone based on shape.
- Describe the three main components of a long bone.
The bones of your body are mineralized structures that make up a major portion of your skeleton. In the broad sense, a bone is composed of bone tissue, cartilage, ligaments, tendons, vasculature, and nervous tissue. Bone tissue is a collection of specialized cells (osteoblasts, osteoclasts, osteocytes), organic extracellular matrix proteins (collagen and proteoglycans), and inorganic salt crystals that work together to provide strength and flexibility.
Although all bones have a similar composition, their large-scale structures and functions differ. One way to classify bone tissue is based on its microscopic structure.
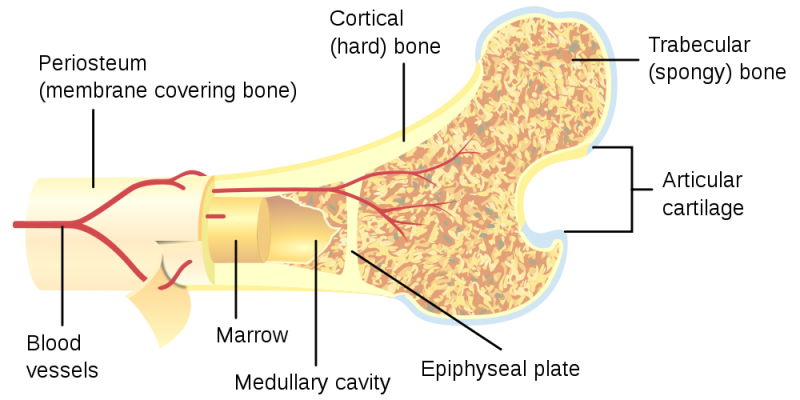
- Bone tissue with a tightly packed microstructure arranged into rings (osteons) is called compact bone (also called cortical or lamellar bone). Compact bone structure gives bones their stiffness. However, if bone structures were made only of compact bone, they would be very heavy and brittle.
- Bone tissue with a porous microstructure is spongy bone (also called cancellous or trabecular bone). Spongy bone consists of branching bone structures called trabeculae. Spongy bone helps to reduce the weight and brittleness of bone and is found at the ends of bone where forces are high. Spongy bone allows bones to bend a slight amount without cracking.
Classification of Bones by Shape
The bones of the human skeleton are classified by their shape: long bones, short bones, flat bones, sutural bones, sesamoid bones, and irregular bones.
Short bones, or cuboidal bones, are bones that are the same width and length, giving them a cube-like shape. For example, the bones of the wrist (carpals) and ankle (tarsals) are short bones.
Flat bones are thin and relatively broad bones that are found where extensive protection of organs is required or where broad surfaces of muscle attachment are required. Examples of flat bones are the sternum (breast bone), ribs, scapulae (shoulder blades), and the roof of the skull.
Irregular bones are bones with complex shapes. These bones may have short, flat, notched, or ridged surfaces. Examples of irregular bones are the vertebrae, hip bones, and several skull bones.
Sesamoid bones are small, flat bones and are shaped similarly to a sesame seed. The patellae are sesamoid bones. Sesamoid bones develop inside tendons and may be found near joints at the knees, hands, and feet.
Sutural bones are small, flat, irregularly shaped bones. They may be found between the flat bones of the skull. They vary in number, shape, size, and position.
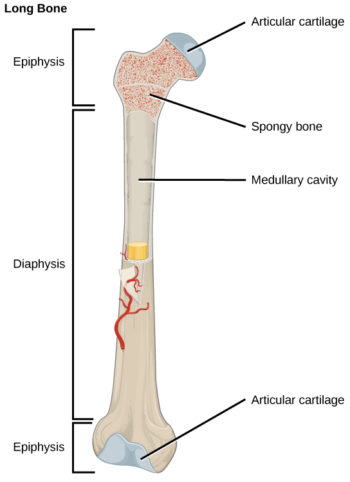
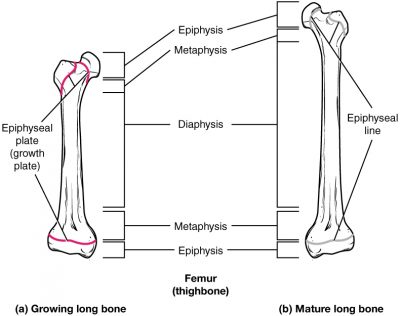
Long bones are longer than they are wide and have a shaft and two ends. The diaphysis, or central shaft, contains bone marrow in a medullary cavity. The rounded ends called epiphyses are covered with articular cartilage and are filled with red bone marrow, which produces blood cells. Most of the limb bones are long bones—for example, the femur, tibia, ulna, and radius. Exceptions to this include the patella and the bones of the wrist and ankle.
All bones have surface markings and characteristics that make a specific bone unique. There are holes, depressions, smooth facets, lines, projections, and other markings. These usually represent passageways for vessels and nerves, points of articulation with other bones, or points of attachment for tendons and ligaments.
Learn By Doing 10.3
Most of the bones of the arms and hands are _______ bones.
- flat bones
- short bones
- sesamoid bones
- irregular bones
- long bones
Which of the following occurs in the spongy bone of the epiphysis?
- bone growth
- bone remodeling
- hematopoiesis
- shock absorption
The diaphysis contains ________.
- the metaphysis
- fat stores
- spongy bone
- compact bone
If the articular cartilage at the end of one of your long bones were to degenerate, what symptoms do you think you would experience? Why?
Joints and Skeletal Movement
Learning Objectives
- Analyze the differences between fibrous, cartilaginous, and synovial joints.
- Describe the structure of a synovial joint.
The point at which two or more bones meet is called a joint or articulation. Joints are responsible for movement, such as the movement of limbs, and stability, such as the stability found in the bones of the skull. Joints can be classified based on their structure. The structural classification divides joints into fibrous, cartilaginous, and synovial joints depending on the material composing the joint and the presence or absence of a cavity in the joint. The bones of fibrous joints are held together by fibrous connective tissue. There is no cavity, or space, present between the bones, so most fibrous joints do not move at all or are only capable of minor movements. The joints between the bones in the skull and between the teeth and the bone of their sockets are examples of fibrous joints.
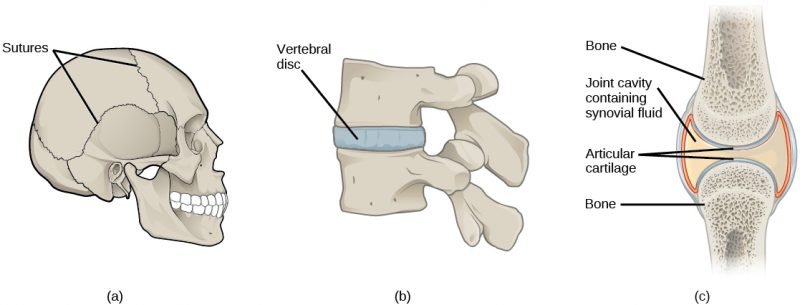
Cartilaginous joints are joints in which the bones are connected by cartilage. An example is found at the joints between vertebrae, the so-called “disks” of the backbone. Cartilaginous joints allow for very little movement. Synovial joints are the only joints that have a space between the adjoining bones. This space is referred to as the joint cavity and is filled with fluid. The fluid lubricates the joint, reducing friction between the bones and allowing for greater movement. The ends of the bones are covered with cartilage, and the entire joint is surrounded by a capsule. Synovial joints are capable of the greatest movement of the joint types. Knees, elbows, and shoulders are examples of synovial joints.
The wide range of movement allowed by synovial joints produces different types of movements. Angular movements are produced when the angle between the bones of a joint changes. Flexion, or bending, occurs when the angle between the bones decreases. Moving the forearm upward at the elbow is an example of flexion. Extension is the opposite of flexion in that the angle between the bones of a joint increase. Rotational movement is the movement of a bone as it rotates around its own longitudinal axis. Movement of the head as in saying “no” is an example of rotation.
Learn By Doing 10.4
Which type of joint provides the greatest range of motion?
- fibrous
- cartilaginous
- synovial
Structure of Bones
- Compare and contrast compact (cortical) bone with spongy (cancellous) bone.
- Differentiate between endosteum and periosteum.
- Describe the functions of red and yellow bone marrow.
Although bones vary greatly in size and shape, they all have certain structural similarities. Bones are organs. (Recall that organs are made up of two or more types of tissues.) The two main types of bone tissue are compact bone and spongy bone. Compact bone makes up the dense outer layer of bones. Spongy bone is lighter and less dense than compact bone and is found toward the center of the bone. Periosteum (from peri = around and osteo = bone) is the tough, shiny, white membrane that covers all surfaces of bones except the joint surfaces. Periosteum is composed of a layer of fibrous connective tissue and a layer of bone-forming cells. Bones consist of different types of tissue including compact bone, spongy bone, bone marrow, and periosteum. Compact bone makes up the dense outer layer of bones. Its functional unit is the osteon. Compact bone is very hard and strong. Spongy bone is found inside bones and is lighter and less dense than compact bone. This is because spongy bone is porous. Red bone marrow is a soft connective tissue that produces blood cells. It is found inside the pores of spongy bone. Periosteum is a tough fibrous membrane that covers and protects the outer surfaces of bones.
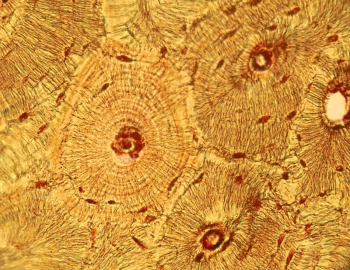
Compact Bone
Just below the periosteum is the hard layer of compact bone tissue. It is so-called due to its high density, and it accounts for about 80% of the total bone mass of an adult skeleton. Compact bone is extremely hard and is made up of many cylinder-shaped units called osteons. Osteons act like strong pillars within the bone to give the bone strength and allow it to bear the weight of the attached muscles and withstand the stresses of movement. Osteons are made up of rings of calcium salts and collagen fibers called bone matrix. Bone matrix is a mixture of calcium salts, such as calcium phosphate and calcium hydroxide, and collagen (a type of protein), which form hollow tubes that look similar to the rings on a tree. Each of these matrix tubes is a lamella, which means “thin plate” (plural: lamellae). The calcium salts form crystals that give bones great strength, but the crystals do not bend easily and tend to shatter if stressed. Collagen fibers are tough and flexible. All collagen fibers within a single lamella are lined up in the same direction, which gives each lamella great strength. Overall, the protein-calcium crystal combination in the matrix allows bones to bend and twist without breaking easily. The collagen fibers also act as a scaffold for the laying down of new calcium salts.
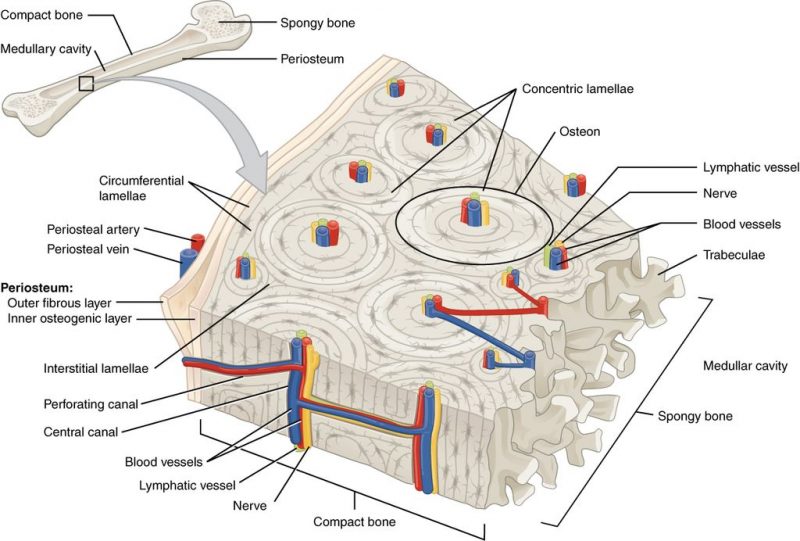
In the center of each osteon is a central canal. The canal serves as a passageway for blood vessels and nerves. Within each osteon, many mature bone cells called osteocytes are located. Osteocytes are found in little pockets called lacunae that are sandwiched between layers of bone matrix. You can see lamellae and osteocytes in their lacunae in the figure below. Osteocytes are responsible for monitoring the protein and mineral contents of the bone, and they direct both the release of calcium into the blood and the uptake up of calcium salts into the bone. Other bone cells, called osteoblasts, secrete the organic content of the matrix and are responsible for the growth of new bone. Osteoblasts are found near the surface of bones. Osteoclasts are bone cells that remove calcium salts from bone matrix. These bone cells will be discussed in further detail below.
 |
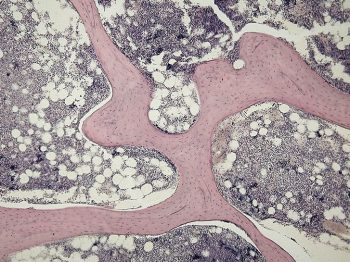 |
Spongy Bone
Whereas compact bone tissue forms the outer layer of all bones, spongy bone or cancellous bone forms the inner layer of all bones. While it is less dense than compact bone, the term “spongy” refers only to the appearance of the bone, as spongy bone is quite strong. The lamellae of spongy bone form an open, porous network of bony branches, or beams, called trabeculae, that give the bone strength and make the bone lighter. This also allows room for blood vessels and bone marrow. Spongy bone does not have osteons; instead, nutrients reach the osteocytes of spongy bone by diffusion through tiny openings in the surface of the spongy bone. Spongy bone makes up the bulk of the interior of most bones including the vertebrae.
Bone Marrow
Many bones also contain a soft connective tissue called bone marrow. There are two types of bone marrow. Red marrow produces red blood cells, platelets, and most of the white blood cells in the body. Yellow marrow produces some white blood cells but is primarily made of fat cells. Both types of bone marrow contain numerous blood vessels and capillaries. In newborns, bones contain only red marrow. As the child ages, red marrow is mostly replaced by yellow marrow. In adults, red marrow is mostly found in the flat bones of the skull, the ribs, the vertebrae, and the pelvic bones. It is also found between the spongy bone at the very top of the femur and the humerus.
Periosteum and Endosteum
The outer surfaces of bones—except where they make contact with other bones at joints—are covered by periosteum. Periosteum has a tough, external fibrous layer and an internal layer that contains osteoblasts (bone-building cells). The periosteum is richly supplied with blood, lymph, and pain receptors, which make it very sensitive to manipulation. Periosteum provides nourishment to the bone through a rich blood supply. The periosteum is connected to the bone by strong collagen fibers called Sharpey’s fibers, which extend into the outer circumferential lamellae of the compact bone.
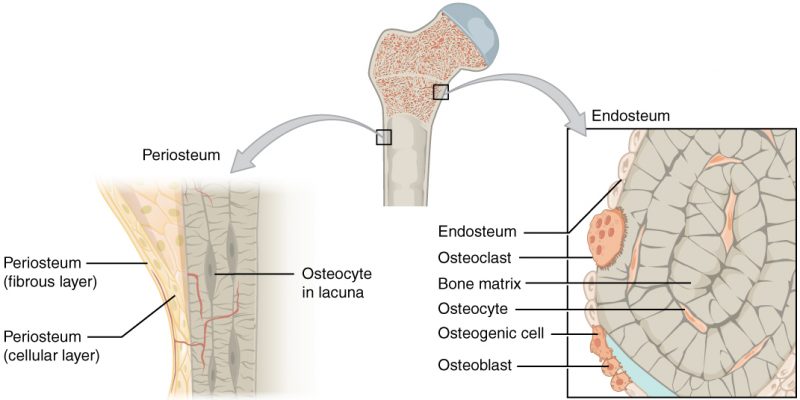
Endosteum is a thin vascular membrane that lines the medullary cavity of long bones and coats the trabeculae of spongy bone.
Learn By Doing 10.5
Why are most bones composed of both spongy and compact bone?
- Spongy bone adds weight; compact bone reduces brittleness.
- Spongy bone reduces weight and brittleness; compact bone adds stiffness.
- Spongy bone reduces weight; compact bone reduces brittleness.
- Spongy bone reduces brittleness; compact bone reduces weight and adds stiffness.
Which of the following statements about bone tissue is false?
- Compact bone tissue is made of cylindrical osteons that are aligned such that they travel the length of the bone.
- Central canals contain blood vessels only.
- Central canals contain blood vessels and nerve fibers.
- Spongy tissue is found on the interior of the bone, and compact bone tissue is found on the exterior.
If you wanted to maintain the strength of a bone but lower the chance it would break when bent, which of the following would you change?
Hints: Osteons make the bones stronger and more brittle, so they break more easily when bent. Trabeculae are found in spongy bone, and Osteons are found in compact bone.
- Decrease the amount of spongy bone
- Increase the amount of compact bone
- Increase the number of trabeculae; decrease the number of osteons
- Increase the number of osteons; decrease the number of trabeculae
The fibrous membrane covering the outer surface of the bone is the ________.
- periosteum
- epiphysis
- endosteum
- diaphysis
Which of the following are found in compact bone and spongy bone?
- osteons
- central canals
- lamellae
- lacunae
Which of the following is only found in spongy bone?
- canaliculi
- perforating canals
- trabeculae
- calcium salts
In what ways is the structural makeup of compact and spongy bone well suited to their respective functions?
Cell Types in Bone
Learning Objective
Bone, or osseous tissue, is a connective tissue that constitutes the endoskeleton. It contains specialized cells and a matrix of mineral salts and collagen fibers. The mineral salts primarily include hydroxyapatite, a mineral formed from calcium phosphate. Calcification is the process of deposition of mineral salts on the collagen fiber matrix. This crystallizes and hardens the tissue. The process of calcification only occurs in the presence of collagen fibers. Bone consists of four types of cells: osteoblasts, osteoclasts, osteocytes, and osteoprogenitor cells.
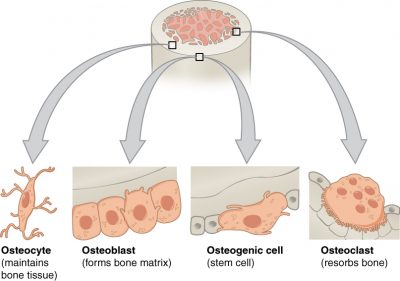
- Osteoprogenitor cells are pluripotent stem cells that divide to produce cells that differentiate into osteoblasts.
- Osteoblasts are bone-forming cells that are located on the inner and outer surfaces of bones. They make a collagen-rich protein mixture (called osteoid) that mineralizes to become solid bone matrix. Osteoblasts are immature bone cells. Osteoblasts that become trapped in the bone matrix differentiate into osteocytes.
- Osteocytes are the main cells in bony connective tissue; these cells cannot divide. These mature bone cells differentiate from osteoblasts that become trapped by mineralized bone matrix. The spaces that osteocytes occupy are called lacunae. Osteocytes are star-shaped and have many processes that reach out through narrow channels in the mineralized bone called canaliculi.
- Osteoclasts are the cells responsible for bone resorption. Located on bone surfaces, osteoclasts are large cells with as many as 50 nuclei! They secrete acids and hydrolytic enzymes that dissolve the bone matrix. The minerals are released into the blood, and so this process helps to regulate calcium concentrations in body fluids. Bone may also be resorbed if mechanical stresses on the bone change. This remodeling allows our bones to respond to changes in use.
Osteoclasts constantly remove minerals from the bone, and osteoblasts constantly produce the matrix that binds minerals into the bone, so both of these cells are important in calcium homeostasis.
| Cell type | Function | Location |
| Osteogenic cells | Develop into osteoblasts | Deep layers of the periosteum and the marrow |
| Osteoblasts | Bone deposition, secretion of organic parts of the matrix (collagen) | In growing portions of bone, including periosteum and endosteum, found near the surfaces of bones |
| Osteocytes | Monitor the protein and mineral contents of bones and direct both the release of calcium into the blood and the uptake of calcium salts into the bone | Entrapped in a matrix between lamellae |
| Osteoclasts | Bone resorption; Responsible for the breakdown of matrix and the release of calcium salts into the blood. | Bone surfaces and at sites of old, injured, or unneeded bone |
Learn By Doing 10.6
Think of the bones of your body as a rapidly expanding city. When the old buildings get outdated, they are either remodeled to make enhancements or knocked down to make room for the new ones. As soon as a building is knocked down, a new one is erected in its place. The construction crew recycles the old building materials. Many city planners constantly monitor the building’s progress and talk with one another about which sections of the city will get the available resources. For the questions below, choose which of the following types of bone cells fit best: osteoblasts, osteoclasts, and osteocytes.
- In the city expansion project analogy, which cells are the demolition crew?
- In the city expansion project analogy, which cells are the construction crew?
- In the city expansion project analogy, which cells are the city planners?
When would osteoblasts be activated?
- When the osteoclasts activate them.
- When the bone is exposed to regular stress.
- When the bone is immobilized for an extended time.
- When there is a lack of phosphorus in the body.
Changes in the Skeletal System: Ossification, Bone Growth, Remodeling, and Repair.
Learning Objectives
- Explain the function of cartilage in ossification.
- List the steps of intramembranous ossification.
- List the steps of endochondral ossification.
- Explain how activity at the epiphyseal plate leads to growth.
- Compare and contrast the processes of modeling and remodeling.
- Differentiate between ossification, growth, remodeling, and repair of bone.
Bone Formation
Bone is a replacement tissue; that is, it uses a model tissue on which to lay down its mineral matrix. For skeletal development, the most common template is cartilage. During fetal development, a framework is laid down that determines where bones will form. This framework is a flexible, semi-solid matrix produced by chondroblasts and consists of hyaluronic acid, chondroitin sulfate, collagen fibers, and water. As the matrix surrounds and isolates chondroblasts, they are called chondrocytes. Unlike most connective tissues, cartilage is avascular, meaning that it has no blood vessels supplying nutrients and removing metabolic wastes. All of these functions are carried on by diffusion through the matrix. This is why damaged cartilage does not repair itself as readily as most tissues do.
Throughout fetal development and into childhood growth and development, bone forms on the cartilaginous matrix. By the time a fetus is born, most of the cartilage has been replaced with bone. Some additional cartilage will be replaced throughout childhood, and some cartilage remains in the adult skeleton.
Ossification, or osteogenesis, is the process of bone formation by osteoblasts. Ossification is distinct from the process of calcification; whereas calcification takes place during the ossification of bones, it can also occur in other tissues. Ossification begins approximately six weeks after fertilization in an embryo. Before this time, the embryonic skeleton consists entirely of fibrous membranes and hyaline cartilage. The development of bone from fibrous membranes is called intramembranous ossification; development from hyaline cartilage is called endochondral ossification. Bone growth (often referred to as bone lengthening) continues until approximately age 25. Bones can grow in thickness throughout life, but after age 25, osteoblasts function primarily in bone remodeling and repair.
Intramembranous Ossification
Intramembranous ossification is the process of bone development from fibrous membranes. It is involved in the formation of the flat bones of the skull, the mandible, and the clavicles. Ossification begins as mesenchymal cells form a template of the future bone. They then differentiate into osteoblasts at the ossification center. Osteoblasts secrete the extracellular matrix and deposit calcium, which hardens the matrix. The non-mineralized portion of the bone or osteoid continues to form around blood vessels, forming spongy bone. Connective tissue in the matrix differentiates into red bone marrow in the fetus. The spongy bone is remodeled into a thin layer of compact bone on the surface of the spongy bone.
Endochondral Ossification
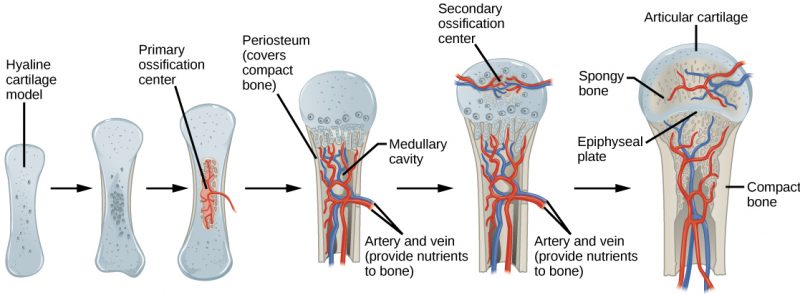
Endochondral ossification is the process of bone development from hyaline cartilage. All of the bones of the body, except for the flat bones of the skull, mandible, and clavicles, are formed through endochondral ossification. In long bones, chondrocytes form a template of hyaline cartilage that corresponds to the diaphysis. Responding to complex developmental signals, the matrix begins to calcify. This calcification prevents the diffusion of nutrients into the matrix, resulting in chondrocytes dying and the opening up of cavities in the diaphysis cartilage. Blood vessels invade the cavities, and osteoblasts and osteoclasts modify the calcified cartilage matrix into spongy bone. Osteoclasts then break down some of the spongy bone to create a medullary cavity in the center of the diaphysis. Dense, irregular connective tissue forms a sheath (periosteum) around the bones. The periosteum assists in attaching the bone to surrounding tissues, tendons, and ligaments. The bone continues to grow and elongate as the cartilage cells at the epiphyses divide. In the last stage of prenatal bone development, the centers of the epiphyses begin to calcify. Secondary ossification centers form in the epiphyses as blood vessels, and osteoblasts enter these areas and convert hyaline cartilage into spongy bone. Until adolescence, hyaline cartilage persists at the epiphyseal plate (growth plate), which is the region between the diaphysis and epiphysis that is responsible for the lengthwise growth of long bones.
Bone Growth
The skeletons of babies and children have many more bones and more cartilage than adults have. As a child grows, these “extra” bones, such as the bones of the skull (cranium) and the tailbone (sacrum), fuse together, and cartilage cells (chondrocytes) are gradually replaced by bone cells (osteocytes).
An infant is born with zones of cartilage called epiphyseal plates between segments of bone to allow further growth of the bone. When the child reaches skeletal maturity (between the ages of 18 and 25 years), all of the cartilage in the plate is replaced by bone, which stops further growth.
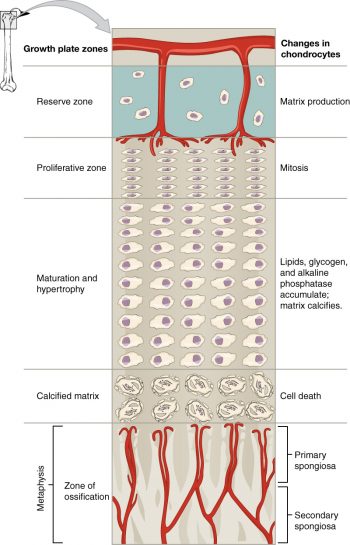
Bones grow in length at the epiphyseal plate by a process that is similar to endochondral ossification. The chondrocytes in the region of the epiphyseal plate reproduce by cell division and push older chondrocytes down toward the diaphysis. Eventually, these chondrocytes age and die. Osteoblasts move into this region and replace the chondrocytes with bone matrix. This process lengthens the bone and continues throughout childhood and the adolescent years until cartilage growth slows down and finally stops. When cartilage growth stops (usually in the early twenties), the epiphyseal plate completely ossifies so that only a thin epiphyseal line remains, and the bones can no longer grow in length. Bone growth is under the influence of growth hormone from the anterior pituitary gland and sex hormones from the ovaries and testes. Even though bones stop growing in length in early adulthood, they can continue to increase in thickness or diameter throughout life in response to stress from increased muscle activity or weight-bearing exercise.
Long bones continue to lengthen, potentially until adolescence, through the addition of bone tissue at the epiphyseal plate. They also increase in width through appositional growth.
Thickening of Long Bones
Appositional growth is the increase in the diameter of bones by the addition of bony tissue at the surface of bones. Osteoblasts at the bone surface secrete bone matrix, and osteoclasts on the inner surface break down bone. The osteoblasts differentiate into osteocytes. A balance between these two processes allows the bone to thicken without becoming too heavy.
Bone Remodeling
Bone renewal continues after birth into adulthood. Old bone tissue is replaced by new bone tissue. This process underlies the normal process of bone remodeling and healing of breakage. It involves the processes of bone deposition by osteoblasts and bone resorption by osteoclasts. Normal bone growth requires vitamins D, C, and A, plus minerals such as calcium, phosphorous, and magnesium. Hormones such as parathyroid hormone, growth hormone, and calcitonin are also required for proper bone growth and maintenance.
Bone turnover rates are quite high, with ten percent of the adult skeleton being replaced every year. Differences in turnover rate exist in different areas of the skeleton and in different areas of a bone. For example, the bone in the head of the femur may be fully replaced every six months, whereas the bone along the shaft is altered much more slowly.
Bone remodeling allows bones to adapt to stresses by becoming thicker and stronger when subjected to stress. Bones that are not subject to normal stress, for example when a limb is in a cast, will begin to lose mass.
Bone Repair
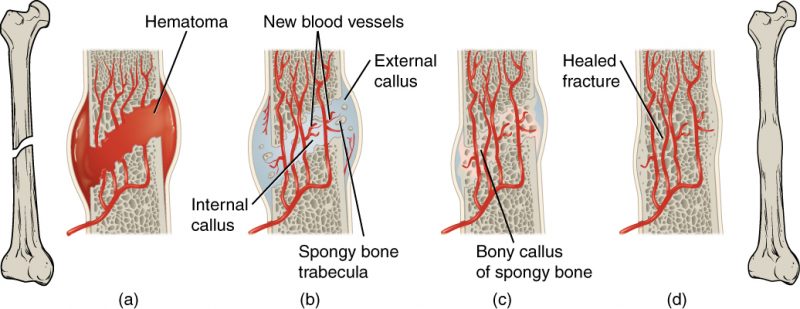
A fractured or broken bone undergoes repair in four stages:
- Blood vessels in the broken bone tear and hemorrhage, resulting in the formation of clotted blood, or a hematoma, at the site of the break. The severed blood vessels at the broken ends of the bone are sealed by the clotting process, and bone cells that are deprived of nutrients begin to die.
- Within days of the fracture, capillaries grow into the hematoma, and phagocytic cells begin to clear away the dead cells. Though fragments of the blood clot may remain, fibroblasts and osteoblasts enter the area and begin to reform bone. Fibroblasts produce collagen fibers that connect the broken bone ends, and osteoblasts start to form spongy bone. The repair tissue between the broken ends of two bones is called a fibrocartilaginous callus, as it is composed of both hyaline and fibrocartilage.
- The fibrocartilaginous callus is converted into a bony callus of spongy bone. It takes about two months for the broken bone ends to be firmly joined together after the fracture. This is similar to the endochondral formation of bone, as cartilage becomes ossified; osteoblasts, osteoclasts, and bone matrix are present.
- The bony callus is then remodeled by osteoclasts and osteoblasts, with excess material on the exterior of the bone and within the medullary cavity being removed. Compact bone is added to create bone tissue that is similar to the original, unbroken bone. This remodeling can take many months, and the bone may remain uneven for years.
Learn By Doing 10.7
Which of the following cells is not properly matched with its function in bone formation?
- Osteoblasts – become trapped in the matrix, where they differentiate into osteocytes.
- Chondroblasts- differentiate into chondrocytes.
- Osteocytes- secrete bone matrix.
Why is cartilage slow to heal?
- because it eventually develops into bone
- because it is semi-solid and flexible
- because it does not have a blood supply
- because endochondral ossification replaces all cartilage with bone
In endochondral ossification, what happens to the chondrocytes?
- They develop into osteocytes.
- They die in the calcified matrix that surrounds them, and this forms the medullary cavity.
- They grow and form the periosteum.
- They group together to form the primary ossification center.
Bones grow in length due to activity in the ________.
- epiphyseal plate
- perichondrium
- periosteum
- medullary cavity
Bone remodeling allows for the skeletal response to mechanical use and nutritional status. For each situation below decide if there would be a net overall resorption of bone or deposition of bone.
- A person’s arm is immobilized because of an elbow problem.
- An astronaut is in low gravity for an extended time.
Hint: Even when astronauts “work” their bodies, the lack of gravity provides little resistance to muscles and the bones they are connected to. - There is excess calcium in the blood.
Hint: Consider the feedback loop that regulates blood calcium levels. - Over-active osteoblasts
Hint: Consider the role of osteoblasts in bone remodeling. - Along the margins of a bone fracture
Hint: In order for a fracture to heal properly, what would have to happen to the bone?
Bone and Homeostasis
Learning Objectives
- List the nutrients that affect bone health
- Discuss the role that nutrients play in bone health
- Describe the effects of hormones on bone tissue
All of the organ systems of your body are interdependent, and the skeletal system is no exception. The food you take in via your digestive system and the hormones secreted by your endocrine system affect your bones. Even using your muscles to engage in exercise has an impact on your bones.
Exercise and Bone Tissue
During long space missions, astronauts can lose approximately 1 to 2 percent of their bone mass per month. This loss of bone mass is thought to be caused by the lack of mechanical stress on astronauts’ bones due to the low gravitational forces in space. Lack of mechanical stress causes bones to lose mineral salts and collagen fibers, and thus strength. Similarly, mechanical stress stimulates the deposition of mineral salts and collagen fibers. The internal and external structure of a bone will change as stress increases or decreases so that the bone is an ideal size and weight for the amount of activity it endures. That is why people who exercise regularly have thicker bones than people who are more sedentary. It is also why a broken bone in a cast atrophies while its contralateral mate maintains its concentration of mineral salts and collagen fibers. The bones undergo remodeling as a result of forces (or lack of forces) placed on them.
Numerous controlled studies have demonstrated that people who exercise regularly have greater bone density than those who are more sedentary. Any exercise will stimulate the deposition of more bone tissue, but resistance training has a greater effect than cardiovascular activities. Resistance training is especially important to slow down the eventual bone loss due to aging and for preventing osteoporosis.
Nutrition and Bone Tissue
The vitamins and minerals contained in all of the food we consume are important for all of our organ systems. However, there are certain nutrients that affect bone health.
You already know that calcium is a critical component of bone, especially in the form of calcium phosphate and calcium carbonate. Since the body cannot make calcium, it must be obtained from the diet. However, calcium cannot be absorbed from the small intestine without vitamin D which is a fat-soluble vitamin. Therefore, intake of vitamin D is also critical to bone health. In addition to vitamin D’s role in calcium absorption, it also plays a role, though not as clearly understood, in bone remodeling.
Milk and other dairy foods are not the only sources of calcium. This important nutrient is also found in green leafy vegetables, broccoli, intact salmon, and canned sardines with their soft bones. Nuts, beans, seeds, and shellfish provide calcium in smaller quantities.
Except for fatty fish like salmon and tuna, or fortified milk or cereal, vitamin D is not found naturally in many foods. The action of sunlight on the skin triggers the body to produce its own vitamin D, but many people, especially those of darker complexion and those living in northern latitudes where the sun’s rays are not as strong, are deficient in vitamin D. In cases of deficiency, a doctor can prescribe a vitamin D supplement.
Hormones and Bone Tissue
The endocrine system produces and secretes hormones, many of which interact with the skeletal system. These hormones are involved in controlling bone growth, maintaining bone once it is formed, and remodeling it.
Several hormones are necessary for controlling bone growth and maintaining the bone matrix. The pituitary gland secretes growth hormone (GH), which, as its name implies, controls bone growth in several ways. It triggers chondrocyte proliferation in epiphyseal plates, resulting in the increasing length of long bones. GH also increases calcium retention, which enhances mineralization, and stimulates osteoblastic activity, which improves bone density.
GH is not alone in stimulating bone growth and maintaining osseous tissue. Thyroxine, a hormone secreted by the thyroid gland promotes osteoblastic activity and the synthesis of bone matrix. During puberty, the sex hormones (estrogen in girls and testosterone in boys) also come into play. They too promote osteoblastic activity and production of bone matrix, and in addition, are responsible for the growth spurt that often occurs during adolescence. They also promote the conversion of the epiphyseal plate to the epiphyseal line (i.e., cartilage to its bony remnant), thus bringing an end to the longitudinal growth of bones. Additionally, the kidney converts Vitamin D into calcitriol, its active form. Calcitriol stimulates the absorption of calcium and phosphate from the digestive tract.
Bone modeling and remodeling require osteoclasts to resorb unneeded, damaged, or old bone and osteoblasts to lay down new bone. Two hormones that affect osteoclasts are parathyroid hormone (PTH) and calcitonin. PTH stimulates osteoclast proliferation and activity. As a result, calcium is released from the bones into circulation, thus increasing the calcium ion concentration in the blood. PTH also promotes the reabsorption of calcium by the kidney tubules, which can affect calcium homeostasis (see below).
Remodeling, or bone turnover, is the process of resorption of minerals followed by replacement by bone matrix, which causes little overall change in the shape of the bone. This process occurs throughout a person’s life. Osteoblasts and osteoclasts communicate with each other for this purpose. The purpose of remodeling is to regulate the level of calcium in the blood, repair micro-damaged bones (from everyday stress), and shape the skeleton during skeletal growth.
The process of bone resorption by the osteoclasts releases stored calcium into circulation and is an important process in regulating blood calcium balance. As bone deposition actively fixes circulating calcium in its mineral form by removing it from the bloodstream, resorption actively unfixes it, thereby increasing circulating calcium levels. These processes occur in tandem at site-specific locations.
When blood calcium levels decrease below normal, calcium is released from the bones so that there will be an adequate supply for blood clotting, muscle contraction, and nervous system function. When blood calcium levels are increased, the excess calcium is stored in the bone matrix. The dynamic process of releasing and storing calcium goes on almost continuously.
The small intestine is also affected by PTH, albeit indirectly. Because another function of PTH is to stimulate the synthesis of vitamin D, and because vitamin D promotes intestinal absorption of calcium, PTH indirectly increases calcium uptake by the small intestine. Calcitonin, a hormone secreted by the thyroid gland, has some effects that counteract those of PTH. Calcitonin inhibits osteoclast activity and stimulates calcium uptake by the bones, thus reducing the concentration of calcium ions in the blood. As evidenced by their opposing functions in maintaining calcium homeostasis, PTH and calcitonin are generally not secreted at the same time. The table below summarizes the hormones that influence the skeletal system.
| Hormone | Role |
| Growth hormone | Increases the length of long bones; enhances mineralization; and improves bone density |
| Thyroxine | Stimulates bone growth and promotes the synthesis of bone matrix |
| Sex hormones | Promote osteoblastic activity and production of bone matrix; responsible for adolescent growth spurt; promote the conversion of the epiphyseal plate to the epiphyseal line |
| Calcitriol | Stimulates the absorption of calcium and phosphate from the digestive tract |
| Parathyroid hormone | Stimulates osteoclast proliferation and resorption of bone by osteoclasts; promotes reabsorption of calcium by kidney tubules; indirectly increases calcium absorption by the small intestine |
| Calcitonin | Inhibits osteoclast activity and stimulates calcium uptake by bones |
Learn By Doing 10.8
Bones affected by osteoporosis lose bone mass and mineral content. Which of the following could result in the same loss of bone mass and mineral content?
- Overactive osteoclasts result in excess deposition.
- Overactive osteoclasts result in excess resorption
- Overactive osteoblasts result in excess resorption
Calcium cannot be absorbed from the small intestine if ________ is lacking.
- vitamin D
- vitamin K
- calcitonin
- fluoride
With respect to their direct effects on osseous tissue, which pair of hormones has actions that oppose each other?
- estrogen and testosterone
- calcitonin and calcitriol
- estrogen and progesterone
- calcitonin and parathyroid hormone
There is a regular exchange of calcium between blood and bone which is part of a negative feedback loop. Answer the following questions about this particular feedback loop.
What is the variable that is being regulated?
- amount of parathyroid hormone
- levels of calcium in the blood
- parathyroid gland
- levels of calcium in the bone
What is the receptor?
- levels of calcium in the blood
- parathyroid gland
- osteoclasts and osteoblasts
- all of the above
What is the control center?
- osteoclasts
- blood levels of calcium
- parathyroid gland
- bone
What is the effector?
- altered levels of parathyroid hormone
- altered osteoclast function
- bone
- parathyroid gland
If a tumor develops in a parathyroid gland, it can cause the gland to continuously release high levels of parathyroid hormone (called hyperparathyroidism). What impact, if any, would you expect hyperparathyroidism to have on the skeletal system?
- altered articulations
- very strong bones
- no change
- weak bones
“Learn By Doing” and “Did I Get This?” Feedback
Learn By Doing 10.1
Bone tissue can be described as ________.
- dead calcified tissue
- cartilage
- the skeletal system
- dense, hard connective tissue
Which function of the skeletal system would be especially important if you were in a car accident?
- storage of minerals
- protection of internal organs
- facilitation of movement
- fat storage
Without red marrow, bones would not be able to ________.
- store phosphate
- store calcium
- make blood cells
- move like levers
Yellow marrow has been identified as ________.
- an area of fat storage
- a point of attachment for muscles
- the hard portion of bone
- the cause of kyphosis
Which of the following can be found in areas of movement?
- hematopoiesis
- cartilage
- yellow marrow
- red marrow
The skeletal system is made of ________.
- muscles and tendons
- bones and cartilage
- vitreous humor
- minerals and fat
Learn By Doing 10.2
The appendicular skeleton is associated with which function?
- protection of the internal organs
- interaction with the environment
- organizing the structural center of the body
- all of the above are correct
Hint: The appendicular skeleton contains the bones of the arms and legs, and it does not contain major bones along the axis of the body.
Select the name of the bone that is being described from the following: ribs, mandible, sternum, cranium, vertebrae
- The cranium supports facial structures and encloses and protects the brain.
- The ribs provide protection for the organs of the upper body.
- The vertebrae permit mechanical stability for the body and protect the spinal cord.
- The sternum provides attachment for many (not all) ribs.
- The mandible permits chewing.
Which of the following attaches to the vertebral column and the lower limbs?
- Sternal girdle
- Patella girdle
- Pectoral girdle
- Pelvic girdle
Indicate whether each of the following represents a bone in the axial or appendicular skeleton or indicate that it is not a bone at all.
- Mandible axial
- Tibula not a bone
- Hyoid axial
- Clavicle appendicular
- Sternum axial
- Radius appendicular
- Ulna appendicular
- Hydro not a bone
- Vertebrae axial
- Scapula appendicular
- Patella appendicular
- Fibia appendicular
Learn By Doing 10.3
Most of the bones of the arms and hands are _______ bones.
- flat bones
- short bones
- sesamoid bones
- irregular bones
- long bones
Which of the following occurs in the spongy bone of the epiphysis?
- bone growth
- bone remodeling
- hematopoiesis
- shock absorption
The diaphysis contains ________.
- the metaphysis
- fat stores
- spongy bone
- compact bone
If the articular cartilage at the end of one of your long bones were to degenerate, what symptoms do you think you would experience? Why?
Our answer: If the articular cartilage at the end of one of your long bones were to deteriorate, which is actually what happens in osteoarthritis, you would experience joint pain at the end of that bone and limitation of motion at that joint because there would be no cartilage to reduce friction between adjacent bones and there would be no cartilage to act as a shock absorber.
Learn By Doing 10.4
Which type of joint provides the greatest range of motion?
- fibrous
- cartilaginous
- synovial
Learn By Doing 10.5
Why are most bones composed of both spongy and compact bone?
- Spongy bone adds weight; compact bone reduces brittleness.
- Spongy bone reduces weight and brittleness; compact bone adds stiffness.
- Spongy bone reduces weight; compact bone reduces brittleness.
- Spongy bone reduces brittleness; compact bone reduces weight and adds stiffness.
Which of the following statements about bone tissue is false?
- Compact bone tissue is made of cylindrical osteons that are aligned such that they travel the length of the bone.
- Central canals contain blood vessels only.
- Central canals contain blood vessels and nerve fibers.
- Spongy tissue is found on the interior of the bone, and compact bone tissue is found on the exterior.
If you wanted to maintain the strength of a bone but lower the chance it would break when bent, which of the following would you change?
Hints: Osteons make the bones stronger and more brittle, so they break more easily when bent. Trabeculae are found in spongy bone, and osteons are found in compact bone.
- Decrease the amount of spongy bone
- Increase the amount of compact bone
- Increase the number of trabeculae; decrease the number of osteons
- Increase the number of osteons; decrease the number of trabeculae
The fibrous membrane covering the outer surface of the bone is the ________.
- periosteum
- epiphysis
- endosteum
- diaphysis
Which of the following are found in compact bone and spongy bone?
- osteons
- central canals
- lamellae
- lacunae
Which of the following is only found in spongy bone?
- canaliculi
- perforating canals
- trabeculae
- calcium salts
In what ways is the structural makeup of compact and spongy bone well suited to their respective functions?
Learn By Doing 10.6
Think of the bones of your body as a rapidly expanding city. When the old buildings get outdated, they are either remodeled to make enhancements or knocked down to make room for the new ones. As soon as a building is knocked down, a new one is erected in its place. The construction crew recycles the old building materials. Many city planners constantly monitor the building’s progress and talk with one another about which sections of the city will get the available resources. For the questions below, choose which of the following types of bone cells fit best: osteoblasts, osteoclasts, and osteocytes.
- In the city expansion project analogy, which cells are the demolition crew? osteoclasts
- In the city expansion project analogy, which cells are the construction crew? osteoblasts
- In the city expansion project analogy, which cells are the city planners? osteocytes
When would osteoblasts be activated?
- When the osteoclasts activate them.
- When the bone is exposed to regular stress.
- When the bone is immobilized for an extended time.
- When there is a lack of phosphorus in the body.
Learn By Doing 10.7
Which of the following cells is not properly matched with its function in bone formation?
- Osteoblasts – become trapped in the matrix, where they differentiate into osteocytes.
- Chondroblasts- differentiate into chondrocytes.
- Osteocytes- secrete bone matrix.
Why is cartilage slow to heal?
- because it eventually develops into bone
- because it is semi-solid and flexible
- because it does not have a blood supply
- because endochondral ossification replaces all cartilage with bone
In endochondral ossification, what happens to the chondrocytes?
- They develop into osteocytes.
- They die in the calcified matrix that surrounds them, and this forms the medullary cavity.
- They grow and form the periosteum.
- They group together to form the primary ossification center.
Bones grow in length due to activity in the ________.
- epiphyseal plate
- perichondrium
- periosteum
- medullary cavity
Bone remodeling allows for the skeletal response to mechanical use and nutritional status. For each situation below decide if there would be a net overall resorption of bone or deposition of bone.
- A person’s arm is immobilized because of an elbow problem. resorption
- An astronaut is in low gravity for an extended time. resorption
Hint: Even when astronauts “work” their bodies, the lack of gravity provides little resistance to muscles and the bones they are connected to. - There is excess calcium in the blood. deposition
Hint: Consider the feedback loop that regulates blood calcium levels. - Over-active osteoblasts deposition
Hint: Consider the role of osteoblasts in bone remodeling. - Along the margins of a bone fracture deposition
Hint: In order for a fracture to heal properly, what would have to happen to the bone?
Learn By Doing 10.8
Bones affected by osteoporosis lose bone mass and mineral content. Which of the following could result in the same loss of bone mass and mineral content?
- Overactive osteoclasts result in excess deposition.
- Overactive osteoclasts result in excess resorption
- Overactive osteoblasts result in excess resorption
Calcium cannot be absorbed from the small intestine if ________ is lacking.
- vitamin D
- vitamin K
- calcitonin
- fluoride
With respect to their direct effects on osseous tissue, which pair of hormones has actions that oppose each other?
- estrogen and testosterone
- calcitonin and calcitriol
- estrogen and progesterone
- calcitonin and parathyroid hormone
There is a regular exchange of calcium between blood and bone which is part of a negative feedback loop. Answer the following questions about this particular feedback loop.
What is the variable that is being regulated?
- amount of parathyroid hormone
- levels of calcium in the blood
- parathyroid gland
- levels of calcium in the bone
What is the receptor?
- levels of calcium in the blood
- parathyroid gland
- osteoclasts and osteoblasts
- all of the above
What is the control center?
- osteoclasts
- blood levels of calcium
- parathyroid gland
- bone
What is the effector?
- altered levels of parathyroid hormone
- altered osteoclast function
- bone
- parathyroid gland
If a tumor develops in a parathyroid gland, it can cause the gland to continuously release high levels of parathyroid hormone (called hyperparathyroidism). What impact, if any, would you expect hyperparathyroidism to have on the skeletal system?
- altered articulations
- very strong bones
- no change
- weak bones
