Control and Regulation 2
19 Reproductive Systems
Sexual Reproduction and Sex Determination
Learning Objectives
- Define sexual reproduction.
- Describe how sex is determined in humans.
Animal reproduction is necessary for the survival of a species. In the animal kingdom, there are innumerable ways that species reproduce. Asexual reproduction produces genetically identical organisms (clones), whereas, in sexual reproduction, the genetic material of two individuals combines to produce offspring that are genetically different from their parents. During sexual reproduction, the male gamete (sperm) may be placed inside the female’s body for internal fertilization, or the sperm and eggs may combine outside the body in external fertilization. In humans, sexual reproduction is the combination of haploid reproductive cells from two individuals to form a third individual that is diploid and a genetically unique offspring.
Sexual reproduction produces offspring with novel combinations of genes. This can be an adaptive advantage in unstable or unpredictable environments. Species that reproduce sexually must maintain two different types of individuals, males and females, which can limit the ability to colonize new habitats as both sexes must be present. As humans, we are used to thinking of animals as having two separate sexes—male and female—determined at conception.
Mammalian sex determination is determined genetically by the presence of X and Y chromosomes. In general, individuals homozygous for X (XX) are female and heterozygous individuals (XY) are male. The presence of a specific gene on the Y chromosome begins the development of male characteristics and its absence results in female characteristics.
Human Reproductive Anatomy
Learning Objective
As animals became more complex, specific organs and organ systems evolved to support specific functions for the organism. The reproductive structures that evolved in land animals allow males and females to mate, fertilize internally, and support the growth and development of offspring.
The reproductive tissues of male and female humans develop similarly in utero until a low level of the hormone testosterone is released from male gonads. Testosterone causes undeveloped tissues to differentiate into male sexual organs. When testosterone is absent, the tissues develop into female sexual tissues. Primitive gonads become testes or ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female; that is, they are homologous structures.
Adult Male Reproductive Anatomy
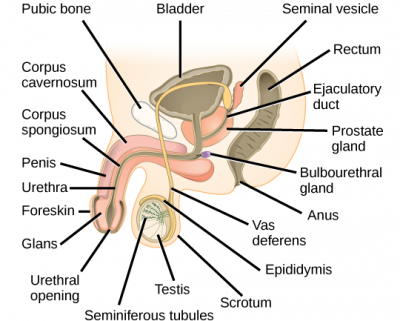
The penis is an organ that drains urine from the renal bladder and functions as a copulatory organ during intercourse. The penis contains three tubes of erectile tissue running through the length of the organ. These consist of a pair of tubes on the dorsal side called the corpus cavernosum, and a single tube of tissue on the ventral side called the corpus spongiosum. This tissue becomes engorged with blood, becoming erect and hard in preparation for intercourse. The organ is inserted into the vagina culminating with ejaculation. During intercourse, the smooth muscle sphincters at the opening of the renal bladder close to prevent urine from entering the penis.
An orgasm is a two-stage process: first, glands and accessory organs connected to the testes contract, then semen (containing sperm) is expelled through the urethra during ejaculation. After intercourse, the blood drains from the erectile tissue, and the penis becomes flaccid.
In the male reproductive system, the scrotum houses the testicles or testes (singular: testis), including providing passage for blood vessels, nerves, and muscles related to testicular function. The testes are a pair of male reproductive organs that produce sperm and some reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 in) in size and divided into wedge-shaped lobules by connective tissue called septa. Coiled in each wedge are seminiferous tubules that produce sperm.
Sperm are immobile at body temperature; therefore, the scrotum and penis are external to the body so that a proper temperature is maintained for motility. In land mammals, the pair of testes must be suspended outside the body at about 2° C lower than body temperature to produce viable sperm. Infertility can occur in land mammals when the testes do not descend through the abdominal cavity during fetal development.
Sperm are born in seminiferous tubules that are coiled inside the testes. The walls of the seminiferous tubules are made up of the developing sperm cells, with the least developed sperm at the periphery of the tubule and the fully developed sperm in the lumen. The sperm cells are mixed with “nursemaid” cells called Sertoli cells which protect the germ cells and promote their development. Other cells mixed in the wall of the tubules are the interstitial cells of Leydig. These cells produce high levels of testosterone once the male reaches adolescence.
When the sperm have developed flagella and are nearly mature, they leave the testicles and enter the epididymis. This structure resembles a comma and lies along the top and posterior portion of the testes; it is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens (or ductus deferens). The vas deferens loops up behind the bladder and forms the ejaculatory duct as it combines with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm from being passed out of the body during ejaculation and thus preventing fertilization.
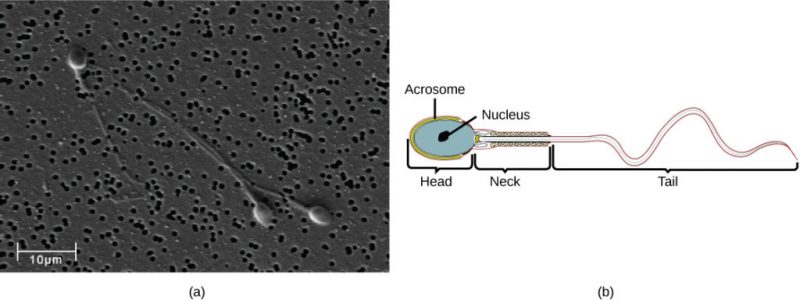
Semen is a mixture of sperm and fluids from accessory glands that contribute most of the semen’s volume. Sperm are haploid cells consisting of a flagellum as a tail, a midpiece or neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material. An acrosome is found at the top of the head of the sperm. This structure contains lysosomal enzymes that can digest the protective coverings that surround the egg. This helps the sperm penetrate and fertilize the egg. An ejaculate will contain from two to five milliliters of fluid with from 50–120 million sperm per milliliter.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles, the prostate gland, and the bulbourethral gland. The seminal vesicles are a pair of glands that lie along the posterior border of the urinary bladder. The glands make a solution that is thick, yellowish, and alkaline. As sperm are only motile in an alkaline environment, a basic pH is important to reverse the acidity of the vaginal environment. The solution also contains mucus, fructose (a sperm mitochondrial nutrient), a coagulating enzyme, ascorbic acid, and local-acting hormones called prostaglandins. The seminal vesicle glands account for 60 percent of the bulk of semen.
The walnut-shaped prostate gland surrounds the urethra, the connection to the urinary bladder. It has a series of short ducts that directly connect to the urethra. The gland is a mixture of smooth muscle and glandular tissue. The muscle provides much of the force needed for ejaculation to occur. The glandular tissue makes a thin, milky fluid that contains citrate (a nutrient), enzymes, and prostate-specific antigen (PSA). PSA is a proteolytic enzyme that helps to liquefy the ejaculate several minutes after release from the male. Prostate gland secretions account for about 30 percent of the bulk of semen.
The bulbourethral gland, or Cowper’s gland, releases its secretion prior to the release of the bulk of the semen. It neutralizes any acid residue in the urethra left over from urine. This usually accounts for a couple of drops of fluid in the total ejaculate and may contain a few sperm. Withdrawal of the penis from the vagina before ejaculation to prevent pregnancy may not work if sperm are present in the bulbourethral gland secretions. The location and functions of the male reproductive organs are summarized in Table 19.1.
| Organ | Location | Function |
| Scrotum | External | Carry and support testes |
| Penis | External | Deliver urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contribute to semen production |
| Bulbourethral Glands | Internal | Clean urethra at ejaculation |
Adult Female Reproductive Anatomy
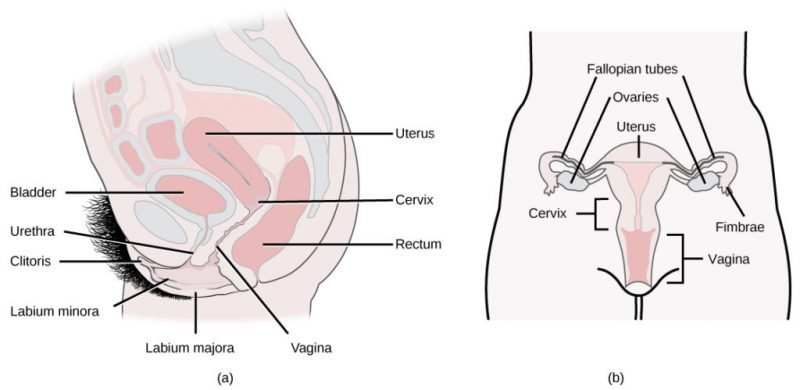
A number of reproductive structures are exterior to the female’s body. These include the breasts and the vulva. The vulva consists of the mons pubis, glans clitoris, labia majora, labia minora, and vestibular glands. The location and functions of the female reproductive organs are summarized in Table 19.2. The vulva is an area associated with the vestibule, which includes the structures found in the inguinal (groin) area of women. The mons pubis is a round, fatty area that overlies the pubic symphysis. The glans clitoris is a structure with erectile tissue that contains a large number of sensory nerves and serves as a source of stimulation during intercourse. The labia majora are a pair of elongated folds of tissue that run posteriorly from the mons pubis and enclose the other components of the vulva. The labia majora derive from the same tissue that produces the scrotum in a male. The labia minora are thin folds of tissue centrally located within the labia majora. These labia protect the openings to the vagina and urethra. The mons pubis and the anterior portion of the labia majora become covered with hair during adolescence; the labia minora is hairless. The greater vestibular glands are found at the sides of the vaginal opening and provide lubrication during intercourse.
| Organ | Location | Function |
| Clitoris | External | Sensory organ |
| Mons pubis | External | Fatty area overlying pubic bone |
| Labia majora | External | Covers labia minora |
| Labia minora | External | Covers vestibule |
| Greater vestibular glands | External | Secrete mucus; lubricate the vagina |
| Breast | External | Produce and deliver milk |
| Ovaries | Internal | Carry and develop eggs |
| Oviducts (Fallopian tubes) | Internal | Transport the egg to the uterus |
| Uterus | Internal | Support developing embryo |
| Vagina | Internal | Common tube for intercourse, birth canal, passing menstrual flow |
The breasts consist of mammary glands and adipose tissue. The size of the breast is determined by the amount of fat deposited behind the gland. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
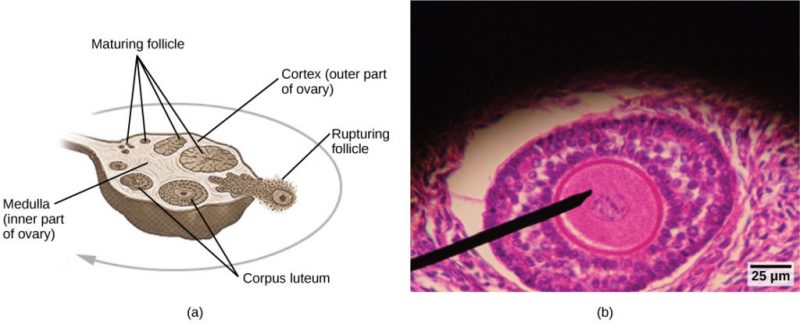
Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina. The pair of ovaries is held in place in the abdominal cavity by a system of ligaments. Ovaries consist of a medulla and cortex: the medulla contains nerves and blood vessels to supply the cortex with nutrients and remove waste. The outer layers of cells of the cortex are the functional parts of the ovaries. The cortex is made up of follicular cells that surround eggs that develop during fetal development in utero. During the beginning of the ovarian cycle, a batch of follicular cells develops and prepares an egg for release. At ovulation, one follicle ruptures, and one egg is released.
The oviducts, or fallopian tubes, extend from the superior uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbriae. When an egg is released at ovulation, the fimbriae help the non-motile egg enter into the tube and passage to the uterus. The walls of the oviducts are ciliated and are made up mostly of smooth muscle. The cilia beat toward the middle, and the smooth muscle contracts in the same direction, moving the egg toward the uterus. Fertilization usually takes place within the oviducts, and the developing embryo is moved toward the uterus for development. It usually takes the egg or embryo a week to travel through the oviduct. Sterilization in women is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed.
The uterus is a structure about the size of a woman’s fist. This is lined with an endometrium rich in blood vessels and mucus glands. The uterus supports the developing embryo and fetus during gestation. The thickest portion of the wall of the uterus is made of smooth muscle, a layer called the myometrium. Contractions of the smooth muscle in the uterus aid in passing the baby through the vagina during labor. A portion of the lining of the uterus sloughs off during each menstrual period and then builds up again in preparation for implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina. The cervix functions as the birth canal.
The vagina is a muscular tube that serves several purposes. It allows the menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the vessel for the delivery of offspring. It is lined by stratified squamous epithelial cells to protect the underlying tissue.
Sexual Response
Learning Objective
The sexual response in humans is both psychological and physiological. Both sexes experience sexual arousal through psychological and physical stimulation. There are four phases of the sexual response. During phase one, called excitement, vasodilation leads to vasocongestion in erectile tissues in both men and women. The nipples, clitoris, labia, and penis engorge with blood and become enlarged. Vaginal secretions are released to lubricate the vagina to facilitate intercourse. During the second phase, called the plateau, stimulation continues, the outer third of the vaginal wall enlarges with blood, and breathing and heart rate increase.
During phase three or orgasm, rhythmic, involuntary contractions of muscles occur in both sexes. In the male, the reproductive accessory glands and tubules constrict placing semen in the urethra, then the urethra contracts expelling the semen through the penis. In women, the uterus and vaginal muscles contract in waves that may last slightly less than a second each. During phase four or resolution, the processes described in the first three phases reverse themselves and return to their normal state. Men experience a refractory period in which they cannot maintain an erection or ejaculate for a period of time ranging from minutes to hours.
Gametogenesis
Learning Objective
Gametogenesis, the production of sperm and eggs, takes place through the process of meiosis. During meiosis, two cell divisions separate the paired chromosomes in the nucleus and then separate the chromatids that were made during an earlier stage of the cell’s life cycle. Meiosis produces haploid cells with half of each pair of chromosomes normally found in diploid cells. The production of sperm is called spermatogenesis, and the production of eggs is called oogenesis.
Spermatogenesis occurs in the wall of the seminiferous tubules, with stem cells at the periphery of the tube and spermatozoa at the lumen of the tube. Immediately under the capsule of the tubule are diploid, undifferentiated cells. These stem cells, called spermatogonia (singular: spermatagonium), go through mitosis with one offspring going on to differentiate into a sperm cell and the other giving rise to the next generation of sperm.
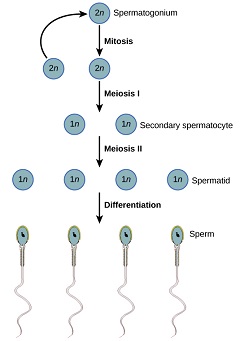
Meiosis starts with a cell called a primary spermatocyte. At the end of the first meiotic division, a haploid cell is produced called a secondary spermatocyte. This cell is haploid and must go through another meiotic cell division. The cell produced at the end of meiosis is called a spermatid, and when it reaches the lumen of the tubule and grows a flagellum, it is called a sperm cell. Four sperm result from each primary spermatocyte that goes through meiosis.
Stem cells are deposited during gestation and are present at birth through the beginning of adolescence but in an inactive state. During adolescence, gonadotropic hormones from the anterior pituitary cause the activation of these cells and the production of viable sperm. This continues into old age.
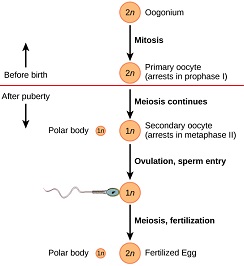
Oogenesis occurs in the outermost layers of the ovaries. As with sperm production, oogenesis starts with a germ cell called an oogonium (plural: oogonia), but this cell undergoes mitosis to increase in number, eventually resulting in up to about one to two million cells in the female embryo.
The cell starting meiosis is called a primary oocyte. This cell will start the first meiotic division and be arrested in its progress. At the time of birth, all future eggs are in the prophase stage. In adolescence, anterior pituitary hormones cause the development of a number of follicles in an ovary. This results in the primary oocyte finishing the first meiotic division. The cell divides unequally, with most of the cellular material and organelles going to one cell, called a secondary oocyte, and only one set of chromosomes and a small amount of cytoplasm going to the other cell. This second cell is called a polar body and usually dies. Meiosis stops again until and unless fertilization occurs. At ovulation, this secondary oocyte will be released and travel toward the uterus through the oviduct. If the secondary oocyte is fertilized, the cell continues through meiosis II, producing a second polar body and a fertilized egg containing all 46 chromosomes of a human being, half of them coming from the sperm.
Egg production begins before birth, is arrested during meiosis until puberty, and then individual cells continue through each menstrual cycle. One egg is produced from each meiotic process, with the extra chromosomes going into polar bodies that degenerate and are reabsorbed by the body.
Hormonal Control of Human Reproduction
Learning Objectives
- Describe the roles of male and female reproductive hormones.
- Discuss the interplay of the ovarian and menstrual cycles and how both end at menopause.
The human male and female reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. In both sexes, the hypothalamus monitors and causes the release of hormones from the pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. (Note that the body must reach puberty in order for the adrenals to release the hormones that must be present for GnRH to be produced.) Although FSH and LH are named after their functions in female reproduction, they are produced in both sexes and play important roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
Male Reproduction
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells to begin facilitating spermatogenesis using negative feedback. LH also enters the testes and stimulates the interstitial cells of Leydig to make and release testosterone into the testes and the blood.
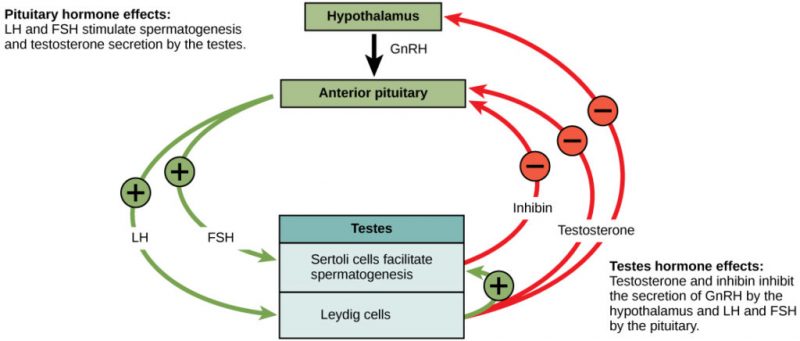
Testosterone, the hormone responsible for the secondary sexual characteristics that develop in the male during adolescence, stimulates spermatogenesis. These secondary sex characteristics include a deepening of the voice, the growth of facial, axillary, and pubic hair, and the beginnings of the sex drive.
A negative feedback system occurs in the male with rising levels of testosterone acting on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH. The Sertoli cells produce the hormone inhibin, which is released into the blood when the sperm count is too high. This inhibits the release of GnRH and FSH, which will cause spermatogenesis to slow down. If the sperm count reaches 20 million/ml, the Sertoli cells cease the release of inhibin, and the sperm count increases.
Female Reproduction
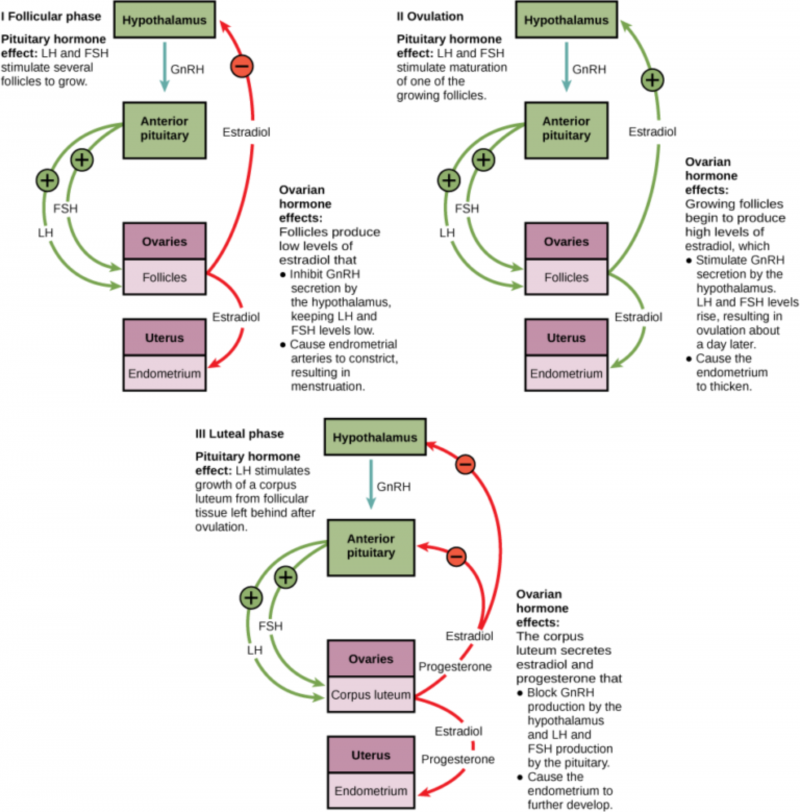
The control of reproduction in females is more complex. As with the male, the anterior pituitary hormones cause the release of the hormones FSH and LH. In addition, estrogens and progesterone are released from the developing follicles. Estrogen is the reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption; it is also responsible for the secondary sexual characteristics of females. These include breast development, flaring of the hips, and a shorter period necessary for bone maturation. Progesterone assists in endometrial re-growth and inhibition of FSH and LH release.
In females, FSH stimulates the development of egg cells, called ova, which develop in structures called follicles. Follicle cells produce the hormone inhibin, which inhibits FSH production. LH also plays a role in the development of ova, induction of ovulation, and stimulation of estradiol and progesterone production by the ovaries. Estradiol and progesterone are steroid hormones that prepare the body for pregnancy. Estradiol produces secondary sex characteristics in females, while both estradiol and progesterone regulate the menstrual cycle.
The Ovarian Cycle and Uterine Cycle
The ovarian cycle governs the preparation of endocrine tissues and the release of eggs, while the uterine cycle governs the preparation and maintenance of the uterine lining. These cycles occur concurrently and are coordinated over a 22–32 day cycle, with an average length of 28 days.

Ovarian Cycle: The first half of the ovarian cycle is the follicular phase. Slowly rising levels of FSH and LH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they begin releasing estrogens and a low level of progesterone. Just prior to the middle of the cycle (approximately day 14), the high level of estrogen causes FSH and especially LH to rise rapidly, then fall. The spike in LH causes ovulation: the most mature follicle ruptures and releases its egg. The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate. Following ovulation, the ovarian cycle enters the luteal phase, which runs from about day 15 to 28. The name luteal phase refers to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a structure called a corpus luteum. The corpus luteum produces estrogen and progesterone. The progesterone inhibits the release of further FSH and LH. The inhibition of FSH and LH prevents any further eggs and follicles from developing while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days. If implantation of a fertilized egg does not occur, the corpus luteum regresses, and progesterone and estrogen levels drop. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, which releases FSH and LH and starts the cycle again.
Uterine Cycle: The uterine cycle is a function of the ovarian cycle, meaning that the changes in the endometrium of the uterus are the result of changes in hormones produced by the ovary. It has 3 phases, beginning with menstruation, followed by the proliferative and secretory phases. If a pregnancy (implantation) does not occur, the endometrial lining is sloughed off, and menstruation proceeds. After about five days, in response to rising levels of estrogen, the uterine cycle enters the proliferative phase. The endometrium begins to regrow, replacing the blood vessels and glands that have deteriorated. From day 15 to 28, the production of an increasing amount of progesterone by the corpus luteum facilitates the regrowth of the uterine lining during the secretory phase. The uterus is being prepared to accept a fertilized egg, should it occur during this cycle. Progesterone maintains the endometrium to help ensure pregnancy should fertilization happen. If it does not, the endometrium begins to degenerate as the progesterone levels drop, initiating the next uterine cycle.
Menopause: As women approach their mid-40s to mid-50s, their ovaries begin to lose their sensitivity to FSH and LH. Menstrual periods become less frequent and finally cease; this is menopause. There are still eggs and potential follicles on the ovaries, but without the stimulation of FSH and LH, they will not produce a viable egg to be released. The outcome of this is the inability to have children.
The side effects of menopause include hot flashes, heavy sweating (especially at night), headaches, some hair loss, muscle pain, vaginal dryness, insomnia, depression, weight gain, and mood swings. Estrogen is involved in calcium metabolism; without it, blood levels of calcium decrease. To replenish the blood, calcium is lost from bone which may decrease bone density and lead to osteoporosis. Supplementation of estrogen in the form of hormone replacement therapy (HRT) can prevent bone loss, but the therapy can have negative side effects. While HRT is thought to give some protection from colon cancer, osteoporosis, heart disease, macular degeneration, and possibly depression, its negative side effects include, in some women, increased risk of stroke or heart attack, blood clots, breast cancer, ovarian cancer, endometrial cancer, gall bladder disease, and possibly dementia.
Fertilization
Learning Objectives
- Define the term fertilization
- Discuss internal fertilization
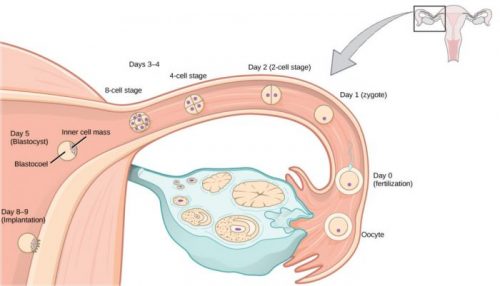
In humans, sexual reproduction starts with the combination of a sperm and an egg in a process called internal fertilization. Once fertilized, the eggs develop inside the female. Fertilization is the process by which gametes (an egg and sperm) fuse to form a zygote. The egg and sperm each contain one set of chromosomes. To ensure that the offspring has only one complete diploid set of chromosomes, only one sperm must fuse with one egg. In humans and mammals, the egg is protected by a layer of an extracellular matrix consisting mainly of glycoproteins called the zona pellucida. When a sperm binds to the zona pellucida, a series of biochemical events, called acrosomal reactions, take place. The acrosome contains digestive enzymes that initiate the degradation of the glycoprotein matrix protecting the egg and allowing the sperm plasma membrane to fuse with the egg plasma membrane. The fusion of these two membranes creates an opening through which the sperm nucleus is transferred into the ovum. The nuclear membranes of the egg and sperm break down, and the two haploid genomes condense to form a diploid genome.
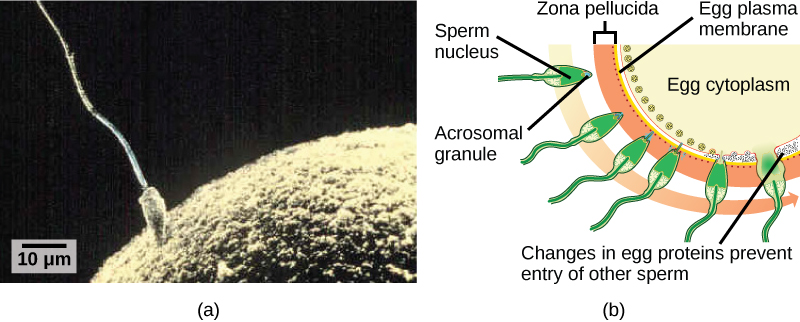
To ensure that no more than one sperm fertilizes the egg, once the acrosomal reactions take place at one location of the egg membrane, the egg releases proteins in other locations to prevent other sperm from fusing with the egg. If this mechanism fails, multiple sperm can fuse with the egg, resulting in polyspermy. The resulting embryo is not genetically viable and dies within a few days.
Contraception and Birth Control
The prevention of pregnancy comes under the terms contraception or birth control. Strictly speaking, contraception refers to preventing the sperm and egg from joining. Both terms are, however, frequently used interchangeably.
| Method | Examples | Failure Rate in Typical Use Over 12 Months |
| Barrier | male condom, female condom, sponge, cervical cap, diaphragm, spermicides | 15 to 24% |
| Hormonal | oral, patch, vaginal ring | 8% |
| injection | 3% | |
| implant | less than 1% | |
| Other | natural family planning | 12 to 25% |
| withdrawal | 27% | |
| sterilization | less than 1% |
Table 19.3 lists common methods of contraception. The failure rates listed are not the ideal rates that could be realized but the typical rates that occur. A failure rate is the number of pregnancies resulting from the method’s use over a twelve-month period. Barrier methods, such as condoms, cervical caps, and diaphragms, block sperm from entering the uterus, preventing fertilization. Spermicides are chemicals that are placed in the vagina that kill sperm. Sponges, which are saturated with spermicides, are placed in the vagina at the cervical opening. Combinations of spermicidal chemicals and barrier methods achieve lower failure rates than the methods when used separately.
Nearly a quarter of the couples using barrier methods, natural family planning, or withdrawal can expect a failure of the method. Natural family planning is based on monitoring of the uterine cycle and having intercourse only during times when the egg is not available. A woman’s body temperature may rise a degree Celsius at ovulation, and the cervical mucus may increase in volume and become more pliable. These changes give a general indication of when intercourse is more or less likely to result in fertilization. Withdrawal involves the removal of the penis from the vagina during intercourse before ejaculation occurs. This is a risky method with a high failure rate due to the possible presence of sperm in the bulbourethral gland’s secretion, which may enter the vagina prior to removing the penis.
Hormonal contraception uses synthetic progesterone (sometimes in combination with estrogen), to inhibit the hypothalamus from releasing FSH or LH and thus prevent an egg from being available for fertilization. The method of administering the hormone affects the failure rate. The most reliable method, with a failure rate of less than 1 percent, is the implantation of the hormone under the skin. The same rate can be achieved through the sterilization or placement of an intrauterine device (IUD). Sterilization involves vasectomy in the man and tubal ligation in the woman. IUDs are inserted into the uterus and establish an inflammatory condition that prevents fertilized eggs from implanting into the uterine wall.
Compliance with the contraceptive method is a strong contributor to the success or failure rate of any particular method. The only method that is completely effective at preventing conception is abstinence. The choice of contraceptive method depends on the goals of the woman or couple. Tubal ligation and vasectomy are considered permanent prevention, while other methods are reversible and provide short-term contraception.
Termination of an existing pregnancy can be spontaneous or voluntary. Spontaneous termination is a miscarriage and usually occurs very early in the pregnancy, usually within the first few weeks. This occurs when the fetus cannot develop properly, and the gestation is naturally terminated. Voluntary termination of a pregnancy is an abortion. Laws regulating abortion vary between states and tend to view fetal viability as the criteria for allowing or preventing the procedure.
Infertility
Infertility is the inability to conceive a child or carry a child to birth. About 75 percent of causes of infertility can be identified; these include diseases, such as sexually transmitted diseases that can cause scarring of the reproductive tubes in either men or women or developmental problems frequently related to abnormal hormone levels in one of the individuals. Inadequate nutrition, especially starvation, can delay menstruation. Stress can also lead to infertility. Short-term stress can affect hormone levels, while long-term stress can delay puberty and cause less frequent menstrual cycles. Other factors that affect fertility include toxins (such as cadmium), tobacco smoking, marijuana use, gonadal injuries, and aging.
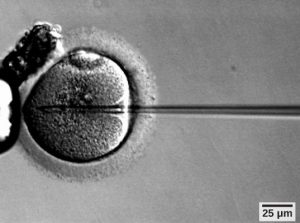
If infertility is identified, several assisted reproductive technologies (ART) are available to aid conception. A common type of ART is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the man, and they are combined with the eggs and supported through several cell divisions to ensure the viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure that injects sperm into an egg can be used. This is called intracytoplasmic sperm injection (ICSI). IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use. The procedures can also result in multiple births.
