Transport of Fluids within the Body
15 Urinary System
Introduction to the Urinary System
Learning Objective

Usually, when we think of the urinary system, we think about getting rid of waste products in our urine. The urinary system, however, involves more than just waste removal. The urinary system plays many important roles in the maintenance of homeostasis. This means this system helps to regulate the internal conditions of the whole body. For instance, if the body is dehydrated, the body will function to conserve the liquid. Consequently, the body does not produce large volumes of urine. Much of this proper maintenance of homeostasis is a function of the kidneys.
The roles of the urinary system include filtering the blood to remove toxins, maintaining water levels, maintaining appropriate levels of some vitamins and minerals, maintaining acid-base and electrolyte balances, and interacting with the circulatory system to help regulate blood pressure and red blood cell count. In a three-way interaction with both the respiratory and circulatory systems, the urinary system helps stabilize blood oxygen and carbon dioxide levels.
The final outcome of the above functions of the urinary system is excretion. Excretion is the removal of wastes generated by the normal processes of cell metabolism in the body. Such metabolic wastes include urea, uric acid, creatinine, creatine, bilirubin, and ammonia. The metabolic wastes originate in the cells throughout the body and are moved into the blood. If allowed to accumulate, these wastes would be toxic to the body. All of the organs of the urinary system are involved in the removal of these metabolic wastes by contributing to the process of excretion. Other body systems that are also involved in excretion are the respiratory system, integumentary system (the skin), and digestive system. Excretion and elimination are two similar processes. Excretion specifically refers to the removal of the waste products of metabolism from the body. Elimination is the expulsion of undigested or unmetabolized waste products from the body.
The major functions of the urinary system include:
- Excretion of metabolic waste products such as urea, uric acid, creatinine, bilirubin, and ammonia,
- Maintenance of homeostasis, or the ability of the urinary system to regulate its internal conditions,
- Detoxifying harmful substances in the body,
- Maintenance of proper water levels, vitamin and mineral levels, and acid-base and electrolyte levels,
- Interaction with the respiratory and circulatory systems helps to stabilize blood oxygen and carbon dioxide levels.
If the kidneys fail, these functions are compromised or lost altogether, with devastating effects on homeostasis. The affected individual might experience weakness, lethargy, shortness of breath, anemia, widespread edema (swelling), metabolic acidosis, rising potassium levels, heart arrhythmias, and more. Each of these functions is vital to your well-being and survival. The urinary system, controlled by the nervous system, also stores urine until a convenient time for disposal and then provides the anatomical structures to transport this waste liquid to the outside of the body. Failure of nervous control or the anatomical structures leading to a loss of control of urination results in a condition called incontinence.
This chapter will help you to understand the anatomy of the urinary system and how it enables the physiologic functions critical to homeostasis. It is best to think of the kidney as a regulator of plasma makeup rather than simply a urine producer. As you read each section, ask yourself this question: “What happens if this does not work?” This question will help you to understand how the urinary system maintains homeostasis and affects all the other systems of the body and the quality of one’s life.
Learn By Doing 15.1
Which is not a function of the urinary system?
- detoxification
- maintaining electrolyte homeostasis
- digestion of liquids
- regulation of blood pressure
What is the difference between excretion and elimination?
Urinary Structures and Functions
Learning Objectives
- Identify the gross anatomy of the urinary tract.
- Identify the major blood vessels entering and exiting the kidney.
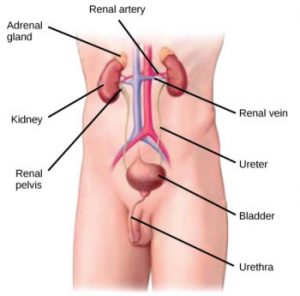
As noted above, much of the maintenance of proper chemical balance, or homeostasis, is the function of the kidneys. The kidneys are a pair of bean-shaped structures that are located just below and posterior to the liver in the peritoneal cavity. The adrenal glands sit on top of each kidney and are also called the suprarenal glands.
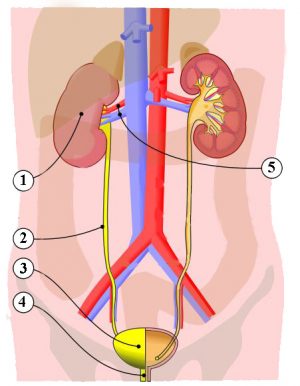
The process begins with blood that contains metabolic waste entering each of the two kidneys through the renal artery. Urine is produced by microscopic structures called nephrons in the kidneys. Once filtered, the blood exits through the renal vein. Urine leaves each kidney through a ureter. Each ureter transports the urine via peristalsis to the urinary bladder (a hollow, muscular chamber that collects and stores urine). A single urethra transports urine from the urinary bladder to the outside of the body. The urethra transports urine from the bladder to the outside of the body for disposal. The urethra is the only urologic organ that shows any significant anatomic difference between males and females; all other urine transport structures are identical.
This process through the smooth muscles is otherwise known as peristalsis. An internal urethral sphincter muscle and an external urethral sphincter muscle help keep the urine in the bladder until the process of urination. The internal urethral sphincter muscle surrounds the neck of the urinary bladder at the juncture of the bladder with the urethra. This smooth muscle opens reflexively when the bladder muscle contracts and builds up pressure. The external urethral sphincter muscle is located at the external opening of the urethra. This skeletal muscle is under voluntary control, and as a result of voluntary control, urination can be delayed for a time.
Urine is a fluid of variable composition that requires specialized structures to remove it from the body safely and efficiently. Blood is filtered, and the filtrate is transformed into urine at a relatively constant rate throughout the day. This processed liquid is stored until a convenient time for excretion. All structures involved in the transport and storage of urine are large enough to be visible to the naked eye. This transport and storage system not only stores the waste, but it protects the tissues from damage due to the wide range of pH and osmolarity of the urine, prevents infection by foreign organisms, and for the male, provides reproductive functions.
The process of urination is known as micturition which begins with blood carrying various wastes that enter each of the two kidneys through the renal artery and ends when urine exits out of the body through the urethra.
Learn By Doing 15.2
Match the location number on the diagram to the correct name and definition.
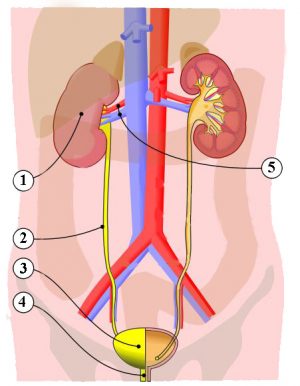 |
Name | Definition |
| Ureters | This is where the nephrons produce urine. | |
| Urinary bladder | Urine travels from the kidneys by circular contraction and is transported to the bladder through these. | |
| Kidney | Here is where urine is temporarily contained by internal and
external sphincter muscles. |
|
| Renal artery and vein | Here is where the entire process ends when urine exits out of the body through this. | |
| Urethra | The urinary process begins with blood carrying various wastes entering each of the two kidneys through one of these. Filtered blood exits the kidney through one of these. |
When enough urine has been produced in the ____1____ it leaves the through the ureters and urine is then transported to the ____2____.____3____ occurs in the smooth muscles and is the process of how stored urine moves from the kidneys, through the ureters, and into the bladder. This process using smooth muscle is otherwise known as peristalsis. The process of urination is referred to as ____4____ and urine is ultimately released through the ____5____. This body part connects the bladder to the outside of the body.
|
1 |
2 |
3 |
4 |
5 |
|
ureters kidneys bladder |
ureters kidneys bladder |
Circular contraction Circular reflexes Cyclical elongation |
micturition micturition circular contraction |
urethra sex organs kidneys |
Osmoregulation and Osmotic Balance
Learning Objective
Osmoregulation and osmotic balance are important bodily functions, resulting in water and salt balance. This regulation equalizes the number of solute molecules across a semi-permeable membrane by the movement of water to the side of higher solute concentration.
Recall that osmosis is the diffusion of water across a membrane in response to osmotic pressure caused by an imbalance of molecules on either side of the membrane. Osmoregulation is the process of maintenance of salt and water balance (osmotic balance) across membranes within the body’s fluids, which are composed of water, plus electrolytes and non-electrolytes. An electrolyte is a solute that dissociates into ions when dissolved in water. A non-electrolyte, in contrast, doesn’t dissociate into ions during water dissolution. Both electrolytes and non-electrolytes contribute to the osmotic balance. The body’s fluids can be divided into three categories depending on where they are located: 1) blood plasma, 2) the cytosol within cells, and 3) interstitial fluid, the fluid that exists in the spaces between cells and tissues of the body. The membranes of the body (such as the pleural, serous, and cell membranes) are semi-permeable membranes. Semi-permeable membranes are permeable (or permissive) to certain types of solutes and water. Solutions on two sides of a semi-permeable membrane tend to equalize in solute concentration by the movement of solutes and/or water across the membrane.
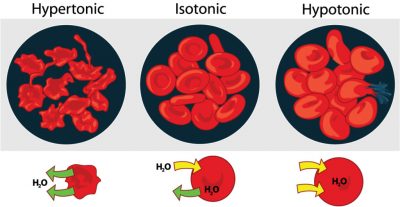
As seen in the figure, a cell placed in water tends to swell due to the gain of water from the hypotonic or low-solute environment. A cell placed in a solution with higher solute concentration, on the other hand, tends to make the membrane shrivel up due to loss of water into the hypertonic or high solute environment. Isotonic environments have an equal concentration of solutes inside and outside the cell; this equalizes the osmotic pressure on either side of the cell membrane which is a semi-permeable membrane.
The body does not exist in isolation. There is a constant input of water and electrolytes into the system. While osmoregulation is achieved across membranes within the body, excess electrolytes and wastes are transported to the kidneys and excreted, helping to maintain osmotic balance.
Need for Osmoregulation
Biological systems constantly interact and exchange water and nutrients with the environment by way of the consumption of food and water and through excretion in the form of sweat, urine, and feces. Without a mechanism to regulate osmotic pressure, or when a disease damages this mechanism, there is a tendency to accumulate toxic waste and water, which can have dire consequences.
Mammalian systems have evolved to regulate not only the overall osmotic pressure across membranes but also specific concentrations of important electrolytes in the three major fluid compartments: blood plasma, extracellular fluid, and intracellular fluid. Since osmotic pressure is regulated by the movement of water across membranes, the volume of the fluid compartments can also change temporarily. Because blood plasma is one of the fluid components, osmotic pressures have a direct bearing on blood pressure.
Learn By Doing 15.3
Why is excretion important in order to achieve osmotic balance?
Urinary Levels of Organization
The primary function of the urinary system is to maintain homeostasis of fluid and small molecules within the body. We will start with a molecular characterization of urine followed by molecular and tissue-level descriptions of the structures that are responsible for the formation of the urine. Then we will follow the movement of material from the bloodstream, through the functional units of the kidney through the other organs of the urinary system, and out of the body.
Molecular level – The Components of Urine
Learning Objectives
- Define the chemical properties of urine.
- Describe normal urine composition and the reasons why certain molecules are measured in lab tests of urine.
Our input of water varies greatly from day to day. Despite major differences in fluid intake, the total volume of fluid within the body remains relatively constant. The body’s fluid homeostasis is achieved largely due to the kidneys’ ability to regulate how much water is excreted in urine. If a person with healthy kidneys drinks a large volume of fluids, the kidneys will produce a large volume of urine. When a person with healthy kidneys does not drink enough fluids or experiences significant fluid loss, the kidneys will produce a small amount of concentrated urine to conserve water.
Urine is composed of urea, chloride, sodium, potassium, creatinine, and other compounds (ions, inorganic and organic). Urea is an organic breakdown product of nitrogenous materials. The table below lists some of the clinical characteristics of normal urine.
| Characteristic | Normal Value/Nature |
| Color/transparency | Yellow/clear |
| Odor | Varies from slightly aromatic to ammonia-like; food and beverages can change the odor |
| pH | 4.5 to 8.0 (average: 6.0) |
| Water content | 95 to 97 percent |
| Volume | 1 to 2 liters/ day (quarts/day) |
Learn By Doing 15.4
Match each of the molecules below to the reason it is measured in urine.
Creatinine, Sodium, Urea
- The amount of this in the urine helps to evaluate overall kidney functioning. It also gives an indication of other chemicals in the body such as the amount of protein.
- The amount of this in urine is indicative of your level of hydration. A urine test will determine the kidney’s ability to keep or discard excess of this from the urine.
- The level of this in a urine test reveals a person’s protein balance. In addition, excretion of this in the urine is indicative of overall kidney functioning.
Is urine more or less dense than water?
- less dense
- more dense
- similar density
Hint: Density is the mass per volume of a fluid. Specific gravity is the ratio of the density of a given fluid compared to water.
How much volume is urinated per day by a healthy adult?
- 1-2 mL
- 1-2 L
- 1-2 μL
- 100-200L
As noted above, the volume of urine can vary. Why would the volume change? (The answer needs to be more complete than simply, “drinking more would change the volume”.)
The Nephron, Unit of Function in the Kidney
Learning Objectives
- Describe the anatomy of the nephron.
- Identify and describe the functional process of urine formation, including filtration, reabsorption, and secretion.
- Follow the flow of blood through the nephron.
As the chief functional organ in the urinary system, the kidneys excrete nitrogenous (nitrogen-containing) wastes and are involved in regulating the volume, composition, and pH of the blood. The kidneys receive one-fourth of total cardiac output, a reflection of their function as blood processors. Each kidney contains about one million nephrons, the structural and functional units of the kidneys. Nephrons are made up of epithelial cells with an underlying non-cellular layer or basement membrane that separates the filter in the lumen fluid from the interstitial space.
Each nephron is made up of a high-pressure capillary bed called a glomerulus and a renal tubule. The ends of multiple nephrons join a common collecting duct. The nephrons are involved in three functions: filtration, reabsorption, and secretion. The structure within each nephron that actually filters blood plasma is the renal corpuscle.The renal corpuscle includes the glomerulus and glomerular capsule. The renal tubule is attached to the glomerular capsule and receives the filtered fluid, called glomerular filtrate. Very thin and a little over an inch long, the renal tubule has three major consecutive segments that the filtrate flows through a proximal convoluted tubule(PCT), the nephron loop (loop of Henle), and a distal convoluted tubule(DCT).
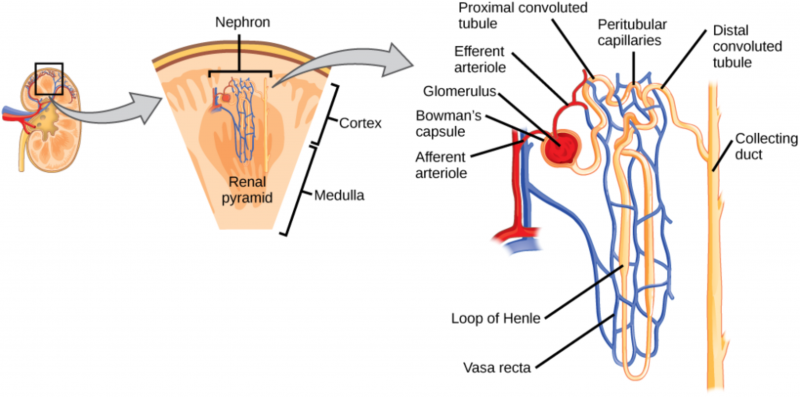
The Glomerulus
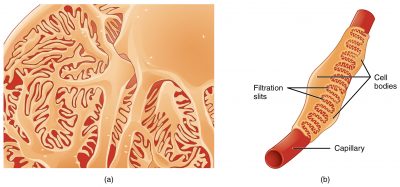
The renal corpuscle is made up of a tangled capillary network called the glomerulus and a cup-shaped structure called the glomerular capsule (Bowman’s capsule) surrounding the glomerulus. The glomerular capsule has an external layer made of simple squamous epithelium. Although this layer is not involved in the production of filtrate, it helps to maintain the shape of the capsule. An inner layer adheres to the glomerular capillaries and is composed of a special type of simple squamous epithelial cells called podocytes. These cells interlock, forming filtration slits. Filtrate from the glomerulus passes through filtration slits and enters the capsular space (Bowman’s space).
The Proximal Convoluted Tubule
The proximal convoluted tubule (convoluted refers to the coiled shape) tubule connects the glomerular capsule to the nephron loop. The surface of the simple cuboidal epithelial cells making up the proximal convoluted tubule are covered in microvilli. The microvilli and the length of the proximal convoluted tubule dramatically increase the surface area available for reabsorbing water and solutes and for secreting substances into the filtrate.
The Nephron Loop
The renal corpuscle, the proximal convoluted tubule, and the juncture between the proximal convoluted tubule and the nephron loop are located in the outer rim of the kidney, called the renal cortex. The first part of the nephron loop, the descending limb of the nephron loop, drops into the middle of the kidney, called the renal medulla. In the renal medulla, the loop makes a sharp, almost 180-degree turn back toward the renal cortex as the ascending limb of the nephron loop. The ascending limb is continuous with the distal convoluted tubule. The ascending and descending limbs of the nephron loop have two distinct parts: a thin section of the limb and a thick section of the limb. In the thin section of the limb, the diameter of the tubule is distinctly smaller than the diameter of the rest of the nephron tubules. In the thin sections of the limbs, the epithelium is thinner simple squamous epithelium that is permeable to water. In the thick sections of the limbs, the epithelium is simple cuboidal epithelium that is highly impermeable to water. Regardless of being in the thin or the thick segments, the lumen is the same size as the lumen in the rest of the renal tubule.
Distal Convoluted Tubule
The final segment of the nephron is the distal convoluted tubule. As the ascending limb of the nephron loop reaches the renal cortex, it becomes the distal convoluted tubule. The distal convoluted tubule extends to the collecting duct. The distal convoluted tubule is composed of simple cuboidal epithelium with very few microvilli and no brush border.
Capillaries of the Nephron
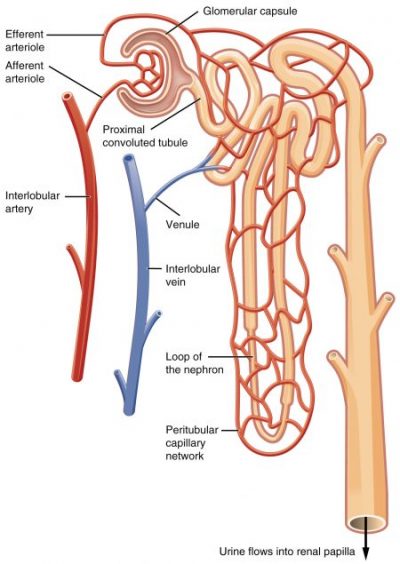
The glomerulus is not the only capillary bed associated with nephrons. Peritubular capillaries are branches of the efferent arterioles that drain the glomeruli and recover most of the filtrate produced in the renal corpuscle. Glomerular capillaries differ from other capillary beds in the body because they are both supplied by and drained by arterioles. The feeder afferent arterioles are branches of the cortical radiate arteries. The draining efferent arterioles branch into the peritubular capillary network around the proximal and distal convoluted tubules or the vasa recta around the nephron loop. The diameter of the draining efferent arterioles is smaller than that of the afferent arterioles, giving the efferent arterioles higher resistance. Because of this, the glomerulus has a high blood pressure that allows it to filter high volumes of fluid and solutes out of the blood and into the glomerular capsule. The nephrons’ segments reabsorb approximately 99 percent of this filtrate. The peritubular capillaries adhere to neighboring convoluted tubules and drain into neighboring venules. These low-pressure and porous capillaries easily reabsorb the water and solutes that the tubule recovers from the filtrate. In some nephrons, rather than breaking up into peritubular capillaries, the efferent arterioles form clusters of thin-walled vasa recta. Important for the formation of concentrated urine, the vasa recta are long, straight capillaries that reach deep into the medulla alongside the longest nephron loops where they can collect reabsorbed substances from the loop segments.
Collecting Ducts
As the functional units of the kidneys, the primary role of the nephrons is to filter plasma, reabsorb what the body would like to keep and excrete the rest. Any substances not reabsorbed in the tubules of the nephrons flow into one of the thousands of collecting ducts in the kidney. Each collecting duct receives fluid from several nephrons and then transports it to an area called the renal pelvis.
Learn By Doing 15.5
The primary function of the collecting ducts, located in the kidneys, is to:
- Filter plasma, reabsorb what the body would like to keep, and excrete the rest.
- Facilitate the process of urine traveling through the smooth muscles, otherwise known as parasitosis.
- Collect any substance not reabsorbed along the nephrons.
- Expand the surface area that is available for reabsorbing water and solutes.
The part of the kidneys that makes them functional organs is/are called:
- loop of Henle
- microvilli
- nephrons
- renal tubule
The renal corpuscle is the first site of exchange between the cardiovascular system and the urinary system. Which of the following correctly pairs the structures with the contents of the structure?
- The glomerulus contains cardiovascular capillaries, and the glomerular (Bowman’s) capsule contains the urinary filtrate.
- The glomerular capsule contains cardiovascular capillaries, and the glomerulus contains the urinary filtrate.
- The glomerulus contains both the cardiovascular capillaries and the urinary filtrate.
- The glomerular capsule contains both the cardiovascular capillaries and the urinary filtrate.
Which of the following is the correct order of tubules after the glomerular capsule?
- proximal convoluted tubule, nephron loop, distal convoluted tubule, collecting duct
- proximal convoluted tubule, distal convoluted tubule, loop of Henle, collecting duct
- loop of Henle, proximal convoluted tubule, distal convoluted tubule, collecting duct
- collecting duct, proximal convoluted tubule, distal convoluted tubule, loop of Henle
Which are not blood vessel structures associated with nephrons?
- glomerulus
- alveolar capillaries
- peritubular capillaries
- vasa recta
Urine Formation
To produce urine, nephrons and collecting ducts carry out three basic functions: glomerular filtration, tubular reabsorption, and tubular secretion.
The first step in urine production is glomerular filtration. In this process, water and most of the solutes in blood plasma pass through the wall of glomerular capillaries, first into the glomerular capsule and then into the renal tubule. The product of glomerular filtration is referred to as glomerular filtrate.
During tubular reabsorption, cells of the tubule reabsorb almost all water and a variety of solutes from the filtrate as it flows through the renal tubule and collecting duct. These reabsorbed substances are then returned to the blood in the peritubular capillaries and vasa recta. In contrast to absorption, in which new substances enter the body (e.g., through the gastrointestinal tract), reabsorption refers to substances that have been removed from the blood being returned to the blood.
In the process of tubular secretion, the renal tubule and collecting duct actively transport substances (e.g., wastes, drugs, excess ions) from the blood in the peritubular capillaries. Secretion, in this case, refers to the removal of substances from the blood. In contrast, the secretion of hormones or enzymes, for example, refers to cells releasing substances into blood, ducts, and interstitial fluid.
Learn By Doing 15.6
Production of urine that modifies plasma makeup is the result of ________.
- filtration
- absorption
- secretion
- filtration, absorption, and secretion
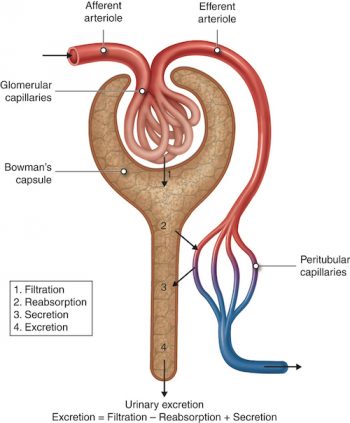
The normal amount of filtrate produced as a result of glomerular filtration is so high that the amount of fluid entering the proximal convoluted tubules in 30 minutes is greater than the total blood plasma volume. Clearly, some of this fluid must be reclaimed and sent back into the bloodstream to maintain water balance and ion concentrations. This reclamation process occurs through reabsorption in the tubules. Secretion is essentially the opposite of reabsorption. It removes the additional solutes from the plasma and actively transports them to the tubule. Many students get confused initially with the concept that secretion means substances end up in the urine and reabsorption means substances end up back in the blood.
The glomerular capillaries filter about one-fifth of the plasma that flows through the kidneys into the renal tubules. Glomerular filtration works like any other filtration process. For example, a coffee filter prevents large coffee grounds from passing through it while allowing the passage of water and small solutes such as flavor molecules and caffeine. In the same way, the glomerular filtration membrane blocks the passage of blood cells and proteins while allowing water and other solutes from the blood to pass into the glomerular capsule. These substances are forced through the membrane by the higher hydrostatic pressure in the glomerular capillary than in the capsular space.
As described above, a porous filtration membrane separates the inside of the glomerular capsule from the blood. It is made of glomerular capillary endothelium, the gel-like basal lamina basement membrane, and the podocyte-formed filtration slit. Water and solutes smaller than about three nanometers in diameter (e.g., glucose, amino acids, nitrogenous wastes) pass freely across the membrane between the blood and capsule. This means there are similar concentrations of these substances in both the blood and the glomerular filtrate. Some bigger molecules may find a way through the membrane, but molecules larger than five nanometers (large proteins and blood cells) do not usually get into the tubule.
Reabsorption starts as soon as filtrate enters the proximal convoluted tubules. Before the reabsorbed substances can reenter the blood, they must pass through barriers: both membranes of cells in the tubule and the endothelium of the peritubular capillaries.
Reabsorption returns about 99 percent of filtered water and many filtered solutes to the bloodstream. Although cells in the proximal convoluted tubule perform most reabsorption, epithelial cells all along the length of the renal tubule and the collecting duct also contribute to this process. To maintain normal plasma levels, almost every organic nutrient (e.g., glucose, amino acids) is completely reabsorbed. The amount of water and the number of ions reabsorbed is determined by hormonal signals and is based on homeostatic needs. The scope of reabsorption can be appreciated by looking at water. Each day, about 180 liters (190 quarts) of water are filtered in the kidneys. Only 1–2 liters (1–2 quarts) are excreted in urine; the rest is reabsorbed in the kidneys.
Tubular secretion transfers unwanted substances from the blood and tubule cells into the tubular fluid. With the exception of potassium ions, most secretion occurs in the proximal convoluted tubule. However, some secretion also occurs in the cortical regions of the collecting ducts and in the late distal convoluted tubule.
Tubular secretion is important for a number of reasons. It removes substances that are not easily filtered, such as some drugs and metabolites that are securely attached to plasma proteins. Second, it disposes of unwanted substances or end products that have been reabsorbed passively, such as urea and uric acid. Third, it eliminates excess potassium ions. Finally, it regulates blood pH. As an example, when blood pH becomes too acidic, secretion adds more hydrogen ions (acid) into the filtrate and retains more bicarbonate ions (a base).
The figure and table below summarize filtration, reabsorption, and secretion.
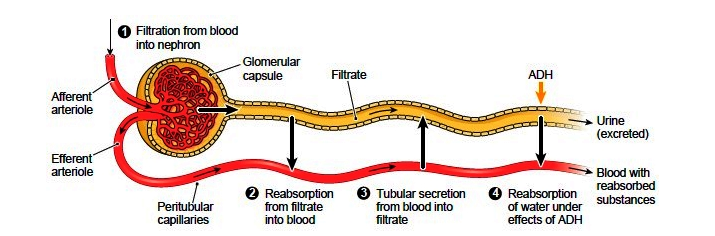
| Nephron Structure | Function | Description |
| Glomerulus/ Glomerular Capsule | Filtration | The glomerulus is a capillary network found in close proximity to the nephron that filters plasma into the nephron. Proteins and blood cells are retained in the glomerular capillary. |
| Tubules and nephron loop (loop of Henle) | Reabsorption | Epithelial cells actively transport some substances from the tubular fluid back into the blood. Other substances, such as water, are passively reabsorbed in some segments. |
| Capillaries (specifically Peritubular) | Secretion | Epithelial cells actively secrete certain substances from the blood into the tubular lumen. |
| Collecting duct | Collection | Accumulates any material that is not returned to the blood in the preceding segments. Secretes or reabsorbs H+, HCO3+, and K+ ions. Reabsorbs water under the influence of anti-diuretic hormone. Anything left in the distal end of the collecting duct will l be excreted as urine |
Learn By Doing 15.7
To produce urine, nephrons and collecting ducts carry out three basic functions:
1. Glomerular filtration is
- the first step in urine production is where water and most of the solutes in blood plasma pass through into the renal tubule.
- a process where reabsorbed substances are returned to the blood as it travels along the peritubular capillaries and vasa recta.
- is the additional removal of substances from the blood in the peritubular capillary network or the vasa recta.
2. Reabsorption is
- when cells of the tubule reabsorb almost all water and solutes from the filtrate as it flows through the renal tubule and collecting duct and returns the fluid and solutes to the blood.
- when cells in the renal tubule and collecting duct collect substances (e.g., wastes, drugs, excess ions) from the filtrate as it flows through the tubule and duct.
- when water and most of the solutes in blood plasma pass through the wall of glomerular capillaries.
3. Secretion occurs
- when cells in the renal tubule and collecting duct remove additional substances from the blood as it flows through the peritubular capillaries or the vasa recta.
- when water and solutes in blood plasma pass through the wall of glomerular capillaries, first into the glomerular capsule and then into the renal tubule.
- upon the return of substances to the bloodstream.
Doctors will look for the serum proteins in the urine as a test for kidney damage. Why?
Why are most of the substances filtered through the kidneys reabsorbed? Why is urea the one substance that is not reabsorbed to the extent that the others are?
Kidneys
Learning Objectives
- Describe the structure of the kidneys and the functions of the parts of the kidney.
- Describe the internal and external structure of the kidney, including its location and covering.
- Identify, and describe the structure and location of the ureters, urinary bladder, and urethra.
Although the kidneys are the major osmoregulatory organ, the skin and lungs also play a role in the process. Water and electrolytes are lost through sweat glands in the skin, which helps moisturize and cool the skin surface, while the lungs expel a small amount of water in the form of mucous secretions and via evaporation of water vapor.
Kidney Structure
Kidneys filter blood and purify it. All the blood in the human body is filtered many times a day by the kidneys; these organs use up almost 25 percent of the oxygen absorbed through the lungs to perform this function. Oxygen allows kidney cells to efficiently manufacture chemical energy in the form of ATP through aerobic respiration. The final filtrate coming out of the kidneys is called urine.
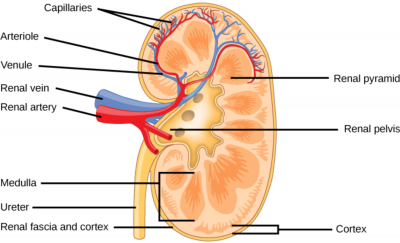
Externally, the kidneys are surrounded by three layers. The outermost layer is a tough connective tissue layer called the renal fascia. The second layer is called the perirenal fat capsule, which helps anchor the kidneys in place. The third and innermost layer is the renal capsule. Internally, the kidney has three regions—an outer cortex, a medulla in the middle, and the renal pelvis in the region called the hilum of the kidney. The hilum is the concave part of the bean-shape where blood vessels and nerves enter and exit the kidney; it is also the point of exit for the ureters.
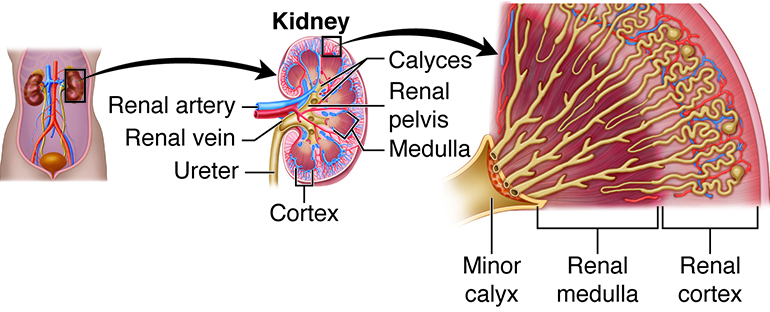
The renal cortex is granular due to the presence of nephrons—the functional unit of the kidney. The medulla consists of multiple pyramidal tissue masses called renal pyramids. In between the pyramids are spaces called renal columns through which the blood vessels pass. The tips of the pyramids, called renal papillae, point toward the renal pelvis. There are, on average, eight renal pyramids in each kidney. The renal pyramids along with the adjoining cortical region are called the lobes of the kidney. The renal pelvis leads to the ureter on the outside of the kidney. On the inside of the kidney, the renal pelvis branches out into two or three extensions called the major calyces, which further branch into the minor calyces. The collecting ducts empty into the renal papillae that in turn empty into the calyces. The ureters are urine-bearing tubes that exit the kidney and empty into the urinary bladder.
Because the kidney filters blood, its network of blood vessels is an important component of its structure and function. The arteries, veins, and nerves that supply the kidney enter and exit at the renal hilum. Renal blood supply starts with the branching of the aorta into the renal arteries (which are each named based on the region of the kidney they pass through) and ends with the exiting of the renal veins to join the inferior vena cava. The renal arteries split into several segmental arteries upon entering the kidneys. Each segmental artery splits further into several interlobar arteries and enters the renal columns, which supply the renal lobes. The interlobar arteries split at the junction of the renal cortex and medulla to form the arcuate arteries. The arcuate “bow-shaped” arteries form arcs along the base of the medullary pyramids. Cortical radiate arteries, as the name suggests, radiate out from the arcuate arteries. The cortical radiate arteries branch into numerous afferent arterioles and then enter the capillaries supplying the nephrons. Veins trace the path of the arteries and have similar names, except there are no segmental veins.
Example: Kidney Stones
As we learned in this chapter, the kidney plays a very important role in the body as it filters out waste products. Sometimes kidney stones can form when there is a build-up of specific minerals in your urine. Kidney stones are hard, pebble-like pieces of material that form in one or both of your kidneys. They rarely cause permanent damage if treated by a healthcare professional.
Kidney stones vary in size and shape. They may be as small as a grain of sand or as large as a pea. Rarely, some kidney stones are as big as golf balls. Kidney stones may be smooth or jagged and are usually yellow or brown. A small kidney stone may pass through your urinary tract on its own, causing little or no pain. A larger kidney stone may get stuck along the way. A kidney stone that gets stuck can block your flow of urine, causing severe pain or bleeding.
There are different types of kidney stones, depending on what type of mineral buildup has occurred:
- Calcium stones. Calcium stones, including calcium oxalate stones and calcium phosphate stones, are the most common types of kidney stones. Calcium oxalate stones are more common than calcium phosphate stones. Calcium from food does not increase your chance of having calcium oxalate stones. Normally, extra calcium that isn’t used by your bones and muscles goes to your kidneys and is flushed out with urine. When this doesn’t happen, the calcium stays in the kidneys and joins with other waste products to form a kidney stone.
- Uric acid stones. A uric acid stone may form when your urine contains too much acid. Eating a lot of fish, shellfish, and meat—especially organ meat—may increase uric acid in urine.
- Struvite stones. Struvite stones may form after you have a UTI. They can develop suddenly and become large quickly.
- Cystine stones. Cystine stones result from a disorder called cystinuria that is passed down through families. Cystinuria causes the amino acid cystine to leak through your kidneys and into the urine.
Learn By Doing 15.8
Match the terms below to the correct description.
Terms: renal hilum, renal fascia, papillary ducts, renal medulla, nephrons, adipose capsule, renal capsule, renal cortex
- There are about one million of these functional units in each kidney.
- This structure preserves the form of the kidney while protecting it from damage due to trauma
- The primary purpose of this area, located under the superficial layer of the kidney, is to maintain the proper balance of salt and water in the blood.
- This is a concave area where the renal artery enters the kidney.
- Urine produced by nephrons empties into these.
- This fastens each kidney to neighboring structures and to the abdominal wall.
- This superficial layer of the kidney acts as a filter for the blood and so removes metabolic waste.
- This fatty tissue surrounds the renal capsule and provides additional protection and helps to anchor the kidney in place.
Describe the three major regions of the kidney’s internal structure.
The Ureters
The ureters are a pair of thin, muscular tubes that transport urine from the kidneys to the bladder. Beginning at the level of the second lumbar vertebra, the location of the ureters is retroperitoneal. Each ureter runs inferiorly and enters the posterolateral wall of the urinary bladder. This angle of entry is important because it helps prevent urine from flowing back into the ureters when the bladder fills with urine. In addition, accumulating urine increases the internal pressure of the bladder, and this pressure compresses and seals the distal portion of the ureters.
There are three layers in the ureter wall. The innermost mucosa lining contains transitional epithelium capable of stretching but is impermeable to urine. The ability to stretch allows the ureter wall to accommodate changing volumes of urine. The middle muscularis layer is composed of two layers of smooth muscle: an inner longitudinal layer and an outer circular layer. In the lower third of the ureter, the muscularis has a third outer layer of longitudinal muscle fibers. The muscularis layer is responsible for the peristaltic contractions needed to move urine through the ureters and into the bladder. The external layer of the ureter wall, the adventitia, is made of fibrous connective tissue and helps anchor the ureter to the abdominal wall.
When urine enters and distends the ureters, stretch receptors are stimulated. Reflexive action results in the contraction of the muscularis and movement of the urine into the bladder. The power and frequency of peristalsis are directly related to the rate of urine formation. Although the ureters are innervated by both sympathetic and parasympathetic fibers, the nervous system does not appear to have major involvement in the transport of urine in these organs.
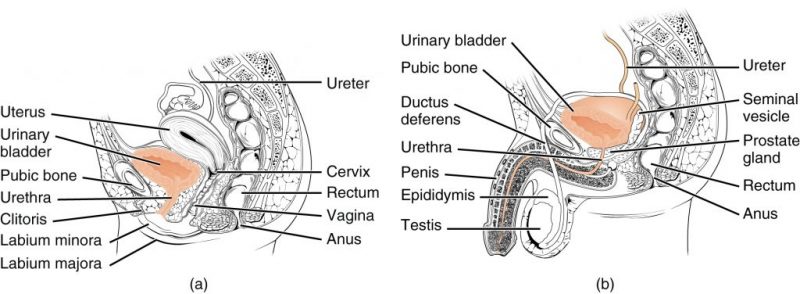
The Urinary Bladder
The urinary bladder is a hollow, collapsible muscular sac that serves as a temporary storage facility for urine. It is located in the pelvic cavity, just posterior to the pubic symphysis. In females, the bladder lies anterior to the vagina and inferior to the uterus. In males, it is immediately anterior to the rectum. Peritoneal folds hold the bladder in place.
The bladder can hold up to about a liter of urine, although this amount varies from person to person. Despite its capacity to enlarge, an overfull bladder can burst, but it is more likely that excess urine will leak out of the urethra. When empty, the bladder collapses into a pyramidal shape. When a small amount of urine accumulates, it is spherical. When a larger volume of urine accumulates, the bladder becomes pear-shaped and ascends into the abdominal cavity. There are three openings in the bladder: two for the ureters and one for the urethra. These openings frame a triangular region at the base of the bladder called the trigone.
The bladder wall is made up of a mucosa with transitional epithelium, a submucosa, a thick muscularis called the detrusor muscle, and a fibrous adventitia. The adventitia is on the inferior surface only. In contrast, the peritoneum covers the superior surface. The detrusor muscle is composed of inner and outer layers of longitudinal smooth muscle fibers and an intermediate layer of circular muscle fibers.
The Urethra
The urethra is a small muscular tube that transports urine from the bladder out of the body. The urethra is five times longer in males (8 inches, 20 cm) than in females (1.6 inches, 4 cm). In males, the urethra is also part of the reproductive system, providing a passageway for semen as well as urine. The course of the urethra also differs between the sexes. In females, fibrous connective tissue binds it to the anterior vaginal wall, and its external urethral orifice(external opening) is located anterior to the vaginal opening and posterior to the clitoris. In males, the urethra is divided into three regions. The prostatic urethra is surrounded by the prostate. The membranous urethra passes through the urogenital diaphragm. The spongy urethra runs through the penis and ends at the external urethral orifice.
At the bladder-urethra junction, the circular fibers of the bladder’s detrusor muscle form the internal urethral sphincter. When urine is not draining from the bladder, this involuntary sphincter closes off the urethra to prevent the leakage of urine when you are not voiding. At the point where the urethra passes through the urogenital diaphragm, it is surrounded by the external urethral sphincter, a skeletal muscle. The external sphincter is voluntarily controlled and is kept contracted until voiding.
Example: Urinary Tract Infections
Urinary tract infections (UTIs) are the most common type of bacterial infection. Women are predisposed to UTIs because their urethras are shorter than those of men. Moreover, the urethra’s external opening in women is closer to the anus than it is in men. Over 50 percent of women will have a UTI at some point during their lifetime. Fecal bacteria such as Escherichia coli (E. coli) can easily travel up the urethra. This is why women should never wipe the anus in a forward direction after defecation. However, most UTIs in women occur as a result of sexual activity. During intercourse, bacteria from the external genital area and the vagina can be pushed up the short urethra toward the bladder. The use of spermicides actually increases the risk of UTIs because spermicides kill bacteria that would otherwise help destroy infectious fecal bacteria in the vagina. Drinking plenty of water and urinating immediately after sexual activity can help prevent UTIs by flushing bacteria out of the urethra. Infection of the urethra (urethritis) can easily spread to the urinary bladder (cystitis) and sometimes to the kidneys (pyelitis or pyelonephritis). Symptoms of a UTI include pain during urination (dysuria), frequent urination or an urgent need to urinate, cloudiness or blood in the urine (hematuria), urine with a strong odor, nausea, and fever. Fortunately, most UTIs respond to antibiotics. Analgesics may also be prescribed to reduce discomfort. Unfortunately, having a UTI increases the chances of having subsequent UTIs.
Learn By Doing 15.9
Which renal functions are the ureters involved with?
- Excretion
- Elimination
- Both
- Neither
What holds the bladder in place?
- the bladder is free to move
- folds in the peritoneum
- adipose tissue
- the ureters
What are the main differences between the male and female urethras?
- The female urethra is longer and is part of the reproductive system.
- The male urethra is longer and is part of the reproductive system.
- The female urethra is longer but is not part of the reproductive system.
- The male urethra is longer but is not part of the reproductive system.
Why are women for likely to have a urinary tract infection when compared to men?
- Women’s urethras are longer than those of men; the urethra’s external opening in women is closer to the anus than it is in men.
- Women’s urethras are shorter than those of men; the urethra’s external opening in women is closer to the anus than it is in men.
- Women’s urethras are shorter than those of men; the urethra’s external opening in men is closer to the anus than it is in men.
- Women and men have an equal chance of having a UTI.
Regulation of Kidney Function
Hormonal Regulation
While the kidneys operate to maintain osmotic balance and blood pressure in the body, they also act in concert with hormones. Hormones are small molecules that act as messengers within the body. Hormones are typically secreted from one cell and travel in the bloodstream to affect a target cell in another portion of the body. Different regions of the nephron bear specialized cells that have receptors to respond to chemical messengers and hormones.
The table below summarizes the hormones that control osmoregulatory functions.
| Hormone | Where produced | Function |
| Epinephrine and Norepinephrine | Adrenal medulla | can decrease kidney function temporarily through vasoconstriction |
| Renin | Kidney nephrons | Increases blood pressure by acting on angiotensinogen |
| Angiotensin | Liver | Angiotensin II affects multiple processes and increases blood pressure |
| Aldosterone | Adrenal cortex | Prevents loss of sodium and water |
| Anti-diuretic hormone (vasopressin) | Hypothalamus (stored in the posterior pituitary) | Prevents water loss |
| Atrial natriuretic peptide | Heart atrium | Decreases blood pressure by acting as a vasodilator and increasing glomerular filtration rate; decreases sodium reabsorption in kidneys |
Neural Regulation
The sympathetic nerve fibers that innervate renal blood vessels provide an extrinsic regulatory mechanism for glomerular filtration. During extreme stress or blood loss, the sympathetic nervous system must meet the needs of the body as a whole, for example, by temporarily reducing kidney activity and redirecting blood to other vital organs. In such situations, neural controls override renal autoregulation. The sympathetic nerve fibers release the neurotransmitter norepinephrine. Norepinephrine activates alpha-adrenergic receptors on vascular smooth muscle and causes afferent arterioles to constrict. The resulting reduced blood flow into glomerular capillaries lowers net filtration pressure. This decreased renal blood flow helps maintain blood volume by reducing urine output and increasing perfusion to other body tissues.
Learn By Doing 15.10
Kidneys help synthesize calcitriol, an enzyme that is found in the digestive, endocrine, and integumentary systems. Explain how calcitriol benefits the entire body.
- Calcitriol is necessary as it allows for the passage and direction of sperm.
- Calcitriol is necessary to help regulate the volume of lymph and interstitial fluid.
- Calcitriol is necessary for the absorption of dietary calcium in the digestive and integumentary systems which promotes bone reabsorption in the endocrine system.
- Calcitriol is necessary to prevent the abnormal function of enzymatic pathways in the respiratory system.
Homeostatic Functions
The kidneys do most of the work of the urinary system. In addition to being the major excretory organs, the kidneys are important regulators of the volume and chemical composition of blood, and they maintain the correct balance between water and salts, and between acids and bases, in the body. They also regulate blood glucose levels, produce hormones, and metabolize vitamin D to its active form, calcitriol.
| Function | Description |
| Regulate ionic composition of blood | Homeostatic maintenance of plasma levels of ions, including sodium, potassium, phosphate, calcium, and chloride ions |
| Regulate blood pH | Buffer hydrogen ion levels in the blood by excreting some in urine and by conserving bicarbonate ions, which buffer hydrogen ions in the blood |
| Regulate blood volume | Either conserve water or eliminate it in urine |
| Regulate blood pressure | Secrete renin, which activates the renin-angiotensin-aldosterone system and increases blood pressure |
| Maintain blood osmolarity | Regulate water loss and solute loss in urine |
| Produce hormones | Help control calcium homeostasis with calcitriol and stimulates the formation of red blood cells with erythropoietin |
| Regulate blood glucose | Perform gluconeogenesis, releasing glucose into the blood to maintain normal levels |
| Excrete waste/foreign substance | Form urine, which eliminates unneeded substances, wastes from metabolic reactions (e.g., ammonia, bilirubin, uric acid), and foreign substances (e.g., drugs, environmental toxins) |
Integration of the Urinary System
The urinary system is responsible for only a part of our body’s ability to exchange material with the environment. It is not the only excretory system in the body. Several other organs, tissues, and processes are also involved in excretion. These structures temporarily store wastes, transport them for removal, or excrete the wastes and excess materials from the body.
Excretory Organs
The digestive system participates in waste removal in two ways. First, the liver detoxifies some substances. One example is the conversion of ammonia into urea. The large intestine is also considered an excretory organ. It eliminates a number of substances through defecation, including undigested food, water, carbon dioxide, water, salts, cholesterol, and heat. The respiratory system may seem like an unlikely waste remover, but when we exhale, the lungs excrete carbon dioxide and also rid the body of heat and some water vapor. Finally, the sweat glands in the skin are important excretory structures. They help dispose of excess water, heat, and carbon dioxide, as well as small amounts of salts and urea.
Table of Excretory Organs
| Organ System | Organ | Major Excretory Function |
| Digestive | Large intestine | Defecation removes solid waste and some water |
| Integumentary | Skin/sweat glands | Remove water, salts, and other wastes |
| Respiratory | Lungs | Remove carbon dioxide |
| Urinary | Kidneys | Remove wastes and excess substances from the blood |
Integrations of Body Systems
The kidneys are critical organs because they regulate blood volume and blood pressure. These organs perform this regulatory role by altering the amount of water that is eliminated in urine, as well as by releasing the chemicals renin and erythropoietin. When blood pressure drops, the kidneys secrete renin, which is both a hormone and an enzyme. Renin activates a hormonal pathway that increases blood pressure. When oxygen levels in body tissues decrease, the kidneys secrete the hormone erythropoietin. Erythropoietin stimulates the bone marrow to increase the production of red blood cells.
The kidneys regulate ion concentrations in blood plasma by returning some ions to the bloodstream and by excreting excess ions in urine. They control blood pH by adjusting the number of hydrogen ions and bicarbonate ions that are reabsorbed or secreted in urine. The kidneys also reclaim valuable nutrients from the filtrate and return them to systemic circulation.
The urinary system also affects all other body systems, whether directly or indirectly. The table below shows interactions between the urinary system and other body systems
| Body System | Urinary System Interaction | Effects |
| All Systems | Eliminates metabolic wastes· Maintains fluid, electrolyte, and acid-base balances | Controls volume, pH, and composition of body fluids· Homeostasis |
| Cardiovascular | Kidneys increase/decrease reabsorption of water filtered from blood· Cells in kidneys release renin when blood pressure decreases | Helps regulate blood volume and blood pressure· Renin-angiotensin-aldosterone system increases blood pressure |
| Digestive | Kidneys help synthesize calcitriol, the active form of vitamin D synthesized in the liver | Calcitriol is necessary for the absorption of dietary calcium |
| Endocrine | Kidneys help synthesize calcitriol· Kidneys release erythropoietin | Calcitriol is an endocrine hormone that promotes bone reabsorption· Erythropoietin stimulates red blood cell production |
| Integumentary (skin) | Kidneys work with the skin to synthesize calcitriol· Kidneys maintain fluid balance | Calcitriol is necessary for the absorption of dietary calcium· Fluid balance necessary for perspiration |
| Lymphatic/ Immune | Kidneys increase/decrease the reabsorption of water filtered from the blood | Helps regulate the volume of lymph and interstitial fluid |
| Muscular | Kidneys help regulate calcium and phosphate levels in the blood | Calcium and phosphate balance important for muscular contractions |
| Nervous | Kidneys are responsible for gluconeogenesis (a metabolic pathway that results in the formation of glucose from non-carbohydrate substrates such as lactate, glycerol, and certain amino acids) | Glucose is necessary for the production of adenosine triphosphate in neurons |
| Reproductive | The urethra is a dual passageway in males. In pregnant women, the urinary system eliminates wastes for the mother and fetus. | Allows passage and direction of sperm· Eliminates metabolic wastes of the fetus |
| Respiratory | Kidneys work with the lungs to adjust the pH of body fluids | Prevent abnormal function of enzymatic pathways |
| Skeletal | Kidneys help regulate calcium and phosphate levels in the blood | Calcium and phosphates are essential for bone deposition |
Let’s Summarize
The urinary system is one of several excretory systems in the body. The digestive system participates in waste removal in two ways. First, the liver detoxifies some substances. Second, the large intestine eliminates substances through defecation (undigested food, water, carbon dioxide, water, salts, cholesterol, and heat). The respiratory system removes waste through exhalation (carbon dioxide, some heat, and some water vapor). The sweat glands help dispose of excess water, heat, and carbon dioxide.
The kidneys have an endocrine function. Renin is an enzyme secreted by the kidneys that initiates the pathway leading to the production of angiotensin II and the secretion of aldosterone. Erythropoietin is secreted by the kidneys when oxygen levels in the kidney decrease.
The urinary system participates in the homeostasis of other systems in many ways. For the cardiovascular system, the urinary system helps regulate blood volume and blood pressure. For the digestive system, the kidneys produce calcitriol, the functional form of vitamin D necessary for the absorption of dietary calcium. For the endocrine system, calcitriol promotes bone reabsorption. For the integumentary system, the skin and kidneys both play a role in the production of calcitriol. For the lymphatic system, the urinary system helps regulate the volume of lymph and interstitial fluid. For the muscular system, the urinary system helps with calcium and phosphate balance for muscular contractions. For the nervous system, the urinary system is responsible for some gluconeogenesis to ensure the availability of glucose for neuron metabolism. For the reproductive system, the urinary system allows for the passage and direction of sperm in males and eliminates metabolic wastes of the fetus (via the maternal cardiovascular system) For the respiratory system; the urinary system helps maintain acid-base balance. For the skeletal system, the urinary system assists with the maintenance of calcium and phosphate balance which is essential for bone deposition. For all body systems, the urinary system helps with homeostasis by influencing the volume, pH, and composition of body fluids.
*
“Learn By Doing” and “Did I Get This?” Feedback
Learn By Doing 15.1
Which is not a function of the urinary system?
- detoxification
Incorrect. The urinary system filters out toxins; the kidney and the liver are the primary detoxification centers. - maintaining electrolyte homeostasis
Incorrect. Along with the regulation of fluids, the urinary system helps in regulating electrolytes and pH. - digestion of liquids
Correct. It is convenient to think that foods are processed by the digestive system and eliminated as feces and liquids are processed by the urinary system and eliminated as urine. However, many fluids are processed through the digestive system; the urinary system processes fluids from the bloodstream. - regulation of blood pressure
Incorrect. The urinary system is involved with fluid homeostasis which helps regulate blood pressure.
What is the difference between excretion and elimination?
Our Answer: The Urinary system utilizes the process of excretion to rid the body of the nitrogenous waste products of metabolism. It will also rid the body of some unmetabolized drugs through the process of elimination. The digestive system utilizes elimination to rid the body of undigestable materials.
Learn By Doing 15.2
Match the location number on the diagram to the correct name and definition.
 |
# | Name | Definition |
| 2 | Ureters | This is where the nephrons produce urine. | |
| 3 | Urinary bladder | Urine travels from the kidneys by circular contraction and is transported to the bladder through these. | |
| 1 | Kidney | Here is where urine is temporarily contained by internal and
external sphincter muscles. |
|
| 5 | Renal artery and vein | Here is where the entire process ends when urine exits out of the body through this. | |
| 4 | Urethra | The urinary process begins with blood carrying various wastes entering each of the two kidneys through one of these. Filtered blood exits the kidney through one of these. |
When enough urine has been produced in the kidneys, it leaves the through the ureters, and urine is then transported to the bladder. Circular contraction occurs in smooth muscle and is the process of how stored urine moves from the kidneys through the ureters and into the bladder. This process through the smooth muscles is otherwise known as peristalsis. The process of urination is referred to as micturition, and urine is ultimately released through the urethra. This body part connects the bladder to the outside of the body.
|
1 |
2 |
3 |
4 |
5 |
| ureters
kidneys bladder |
ureters
kidneys bladder |
Circular contraction
Circular reflexes Cyclical elongation |
micturition
micturition circular contraction |
urethra
sex organs kidneys |
Learn By Doing 15.3
Why is excretion important in order to achieve osmotic balance?
Our Answer: Excretion allows an organism to rid itself of waste molecules that could be toxic if allowed to accumulate. It also allows the organism to keep the amount of water and dissolved solutes in balance.
Learn By Doing 15.4
Creatinine, Sodium, Urea
- Creatinine: The amount of this in the urine helps to evaluate overall kidney functioning. It also gives an indication of other chemicals in the body such as the amount of protein.
- Sodium: The amount of this in urine is indicative of your level of hydration. A urine test will determine the kidney’s ability to keep or discard excess of this from the urine.
- Urea: The level of this in a urine test reveals a person’s protein balance. In addition, excretion of this in the urine is indicative of overall kidney functioning.
Is urine more or less dense than water?
- less dense
Incorrect. Although urine mixes with water, it is actually more dense from the salts in the urine. - more dense
Correct. Since urine contains electrolytes and other molecules, it is more dense than water. - similar density
Incorrect. Urine and water have similar densities (within 5%), but the density of urine is always greater than or equal to water.
How much volume is urinated per day by a healthy adult?
- 1-2 mL
Incorrect. This is the volume of a teaspoon of water. - 1-2 L
Correct. Healthy and hydrated adults urinate the same volume as a 2L bottle. - 1-2 μL
Incorrect. This is the volume of a single drop of water. - 100-200L
Incorrect. There are only 40 liters of water in the body at any time.
As noted above, the volume of urine can vary. Why would the volume change? (The answer needs to be more complete than simply, “drinking more would change the volume”.)
Our Answer: Despite the volume of liquid varying from day to day, the total volume of fluid within the body typically remains the same. This is due to the body’s fluid homeostasis. Through homeostasis, a person will urinate more when drinking a large amount of fluid. Conversely, when an inadequate amount of fluids are not taken in, the kidneys will produce a small amount of concentrated urine to preserve water. So, through homeostasis, the amount of fluid in the body will remain about the same.
Learn By Doing 15.5
The primary function of the collecting ducts, located in the kidneys, is to:
- Filter plasma, reabsorb what the body would like to keep, and excrete the rest.
Incorrect. The primary role of the nephrons is to filter plasma, reabsorb what the body would like to keep and excrete the rest. The primary function of the collecting ducts, located in the kidneys, is to collect any substance not reabsorbed along the nephrons. - Facilitate the process of urine traveling through the smooth muscles, otherwise known as parasitosis.
Incorrect. Circular contraction occurs through the smooth muscle, is otherwise known as parasitosis, and is responsible for urine traveling to the bladder. The primary function of the collecting ducts, located in the kidneys, is to collect any substance not reabsorbed along the nephrons. - Collect any substance not reabsorbed along the nephrons.
Correct. The primary function of the collecting ducts, located in the kidneys, is to collect any substance not reabsorbed along the nephrons. - Expand the surface area that is available for reabsorbing water and solutes.
Incorrect. Microvilli form a brush border and greatly expand the surface area available for reabsorbing water and solutes. The primary function of the collecting ducts, located in the kidneys, is to collect any substance not reabsorbed along the nephrons.
The part of the kidneys that makes them functional organs is/are called:
- loop of Henle (nephron loop)
Incorrect: Once section of the nephron is the descending limb of the loop of Henle; however, nephrons are a more complete response. - microvilli
Incorrect: Microvilli form a brush border, like the one in the small intestine, and are not the part of the kidneys that makes them functional. - nephrons
Correct: The functional units of the kidneys are called nephrons. - renal tubule
Incorrect: The renal tubule first is part of a greater system that includes the proximal convoluted tubule and includes dense microvilli on their luminal surfaces.
The renal corpuscle is the first site of exchange between the cardiovascular system and the urinary system. Which of the following correctly pairs the structures with the contents of the structure?
- The glomerulus contains cardiovascular capillaries, and the glomerular (Bowman’s) capsule contains the urinary filtrate.
Correct. Each nephron in the kidneys contains a glomerulus, which is a capillary bed where blood is filtered. The glomerular capsule, or Bowman’s capsule, receives the filtrate from the glomerulus. - The glomerular capsule contains cardiovascular capillaries, and the glomerulus contains the urinary filtrate.
Incorrect. The glomerulus is a capillary bed where the blood is filtered. The glomerular capsule receives the filtrate from the glomerulus. - The glomerulus contains both the cardiovascular capillaries and the urinary filtrate.
Incorrect. The glomerulus is a capillary bed where the blood is filtered. The glomerular capsule receives the filtrate from the glomerulus. - The glomerular capsule contains both the cardiovascular capillaries and the urinary filtrate.
Incorrect. The glomerulus is a capillary bed where the blood is filtered. The glomerular capsule receives the filtrate from the glomerulus.
Which of the following is the correct order of tubules after the glomerular capsule?
- proximal convoluted tubule, nephron loop, distal convoluted tubule, collecting duct
- proximal convoluted tubule, distal convoluted tubule, loop of Henle, collecting duct
- loop of Henle, proximal convoluted tubule, distal convoluted tubule, collecting duct
- collecting duct, proximal convoluted tubule, distal convoluted tubule, loop of Henle
Which are not blood vessel structures associated with nephrons?
- glomerulus
- alveolar capillaries (These are found around the alveoli in the lungs.)
- peritubular capillaries
- vasa recta
Learn By Doing 15.6
Production of urine that modifies plasma makeup is the result of ________.
- filtration
- absorption
- secretion
- filtration, absorption, and secretion (All three processes can and do alter the molecular composition of plasma.
Learn By Doing 15.7
To produce urine, nephrons and collecting ducts carry out three basic functions:
One, glomerular filtration is
- the first step in urine production is where water and most of the solutes in blood plasma pass through into the renal tubule.
Correct. Glomerular filtration is the first step in urine production where water and most of the solutes in blood plasma pass through into the renal tubule. - a process where reabsorbed substances are returned to the blood as it travels along the peritubular capillaries and vasa recta.
Incorrect. Tubular reabsorption is a process where reabsorbed substances are returned to the blood as it travels along the peritubular capillaries and vasa recta. - is the additional removal of substances from the blood in the peritubular capillary network or the vasa recta.
Incorrect. Secretion refers to the removal of additional substances from the blood after filtration in the renal corpuscle.
Two, reabsorption is
- when cells of the tubule reabsorb almost all water and solutes from the filtrate as it flows through the renal tubule and collecting duct and returns the fluid and solutes to the blood.
Correct. Reabsorption is when cells of the tubule reabsorb almost all water and solutes from the filtrate as it flows through the peritubular capillaries. - when cells in the renal tubule and collecting duct collect substances (e.g., wastes, drugs, excess ions) from the filtrate as it flows through the tubule and duct.
Incorrect. Secretion is when cells in the renal tubule and collecting duct collect substances (e.g., wastes, drugs, excess ions) from the blood as it flows through the peritubular capillaries. - when water and most of the solutes in blood plasma pass through the wall of glomerular capillaries.
Incorrect. Glomerular filtration is when water and most of the solutes in blood plasma pass through the wall of glomerular capillaries.
Three, secretion occurs
- when cells in the renal tubule and collecting duct remove additional substances from the blood as it flows through the peritubular capillaries or the vasa recta.
Correct. Secretion occurs when cells in the renal tubule and collecting duct remove additional substances from the blood as it flows through the peritubular capillaries. - when water and solutes in blood plasma pass through the wall of glomerular capillaries, first into the glomerular capsule and then into the renal tubule.
Incorrect. Glomerular filtration is when water and solutes in blood plasma pass through the wall of glomerular capillaries, first into the glomerular capsule and then into the renal tubule. - upon the returning of substances to the bloodstream.
Incorrect. Reabsorption is the returning of substances to the bloodstream.
Doctors look for the serum proteins in the urine as a test for kidney damage. Why?
Our Answer: If serum proteins are filtered through the glomerulus that means that the filtration membrane may be damaged. Normally proteins are blocked by size.
Why are most of the substances filtered through the kidneys reabsorbed? Why is urea the one substance that is not reabsorbed to the extent that the others are?
Our Answer: To maintain normal plasma levels, almost every organic nutrient is reabsorbed while urea is the waste product of the urinary system.
Learn By Doing 15.8
Match the terms below to the correct description.
Terms: renal hilum, renal fascia, papillary ducts, renal medulla, nephrons, adipose capsule, renal capsule, renal cortex
| Term | Description |
| nephrons | There are about one million of these functional units in each kidney. |
| renal capsule | This structure preserves the form of the kidney while protecting it from damage due to trauma. |
| renal medulla | The primary purpose of this area, located under the superficial layer of the kidney, is to maintain the proper balance of salt and water in the blood. |
| renal hilum | This is a concave area where the renal artery enters the kidney. |
| papillary ducts | Urine produced by nephrons empties into these. |
| renal fascia | This fastens each kidney to neighboring structures and to the abdominal wall. |
| renal cortex | This superficial layer of the kidney acts as a filter for the blood and so removes metabolic waste. |
| adipose capsule | This fatty tissue surrounds the renal capsule and provides additional protection and helps to anchor the kidney in place. |
Describe the three major regions of the kidney’s internal structure.
Our Answer: Internally, the kidney has three regions—an outer cortex, a medulla in the middle, and the renal pelvis in the region called the hilum of the kidney, which is the concave part of the “bean” shape.
Learn By Doing 15.9
Which renal functions are the ureters involved with?
- Excretion
Incorrect. The exchange with the blood to remove toxins only occurs in the kidney. - Elimination
Correct. Ureters are part of the elimination process since they move urine from the kidneys. - Both
Incorrect. The exchange with the blood to remove toxins only occurs in the kidney. - Neither
Incorrect. We don’t urinate directly from our ureters, but they are necessary for the process of elimination.
What holds the bladder in place?
- the bladder is free to move
Incorrect. Since there are large amounts of blood vessels in the abdomen, it is not a good idea for organs to move around. - folds in the peritoneum
Correct. The urinary bladder is located in the pelvic cavity, just posterior to the pubic symphysis, and is held in place by peritoneal folds. - adipose tissue
Incorrect. Kidneys are cushioned by adipose tissue but not the bladder. - the ureters
Incorrect. This would probably put too much mechanical stress on the ureters.
What are the main differences between the male and female urethras?
- The female urethra is longer and is part of the reproductive system.
Incorrect. The female urethra is shorter and is not part of the reproductive system. - The male urethra is longer and is part of the reproductive system.
Correct. The male urethra is longer and is part of the reproductive system. - The female urethra is longer but is not part of the reproductive system.
Incorrect. The female’s is shorter and is not part of the reproductive system. - The male urethra is longer but is not part of the reproductive system.
Incorrect. Although the male urethra is longer, it is not part of the reproductive system.
Why are women for likely to have a urinary tract infection when compared to men?
- Women’s urethras are longer than those of men; the urethra’s external opening in women is closer to the anus than it is in men.
Incorrect. Women are predisposed to UTIs because their urethras are actually shorter than those of men. In addition, the external opening of the urethra in women is closer to the anus than it is in men. - Women’s urethras are shorter than those of men; the urethra’s external opening in women is closer to the anus than it is in men.
Correct. Women are predisposed to UTIs because their urethras are shorter than those of men. In addition, the external opening of the urethra in women is closer to the anus than it is in men. - Women’s urethras are shorter than those of men; the urethra’s external opening in men is closer to the anus than it is in men.
Incorrect. Women are predisposed to UTIs because their urethras are shorter than those of men. However, the external opening of the urethra in women is closer to the anus than it is in men. - Women and men have an equal chance of having a UTI.
Incorrect. Women are more likely than men to have a UTI.
Learn By Doing 15.10
Kidneys help synthesize calcitriol, an enzyme that is found in the digestive, endocrine, and integumentary systems. Explain how calcitriol benefits the entire body.
- Calcitriol is necessary as it allows for the passage and direction of sperm.
Incorrect. In the urinary system, the urethra in males acts as a dual passageway for urine and sperm. Calcitriol is independent of the reproductive system. - Calcitriol is necessary to help regulate the volume of lymph and interstitial fluid.
Incorrect. Kidneys increase/decrease the reabsorption of water filtered from blood to help regulate the volume of lymph and interstitial fluid. This works in conjunction with the lymphatic/ immune system. - Calcitriol is necessary for the absorption of dietary calcium in the digestive and integumentary systems which promotes bone reabsorption in the endocrine system.
Correct. Calcitriol is necessary for the absorption of dietary calcium in the digestive and integumentary systems which promotes bone reabsorption in the endocrine system. - Calcitriol is necessary to prevent the abnormal function of enzymatic pathways in the respiratory system.
Incorrect. Kidneys work with the lungs to adjust the pH of body fluid which prevents the abnormal function of enzymatic pathways. Calcitriol is independent of the respiratory system.
