Protection from Pathogens
16 Integumentary System
The integumentary system is one of the main protective systems of the human body. It contains your skin, hair, nails, and several glands. Did you know your skin is the largest organ in your body? It makes up approximately 7% of your body weight! The skin is also known as your integument or covering. Have you ever heard the expression that “beauty is only skin deep”? It’s an interesting statement because everything you see in another person’s appearance is dead! The layer of skin and hair that are visible are actually dead epithelial cells!
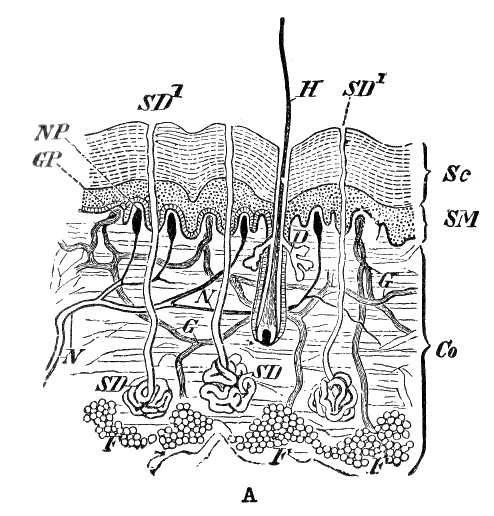
The skin is actually formed from two layers: the superficial epidermis layer, which is composed of epithelial tissue, and the deeper connective tissue layer known as the dermis. The hypodermis is below the dermis and is composed of loose connective tissue. When you give a subcutaneous (or sub-Q) injection, you inject the drug into the hypodermis layer. Subcutaneous means below the cutaneous membrane which is another term for your skin. One medication commonly given via this method is insulin.
Let’s test your knowledge of some common facts and myths about the integumentary system.
Learn By Doing 16.1
Decide whether each of the following statements is a fact or a myth.
- The skin can regenerate.
- A bald person will get colder faster than a person with a full head of hair.
- Shaving makes hair grow back faster.
- Squinting or frowning a lot can form wrinkles.
- Sunlight has some important health benefits.
- Tanning from a tanning bed is less dangerous than sun tanning.
The Integumentary System and Homeostasis
Let’s check out the integumentary system in action in the following case study.
You and your friend, Tori, are baking cookies. It’s the end of the semester, and you both have been craving chocolate chip goodness. While the cookies are in the oven, you and Tori decide to study your anatomy and physiology. You are currently studying the integumentary system. The timer goes off, and Tori jumps up, very excited, grabs a dish towel, and pulls the cookie sheet out of the oven. “OWW!” Tori yells – as she drops the cookie sheet onto the table. “I just burned my hand on the cookie sheet”.
You reply, “Quick, rinse it under cold water; I think that is supposed to stop the burn.”
“It really hurts!” Tori exclaims while running her hand under the cool water from the faucet.
“Let me see your hand,” you tell Tori.
When she shows you, you notice a couple of blisters beginning to form on her fingers and palm. “I think you burned through your epidermis layer and maybe to the dermis. Don’t blisters mean you have a second-degree burn?” you ask her.
“What does that mean?” Tori asks. “Should I go to that prompt care place?”
“Let’s look it up; I think if you keep it clean, you will be ok. There are several layers of cells in the epidermis, aren’t there?” you ask. “Our textbook says if the skin blisters it is a sign of a second-degree burn. These burns don’t typically damage the lower layer, the dermis.”
“It’s a good thing it didn’t burn through the dermis; then I would be more prone to other infections, wouldn’t I? Didn’t we read about the skin protecting us from microbes around us?” Tori asks.
The integumentary system is vital for our body’s homeostasis. As we saw with Tori, the skin is an important barrier for protection. If the skin is damaged from a burn or torn, it opens up an entry point for microbes to enter our body. This is why we always wear protective gloves when handling body fluids. The gloves protect us in case there are any openings in our skin. It’s better to be extra cautious about this. Our epidermis is multi-layered to make it better suited for protection. If Tori’s burn had penetrated deeper, it also would have increased fluid loss and dehydration. The skin functions as a cover to keep interstitial fluids inside rather than seeping out. Every day we lose a small amount of water through our skin and our lungs from breathing. This water loss is termed insensible perspiration and is accelerated when in dry air. Our cells in the epidermis produce a protein known as keratin that helps to decrease water loss from our skin. If skin becomes dry, it cracks and creates an opening in our defenses. When you think of maintaining homeostasis, protection is probably one of the first processes you think of, and the skin is vital for this.
The integumentary system is also crucial for body temperature regulation. When we are too warm, blood vessels going to the skin open up (vasodilate) and more blood flows to the surface of the skin to release heat to cool the body. Our skin turns pink or red when this happens. If body temperature continues to rise, our sweat glands become active, and we sweat to cool off (this is termed sensible perspiration). When we are cold, the blood vessels shrink (vasoconstrict) to decrease blood flow and consequently heat loss from our skin. Our skin might turn blue from the decrease in blood flow. We also have a layer of body hair covering our body which insulates and helps us retain heat. It’s a good idea to wear a hat when in cold weather to reduce heat loss from our heads!
Another function of the skin isn’t commonly known. The skin produces vitamin D in response to sunlight or UV radiation. Vitamin D is a very important vitamin; it’s crucial for calcium absorption from our food and has recently been shown to have anti-cancer properties. If our vitamin D levels fall, this could impact our skeletal system by decreasing the absorption of calcium and consequently the amount that gets to our bones.
Our skin is also tied to our nervous system. One of our main senses – touch– is dependent on numerous receptors located in our skin. We can feel and process information regarding pressure, temperature, light touch, and pain through our skin. If Tori didn’t feel pain when she touched the hot cookie sheet, she wouldn’t have dropped it to reduce the damage from the heat. Clearly, the integumentary system is more involved in our functioning than clear skin and gorgeous hair!
Learn By Doing 16.2
Tori mentions that the skin protects us from microbes; how do you think it accomplishes this?
Hint: The skin is a very complex organ that is critical for protection and for survival.
- The skin is a covering that keeps things out of our bodies.
- The skin secretes chemicals such as sweat and oils that form an antiseptic layer.
- The skin protects us from dehydration and drying out.
- All of the above are ways the skin protects us.
Now that you’ve read a little more about the integumentary system and Tori, what do you think are the main concerns from a burn?
Hint: think about the functions of the skin as outlined above.
- In severe burns, the body is more susceptible to invasion from microbes and might dehydrate faster from fluid loss.
- The loss of sense of touch and areas vital for the formation of vitamin D from a burn.
- The skin might not be repaired, and the area will be a weak spot for infection.
Components of the Integumentary System
The integumentary system is composed not only of the skin but also nails, glands, and hair. The most numerous component of the integumentary system is the integument or skin. The skin contains the superficial epidermis, which consists of epithelial tissue, and the deeper dermis which is formed from dense irregular connective tissue. The epidermis contains nerve endings for pain, which is why Tori felt the pain of the burn. The epidermis is avascular, which means it doesn’t have blood capillaries. Nutrients get to the epidermis from the vascular dermal layer. Only those cells closest to the dermis are able to receive the nutrients, and these cells have rapid rates of cell division. The cells in the epidermis migrate to the surface and then are shed daily. They are constantly being replaced by the cells deeper. The dermis contains blood vessels, sweat, and oil glands. The dermis also has receptors for touch. Below the dermis is the hypodermis layer. This is the fatty layer that anchors the skin to your body. The hypodermis is technically not part of the integumentary system.
The skin also contains sweat (sudoriferous) and oil (sebaceous) glands. Sweat glands release perspiration to cool us when we overheat. Sweat is mostly water but also contains electrolytes and a waste product known as urea. Urea is one of the main components of urine too! Sebaceous glands produce oil, otherwise known as sebum. Sebum and sweat form a chemical barrier on our skin to decrease bacterial growth on our skin.
Hair and nails are additional structures associated with the integumentary system. Body hair takes up space to compete with pathogens for space on our skin. Body hair also insulates us. Did you know that there are approximately 100,000 hairs on your head and 30,000 in a man’s beard? Fingernails and toenails provide leverage and protection when we grab and manipulate objects.
The epidermis contains the pigment melanin, which protects our cells from UV radiation. Melanin is also responsible for our hair, skin, and eye color. Keratin was previously mentioned and is important for decreasing water loss from our skin. Many skin lotions contain keratin to prevent dry skin. Another important protein is collagen. Collagen provides strength to our skin. Collagen has a white appearance and often when the skin heals extra collagen is placed at the site. Sometimes this results in a white scar.
When you study the integumentary system, you will learn about the chemical and cellular components which work together to maintain the integrity of the system. As consumers, we spend a lot of money on products meant to make our skin and hair look better, younger, and healthier. As you read through this topic, think about whether those products really can make a difference or if they are just the result of well-played marketing campaigns!
Learn By Doing 16.3
The dermis layer is the most superficial layer of the skin.
- True
- False
Which of the following is not part of the integumentary system?
Hint: This question is a little tricky, but only one structure below is not technically part of the integumentary system.
- sebaceous glands
- hair
- hypodermis
- dermis
Which direction is the epidermis from the rest of the body?
Hint: The epidermis is “outside” the entirety of the body.
- ventral
- dorsal
- superficial
- deep
Anatomy of the Integumentary System
Learning Objective
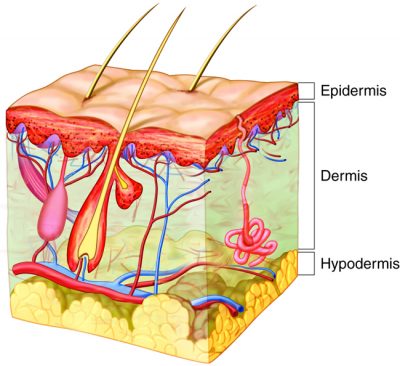
The skin is made up of two mutually dependent layers that are distinguished based on their structure and location. These layers – the epidermis and the dermis – contain a variety of structures, including blood vessels, hair follicles, and sweat glands. Beneath the dermis lies the hypodermis (subcutis). It is composed mainly of fatty tissue.
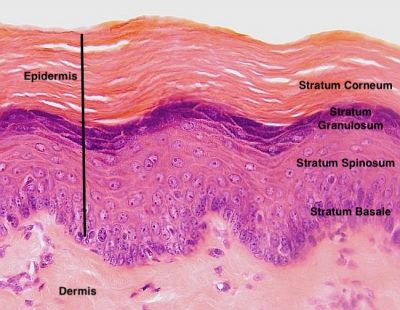
The most superficial layer, the epidermis, is composed of stratified squamous epithelia that are keratinized at the outermost surface, melanocytes, immune cells (Langerhans that modulate immune response), and sensory receptors (Merkel cells that detect light touch). The function of the epidermis layer is “protection.” The keratinocytes and immune cells help protect the skin.
The dermis lies beneath the epidermis and is composed of two layers of connective tissue: a loose layer (papillary) and a dense irregular layer (reticular). Both layers of the dermis contain connective tissue components (collagen, elastin, fibroblasts), plus blood vessels, sensory receptors, and lymphatics. The dermis is a “functional” layer. The dermis is a connective tissue that can stretch and retract because of the strong and elastic extracellular matrix. The dermis also contains nerves.
Beneath these two layers lies the hypodermis, composed of loose connective tissue (adipose and areolar). The hypodermis is the “connection” layer. It connects the integument (epidermis and dermis) to organs and muscles in the body. This layer contains adipose tissue and connective tissue as well as blood vessels, nerves, and immune cells.
Integumentary Levels of Organization
Learning Objective
The levels of organization of the skin and its accessory structures are listed below. You will be exploring these further in the coming pages.
- Molecular level – keratin, melanin, and vitamin D
- Microscopic level – stem cells and skin cells
- Tissue level – epithelial and connective tissue
- Organ level – skin, consisting of the epidermis, dermis, and hypodermis, as well as hair, nails, and glands
Molecular Level
Learning Objectives
Describe how the structure of keratins provides strength to integumentary tissues.
Describe the function of melanin and discuss the consequences of reduced melanin.
Describe the production and function of vitamin D and discuss the consequences of reduced vitamin D.
Keratin
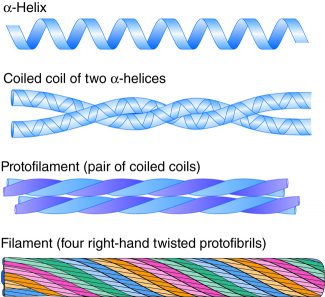
Keratin is a group of fibrous proteins that give hair, nails, and skin their tough, water-resistant properties. In addition to intra- and intermolecular hydrogen bonds, keratins have large amounts of the sulfur-containing amino acid cysteine, which forms disulfide bridges that confer additional strength.
Keratins are an excellent example of protein assembly. Keratins have an alpha-helix secondary structure in the central rod domain. Two keratin proteins then come together, and the helices wind around themselves to form a quaternary structure of a coiled-coil dimer. These dimers then assemble into protofilaments and then filaments. The twists of twists are similar to the fibers inside ropes. However, keratins aren’t twisted by machines; they self-assemble based on their primary structure.
Melanin
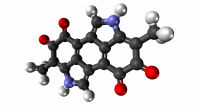
(Credit: Mhotep, CC BY SA)
Melanin is a class of photopigment (“photo,” meaning “light,” and “pigment,” meaning “colored material”) with a molecular structure that allows it to absorb UV (ultraviolet) radiation from the sun. Melanocytes insert granules of melanin into specialized vesicles called melanosomes. These are then transferred into keratinocytes. The melanosomes then accumulate around the nucleus. Melanin transforms the energy from the radiation into harmless heat, and melanin prevents the indirect DNA damage from the sun that is responsible for many skin cancers. Melanin also gives skin, hair, and eyes their color. Melanin is produced by specialty cells called melanocytes inside special vesicles called melanosomes. About 10 days after initial sun exposure, melanin synthesis peaks, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially.
Example: Albinism
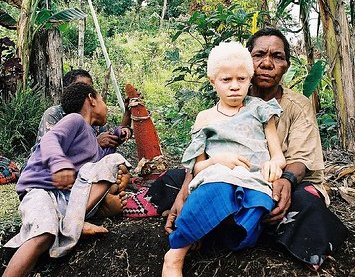
Albinism is a genetic disorder that affects (completely or partially) the coloring of skin, hair, and eyes. The defect is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Melanin protects the DNA of skin cells from the harmful effects of UV rays from the sun. Individuals with albinism need more protection from the sun and must limit their outdoor activities. Treatment of this disorder usually involves addressing the symptoms.
Vitamin D
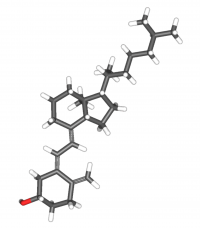
The epidermal layer of human skin synthesizes the precursor to vitamin D when exposed to UV radiation. In the presence of sunlight, a precursor to vitamin D3 is synthesized from cholesterol in the skin. The liver converts this molecule to calcitriol (the active chemical form of the vitamin) in the kidneys. Vitamin D, which is really a hormone, is essential for the normal absorption of calcium and phosphorous, which are required for healthy bones. In the present day, this hormone is added as a supplement to many foods including milk and orange juice, compensating for the need for sun exposure.
In addition to affecting bone health, Vitamin D is essential for general immunity against bacterial, viral, and fungal infections. Recent studies are also finding a link between insufficient vitamin D and cancer.
Example: Rickets
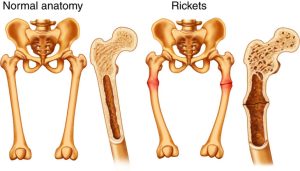 Rickets is a disease of bone deterioration often caused by insufficient vitamin D, leading to insufficient calcium absorption. Children are especially prone to the effects of this vitamin deficiency due to their rapid bone turnover and formation. In adults, the deficiency of vitamin D is called osteomalacia. Typically, rickets is found in developing countries where malnutrition would prevent a proper supply of calcium and dietary vitamin D.
Rickets is a disease of bone deterioration often caused by insufficient vitamin D, leading to insufficient calcium absorption. Children are especially prone to the effects of this vitamin deficiency due to their rapid bone turnover and formation. In adults, the deficiency of vitamin D is called osteomalacia. Typically, rickets is found in developing countries where malnutrition would prevent a proper supply of calcium and dietary vitamin D.Learn By Doing 16.4
How does the structure of keratin create the hard, waterproofing quality of nails, hair, and skin?
- By adding strength with vitamin D.
- By polymerization of intermediate filament proteins.
- By adding strength with dialanine bridges.
- By polymerization of collagen fibers.
Recently, reports in the United States and Europe have shown vitamin D deficiencies and rickets-like symptoms in children. Why?
Hint: Vitamin D is synthesized by the skin when it is exposed to UV light, and a small amount is provided through diet.
- childhood vaccinations
- lack of exercise
- too much time indoors and strong sunscreen
- poor nutrition in children
What disease are people with albinism prone to?
Hints: Albinism is caused by a lack of melanin production. Consider the purpose of melanin.
- acne
- keratosis
- skin
- cancer
- rashes
Microscopic Level – Cells of the Epidermis
Learning Objectives
- Identify the cells of the epidermis based on their location and anatomic structure (stem cells of the stratum basale, keratinocytes, melanocytes, Langerhans cells, Merkel cells).
- Describe the complementary functioning of the cells of the epidermis.
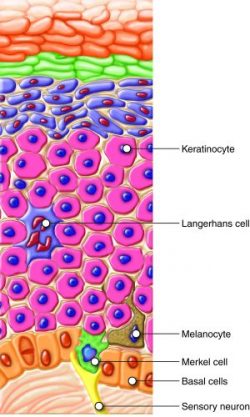
The epidermis (or epithelial layer) is stratified squamous epithelia, composed of four to five layers (depending on body region) of epithelial cells. The top layers of the epidermis are made up of keratinocytes, which are cells containing the protein keratin. The keratinocytes on the most superficial layer of the epidermis are dead and periodically slough away, being replaced by cells from the deeper layers. As keratinocytes move superficially from the deeper layers, they lose cytoplasm and become flattened, allowing for many layers in a relatively small space.
Basal cells are an example of tissue-specific stem cells, meaning they can turn into a variety of cell types found in that tissue. Under normal conditions, daughter basal cells most commonly replace lost keratinocytes.
The deepest layer of the epidermis and the most superficial layer of the dermis give out projections that interlock with each other (like Velcro) and strengthen the bond between the epidermis and the dermis. The projections originating in epithelial cells of the bottom layer of the epidermis are called desmosomes, and the ones originating in the dermis are called dermal papillae. Think of the projections as a formation of folds of cellular matter. The greater the fold, the stronger the connections made.
Merkel cells are sensory receptors that detect light touch. They form synaptic connections with sensory nerves that carry touch information to the brain. These cells are abundant on the surface of the hands and feet.
Melanocytes are cells in the bottom layer of the epidermis that produce the pigment melanin, which gives hair and skin their color. Individuals whose melanocytes produce more melanin have a darker skin color. Cellular extensions of the melanocytes reach up in between the keratinocytes.
Dendritic (Langerhans) cells are tissue macrophages that contribute to the immune function of the skin. They engulf foreign organisms and signal to the immune system. Since the skin is in constant contact with the environment, it is important to have immune cells to help destroy any pathogens that might get past the cell barrier of the epidermis.
Example: Eczema
Learn By Doing 16.5
Some studies report that children who are raised in “overly clean” homes are more likely to develop eczema. What might explain this? Submit your answer and compare it with the answer given.
Which of the following is not matched with its proper description?
- Keratinocytes are found in the upper level of the skin and are usually dead.
- Merkel cells sense deep pressure.
- Basal cells are stem cells that can reproduce.
- Langerhans cells engulf bacteria.
Tissues of the Integumentary System
Learning Objectives
- Identify the tissue type making up the epidermis.
- Identify the cells of the epidermis, dermis, and hypodermis.
Epithelial Tissue
The skin contains many tissue types. The epidermis is classified as epithelial tissue composed of stratified squamous epithelia. The dermis is made of different types of connective tissues including areolar and dense irregular connective tissue and histiocytes (tissue macrophages). The hypodermis contains areolar connective tissue, adipose tissue, and glands.
The epidermis is mainly made up of stratified (layered) squamous (flat) epithelial cells. Epithelial cells found in the different layers of the epidermis have different shapes. Stratification (layering) is important in the epithelial tissue of the integumentary system, which forms a barrier. Epithelial cells found in other systems have other surface cell shapes, including cube-like (cuboid) and column-like (columnar) in a single layer (simple) or multiple cell layers (stratified).
The epidermis contains several cell types of different origins, including keratinocytes (95 percent of the cells are keratinocytes), melanocytes, Langerhans cells, and Merkel cells. The epidermis does not contain blood vessels or nerves, but Merkel cells provide signals to the sensory neurons below this layer in the dermis. Since there are no blood vessels, living cells of the epidermis are nourished by diffusion from the capillaries of the dermal papillae below.
Learn By Doing 16.6
Which of the following is not a cell found in the epidermis?
- Epithelial cells
- Fibroblasts
- Melanocytes
- Keratinocytes
If epithelial tissue has more than a single layer of cells, it is called ____.
- stratified
- pseudostratified
- complex
- simple
Connective Tissue
Learning Objective
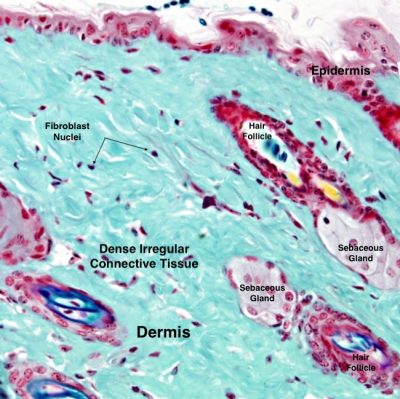
(Credit: Atlas of Animal and Plant Histology, University of Vigo, Spain, CC BY NC SA)
While the epidermis is composed of epithelial cells, the dermis is composed of connective tissue. The dermis connects the epidermis to the hypodermis and provides structure and elasticity from collagen and elastin fibers. These proteins are made by fibroblasts found in the dermis. Collagen and elastin work together: collagens provide strength; elastins, as the name implies, are elastic and allow for distension. The skin must remain strong to protect you from abrasions and other cuts. However, the skin also needs to be able to deform and, hopefully, return to its original shape.
Wrinkles
The permanent folds in the skin caused by a lack of “retraction” are called wrinkles. Wrinkling in the skin is caused by habitual facial expressions, aging, sun damage, smoking, poor hydration, and various other factors. Wrinkling is a surprisingly complex phenomenon. Primarily, sun or other damage to the skin causes a breakdown in collagen and elastin as well as a breakdown in the replacement of these extracellular matrix proteins in the dermis.
Stretch marks
Stretch marks usually accompany rapid weight gain during puberty and pregnancy as well as during the rapid gain of muscle associated with weight lifting. When the dermis (and possibly the hypodermis) is stretched beyond its limits of elasticity, the skin stretches to accommodate the excess pressure. In some cases, the dermis can’t adequately fill in over the stretched areas and may actually tear, causing the epidermis to become thin and making the underlying blood vessels more visible. They initially have a reddish hue but lighten over time as the tissue repairs itself and heals. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen.
Learn By Doing 16.7
The majority of the dermis is composed of:
- Dense irregular fibrous connective tissue
- Stratified squamous epithelium
- Adipose tissue
One cosmetic treatment for wrinkles is Botox. This neurotoxin helps temporarily remove wrinkles caused by repetitive motion, such as crow’s feet. Which of the following explains why this treatment is only temporary and why it cannot fix other types of wrinkles?
Hint: Botox only temporarily immobilizes underlying muscles.
- Botox can decrease the tension of underlying muscles but not repair the damaged extracellular matrix proteins.
- Botox can signal to the muscles to stretch the epidermis back out.
- Botox can reduce the damage by increasing the production of collagen.
- Botox can signal the fibroblast to secrete more extracellular matrix, replacing the damaged fibers.
Why is the combination of elastin and collagen important to the function of the skin?
- Collagen: coloration; elastin: immune response
- Collagen: protection; elastin: distention
- Collagen: distension; elastin: protection
- Collagen: connection; elastin: coloration
Pigmentation of the Skin
Learning Objectives
- Describe the role of melanocytes in producing skin pigmentation and also protecting dividing cells from UV damage.
- Describe the functions of melanocytes.
- Describe sunscreen and UVA and UVB radiation.
Skin contains different types of melanin, including pheomelanin, which is reddish, and eumelanin, which is dark brown. The amount and types of melanin produced are under genetic control. The combinations of the different types of melanin result in the wide range of skin colors and tones seen in humans. While the number of melanocytes does not vary too much between individuals, the skin tone depends on the amount and type of melanin produced by these cells. If a person has more eumelanin-producing melanocytes, that person would have a darker skin color. The predominance of pheomelanin is responsible for the reddish coloration of hair in some individuals.
Exposure to the sun causes melanin to build up because sun exposure stimulates keratinocytes to secrete a peptide hormone that in turn stimulates melanocytes into producing melanin. The melanocytes produce and then transfer the melanin to keratinocytes. This buildup of melanin results in the darkening of the skin or a tan. Increased melanin also protects the skin’s DNA from UV ray damage to some extent, although even very dark-skinned individuals can get skin cancer. Melanin synthesis does not peak until about 10 days after initial sun exposure, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Individuals with darker skin can also get sunburns but are more protected than light-pigmented individuals.
Melanosomes, the cellular organelles that contain melanin, are temporary structures and are eventually destroyed by fusion with lysosomes, which makes tanning impermanent. Too much sun exposure can eventually lead to wrinkling of the skin due to the destruction of the cellular structure of the skin, and in severe cases, it can cause sufficient DNA damage to result in skin cancer. An uneven distribution of melanocytes in the skin results in the appearance of freckles.
Sunscreen and UVA and UVB Radiation
“UV” is an abbreviation for “ultraviolet.” Ultraviolet radiation is a portion of the electromagnetic spectrum between visible light and x-rays. The sun emits two ranges of ultraviolet light that penetrate the earth’s atmosphere: UVA and UVB. The ozone layer partially absorbs UVB radiation, but some still reaches the surface of the Earth. UVA radiation is not filtered, and all of it reaches the surface of the Earth. One of the functions of our integumentary system is to protect us from this UV radiation. Exposure to this radiation can cause skin damage and cancer. Sunscreens are designed to protect our skin from UV radiation. Sunscreens with a sun protection factor (SPF) of 15 or more provide good protection from UVB radiation. To be protected from UVA radiation, you must have a “broad-spectrum” product.
Learn By Doing 16.8
In a person with the genetic disease albinism, the eyes are red. This red color is a result of what?
Hint: Eye color is determined by the same chemical that determines skin color.
- The melanosomes fusing too soon with the lysosomes.
- Too little melanin being produced and the blood vessels showing through.
- An uneven distribution of the melanocytes.
- Too much pheomelanin being produced and giving a reddish tint.
Some people see freckles appear on their noses and cheeks during the summertime and fade during the winter. What would cause this?
- A lower amount of melanin being transferred to the keratinocytes in response to UV radiation.
- Uneven distribution of melanocytes reacting to UV radiation
- Uneven production of melanin in response to temperature
- Freckles cannot just appear during the summer and fade during the winter.
Organ Level
Learning Objective
- Explain why the histology of the epidermis is well-suited for its functions.
- Identify and describe the layers of the epidermis, indicating which are found in thin skin and which are found in thick skin.
- Describe the two different layers of the dermis.
- Explain why the histology of the dermis is well-suited for its functions.
- Identify and describe the subcutaneous tissue, including the tissue types making up subcutaneous tissue.
- Explain why the histology of the subcutaneous layer is well-suited for its functions.
- Describe how the distribution of adipose tissue differs based on gender, age, diet, and exercise.
The skin, the integumentary system’s organ, is composed of the epidermis (epithelial tissue) and dermis (connective tissues), with an underlying hypodermis that is technically not part of the skin organ. Several layers of keratinocytes at the surface form the epidermis. The topmost layer is dead and sheds continuously. It is progressively replaced by stem cells that divide in the basal layer (stratum basale). The dermis connects the epidermis to the hypodermis and provides strength and elasticity due to the presence of collagen and elastin fibers. The hypodermis is the name for the layer of connective tissue that connects the dermis to the underlying organs. It also harbors adipose tissue for fat storage. Let’s look at the structure and function of these parts of the skin organ in detail.
Epidermis
The epidermis (or epithelial layer) is made up of four or five distinct layers (strata), depending on the region of the body. From deep to superficial, they are named the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The stratum lucidum is unique to areas like the palms of the hand (palmar surfaces) and soles of the feet (plantar surfaces), where the skin is thicker than it is in the rest of the body. The stratum basale is made up of the many cell types already discussed, including basal cells, melanocytes, Langerhans cells, and Merkel cells. As you look at the more superficial layers, you see that they become mostly (or completely) composed of keratinocytes, which protect and waterproof the body. As the cells are pushed superficially (toward the surface), they make keratin. As the cells begin to fill with keratin, they become increasingly impervious to water, and it becomes more difficult for osmosis and diffusion to occur inside the cell. In addition, as cells enter each superficial layer (further away from the dermis, which contains the blood supply), the distance across which oxygen and other nutrients must diffuse increases, making it harder for the cells to get the nutrients they need. The keratinocytes in the stratum corneum (the most superficial layer) are usually inert or dead, and periodically slough away, being replaced by cells from the deeper layers.
Example: Exfoliation
Thick Versus Thin Skin
The thickness of thick skin is a function of the upper layers of the epidermis. The uppermost layer of the epidermis called the stratum corneum (stratum = layer, corneum = horny), consisting of keratin-packed dead cells, is substantially thicker in thick skin than in thin skin (more than 300 layers versus 15 layers of cells). The palms of your hands, soles of your feet, and your lips have thick skin. Thick skin is adapted to specialized activities, including gripping, walking, and suckling, and the wear and tear that goes with those activities. Thick skin does not have hair and has few glands.
Most of the rest of your skin is thin. The packed keratin provides most of the protective properties associated with the epidermis. Whereas the stratum corneum of thin skin may be completely shed and replaced in about a week, this replacement may take about a month in thick skin.
Example: Calluses
Dermis
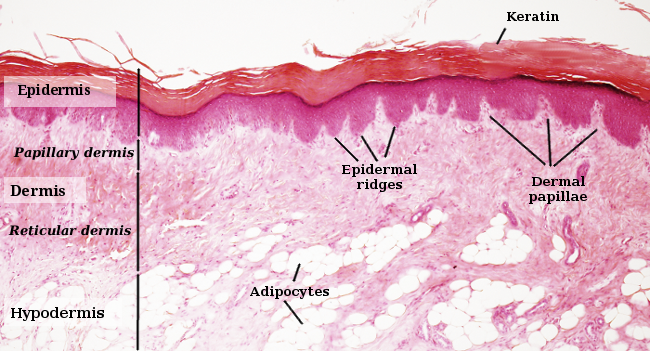
The skin’s dermis is made up of two distinct layers of connective tissue. The papillary layer is made up of loose connective tissue, and the underlying reticular layer is composed of dense irregular connective tissue. This dermal part of the skin (organ) is vasculated (has blood vessels) and innervated (has nerves). As described earlier, the dermis is sparsely populated with fibroblasts that produce collagen and elastin fibers in the extracellular matrix. This leads to a strong and elastic tissue structure. The matrix can also contain mast cells involved in allergic reactions.
Papillary Layer
The fibroblasts are dispersed within the collagen and elastin fibers of the loose connective tissue of the papillary layer. This forms a loose mat, which contains an abundance of small blood vessels. The dermal papillae with blood capillaries interdigitate (become interlocked) with the epidermal ridges of the stratum basale. In addition, the papillary layer contains phagocytes — defensive cells that help fight bacteria or other infections that have breached the skin. This layer is also interspersed with lymph vessels and sensory receptors.
Reticular Layer
The reticular layer appears “reticulated” (net-like) because it is composed of a mesh of collagen fibers and elastin fibers. Fibrocytes form the bundles of collagen that extend into the papillary layer and the hypodermis, making these layers hard to distinguish. The flexible collagen provides structure and strength, while elastin lends limited elasticity to the skin. Collagen also binds with water, keeping the skin hydrated. Water is necessary to maintain the normal elasticity and resiliency (called “turgor”) of the skin. Dehydration causes a loss of turgor; if the skin of a dehydrated person is pinched, it remains domed and does not immediately flatten out.
Collagen injections and Retin-A creams help restore skin turgor by introducing collagen externally in the former case or by stimulating blood flow and repair of the dermis in the latter case.
Hypodermis
The hypodermis (also called the subcutis or subcutaneous layer) functions to connect the integument (epidermis and dermis) to the underlying muscles and organs. The hypodermis is not considered part of the skin but has several important functions. Like the dermis, the hypodermis is made up of loose connective tissue, collagen, and elastic fibers, providing it with some elasticity. Additionally, it contains adipose tissue, which functions as a mode of fat storage. The hypodermis is vascular and contains arteries, veins, and blood capillaries.
Adipose tissue present in the hypodermis accumulates fat, which serves as an energy reserve, insulates the body, and prevents heat loss. The fat distribution changes as our bodies mature and age. It is also hormone-dependent. Men tend to accumulate fat in different areas (neck, arms, lower back, and abdomen) than women (breasts, hips, thighs, and buttocks). Physical inactivity due to a lack of exercise and sedentary jobs, combined with the consumption of high-calorie foods, has resulted in the highest rates of obesity ever seen in our country. While the accumulation of fat provided an evolutionary advantage to our ancestors, who experienced unpredictable bouts of famine, it is now considered a major health threat. Improved diet and increased exercise are the best ways to control body fat accumulation, especially when it gets to levels that increase the risk of heart disease.
Learn By Doing 16.9
Which of the following connects the epidermis to the dermis?
Hint: The dermis is connected to the epidermis by the basal layer of the epidermis.
- Stratum Basale
- Stratum Corneum
- Stratum Granulosum
- Stratum Spinosum
The stratum corneum consists of layers of dead cells. How can these dead cells help protect the living cells underneath?
- They allow for osmosis to occur easily.
- .They secrete antimicrobial oils.
- They allow diffusion to occur easily.
- They are resistant to water penetration.

Fingerprints are created by a combination of “friction ridges” of the human finger. These friction ridges create patterns that are unique to every individual. The interaction of the epidermis with a layer of the dermis creates these ridges. Which layer of the dermis do you think creates fingerprints?
Hint: Which layer is just deep to the epidermis?
- reticular layer
- papillary layer
What is the advantage of not having oil on regions of thick skin including the hands? Submit your answer and compare it with the answer given.
The net-like mesh of collagen fibers in the reticular layer adds to the resilience of the dermis because of what?
- The net-like mesh of collagen binds and holds water.
- Collagen fibers secrete elastin.
- The net-like mesh of collagen fibers stores fat, which holds water.
- The collagen fibers form a loose mat that contains blood vessels and phagocytes.
One of the functions of the subcutaneous level or hypodermis is to provide insulation for the body. What structure allows the hypodermis to perform this function?
- adipose tissue
- elastic fibers
- collagen fibers
Accessory Organs
Learning Objectives
- Describe the structure and roles of the accessory structures of the integumentary system.
- Describe the structure of hair and of a hair follicle.
- Describe four functions of hair.
- Describe the three stages of hair growth.
- Explain common causes of hair loss.
- Describe the structure and function of fingernails and toenails.
- Contrast the structure and function of eccrine (merocrine) glands, apocrine glands, and sebaceous glands.
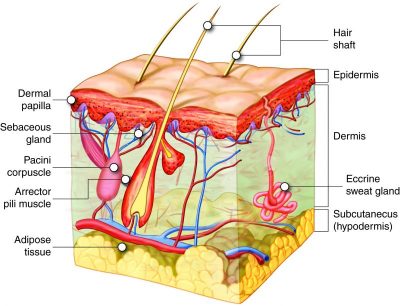
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. Although these structures appear to be part of the dermis, they are actually derived from the epidermis. The hair shaft is made of dead, keratinized cells and gets its color from melanin pigments. Nails are also keratinized and protect the extremities of our fingers and toes from mechanical damage. Sweat glands and sebaceous glands produce sweat and sebum, respectively. Each of these fluids has a role to play in maintaining homeostasis. Sweat helps the body remove excess fluids and electrolyte wastes and also cools down the body’s surface when it gets overheated. Sebum acts as a natural moisturizer of the dead, flaky outer keratin layer of skin and hair. Sebum is also known for its microbicidal and microbiostatic properties.
Hair
Hair is part of the integumentary system. Strands of hair originate from the base of the downward extension of living epithelial cells into the dermis which is called the hair follicle. The dermis surrounds hair follicles, but their cells are part of the epidermis and are separated from the dermis by a basal lamina layer. Hair forms in a manner similar to the skin: rapid division and differentiation of stem cells into keratinocytes that get pushed up and become flattened, dead keratinized cells. The part of the hair that is exposed on the skin surface is called the hair shaft, and the rest of the follicle is called the hair root. The bulge at the base of the hair root is called the hair bulb. The hair bulb surrounds the hair papilla (made up of connective tissue, blood capillaries, and nerve endings).
Just as the layers of the skin form on the inner layers and get pushed out to the surface as the dead skin on the surface sheds, basal cells in the center of the hair bulb divide to form layers of keratinocytes that form the medulla, cortex, and cuticle of the hair bulb. These layers are visible in a longitudinal section of the hair follicle. Keratin formation starts in the cells of the medulla, and the keratin continues to be produced in the cortex and cuticle. Keratinization is completed as the cells are pushed to the skin surface to form the shaft of hair that is externally visible. The external hair is composed entirely of keratin.
Hair serves a variety of functions. For example, hair on the head protects it from the sun and from heat loss; and hair in the nose and ears and around the eyes (eyelashes) defends the body by trapping dust particles that may contain allergens and microbes. Hair on the eyebrows prevents sweat and other particles from bothering the eyes. Hair also has a sensory function due to the innervation of the hair papilla. Hair is extremely sensitive to changes in the environment, much more so than the skin surface. The hair root is connected to smooth muscles called arrector pili that contract in response to stimuli, making the external hair shaft “stand up.” This is visible in humans as goose bumps and even more obvious in animals, such as when a frightened cat’s fur puffs out. In many animals, the puffing out makes the animal appear larger and could possibly enable it to scare off a predator. Another advantage of this ability to cause the hair to stand up is that it can trap air and can act as an insulator, decreasing heat loss.
Just like the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair matrix. Different hair color results from differences in the type of melanin, which is genetically determined. As a person ages, melanin production decreases, and hair tends to lose its color, becoming gray and/or white.
Example: Alopecia
Many individuals can experience hair thinning and/or loss with advanced age. This is called alopecia. This can lead to complete hair loss, called baldness. Most baldness is caused by a genetic sensitivity of hair follicles to the androgen hormone dihydrotestosterone (DHT). DHT causes the hair follicle to receive less blood flow so that the hair follicle begins to atrophy and any hair that is produced is thin.
A common form of baldness is male pattern baldness, which results from a mutation on the X chromosome. It is seen more often in men because men only receive one copy of the X chromosome. Many women may be carriers of this trait, having one normal X chromosome and one X chromosome that has the male pattern baldness gene. Women usually do not exhibit the balding patterns seen in men.
Nails
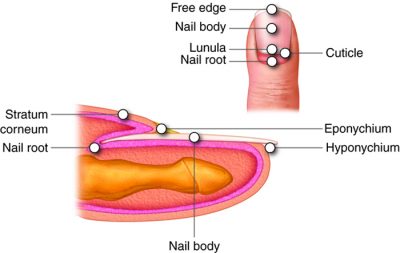
The nail is a specialized structure of the epidermis that occurs at the tips of our fingers and toes. The nail body is formed on the nail bed, and it is designed to protect the tips of our fingers and toes, as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress. The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root. Lateral nail folds, folds of skin that overlap the nail on its side, help anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium. The nail bed is rich in blood vessels, making it appear pink, except at the base, where there is a crescent-shaped region called the lunula. The nail body is composed of keratin-rich, densely packed dead keratinocytes. The area beneath the free edge of the nail, where debris gets lodged, is called the hyponychium.
Sweat (Sudoriferous Glands)
When the body becomes overheated, sweat is produced to cool the body’s temperature and prevent overheating. There are two types of sweat glands responsible for excreting sweat — eccrine (sometimes called merocrine) sweat glands and apocrine sweat glands. Eccrine glands are present throughout the skin surface, especially on the palms of the hand, the soles of the feet, and the forehead. Like hair and nails, they are derived from the epidermis. They are coiled glands that lie in the dermis, with the duct opening to a pore on the skin surface, where the sweat is released (although some may open into hair follicles, like sebaceous glands). The sweat released by eccrine sweat glands is mostly water, with some salt, antibodies, traces of metabolic waste, and a microbe-killing compound called dermcidin. The main function of eccrine sweat glands is to help regulate body temperature through evaporation.
The sympathetic division of the autonomic nervous system controls eccrine glands. The sympathetic division is known as the “fight or flight” division. When you are nervous, you might notice that your palms sweat. This is because when the sympathetic division is activated, it triggers sweating.
Apocrine glands are usually associated with hair follicles and are activated in densely hairy areas like armpits and genitals. They are larger than merocrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis. They release a thicker fluid due to a higher concentration of fatty acids, which may give it a whitish color. These fats are often decomposed by bacteria on the skin, resulting in an unpleasant odor, commonly called body odor. Apocrine glands do not begin to function until puberty. Apocrine sweat glands are stimulated during emotional stress and sexual excitement.
Sebaceous Glands
Sebaceous glands are oil glands that are found all over the body. Most are associated with hair follicles. They generate and excrete a mixture of lipids, called sebum, onto the hair and skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum and hair shaft. Sebum also has antibacterial properties and prevents water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood and become active only after puberty has occurred.
Example: Acne
Learn By Doing 16.10
For the questions below, decide which structure is referenced: hair, nails, sweat glands, or sebaceous glands.
- A person is too hot. Which structure would become active to maintain homeostasis?
Hint: This structure functions to cool you down. - A person stubs his toe. What structure would protect his toe?
Hint: This structure is made of hard keratinized cells. - A person has very dry skin. What structure may not be working well?
Hint: This structure secretes sebum.
Which of the following is not a function of the sweat glands?
- secrete sebum
- secrete excess fluid
- secrete electrolytic waste
- cool down the body
Which type of gland can become blocked and form a “blackhead?”
- endocrine
- compound
- sudoriferous
- sebaceous
Integumentary System and Homeostasis
In earlier sections, you learned about the amazing regenerative capacity of skin: Basal cells divide and differentiate to form keratinocytes, which move superficially to the surface and change their structure along the way. There are some cases where this regenerative property can cause problems and some traumas where regeneration is put to the test.
Example Psoriasis
Wound Repair and Scarring
The first step to repairing damaged skin is the formation of a blood clot that scabs over with time. Many different types of cells are involved in wound repair, especially if the surface area that needs repair is extensive. Before the basal stem cells of stratum basale can re-create the epidermis, fibroblasts mobilize and divide rapidly to repair the damaged tissue, forming a loose, highly vascular tissue called granulation tissue. This increased vascular network helps deliver the oxygen and nutrients necessary for further repair. Immune cells, like macrophages, roam the area and engulf any foreign matter, reducing the chance of infection while also clearing away any tissue debris.
Scars occur when there is repair of skin damage, but the healing process prevents regeneration of the original skin structure. Almost every cut or wound, with the exception of ones that only scratch the surface (epidermal wounds), leads to some degree of scar formation. As the tissue tries to repair itself to the original state, fibroblasts often generate a greater density of collagen fibers than were in the original tissue, which is what results in scar formation. This dense, fibrous structure (connective tissue) has few cells and does not allow for the regeneration of accessory structures (epithelial tissue) like hair follicles, sweat glands, or sebaceous glands.
Sometimes, scarring does not stop when the wound is healed. This results in the formation of a raised or hypertrophic scar called a keloid. In contrast, scars that result from acne and chickenpox have a sunken appearance and are called atrophic scars.
Scarring of the skin after wound healing is a natural process and does not need to be treated further. Application of oil and lotions may reduce the formation of scar tissue by keeping the skin soft and pliable as it heals, allowing the separate edges to be pulled together. However, modern cosmetic procedures like dermabrasion, laser treatments, and filler injections have been invented as remedies for severe scarring. All of these procedures try to reorganize the structure of the epidermis and underlying collagen in the connective tissue to make it look more natural.
Burns
Burns are wounds that result when the skin is exposed to intense heat, radiation, electrical current, or caustic chemicals. Burns cause skin cells to die, disrupting the epithelial barrier that normally prevents fluid loss. Depending on the severity of the burn, dehydration, electrolyte imbalance, and renal and circulatory failure may follow. Burn patients are treated with intravenous fluids to offset the dehydration, as well as intravenous nutrients that enable the body to repair tissues and replenish lost proteins. Another serious threat to a burn patient is the high possibility of infection. Burned skin is extremely susceptible to bacteria and other pathogens, as the loss of body covering provides a direct pathway for the entry of microorganisms.
Burns are classified by the degree of their severity. In first-degree burns, only the epidermis is damaged. Although painful, these burns typically heal on their own within a few days. A typical sunburn is a first-degree burn. Second-degree burns destroy both the epidermis and the dermis. They result in painful blistering of the skin. It is important for individuals with second-degree burns to keep the area clean and sterile in order to prevent infection. If this is done, the burns heal on their own within several weeks.
Third-degree burns are more serious and penetrate the full thickness of the skin, including the subcutaneous (hypodermis) layer. The skin may appear white, red, or black. Fourth-degree burns are the most severe, affecting the underlying muscle and bone as well. Third- and fourth-degree burns are usually not as painful because the nerve endings themselves are damaged. However, a third- or fourth-degree burn results in rapid water loss and infection due to the exposure of the underlying tissue and requires emergency trauma care. Full-thickness burns cannot be repaired locally because the local repair machinery itself is damaged. Full-thickness burns require excision of the affected tissue (amputation in severe cases), followed by grafting of skin from an unaffected part of the body or from skin grown in tissue culture for grafting purposes.
Thermoregulation and Thermal Homeostasis
The integumentary system regulates body temperature through several different means. Recall that sweat glands — accessory structures to the skin — excrete water, salt, and other substances to cool the body when it becomes warm. This is termed “sensible perspiration.” Even if the body does not appear to be noticeably sweating, approximately 500 mL of sweat are secreted a day. If the body becomes excessively warm due to high temperatures, vigorous activity, or a combination of the two, the blood vessels in the integumentary system dilate, and sweat glands produce large amounts of sweat — up to three gallons a day. As the sweat evaporates from the skin surface, the body is cooled; in a way, the skin surface acts like the radiator of a car. The dilated blood vessels in the dermis that account for the redness that many people experience when exercising on a hot day also help in the dissipation of body heat by increasing the superficial blood flow.
When temperatures are cold, the adipose tissue of the hypodermis helps insulate the body. Goosebumps, caused by contraction of the arrector pili muscles, help to insulate by trapping air on the surface of the skin. Additionally, the dermal blood vessels constrict to decrease blood flow (and heat loss) at the skin.
Learn By Doing 16.11
New cells to replace the cells that were damaged originate from:
- plaques
- stratum corneum
- macrophages
- stratum basale
What is the difference between a keloid scar and an atrophic scar?
- There is no difference; they are the same type of scar.
- A keloid scar is sunken, and an atrophic scar is raised.
- A keloid scar is raised, and an atrophic scar is sunken.
- A keloid scar is sunken, and an atrophic scar is hypertrophic.
Examine the image. Match the number in the image to one of the following words:
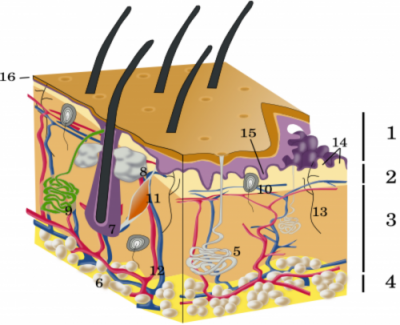
- sensory nerve ending,
- epidermis,
- sebaceous gland,
- hypodermis,
- reticular dermis,
- arrector pili muscle,
- papillary dermis,
- adipose cells,
- epidermal ridges,
- hair follicle,
- apocrine sweat gland,
- blood vessels,
- dermal papillae,
- thin skin,
- eccrine sweat gland,
- Pacini corpuscle
*
“Learn By Doing” and “Did I Get This?” Feedback
Learn By Doing 16.1
Decide whether each of the following statements is a fact or a myth.
- The skin can regenerate. Fact: The skin is made up of both connective and epithelial tissue. The epithelial tissue regenerates quickly. You have a brand-new epidermis approximately every 30 days.
- A bald person will get colder faster than a person with a full head of hair. Fact: A full head of hair insulates and decreases heat loss from the body. An exposed surface, such as a bald head will increase heat loss and make one colder.
- Shaving makes hair grow back faster. Myth: Hair grows from below the skin known as the follicle. Hair growth is not affected by cutting the hair.
- Squinting or frowning a lot can form wrinkles. Fact: Wrinkles occur with aging and a loss of skin flexibility. Making the same facial expressions increases the likelihood of developing wrinkles in those areas.
- Sunlight has some important health benefits. Fact: The skin makes vitamin D in response to UV radiation or sunlight. You only need about 20 minutes of sunlight exposure per day.
- Tanning from a tanning bed is less dangerous than sun tanning. Myth: No matter what the source UV radiation is dangerous to the skin. There are two main types of UV radiation that make it to earth – UVA and UVB. UVA waves have a longer wavelength and penetrate deeper into the skin. Tanning beds specifically use more UVA light which is more dangerous.
Learn By Doing 16.2
Tori mentions that the skin protects us from microbes; how do you think it accomplishes this?
- The skin is a covering that keeps things out of our bodies.
Incorrect. While this is true, there are additional methods the skin uses to protect us. - The skin secretes chemicals such as sweat and oils that form an antiseptic layer.
Incorrect. While this is true, there are additional methods the skin uses to protect us. - The skin protects us from dehydration and drying out.
Incorrect. While this is true, there are other ways the skin protects besides the chemical layer. - All of the above are ways the skin protects us.
Correct. As you can see, the skin has several methods of protecting the body.
Now that you’ve read a little more about the integumentary system and Tori, what do you think are the main concerns from a burn?
- In severe burns, the body is more susceptible to invasion from microbes and might dehydrate faster from fluid loss.
Incorrect. In Tori’s case, her epidermis will completely heal. There is a large surface area of skin on the body for vitamin D production. - The loss of sense of touch and areas vital for the formation of vitamin D from a burn.
Correct. The skin covers to protect us from invasion but also keeps fluids inside our body. - The skin might not be repaired, and the area will be a weak spot for infection.
Incorrect. The epidermis layer of the skin (top layer) heals fairly quickly.
Learn By Doing 16.3
The dermis layer is the most superficial layer of the skin.
- True
- False: The dermis is not the superficial (top) layer of the skin.
Which of the following is not part of the integumentary system?
- sebaceous glands
Incorrect. Sebaceous glands produce sebum or oil which helps to lubricate hair and form a chemical barrier on our epidermis. - hair
Incorrect. Hairs are located all over our body and are structures in the integumentary system. - hypodermis
Correct. The hypodermis is below the dermis and is not considered part of the integumentary system. - dermis
Incorrect. The dermis is one of the main structures of the skin. It contains the blood vessels which provide nutrients to the cells of the epidermis.
Which direction is the epidermis from the rest of the body?
- ventral
Incorrect. Ventral means “toward the front.” On your abdomen, the epidermis is on the ventral side of the body, but “ventral” is incorrect as a general term for the whole body. - dorsal
Incorrect. Dorsal means “toward the back,” like a dorsal fin on a shark. On your back, the epidermis is on the dorsal side of the body, but “dorsal” is incorrect as a general term for the whole body. - superficial
Correct. The outermost layer of skin, called the epidermis, is superficial, towards the outside of the body. - deep
Incorrect. The body is deep compared to the epidermis.
Learn By Doing 16.4
How does the structure of keratin create the hard, waterproofing quality of nails, hair, and skin?
- By adding strength with vitamin D.
Incorrect. Vitamin D will help with calcium absorption and bone strength. - By polymerization of intermediate filament proteins.
Correct. This polymerization of the proteins provides strength. - By adding strength with dialanine bridges.
Incorrect. Keratin has disulfide bridges for strength. - By polymerization of collagen fibers.
Incorrect. Collagen fibers are an important extracellular protein.
Recently, reports in the United States and Europe have shown vitamin D deficiencies and rickets-like symptoms in children. Why?
- childhood vaccinations
Incorrect. There is no link between childhood vaccinations and any disorder or disease. - lack of exercise
Incorrect. Exercise is good for bone and muscle health; however, this would not cause rickets. - too much time indoors and strong sunscreen
Correct. Too much time inside and constantly wearing SPF 100 sunscreen can cause a vitamin D deficiency; sunscreen is very useful in preventing skin damage and skin cancer, but too much of anything is not good. - poor nutrition in children
Incorrect. Although this is a problem in the U.S. and Europe, poor nutrition here generally leads to children being overweight.
What disease are people with albinism prone to?
Hints: Albinism is caused by a lack of melanin production. Consider the purpose of melanin.
- acne
Incorrect. Acne is an issue with the sebaceous glands and is not associated with melanin production. - keratosis
Incorrect. Keratosis (“kerat” stands for “keratin,” and “osis” means “disease”) is a disease of the keratin, which is not generally altered in patients with albinism. - skin cancer
Correct. Without melanin, UV light can damage the DNA of skin cells and may lead to skin cancer. - rashes
Incorrect. Rashes are an immune reaction of the skin, which is not typically due to sun exposure.
Learn By Doing 16.5
Our Answer: It is theorized that if the Langerhans cells don’t experience regular contact with antigens during early childhood development, they then will be more likely to become overactive and begin to attack the body’s own cells.
Which of the following is not matched with its proper description?
- Keratinocytes are found in the upper level of the skin and are usually dead.
Incorrect. Keratinocytes are found above the basal layer, and the outermost ones die and are sloughed off the skin. - Merkel cells sense deep pressure.
Correct. Merkel cells respond to light touch. - Basal cells are stem cells that can reproduce.
Incorrect. Basal cells are stem cells that divide by mitosis to produce new keratinocytes. - Langerhans cells engulf bacteria.
Incorrect. Langerhans cells are dendritic cells that can engulf any foreign organism that gets into the epidermis cell layers.
Learn By Doing 16.6
Which of the following is not a cell found in the epidermis?
- Epithelial cells
Incorrect. Epithelial cells are found in the epidermis. - Fibroblasts
Correct. Fibroblasts are located in the dermis. - Melanocytes
Incorrect. Melanocytes are found in the epidermis. - Keratinocytes
Incorrect. Keratinocytes are found in the epidermis.
If epithelial tissue has more than a single layer of cells, it is called ____.
- stratified
Correct. The stratified epithelium has strata, or layers, of cells. - pseudostratified
Incorrect. Pseudostratified epithelium appears to have more than one layer of cells, but close examination shows that all cells contact the basement membrane. - complex
Incorrect. - simple
Incorrect. Simple epithelium has only one layer of cells.
Learn By Doing 16.7
The majority of the dermis is composed of:
- Stratified squamous epithelium
Incorrect. The epidermis is made of stratified squamous epithelium. - Adipose tissue
Incorrect. The hypodermis contains adipose tissue. - Dense irregular fibrous connective tissue
Correct. This type of tissue organization allows for the blood vessels, muscles, and nerves that serve the skin.
One cosmetic treatment for wrinkles is Botox. This neurotoxin helps temporarily remove wrinkles caused by repetitive motion, such as crow’s feet. Which of the following explains why this treatment is only temporary and why it cannot fix other types of wrinkles?
- Botox can decrease the tension of underlying muscles but not repair the damaged extracellular matrix proteins.
Correct. The toxin will cause paralysis of the facial muscles and reduce wrinkles, but it does not fix the damage, so it is only temporary. - Botox can signal to the muscles to stretch the epidermis back out.
Incorrect. Botox can induce paralysis of the muscles, which does not stretch the epidermis out. - Botox can reduce the damage by increasing the production of collagen.
Incorrect. Botox does not affect the fibroblast cells; it inhibits neural impulses. Fixing the damaged extracellular proteins would fix the problem permanently. - Botox can signal the fibroblast to secrete more extracellular matrix, replacing the damaged fibers.
Incorrect. Botox is a toxin that paralyzes the muscles. The fibroblasts are responsible for making more extracellular proteins.
Why is the combination of elastin and collagen important to the function of the skin?
- Collagen: coloration; elastin: immune response
Incorrect. These extracellular proteins are not involved in coloration or in the immune response. - Collagen: protection; elastin: distention
Correct. Collagen adds to the strength of the skin for protection, and elastin provides elasticity for distention. - Collagen: distension; elastin: protection
Incorrect. Elastin allows for elasticity and distension, not protection. - Collagen: connection; elastin: coloration
Incorrect. Melanin is responsible for coloration.
Learn By Doing 16.8
In a person with the genetic disease albinism, the eyes are red. This red color is a result of what?
- The melanosomes fusing too soon with the lysosomes.
Incorrect. Melanosomes are cells that contain melanin. In albinism, melanin is not produced.
- Too little melanin being produced and the blood vessels showing through.
Correct. With a lack of melanin, the red of the blood can show through in the eyes. - An uneven distribution of the melanocytes.
Incorrect. Uneven distribution of melanocytes can result in freckles, not albinism. - Too much pheomelanin being produced and giving a reddish tint.
Incorrect. Even though pheomelanin does have more of a reddish tint if someone has albinism, they are not producing this type of melanin.
Some people see freckles appear on their noses and cheeks during the summertime and fade during the winter. What would cause this?
- A lower amount of melanin being transferred to the keratinocytes in response to UV radiation.
Incorrect. In the local area of the freckle, more melanin is being transferred to the keratinocytes. - Uneven distribution of melanocytes reacting to UV radiation
Correct. With sun exposure, all melanocytes will produce more melanin in response to UV radiation from the sun, but because melanocytes can be clustered in certain areas of the skin, this distribution becomes more noticeable, producing more melanin in areas with more melanocytes than in the surrounding areas that have fewer melanocytes. - Uneven production of melanin in response to temperature
Incorrect. Even though these melanocytes may produce more melanin, they are not producing it in response to temperature. - Freckles cannot just appear during the summer and fade during the winter.
Incorrect. Although some people genetically inherit the trait for freckles that are present all the time, some freckles can appear in the summer because of the radiation and disappear in the winter.
Learn By Doing 16.9
Which of the following connects the epidermis to the dermis?
- Stratum Basale
Correct. This is the germ layer that contains a variety of cell types and connects the epidermis and dermis. - Stratum Corneum
Incorrect. The corneum layer is away from the dermis. - Stratum Granulosum
Incorrect. This is away from the dermis. - Stratum Spinosum
Incorrect. This choice is close; this stratum is one layer away from the basal layer.
The stratum corneum consists of layers of dead cells. How can these dead cells help protect the living cells underneath?
- They allow for osmosis to occur easily.
Incorrect. Osmosis is the movement of water, which is impaired in these cells. - .They secrete antimicrobial oils.
Incorrect. The sweat glands and sebaceous glands secrete antimicrobial substances. - They allow diffusion to occur easily.
Incorrect. Diffusion is the movement of molecules from an area of high concentration to an area of lower concentration. A layer of dead cells would interfere with diffusion. - They are resistant to water penetration.
Correct. The keratin-filled cells act as a waterproof barrier.

Fingerprints are created by a combination of “friction ridges” of the human finger. These friction ridges create patterns that are unique to every individual. The interaction of the epidermis with a layer of the dermis creates these ridges. Which layer of the dermis do you think creates fingerprints?
- reticular layer Incorrect. The reticular layer is under the papillary layer and does not extend up to the epidermis.
- papillary layer Correct. The papillary layer is just deep to the epidermis, and the dermal papillae cause fingerprints to form.
What is the advantage of not having oil on regions of thick skin including the hands? Submit your answer and compare it with the answer given.
Our Answer: Areas on the body that have thick skin require traction that would be prevented by oil, such as the hand gripping something.
The net-like mesh of collagen fibers in the reticular layer adds to the resilience of the dermis because of what?
- The net-like mesh of collagen binds and holds water.
Correct. In addition to providing structure and strength, the collagen fibers hold water to maintain skin turgor. - Collagen fibers secrete elastin.
Incorrect. Collagen fibers do not secrete elastin; fibroblasts secrete elastin. - The net-like mesh of collagen fibers stores fat, which holds water.
Incorrect. Fat is stored in the hypodermis layer. - The collagen fibers form a loose mat that contains blood vessels and phagocytes.
Incorrect. The fibroblasts secrete collagen and elastin fibers in the papillary layer, which forms a loose mat.
One of the functions of the subcutaneous level or hypodermis is to provide insulation for the body. What structure allows the hypodermis to perform this function?
- adipose tissue
Correct. Adipose tissue stores fat, and fat is a good insulator. - elastic fibers
Incorrect. Elastic fibers add elasticity to the tissue. - collagen fibers
Incorrect. Collagen provides structural support, not insulation.
Learn By Doing 16.10
For the questions below, decide which structure is referenced: hair, nails, sweat glands, and sebaceous glands.
- A person is too hot. Which structure would become active to maintain homeostasis?
Sweat glands secrete sweat, which is mostly water that will evaporate and cool the body. - A person stubs his toe. What structure would protect his toe?
Nails are used for protection. - A person has very dry skin. What structure may not be working well?
Sebaceous glands secrete oil (sebum) that helps moisturize the skin.
Which of the following is not a function of the sweat glands?
- secrete sebum
Correct. Sebum is secreted by sebaceous glands. - secrete excess fluid
Incorrect. Sweat is one mechanism to remove excess fluid from the body. - secrete electrolytic waste
Incorrect. Sweat is a mechanism to excrete electrolytic waste. - cool down the body
Incorrect. The evaporation of sweat cools the body.
Which type of gland can become blocked and form a “blackhead?”
- endocrine
- compound
- sudoriferous
- sebaceous
Learn By Doing 16.11
New cells to replace the cells that were damaged originate from:
- plaques
Incorrect. Plaques form when too many cells accumulate. - stratum corneum
Incorrect. The stratum corneum is the top layer of the epidermis. - macrophages
Incorrect. Macrophages are part of the immune system. - stratum basale
Correct. The stratum basale contains basal stem cells.
What is the difference between a keloid scar and an atrophic scar?
- There is no difference; they are the same type of scar.
Incorrect. These two types of scars are the opposite of each other — one is raised, and one is sunken. - A keloid scar is sunken, and an atrophic scar is raised.
Incorrect. A keloid is a raised scar, also called hypertrophic. An atrophic scar looks sunken. - A keloid scar is raised, and an atrophic scar is sunken.
Correct. A keloid is a raised scar, also called hypertrophic. - A keloid scar is sunken, and an atrophic scar is hypertrophic.
Incorrect. Hypertrophic (keloid) scars are raised, and atrophic scars are sunken.
Examine the image. Match the number in the image to one of the following words:
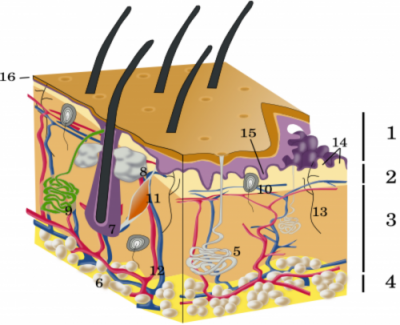
- epidermis
- papillary dermis
- reticular dermis
- hypodermis
- eccrine sweat gland
- adipose cells
- hair follicle
- sebaceous gland
- apocrine sweat gland
- Pacini corpuscle
- arrector pili muscle
- blood vessels
- sensory nerve ending
- dermal papillae
- epidermal ridges
- thin skin
