Exchange with the Environment
12 Respiratory System
Introduction
Hold your breath. Really! See how long you can hold your breath as you continue reading…How long can you do it? Chances are you are feeling uncomfortable already. A typical human cannot survive without breathing for more than 3 minutes, and even if you wanted to hold your breath longer, your autonomic nervous system would take control. This is because every cell in the body needs to run the oxidative stages of cellular respiration, the process by which energy is produced in the form of adenosine triphosphate (ATP). When this occurs, oxygen is used as a reactant, and carbon dioxide is released as a waste product. You may be surprised to learn that although oxygen is a critical need for cells, it is actually the accumulation of carbon dioxide that primarily drives your need to breathe. Carbon dioxide is exhaled, and oxygen is inhaled through the respiratory system, which includes muscles to move air into and out of the lungs, passageways through which air moves, and microscopic gas exchange surfaces covered by capillaries. The circulatory system transports gases from the lungs to tissues throughout the body and vice versa. A variety of diseases can affect the respiratory system, such as asthma, emphysema, chronic obstructive pulmonary disorder (COPD), and lung cancer. All of these conditions affect the gas exchange process and result in labored breathing and other difficulties.
Major Functions of the Respiratory System
Learning Objective
The major function of the respiratory system is to bring in oxygen into the body and remove carbon dioxide from the body. The metabolic pathway that converts the bond energy of nutrients into the usable form of ATP (aerobic cellular respiration) requires oxygen gas and produces carbon dioxide gas as a byproduct. For example:
| C6H12O6 + 6O2 → 6CO2 + 6H2O and energy stored in ATP |
As you can see from the equation, six molecules of oxygen are needed for each molecule of glucose that is broken down, and six molecules of carbon dioxide are produced. Because cells require a continuous supply of ATP, the body, in turn, needs a constant intake of oxygen and a method for the removal of carbon dioxide. Our respiratory system allows us to complete these critical gas exchanges.
The major organs of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help to maintain acid-base balance. Portions of the respiratory system are also used for non-vital functions, such as sensing odors and speech production, and for straining, such as during childbirth or coughing.
Did I Get This 13.1
Replace the numbers in the sentences below with a word from the numbered column.
The main function of the respiratory system is to obtain _____1_____ from the air to be used to convert _____2_____ to _____2_____. The respiratory system also needs to remove _____1_____from the blood.
|
1 |
2 |
|
carbon dioxide |
energy |
|
oxygen |
nutrients |
Respiratory Structures and Functions
Learning Objectives:
- Identify and describe gross & microscopic anatomy of the respiratory tract and related organs.
- Describe the mechanisms of pulmonary ventilation.
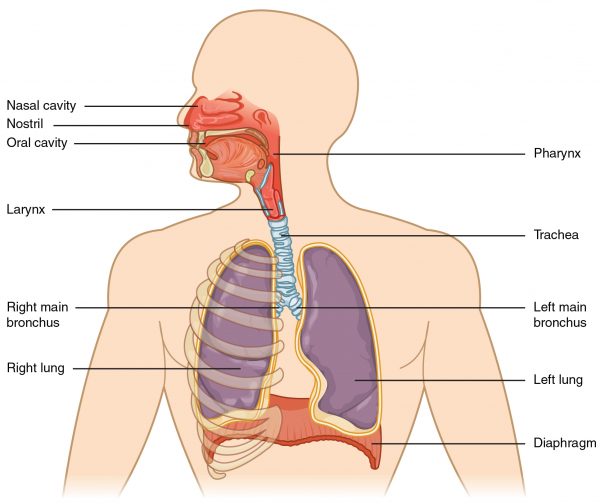
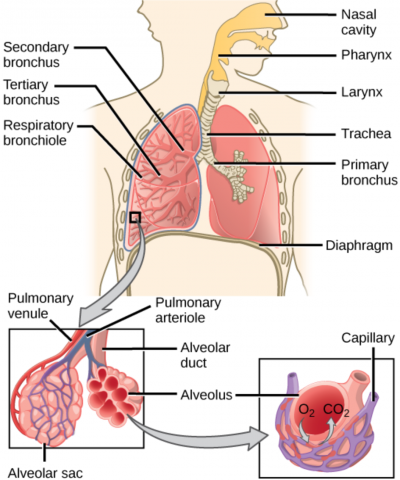
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange. The gas exchange occurs in the respiratory zone.
Conducting Zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. The epithelium of the nasal passages, for example, is essential to sensing odors, and the bronchial epithelium that lines the lungs can metabolize some airborne carcinogens.
The Upper Respiratory Tract
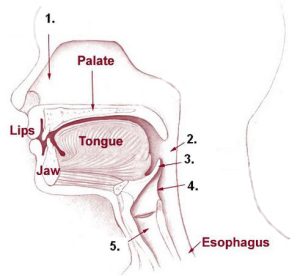
The upper respiratory tract begins with the nose and ends with the larynx.
Nose: The external portion of the nose begins at the base of the frontal bone and extends over the maxilla, with the nasal bone providing the bridge of the nose. Extending from the nasal bone is a collection of hyaline cartilages that make up the bulk of the nose. The medial region of the nose consists of a central cartilage (the septum) with two lateral processes. The tip of the nose is also formed from cartilage. Variations in the size of a person’s nose, or its form, are due to differences in the various cartilages. The visible nose is actually the entryway into the nasal cavity, where the major functions of the nose occur. The openings to the nose, the nares, are lined with coarse hairs to aid in the filtration of particulate matter. The area immediately inside the nares contains a large number of sebaceous glands, sweat glands, and hair follicles.
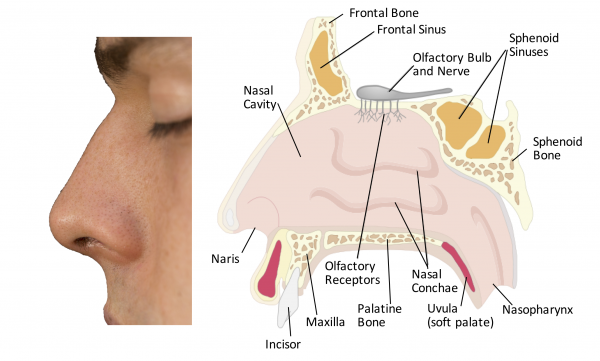
The nasal cavity is divided into the right and left sides by the nasal septum. The roof of the nasal cavity consists of parts of the ethmoid and sphenoid bones. Its floor, the palate, forms the roof of the mouth. It is separated into the hard and soft palate. The anterior hard palate is formed from part of the palatine bone. The posterior soft palate (the uvula) does not contain bone. It moves up during swallowing to close off the nasal cavity, thus preventing material from entering the mouth. The nasal cavity opens into the nasopharynx.
Extending from the nasal septum are pairs of C-shaped structures called conchae. They are covered by a mucus membrane that contains a large number of mucus-secreting cells and blood vessels. (A bloody nose highlights the richness of the blood supply to the membranes on the conchae.) The conchae serve as baffles that increase the surface area of the nasal cavity. The mucus glands and blood vessels aid in humidifying and warming the air coming into the body.
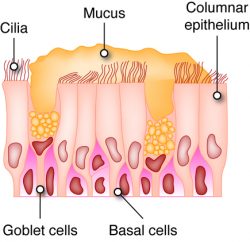
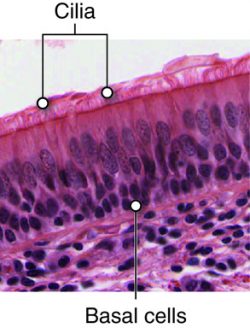
There are two types of epithelial coverings in the nasal cavity: respiratory epithelium and olfactory epithelium. Both types of epithelia appear very similar when viewed through a light microscope. The olfactory mucosa found in the roof of the cavity detects odors. This epithelial layer contains specialized nerve cells that detect odors and transmit impulses to the first cranial nerve. The respiratory epithelium that covers the rest of the nasal cavity is also found through most of the respiratory tract and is pseudo-stratified ciliated columnar epithelia.
Paranasal sinuses: Within the bones surrounding the nasal cavity are paranasal sinuses (a sinus is a hollow area), which function to make the skull lighter as well as moisten and warm incoming air. These sinuses frequently become filled with excess fluid when a person has a head cold. Since the paranasal sinuses serve as resonators for speech and sound it is not surprising that the sound of the voice becomes altered when they are filled with fluid or swollen. The frontal, sphenoid, ethmoid, and maxillary bones all contain sinus cavities.
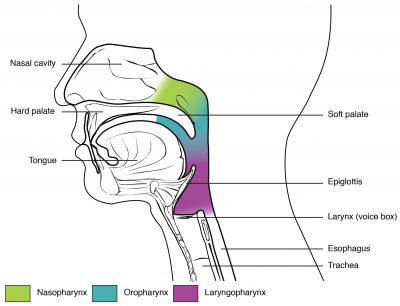
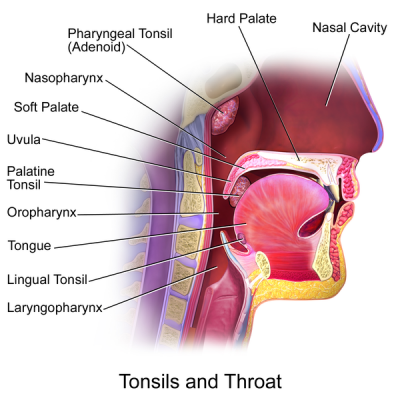
Pharynx: As air passes posteriorly through the nasal cavity, it enters the pharynx. This structure has three distinct areas, the nasopharynx, the oropharynx, and the laryngopharynx. The pharynx connects the nasal passage to the larynx in the throat.
Tonsils: Collectively, the tonsils aid in filtering foreign material that could do harm to the body. The paired pharyngeal tonsils, also known as the adenoids, lie in the posterior wall of the nasopharynx. The other tonsils, the tubal tonsils, protect the auditory tubes and middle ear against entering microorganisms. They are located at the opening of the tube that connects the middle ear to the nasopharynx. The auditory or Eustachian tube equilibrates air pressures between the environment and the middle ear. The orientation of the auditory tube changes during infancy and early childhood. The tube is oriented horizontally until around age two. Consequently, it frequently serves as a point of entry for bacteria in children less than two years of age. Around age two, the auditory tube changes course and slants down from the ear, allowing fluid to drain more readily. Without the fluid to act as a growth medium and pathway to the middle ear, older children usually experience few ear infections. The paired palatine tonsils lie along the two sides of the oropharynx. The lingual (lingual meaning tongue) tonsils are not in the oropharynx but are located at the base of the tongue.
Larynx: After air leaves the pharynx, it enters the larynx, a complex cartilaginous structure that extends from the laryngopharynx and the hyoid bone to the trachea.
The larynx helps regulate the volume of air that enters and leaves the lungs. The structure of the larynx is formed by several pieces of cartilage. The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males.
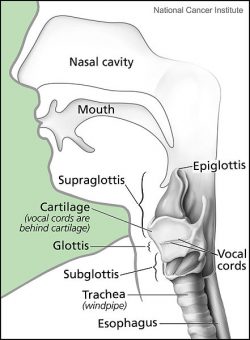
(Credit: Alan Hoofring for the National Cancer Institute, public domain)
In addition to providing a passageway for air, the larynx directs air and food to the appropriate tubes. The airway is blocked by closing off the opening of the trachea with the epiglottis upon swallowing. The vocal cords, which are used in making sounds and speech, can be found within the larynx.
Epiglottis: The epiglottis is made of elastic cartilage and covered with stratified squamous epithelia. It connects loosely to the tongue, the hyoid bone, and the rim of the thyroid cartilage. The epiglottis is normally open, allowing air to freely flow into the rest of the larynx and the trachea. When a person swallows, the front of the epiglottis is raised, and the posterior portion descends, covering the glottis, which is the opening to the vocal cords and trachea. This movement directs food and water to the esophagus and prevents them from entering the bottom portion of the larynx and the upper trachea. If someone tries to talk or laugh and swallow at the same time, the air used to talk or laugh forces the epiglottis open, the swallowed material “goes down the wrong tube,” and choking results.
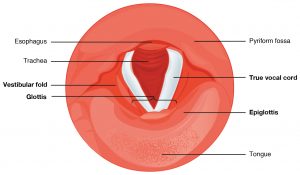
Vocal cords: The vocal cords consist of two pairs of folded tissue in the larynx immediately inferior to the epiglottis. These are the false and true vocal cords respectively. The false vocal cords do not function in making sounds or speech but aid in closing the glottis, which opens to the rest of the larynx and the respiratory system. Below the false vocal cords are the true vocal cords. They are reinforced with elastic fibers and vibrate when adequate air is forced through the gap between them, resulting in sound. Pitch control is achieved by adjusting the tension on the cords. Lessening the tension lowers the pitch. During puberty in males, the cords are usually lengthened making for a deeper sound. Actual speech is achieved with the coordination of muscles in the pharynx, face, tongue, soft palate, and lips.
Learn By Doing 13.1
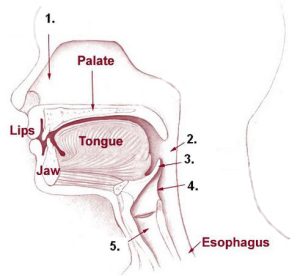
Identify the upper respiratory tract structures in the image.
How would air entering the lungs be different without the nasal cavity? Hint: Think about the structures in the nasal cavity and what their functions are.
If a person has an injury to the epiglottis, what would be the physiological result?
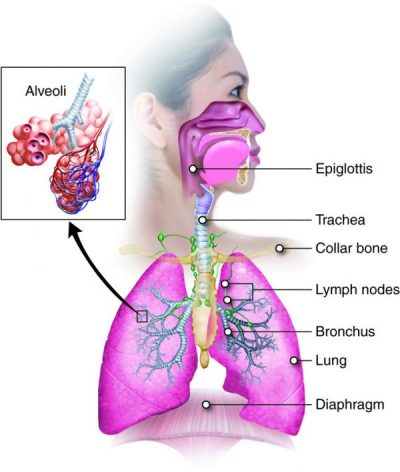
Gross Anatomy of the Lower Respiratory Tract
The lower respiratory tract begins with the trachea, which begins just below the larynx, and ends with small passageways called the terminal bronchioles.
(Credit: Cenveo, CC BY 3.0 United States via OLI-CMU)
The flow of air continues from the larynx to the trachea or windpipe. The main function of the trachea is to funnel the inhaled air to the lungs and the exhaled air back out of the body. The human trachea is a cylinder, about 25 to 30 cm (9.8–11.8 in) long, which sits in front of the esophagus and extends from the pharynx into the thoracic cavity to the lungs. It is made of C-shaped rings of cartilage and smooth muscle. The cartilage provides strength and support to the trachea to keep the passage open. The last cartilage in the trachea has a projection from the anterior surface that extends into the lumen. This projection, the carina, is very sensitive to particulate material and causes coughing when stimulated. The openings of the C-shaped cartilages face the posterior of the trachea and contain smooth muscle. This muscle constricts when someone coughs, increasing the force of the cough. The muscle also constricts during an asthmatic reaction, shrinking the airway and making it harder to breathe. The trachea is lined with cells that have cilia and secrete mucus. The mucus catches particles that have been inhaled, and the cilia move the particles toward the pharynx.
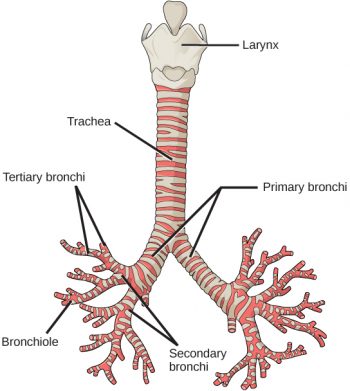
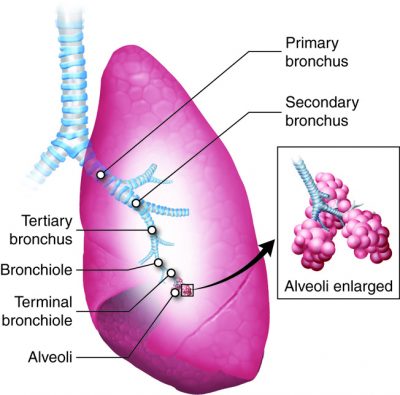
The Bronchi and Bronchioles: The bronchial tree is so named because it resembles a tree that has been turned upside-down. The trachea would be the trunk, the progressively smaller bronchi and bronchioles are the branches, and the alveoli are the leaves.
The end of the trachea divides into two bronchi that enter the right and left lungs. Air enters the lungs through the primary bronchi. Each primary bronchus divides, creating smaller and smaller diameter bronchi. When the passages are under 1 mm (.03 in) in diameter when they are called bronchioles, and they split and spread through the lung. Like the trachea, the bronchus and bronchioles are made of cartilage and smooth muscle. Bronchi are innervated by nerves of both the parasympathetic and sympathetic nervous systems that control muscle contraction (parasympathetic) or relaxation (sympathetic) in the bronchi and bronchioles, depending on the nervous system’s cues. The final bronchioles are the respiratory bronchioles.
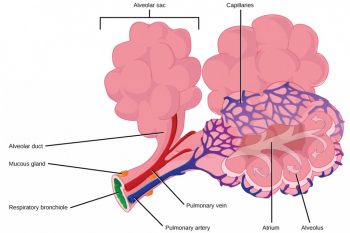
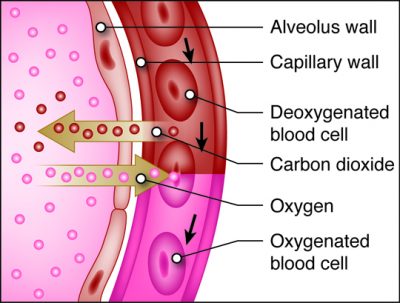
Alveolar ducts are attached to the end of each respiratory bronchiole. At the end of each duct are alveolar sacs, each containing 20 to 30 alveoli (air sacs). Gas exchange occurs only in the alveoli. The alveoli are thin-walled and look like tiny bubbles within the sacs. The alveoli are in direct contact with the capillaries of the circulatory system. Such intimate contact ensures that oxygen will diffuse from the alveoli into the blood. In addition, carbon dioxide will diffuse from the blood into the alveoli to be exhaled. The anatomical arrangement of capillaries and alveoli emphasizes the structural and functional relationship between the respiratory and circulatory systems. Estimates for the surface area of alveoli in the lungs vary around 100 m2. This large area is about the area of half a tennis court. This large surface area, combined with the thin-walled nature of the alveolar cells, allows gases to easily diffuse across the cells.
The bronchial tree is lined by pseudo-stratified ciliated columnar epithelia with goblet cells dispersed among the columnar cells. Mucous glands secrete mucous into the airways, keeping them moist and flexible. Plates of cartilage are found in the walls of the bronchial tree, with the amount of cartilage and the number of plates decreasing as the bronchi and bronchioles become smaller. The terminal bronchioles do not contain cartilage plates; these tubes are small enough to stay open without cartilage. Smooth muscle is found throughout the system, even in the respiratory zone.
The Lungs
The lungs are two of the largest organs of the body, but they are among the lightest. Along with the heart, the lungs take up nearly all of the space in the thorax, superior to the diaphragm. As an organ, the lung is made up of airway tubes and alveoli, making it very light. Elastic connective tissues in the lungs allow them to expand with incoming air and recoil when expelling air. The lungs contain a large amount of surface area in order to efficiently support the exchange of oxygen and carbon dioxide.
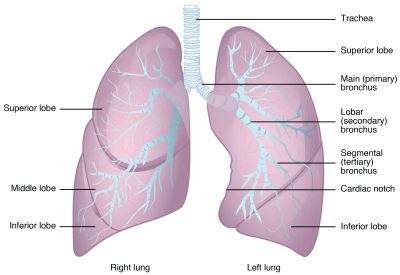
The hilus(meaning depression or pit) of the lungs is an indentation on the medial side of the lungs and the point of entry of blood vessels, primary bronchi, nerves, and lymphatics. This collection of vessels and nerves makes up the root of the lung. The tip or apex of the lungs is a blunted point found just above the clavicles. The posterior, lateral, and anterior sides of the lungs are surrounded by the ribs. These areas are called the costal surfaces of the lungs referring to the costal cartilage surrounding them. The flat, inferior surface of the lungs is found superior to the diaphragm and referred to as the base of the lung. Since the liver is found on the right side of the body and inferior to the diaphragm, the insertion of the diaphragm is slightly raised on the right. Consequently, the right lung is usually slightly shorter than the left. Although the right lung is slightly shorter than the left, the left lung has about 10 percent less mass than the right due to the cardiac notch on the medial side of the left lung. The heart is tucked into this notch. The heart, the right lung, and the left lung are each located in their own anatomical compartment in the upper thorax. The right lung is divided into three lobes. The smaller left lung contains only two lobes.
Each lobe is divided into bronchopulmonary segments separated by connective tissue septa (septa = walls). There are a total of 10 of these segments, and each contains a tertiary bronchiole, a pulmonary and bronchial artery, and a lymphatic branch. The presence of these segments aids in further isolating parts of the lungs to prevent the spread of infection or disease. Connective tissue further divides the segments into lung lobules, the smallest anatomical unit in the lungs.
Learn By Doing 13.2
Examine the image of the tree below. Replace the numbers in the paragraph below with one of the phrases in this table.
| Numbers 1, 3, 5 | Numbers 2, 4, 6 |
 |
| Trachea
Bronchioles Bronchi |
Cartilage
No Cartilage C-shaped rings of cartilage |
The trunk of this tree would represent ___1____ which requires ___ 2___ to remain open. The split in the tree that leads to the two primary branches would represent the ___3____ which requires ___4____ to remain open. The smallest branches of the tree would represent ___5____ which requires ___6____ to remain open.

The connective tissue associated with lobules may be blackened by tobacco smoke or pollution from the environment. The image to the right compares the lungs of a smoker with those of a non-smoker. Usually, the lungs are pink with a relatively smooth surface. The lungs on the right are blackened and irregularly shaped from the accumulation of material inhaled with tobacco smoke. This material can be cleared from the lungs, but only over a long period of time and only if the person stops smoking. Cigarette smoking causes the deaths of over 440,000 people in the United States each year, including people exposed to second-hand smoke. The financial losses associated with these deaths are in excess of 200 billion dollars a year.
There are over 4,000 chemical compounds that are created when the more than 600 chemical ingredients in cigarettes are burned and inhaled. More than 50 of the chemicals produced by the burning of a cigarette are classified as carcinogens. A partial list of these chemicals includes acetone, acetic acid, ammonia, arsenic, benzene, butane, cadmium, carbon monoxide, formaldehyde, lead, naphthalene, methanol, nicotine, tar, and toluene.
The direct effect of many of the chemicals in the smoke is to paralyze and destroy cilia. When the cilia cannot function, mucus accumulates in the lung tubules. Opportunistic bacteria and other microorganisms utilize the mucus to grow and colonize the lungs. Many of these organisms create pathologic conditions inside the lung.
Smoker’s cough is a condition that exists because mucus and other debris accumulate in the lung tissue. These accumulations stimulate the cough reflex as a means to clear the lungs. The inhaled chemicals can also contribute to the breakdown of connective tissue fibers, especially elastin. The degeneration of the connective tissue can lead to emphysema, a form of chronic obstructive pulmonary disease (COPD).
Learn By Doing 13.3
Consider what occurs to cause “Smoker’s cough”. Based on this description, the function of the cilia is to move ___1____ up and out of the lungs. If the cilia are paralyzed or destroyed by chemicals in cigarettes, the body must ___2____ to remove mucus from the lungs. If the mucus is not removed from the lungs, microorganisms can grow in it. This may lead to ___3____ .
| 1 | 2 | 3 |
|
Mucus or Air |
Sneeze or Cough |
COPD or Pneumonia |
Blood and Nerve Supply
The lungs have a dual blood supply. The pulmonary artery brings oxygen-poor blood from the right ventricle of the heart. This blood passes through the pulmonary capillaries, where some carbon dioxide will leave the blood, and a large amount of oxygen will be acquired. The newly oxygenated blood enters the pulmonary veins and returns back to the left side of the heart. The pulmonary circulation holds about 500 milliliters (ml) of blood or about 10 percent of the body’s supply. About 75 ml of blood is in the pulmonary capillaries for gas exchange at any one time. The blood supply that nourishes the tissues of the lungs arrives through the bronchial artery, which branches off of the aorta and carries oxygen-rich blood to support the lung tissues.
Nerves from the pulmonary plexus enter the lungs at the hilus. These nerves contain a mixture of visceral sensory and autonomic nerve fibers that follow the bronchial tree and blood vessels. Parasympathetic nerve stimulation results in bronchoconstriction, constriction of the bronchioles, while sympathetic nerve stimulation results in bronchodilation, dilation of the bronchioles.
Pleura
Each lung is found in a pleural cavity bounded by the pleural membrane, a double-sided membrane that contains a thin layer of pleural fluid. The visceral pleural is a mucus membrane that covers the lungs and folds over at the hilus. The folded membrane continues and becomes the parietal pleura, which lines the inner wall of the thoracic cavity. The space between the two membranes is called the pleural cavity or space. From 1 to 15 ml of pleural fluid is found on the facing surfaces of the pleural membranes. This fluid helps to lubricate the membrane surfaces so that the movement of the lungs during inhaling and exhaling does not cause frictional damage to the tissues. The fluid also lightly holds the two membranes together so that they move together as the chest wall expands and contracts.
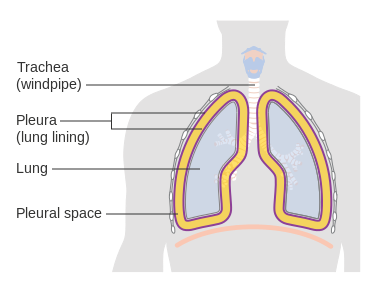
By Cancer Research UK, CC BY SA 4.0
Since pleural fluid is mainly a filtrate of plasma, the factors that affect the amount of pleural fluid production and removal are the same factors that govern interstitial fluid volumes in most regions of the body. The main factors include capillary hydrostatic pressure, capillary colloid osmotic pressure, the permeability (“leakiness”) of the capillaries, and the rate of fluid removal by the lymphatics. Under normal conditions, there is a slow but steady turnover of pleural fluid, but under certain conditions, excess fluid can build up and impede lung expansion. This condition is known as pleural effusion and may be secondary to the blockade of venous drainage by tumors, increased capillary permeability because of infections, etc.
The pleural sac extends below the lungs to the level of the twelfth thoracic vertebrae. Samples of the pleural fluid can be safely taken from this area. Normal pleural fluid is clear and pale yellow in color. It has very few cells free in the fluid. The majority (98 percent) of these cells are immune system cells, with an assortment of cells making up the remaining 2 percent.
Learn By Doing 13.4
Respiratory Functions
Learning Objective
The movement of gases from the atmosphere into the lungs is called ventilation and includes the bulk flow of air from outside the body into the respiratory system (inhalation) and the bulk flow of air from the respiratory system back to the outside (exhalation). External respiration includes the exchange of oxygen and carbon dioxide between the space inside the lungs and the blood. These gases must be transported throughout the body, a process accomplished by blood. Internal respiration includes the exchange of gases between the cells and the blood. The conduit for moving air into the lungs and then returning it to the external environment is referred to as the conducting zone( or division). Gas exchange does not take place in the structures that make up the conducting zone. The conducting zone consists of a system of tubes that connect the nose and mouth to the alveoli. Air movement starts at the nose or mouth and continues through the pharynx, larynx, trachea, and bronchial tree, terminating at the structures of the respiratory zone or division) where external respiration occurs.
The respiratory zone includes the very small respiratory bronchioles, the alveoli, and the blood capillaries. It is critical that both the conducting and respiratory zones function adequately for the body to maintain homeostasis. Organization of conducting and respiratory zones will be the focus of this discussion.
The Conducting Zone
The conducting zone of the respiratory system brings gases into and out of the respiratory system. In addition, the organs and tissues along this path warm the incoming air to approximately body temperature, moisten the air to about 100 percent humidity and begin filtering out any harmful microorganisms or particles that may be suspended in the inhaled air.
Temperatures too far below 37°C (98.6°F) can harm the delicate alveoli and inhibit enzyme function. Damaged alveoli or improperly functioning enzymes could lead to decreased gas diffusion and subsequent homeostatic imbalances. For example, the interconversion of carbon dioxide and carbonic acid is catalyzed by the enzyme carbonic anhydrase. Similar to most other body enzymes, it loses efficiency at lower temperatures. If carbonic anhydrase is not functioning properly, there could be an increase in carbonic acid levels. Since carbonic acid breaks down into bicarbonate ions and free hydrogen ions, there would be a resulting decrease in pH leading to acidosis. The temperature in the respiratory zone is so important that a person who runs in cold weather is advised to put a scarf across their nose and mouth to help pre-warm the air. Otherwise, the tissues in the conducting zone may not be able to warm the air sufficiently to prevent damage to the system.
If the air in the respiratory zone is not near 100 percent humidity, the thin-walled alveoli can become dehydrated and may deteriorate. The alveoli are lined with a very thin layer of water and chemicals that prevent damage to the tissues and help to keep the alveoli open. If the air taken to the respiratory zone doesn’t have sufficient humidity (water vapor), the water layer lining the alveoli will evaporate resulting in damage to the structures and interference with respiration.
The hairs found at the entrance to the nose, along with the mucus and cilia found inside the nose help to trap and remove pathogens and particles taken in with air. Large particles can build up at the entrance of the nose where the hairs trap them. Coal miners, for example, will accumulate coal dust at the opening of their nostrils due to the action of these hairs. Smaller particles, such as some viruses and bacteria will be trapped in the mucus in the nose, and the cilia on the epithelial cells will sweep them to the back of the pharynx. The combined action of the mucus and the cilia is referred to as the mucociliary escalator. Ultimately the mixture of mucus and particles will be swallowed and destroyed by the acid and digestive enzymes in the stomach. This process of trapping and removal of particles and microorganisms occurs throughout the conducting zone and through the first part of the respiratory zone.
The Respiratory Zone
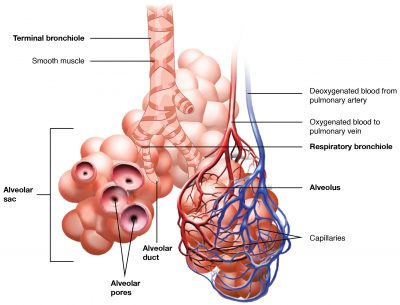
A transition occurs in the composition of the epithelial lining at the end of the terminal bronchioles. The epithelial lining changes to simple cuboidal cells without any intermixed goblet cells. The walls of the tubes at this point become very thin and are called respiratory bronchioles. The loss of the goblet cells means that no mucus is secreted into the bronchioles at this point, but the cilia are still present to sweep away any mucus that should come down into them. Some portions of the respiratory bronchioles are not completely covered by cilia, and a number of phagocytic macrophages are found in this area to compensate for the loss of the cilia. Some gas exchange can occur through the walls of the respiratory bronchioles.
Respiratory bronchioles lead into the alveolar ducts, which still have smooth muscle and some elastic fibers in the walls. Alveolar sacs occur as clusters of alveoli (singular alveolus) sharing a common chamber along the alveolar ducts. It has been estimated that there are 300 million alveoli in the lungs. These alveoli provide a surface area of 27 square meters or an area of 25 feet by 30 feet, which is roughly the size of a three-car garage. Adjacent alveoli are interconnected through alveolar pores.
Pulmonary Ventilation
Pulmonary ventilation is the act of breathing. Pulmonary ventilation brings in air with a new supply of oxygen and a very small amount of carbon dioxide from the atmosphere into the alveoli. This mixture then participates in external respiration, the exchange of oxygen and carbon dioxide between the alveoli and pulmonary capillary blood across the respiratory membrane. Internal respiration is the exchange of gases between the tissues of the body and the blood, which provides oxygen for aerobic cellular respiration and removes carbon dioxide. Aerobic cellular respiration refers to the intracellular use of oxygen and the generation of carbon dioxide waste through metabolic pathways.
Learn By Doing 13.5
Replace the numbers in the paragraph below with one of the following words:
- External respiration
- Ventilation
- Conducting zone
- Respiratory zone
- Cellular Respiration
- Internal respiration
___1___ is the movement of air into the body and the movement of air back out of the body. The channel for moving air into the lungs and back out is referred to as the ___2___. Gas exchange in the lungs is called ___3___, and the location where this gas exchange occurs is called the ___4___. After oxygen-enriched blood is transported through the body, ___5___ occurs. This process then allows ___6___.
Decide whether each of the statements below describes the conducting zone or the respiratory zone of the respiratory tract.
- Responsible for warming and humidifying air entering the body.
- Allows for the passage of air from inside the body to outside the body.
- Allows for gas exchange between the lungs and the blood.
Which of the following is the correct order that air passes through structures in the respiratory system during inspiration?
- Lungs, bronchi, trachea, larynx, pharynx, nasal cavities
- Nasal cavities, larynx, pharynx, trachea, bronchi, lungs
- Lungs, bronchi, trachea, pharynx, larynx, nasal cavities
- Nasal cavities, pharynx, larynx, trachea, bronchi, lungs
In your own words explain why some experts recommend that you should breathe through your nose when temperatures are low.
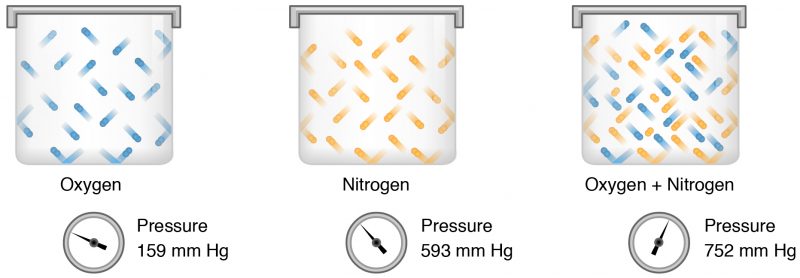
The Role of Gas Pressure in the Respiratory System
Breathing, or ventilation, involves changes in pressure as a result of mechanical work. The physical movement of air into the lungs is a result of the production of differences in total pressure between the interior (alveolar pressure) and exterior (atmospheric pressure) of the respiratory zone. Atmospheric pressure at sea level is typically 1 atmosphere or 760 mmHg, and this value will be used as the reference atmospheric pressure here. One atmosphere is the air pressure that would push a column of mercury up in a thin tube a distance of 760 mm. (Mercury is used because it is a liquid at room temperature, and its density changes very little over pressure and temperature ranges.) In the process of ventilation, air moves down pressure gradients going from an area of higher pressure to an area of lower pressure. Assuming a person is at sea level, if his or her intrapulmonary pressure, the pressure in the alveoli, is less than 1 atm, air enters the lungs and fills the alveoli. If his or her intrapulmonary pressure is greater than 1 atm, then air moves out of the lungs into the environment.
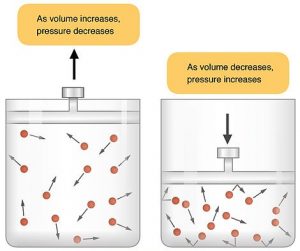
Gases have the property of distributing to fill whatever size and shape container they occupy. If a closed container is made larger (an increase in volume), the total number of gas molecules will stay the same, but they will redistribute to fill the larger space. In doing so, they decrease their concentration (remember that concentration is a property of mass and volume). This increase in volume but not the number of molecules of the gas leads to a corresponding decrease in the pressure exerted by that gas on the walls of the container. If the same closed container is made smaller, the concentration of gases increases( even though the actual number of gas molecules has not changed) and the pressure increases. This is an example of a physical law called Boyle’s Law.
The law is expressed mathematically as:
| P1V1 = P2V2 |
where P = pressure, V = volume, 1 is the initial pressure and volume, and 2 is the resulting pressure and volume.
Boyle’s Law states that, at a constant temperature, the pressure of a gas is inversely proportional to the volume of its container. Very simply, as volume goes up, the pressure goes down, and as volume goes down, the pressure goes up. These properties become important for ventilation because the passage of air into and out of the lungs is controlled by the size of the lungs’ container, the thoracic cavity (thorax). The difference between the example above and the lungs is that the lungs are not a closed system (unless you have a closed glottis), with the opening to the lungs maintained through the conducting zone. But over very short periods of time, Boyle’s law still applies.
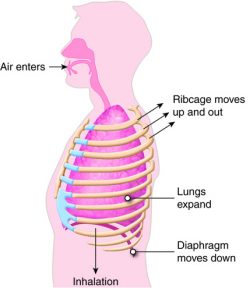
When we inhale, the movement of the diaphragm and the ribs increases the volume of the thorax. This immediately decreases the air pressure within the thorax, creating a pressure gradient between the atmosphere and the alveoli (the latter is called intrapulmonary pressure), and drawing air into the lungs. Air will enter until the atmospheric and intrapulmonary pressures are equal. However, the volume of the thorax remains larger than before the start of inhalation. To exhale, the thorax is allowed to decrease in volume (the ribs and diaphragm return to their original positions), increasing the intrapulmonary pressure and creating a gradient in the opposite direction resulting in the flow of air out to the atmosphere. Changing the size of the thoracic cavity would be impossible if the ribs were solidly attached to the sternum. If they were solidly attached, it would be like trying to move the sides of a birdcage. The costal cartilage allows the ribs to move and expand or contract the chest wall.
Did I Get This 13.2
Choose the correct word, either up or down, to fill in each blank:
As volume goes up, pressure goes _____1_____ , and as volume goes _____2_____, pressure goes up.
Inhalation and Exhalation
 |
 |
Inspiration is the act of inhaling. As stated above, inspiration occurs by increasing the volume of the thorax. This active process involves the use of chest and neck muscles. Resting inspiration is achieved mostly by the movement of the diaphragm. The relaxed shape of the diaphragm resembles a shallow dome with the apex pointing toward the lungs, similar to the shape of an open umbrella. When the diaphragm contracts, it tends to flatten out, expanding the volume of the thorax in an inferior direction. Consequently, the intrapleural and intrapulmonary pressures decrease below atmospheric pressure resulting in air being pulled through the conducting zone and into the lungs. The external intercostal muscles work in conjunction with the diaphragm. The normal orientation of the ribs is around the side of the thorax and angled inferiorly to the sternum. When the external intercostal muscles contract, the ribs are pulled up, also expanding the thoracic cavity in a horizontal direction. In adults, ventilation occurs about 12 times a minute and moves roughly 500 ml of air during each breath. (A deep breath involves a greater shortening of the diaphragm and the external intercostal muscles plus additional contractions of other neck and chest muscles.)
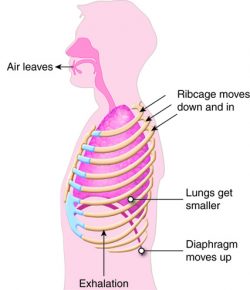
Expiration is the act of exhaling. Resting expiration is a passive process. The muscles used during inspiration relax and allow the chest wall and the diaphragm to move back to their original position, thus decreasing the volume of the thorax and forcing air from the lungs. The compression of the chest wall also aids in moving blood and lymph through the vessels that drain the lungs. Expiration can become an active process when a more forceful exhale is required. In forceful exhalation, the internal intercostal muscles pull the ribs down, helping to compress the chest. The external and internal oblique and transverse abdominal muscles press on the abdominal organs, which move them up against the diaphragm and force the diaphragm higher than it would normally go on relaxation, further decreasing the volume of the thoracic cavity.
Learn By Doing 13.6
Fill in the blanks by selecting the correct word from the table below. (Note that the number in each blank identifies which column to choose from.)
Normal inspiration is a(an) _____1_____ process that primarily relies on the _____2_____ of the _____3_____. By _____4_____ the volume of the thoracic cavity, the pressure _____5_____ allowing air to _____6_____ the lungs. Normal expiration is a(an) _____ 1 _____ process that primarily relies on the _____ 2_____ of the _____ 3 _____.
| 1 | 2 | 3 | 4 | 5 | 6 |
| Passive
Active |
Contraction
Relaxation |
Diaphragm
Internal Intercostals |
Increasing
Decreasing |
Increases
Decreases |
Enter
Exit |
In a situation such as screaming, the process of expiration becomes a(an) ____ 1 _____ process that primarily relies on the _____ 2 _____ of the _____ 3 _____. By _____ 4 _____ the volume of the thoracic cavity more than usual, the pressure _____ 5 _____ even farther, forcing air to _____ 6 _____ the lungs.
| 1 | 2 | 3 | 4 | 5 | 6 |
| Passive
Active |
Contraction
Relaxation |
InternalIntercostals
External Intercostals |
Increasing
Decreasing |
Increases
Decreases |
Enter
Exit |
Respiratory Levels of Organization
Learning Objective
To understand these system-level functions, you will be further exploring structures and processes occurring at all levels of organization. Some examples of major respiratory structures assigned to their structural level of organization of the respiratory system include:
- Chemical level– oxygen, carbon dioxide, bicarbonate, and hydrogen ions
- Macromolecular level– hemoglobin, mucus, and surfactant
- Cellular level– ciliated cells, goblet cells, alveolar cells, and macrophages
- Tissue level– stratified to pseudostratified to simple squamous epithelium
- Organ level– upper respiratory tract, bronchial tree, and lungs
- Organ system level– integration of organs for gas exchange
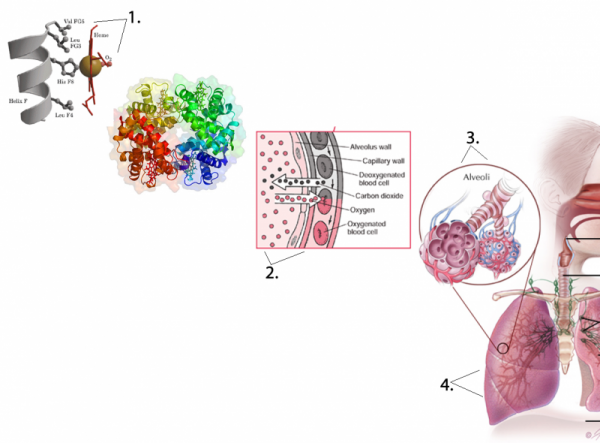
Our bodies exchange oxygen for carbon dioxide at a number of different levels. The mechanics of ventilation drives the exchange of air from the outside environment into the lungs. At a molecular level, oxygen binds to hemoglobin in the red blood cells in the capillaries of the lungs. Some of this oxygen displaces carbon dioxide that was transported from peripheral cells. The exchange of gases occurs in red blood cells (where hemoglobin is concentrated) at the interface of the circulatory system and respiratory system called the respiratory membrane. Oxygen diffuses from the inhaled air in the lungs across the alveolar and capillary membranes and into the blood plasma. It then enters the red blood cells where it will be carried on hemoglobin molecules to the other tissues of the body. Gas exchange at the respiratory membrane is known as external respiration. Gas exchange between the tissues and the blood is internal respiration. At the molecular level carbon dioxide created during cell metabolism diffuses across the cell membrane into the interstitial spaces and extracellular fluid. When it crosses the capillary and red blood cell membrane, some carbon dioxide is picked up by hemoglobin by molecules inside the red blood cell. Inside the cells of the body tissues, oxygen will be used during the process of aerobic cellular respiration. Cellular respiration is a process used by our cells to convert nutrients into energy. The process of aerobic cellular respiration requires oxygen and produces carbon dioxide as a waste product.
Learn By Doing 13.7
Which of the phrases below is associated with ventilation? With internal respiration? With the molecule involved with carrying oxygen and carbon dioxide?With external respiration?
- Gas exchange with tissues
- Gas Transport
- Movement of atmosphere into the body
- Gas exchange with alveoli
How Gases Exchange
Learning Objective
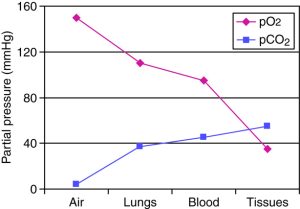
The respiratory system brings in oxygen and exchanges it for carbon dioxide. Oxygen makes up 21% of the air we breathe while carbon dioxide is found at very low levels (0.039%). The diffusion of gases across membranes follows the same principles as the diffusion of solutes in solution across membranes, basically, molecules move down a gradient. The difference is that gases in solution are measured in terms of partial pressure. Partial pressure is the pressure that a given gas in a mixture contributes to the total pressure inside the container or in the atmosphere. The partial pressure is equal to the total pressure times the fraction of the gas.
When we inhale air, all the major components of air are in gas form. However, the oxygen that enters our body must move from the air space in the lungs into the liquids found in our body such as blood plasma and cell cytoplasm. Alternatively, the carbon dioxide in the blood moves from the cell cytoplasm and the plasma into the air of the alveoli.
Exchange of Oxygen and Carbon Dioxide
External Respiration
Air containing oxygen enters the alveoli through the process of ventilation (described earlier). The partial pressure of oxygen in the alveoli is slightly lower than the partial pressure of oxygen found in the atmosphere.
Inhaled air at sea level typically has a partial pressure of oxygen near 160 mmHg. In the alveoli, the partial pressure of oxygen would vary with our ventilation pattern but is typically about 105 mmHg. It is the difference between alveolar oxygen partial pressure and the plasma oxygen partial pressure that drives external respiration across the alveolar membrane. Blood coming through the pulmonary arterial circulation is lower in oxygen, with a typical partial pressure of 40 mmHg. The differential concentration gradient for oxygen to move from the alveolar air into the capillary blood starts at about 65 mmHg (105 mmHg in the alveoli minus 40 mmHg in the blood), providing enough of a difference in partial pressures for oxygen to diffuse from the alveoli into the capillary. Diffusion will occur along the length of the pulmonary capillary until the partial pressures come into equilibrium near 105 mmHg.
The partial pressure of oxygen in the system circulation is slightly lower. As blood enters the left atrium of the heart, a small amount of the pulmonary blood mixes with the bronchial blood that has nourished the lung tissue, lowering the partial pressure so that the actual concentration of oxygen is about 100 mmHg, which is a typical value measured in a sample of arterial blood.
Example: Altitude Sickness
Altitude sickness, also called acute mountain sickness, can strike people climbing to elevations above 8,000 feet (although it typically occurs only at altitudes much higher than this). At elevations high above sea level, there is the same percentage of oxygen (21%) but much less atmospheric pressure. This lowers the partial pressure of the oxygen being inhaled, so less oxygen enters the body. If the body doesn’t adapt well, a person can experience altitude sickness ranging from mild to severe forms. Mild to moderate altitude sickness can cause nausea, vomiting, tachycardia, shortness of breath with exercise, or difficulty sleeping. Mild to moderate cases usually resolve themselves when the person descends to a lower altitude. However, severe cases are another matter. They can result in cyanosis, pulmonary congestion, confusion and stupor, cough with or without blood, a gray or very pale complexion, the inability to walk a straight line, if able to walk at all, and shortness of breath when at rest. These cases require immediate evacuation to lower altitudes. Without treatment, severe altitude sickness may result in death due to pulmonary complications or brain swelling. The good news is that altitude sickness can be prevented. Individuals who climb to extremely high altitudes, like Mount Everest, should do so slowly to allow their bodies to become acclimated to the atmospheric differences.
The functioning of the pressure gradient for carbon dioxide works in the reverse of that for oxygen, with the carbon dioxide partial pressure being higher in the pulmonary arterial blood than in the alveoli. Even with a much smaller gradient for carbon dioxide than for oxygen, nearly as much carbon dioxide diffuses from the blood to the alveoli as oxygen diffuses from the alveoli to the blood because of the much higher solubility of carbon dioxide in the plasma.
Learn By Doing 13.8
Air that enters the lungs from the atmosphere has a_____ 1 _____O2partial pressure than the air in the alveoli of the lungs. The air in the alveoli of the lungs has a slightly lower O2 partial pressure because gas exchange is occurring with the blood and tissues _____ 2 _____ even between breaths. At higher altitudes the partial pressure of oxygen _____ 3 _____ which makes it more difficult for enough oxygen to diffuse into the alveoli of the lungs.
| 1 | 2 | 3 |
| higher
lower |
intermittently
constantly |
increases
decreases |
Internal Respiration
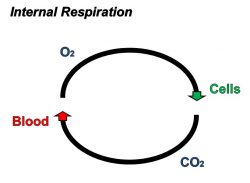
Internal respiration occurs between the blood and systemic tissues of the body. The systemic arteries carry essentially the same concentration of oxygen and carbon dioxide as the pulmonary veins. Oxygen is continually being used by the tissues, and the partial pressure of oxygen in active cells remains below 40 mmHg. Oxygen circulating in the systemic arterial blood readily diffuses across the membranes of the blood vessels into the tissues, replenishing the supply of oxygen in the cells. The final concentration of oxygen and carbon dioxide in the systemic veins is essentially the same as it is in the pulmonary arteries.
Just as the tissues are continually using up oxygen, they are continually producing carbon dioxide. The partial pressure of carbon dioxide in tissues is always greater than 45 mmHg. This accounts for the diffusion of carbon dioxide into the systemic capillaries, raising the pressure to 45 mmHg. The systemic veins carry essentially the same concentration of oxygen and carbon dioxide as the pulmonary arteries.
Learn By Doing 13.9
Choose external respiration, internal respiration, or neither for each of the following:
- The partial pressure of oxygen is higher in the alveoli than the partial pressure of oxygen in the blood plasma. What is this called?
- What is it called when the partial pressure of carbon dioxide is higher in the alveoli than the partial pressure of carbon dioxide in the blood plasma?
- What is it when the partial pressure of oxygen is lower in metabolically active cells than in the blood plasma?
Macromolecules of the Respiratory System
Learning Objective
We will describe 3 macromolecules that are critical to the proper functioning of the Respiratory System: mucus, surfactant, and hemoglobin.
Mucus is a slimy substance secreted by mucus membranes throughout the respiratory system and other organ systems. Mucus formation in the nasal passages and upper respiratory system helps to moisten the air and to trap microorganisms and particles. Throughout the entire respiratory system, mucus helps humidify and buffer the cells that are in direct contact with air. Other organ systems including the digestive, urogenital, visual, and auditory systems use mucus production to protect epithelial cells. While the molecular content varies between organ systems, in general, mucus contains primarily water with enzymes, immunoglobulins (and other immune proteins) salts, and high molecular weight glycoproteins called mucins. Mucins attract large amounts of water. Consequently, mucus serves as a means to maintain local levels of hydration.
Surfactants: At the gas-liquid interface of the alveoli cell membranes, surfactants found in the liquid surface layer lower surface tension. Surface tension arises when water molecules hydrogen bond with each other. The hydrogen bonding of water molecules makes it hard to “pull” the water molecules apart, which must happen for the alveoli to expand. If you have ever tried to pull two wet glass slides apart, you have experienced surface tension created by the hydrogen bonding of water molecules. The molecules in the surfactant interrupt these hydrogen bonds, making it much easier to expand the alveoli during inhalation. The composition of surfactant is 80% phospholipids with the remaining fraction made up of cholesterol and proteins. The alveoli themselves are so small that without the surfactant, the surface tension created by the water on the internal surface of the alveoli would force them to collapse during exhalation.
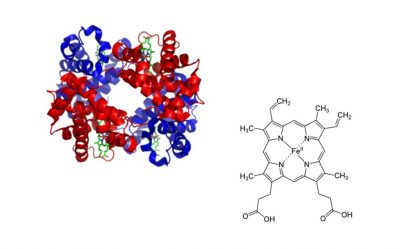 Hemoglobin: The protein used to carry oxygen by nearly all vertebrates is hemoglobin. It functions by binding oxygen in the capillaries of the lungs and carrying it inside red blood cells. When the blood enters capillaries in tissues with a low partial pressure of oxygen, the oxygen will leave the hemoglobin molecule and diffuse into the tissue. Hemoglobin is a complex compound containing two alpha and beta protein chain pairs (globins) and four heme molecules that contain iron in its ferrous (Fe+2) state. Each heme can bind one oxygen molecule, so hemoglobin molecule, because it contains 4 heme groups, can bind up to 4 oxygen molecules. When a hemoglobin molecule is fully bound (saturated) with oxygen, we consider it to be oxyhemoglobin. When it is not fully saturated, it is typically referred to as deoxyhemoglobin, even though it may still have oxygen bound to some of the heme groups. Note that even though an individual hemoglobin molecule can only be 0%, 25%, 50%, 75%, or 100% saturated, we have nearly 300 million hemoglobin molecules in each red blood cell. Collectively they can have any saturation level between 0% and 100%.
Hemoglobin: The protein used to carry oxygen by nearly all vertebrates is hemoglobin. It functions by binding oxygen in the capillaries of the lungs and carrying it inside red blood cells. When the blood enters capillaries in tissues with a low partial pressure of oxygen, the oxygen will leave the hemoglobin molecule and diffuse into the tissue. Hemoglobin is a complex compound containing two alpha and beta protein chain pairs (globins) and four heme molecules that contain iron in its ferrous (Fe+2) state. Each heme can bind one oxygen molecule, so hemoglobin molecule, because it contains 4 heme groups, can bind up to 4 oxygen molecules. When a hemoglobin molecule is fully bound (saturated) with oxygen, we consider it to be oxyhemoglobin. When it is not fully saturated, it is typically referred to as deoxyhemoglobin, even though it may still have oxygen bound to some of the heme groups. Note that even though an individual hemoglobin molecule can only be 0%, 25%, 50%, 75%, or 100% saturated, we have nearly 300 million hemoglobin molecules in each red blood cell. Collectively they can have any saturation level between 0% and 100%.
Example: Respiratory Distress Syndrome of the Newborn Infants
Respiratory distress syndrome of newborn infants (RDS) most commonly affects premature infants whose lungs have not developed fully, children born by cesarean section, and children of diabetic mothers. The lungs of these infants cannot make sufficient quantities of surfactant, making it very difficult for the affected infants’ lungs to expand properly to breathe. Most cases of RDS occur in infants born before 28 weeks gestation as the cells of the lungs responsible for surfactant production, called type II alveolar cells, are generally not very active until later in pregnancy.
Neonates with RDS struggle to breathe, leading to poorly oxygenated blood and cyanosis (the appearance of blue skin). Additional symptoms generally include apnea (periods of breathing cessation) or rapid, shallow breathing. Laboratory procedures can be done to determine the level of fetal lung maturity.
Treatment for RDS often involves the administration of a higher fraction of inhaled oxygen (above the normal 21%), or the use of a ventilator. Artificial surfactant can be given but is still considered experimental. If a premature birth is likely, the expectant mother may be given a steroid such as cortisol to promote maturation of the fetal lungs before birth. The prognosis is dependent upon the severity of the disorder. Children often worsen within the first few days after birth but then usually recover with appropriate treatment.
Learn By Doing 13.10
Mucus lacking _____ 1 _____ would not be able to perform the function of humidifying as well.
The presence of surfactant at the gas-liquid interphase lowers the _____ 2 _____ of the water molecules. This prevents the alveoli from collapsing during _____ 3 _____.
| 1 | 2 | 3 |
| mucins
immunoglobins |
adhesion
surface tension |
inhalation
exhalation |
Identify the parts of hemoglobin. Choose from the following:
- heme
- globin
- iron
The protein part is __________.
The flat (planar) ring structure is __________.
The metal that binds directly to oxygen is __________.
Transport of Oxygen and Carbon Dioxide in the Blood
Learning Objective
Oxygen: Adult humans require about 250 mL of new oxygen to enter the bloodstream per minute to support the internal respiration of their tissues while in a relaxed state. Since oxygen is poorly soluble in our plasma, we do not deliver enough oxygen to our tissues in dissolved form. Therefore we become critically dependent on another mechanism to help deliver sufficient amounts of oxygen to where it is needed. That mechanism utilizes a protein called hemoglobin as a transporter molecule for either oxygen or carbon dioxide. Red blood cells contain high concentrations of hemoglobin.
Forms of Carbon Dioxide: Carbon dioxide is carried in the blood in three forms: dissolved, attached to hemoglobin, and converted to bicarbonate ions. Dissolved CO2 accounts for 7–10 percent of the carbon dioxide carried in the blood. This is also the only form of carbon dioxide that diffuses from the tissues into the blood and from the blood into the alveoli for expulsion from the body. Here, we will examine in depth the transfer of carbon dioxide using hemoglobin or by the formation of bicarbonate.
Carbon dioxide can bind to any protein and form a carbamate compound. The protein found in the highest concentration in red blood cells is hemoglobin, and 20–23 percent of the CO2 carried in the blood is bound to hemoglobin in the form of carbaminohemoglobin. In the capillaries of the systemic tissues, CO2 molecules attach to the hemoglobin molecule. De-oxygenated hemoglobin (hemoglobin with no or less than the maximal oxygen bound, abbreviated HHb), such as that found in metabolically active tissues, binds CO2 easily. In the capillaries of the lungs, the elevated levels of oxygen found in alveoli force the carbon dioxide off the hemoglobin molecule. Although some carbon dioxide is transported as carbaminohemoglobin, the majority, about 70 percent, is dissolved in the blood as bicarbonate ions that arise from the reversible reactions discussed below.
Carbon dioxide in the presence of water can be reversibly converted to carbonic acid. Carbonic acid is not very stable and readily dissociates into a hydrogen ion and a bicarbonate ion. In fact, this is why carbonated beverages are acidic. Carbon dioxide is added to the drink mixture under pressure and dissolves in the beverage. When the CO2 has bubbled out of the beverage, it tastes flat because the acid is gone. The same thing happens in red blood cells, except that red blood cells contain an enzyme called carbonic anhydrase (CA), which is capable of facilitating one million reactions per second per enzyme molecule. Because of the enzyme, most of the CO2 dissolved in the blood is quickly converted to carbonic acid which breaks down to form hydrogen ions and bicarbonate ions.
The chemical reaction for this process is the following:
|
CO2 (in the presence of CA) + H2O ⇆ H2CO3 ⇆ H+ + HCO3– |
Where H2O is water, CA is carbonic anhydrase, H2CO3 is carbonic acid, H+ is a hydrogen ion, and HCO3– is a bicarbonate ion. The second part of the reaction, which produces the hydrogen and bicarbonate ions, does not have an enzyme but depends on the dissociation of the weak acid. This series of reactions provides buffering for the blood, maintaining blood pH within a narrow range. Deviation from this range compromises organ function and can cause death.
Carbon dioxide production occurs in many tissues, especially muscle. The carbon dioxide produced diffuses from the tissue of origin into a systemic capillary and dissolves in the plasma. A small amount of carbon dioxide is transported this way. Most of the CO2 that diffused into the plasma diffuses into a red blood cell and reacts with intracellular water molecules to produce hydrogen and bicarbonate ions.
This work by Cenveo is licensed under a Creative Commons Attribution 3.0 U.S.
When the blood enters the pulmonary capillaries, gaseous carbon dioxide in the plasma diffuses into the alveoli. Some of the bicarbonate diffuses from the plasma into the red blood cells, and a chloride ion passes back into the plasma, reversing the chloride shift that occurred in the capillaries in the systemic tissues. The high partial pressure of oxygen in the alveoli causes the carbaminohemoglobin to dissociate into deoxyhemoglobin, a hydrogen ion, and a molecule of carbon dioxide. The released CO2 is available for diffusion. The free hydrogen ion combines with a bicarbonate ion and reforms carbonic acid. The carbonic acid is converted back to carbon dioxide and water under the influence of carbonic anhydrase.
Learn By Doing 13.11
Carbon dioxide is carried in the blood in three different forms. Which form is least common and can diffuse from the tissues into the blood?
- Converted to bicarbonate ions
- Dissolved
- Attached to hemoglobin
Cells of the Respiratory System
Learning Objective
Epithelial Cell Types
Respiratory epithelial cells include three types: a) ciliated cells, b) goblet cells, and c) basal cells. Ciliated cells have cilia on the surface; Goblet cells, shaped like a wine goblet, secrete mucus. Basal cells, found at the basal region of epithelial sheets, are stem cells used to regenerate and maintain a healthy epithelial cell layer.
The apical surfaces of ciliated epithelia cells possess specialized structures called cilia. Depending upon the tissue cilia may function in either sensory or mechanical capacities. The cilia in the nasal cavity and bronchial tree sweep mucus toward the pharynx to be swallowed or expectorated. Swallowing delivers the microorganisms and particles that were trapped in the mucus to the stomach where the low pH of the stomach will destroy them.
 (Credit: Cenveo, CC BY) |
 (Credit: Cenveo, CC BY) |
The respiratory system interacts with the external environment during ventilation. This interaction can provide contact with pathogens (viruses, bacteria, and other disease-causing organisms), atmospheric debris, and other particulates. We have already covered how sticky mucus traps many pathogens and particles and facilitates removal from the body. Yet the mucus does not trap all inhaled particles. Alveolar macrophages, a type of immune system cell typically remove particles that make it to the level of the alveoli through the process of phagocytosis.
In the alveoli, there are specialized epithelial cells called alveolar cells. Type I alveolar cells are very thin squamous cells through which gases easily diffuse. These cells are so thin that they can only be seen through the use of an electron microscope. Scattered among the squamous cells are type II alveolar cells. Type II alveolar cells are cuboidal epithelial cells with microvilli on their apical surface. These cells make and secrete surfactant, which decreases the surface tension on the alveolar surfaces. The alveoli themselves are so thin that without the surfactant the force of surface tension created by the water on the cell surfaces would cause the alveoli to collapse upon exhalation. Mixed in among the types I and II alveolar cells are macrophages that migrate within the sacs and clean up material that has entered this part of the system. These cells may accumulate and sequester non-biodegradable material that persists in the cells. Cells that contain accumulated material are referred to as dust cells. The alveoli are considered to be functionally sterile due to the combination of the mucus and cilia found through most of the respiratory membranes and the macrophages in the alveoli.
Epithelial Types Throughout the Respiratory System
In the nasal cavities and upper respiratory tract, epithelial cells are primarily ciliated psuedostratified columnar epithelium. The bronchial tree is lined with pseudostratified, ciliated, columnar epithelia with goblet cells dispersed among the columnar cells. At the terminal bronchioles, epithelial become ciliated cuboidal cells without any goblet cells.
Anatomy of the Respiratory-Cardiovascular Junction
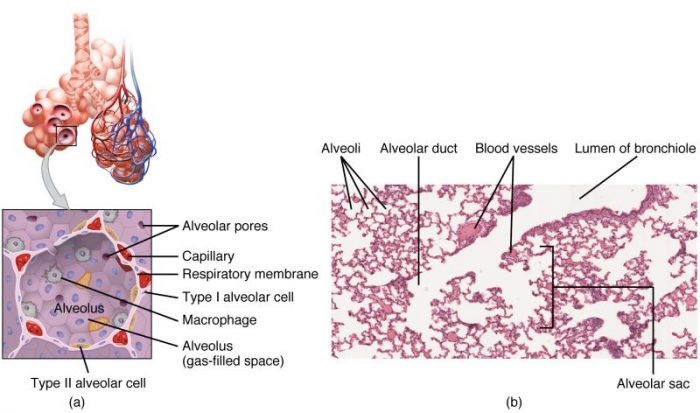
There is intimate contact between respiratory tissue and the blood supply in the lungs. Alveolar sacs in the lungs are wrapped in capillary beds of the cardiovascular system. At the cellular level, the simple squamous alveolar cells are in close contact with the capillaries, which are also one endothelial cell thick.
Oxygen from the inhaled air diffuses from the alveoli to the hemoglobin in the red blood cells. In order to do so, it has to diffuse through the alveolar epithelial cell, the capillary endothelial cell, plasma in the capillary, and into the red blood cell.
Respiratory Levels of Organization Summary
The major function of the respiratory system is to obtain oxygen needed to convert nutrients to energy and to remove carbon dioxide which is a waste product of this reaction. In order to perform this function, the respiratory system must have mechanisms for moving oxygen into the body from the atmosphere and a way to transport the oxygen to tissues throughout the entire body. The respiratory system must also transport carbon dioxide to the lungs to be expelled from the body. Additionally, the respiratory system plays a role in protecting the body from microorganisms and maintaining proper pH levels.
The primary function of the respiratory system, the exchange of oxygen and carbon dioxide, occurs through several processes.
- Ventilation moves air in and out of the lungs.
- External respiration exchanges oxygen and carbon dioxide between the air and the alveoli of the lungs.
- Internal respiration exchanges oxygen and carbon dioxide between the blood and tissues.
- Aerobic cellular respiration uses oxygen to release energy from nutrients.
- To understand how the respiratory system functions, it is studied at the chemical, macromolecular, cellular, tissue, organ, and organ system levels.
- The role of partial pressure in the diffusion of gases in external and internal respiration helps explain why oxygen and carbon dioxide are transported differently.
- The macromolecule level relates the structure of the macromolecules to their functions.
- Mucus- immunoglobulin for immune function, mucin proteins for hydration
- Surfactant- phospholipids that disrupt the surface tension of water in the alveoli to prevent collapse.
- Hemoglobin- iron-containing heme group to transport oxygen and carbon dioxide.
- Transport of oxygen on hemoglobin- the benefit of a tight association and factors that will affect the affinity of hemoglobin for oxygen
- Transport of carbon dioxide as carbaminohemoglobin and bicarbonate as well as the role of carbonic anhydrase
- There are several important cell types that are found in different locations of the respiratory system.
- Epithelial cell types located in the respiratory tree include goblet cells that secrete mucus, ciliated cells that sweep mucus into the pharynx, and basal cells which can regenerate and produce new layers of cells.
- Macrophages located in the lungs will help to provide protection against pathogens.
- Epithelial cells in the alveoli are divided into simple squamous Type I cells that allow for diffusion and also secrete angiotensin-converting enzyme and cuboidal Type II cells that secrete surfactant.
In order to understand how the respiratory system functions, it is important to understand how the different organizational levels function both independently and together. Different portions of the respiratory system contain different cell types that all work together to allow for the diffusion of oxygen and carbon dioxide while providing protection from pathogens.
Respiratory Homeostasis
Learning Objective
The primary physiologic functions of the respiratory system are to provide oxygen for cellular metabolic processes and to remove the gaseous waste product carbon dioxide. When there is an increased need for oxygen (best observed during rigorous exercise), our respiratory system responds with an increased rate and depth of breathing. In response to the adrenal hormone epinephrine, the bronchioles will also dilate, making it easier to move this increased volume in and out. With concurrent increases in cardiac output, we can typically meet our increased demands of those tissues with increased metabolic rates. Most of us do not make a conscious decision to increase our alveolar ventilation, and the sympathetic nervous system does not control the diaphragm. Dilating the airways increases the rate at which air can move in and out but does not affect volume.
Even when there is no need for an increase in oxygen levels in the tissues, the respiratory system will respond with increased ventilation if carbon dioxide levels start to increase. Increased carbon dioxide levels can occur in various forms of metabolic acidosis, where imbalances in metabolism lead to increased carbon dioxide levels in the body. Increased ventilation helps rid the body of carbon dioxide and limits the changes in pH the body would otherwise experience with the rising carbon dioxide levels.
Example: Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a chronic, debilitating disease. COPD is a set of symptoms that can develop as a result of either chronic bronchitis or emphysema. People with chronic bronchitis constantly produce mucus in the conducting division in response to inhaled irritants or mild infections Emphysema is the permanent result of the progressive destruction of lung tissue. It is typically a more severe form of COPD than bronchitis and may lead to death. The leading cause of both conditions is tobacco smoke, inhaled as either first-hand or second-hand smoke. Occasionally, emphysema can develop as a result of exposure to gases or fumes in the workplace. There is a low incidence of COPD resulting from a deficiency of the protein alpha-1-antitrypsin.
The symptoms of COPD include a cough with or without mucus, fatigue, frequent respiratory infections, shortness of breath (dyspnea), the inability to catch one’s breath, and wheezing. As the disease progresses, patients may have more symptoms which can progress in severity. Evaluating Lung sounds and X-rays are not necessarily useful in establishing a diagnosis for COPD. Spirometry and the examination of arterial blood gases to determine the blood concentrations of oxygen and carbon dioxide provide much better diagnostic tools.
As COPD worsens, blood oxygen levels decrease, and blood carbon dioxide levels increase. The decreased oxygen leads to fatigue, dizziness, and decreased activity tolerance these people often experience. The increase in carbon dioxide can lead to respiratory acidosis, ultimately contributing to dysfunction in many of the body’s metabolic pathways.
There is no cure for COPD, but medications can help alleviate its effects. Inhalers that cause bronchodilation and contain steroids to reduce inflammation and mucus secretion are effective in many cases. Other anti-inflammatory medications may also help. If the conditions become severe, steroids can be administered orally or by intravenous methods. Oxygen may be needed, and mechanical breathing assistance may be used.
Additional information is available at the following site: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001153
Learn By Doing 13.12
As a person exercises their muscles require more energy. To produce energy, the muscles require more oxygen. The respiratory system responds to this need by increasing the rate of respiration. Additionally, in response to the epinephrine produced during exercise, the _____ 1 _____ will _____ 2 _____ making it easier to move an increased volume in and out of the lungs.
In addition to providing the body with an increased supply of oxygen, the respiratory system must also maintain the homeostasis of blood pH. If the pH of the blood rises above 7.45, it can result in respiratory alkalosis. If the pH of the blood falls lower than 7.35, the result is respiratory acidosis. If the level of carbon dioxide in the blood increases with no homeostatic influence from the respiratory system, it could result in _____ 3 _____.
Hyperventilating occurs when a person is breathing too fast. This results in the release of too much carbon dioxide. The release of too much carbon dioxide would result in _____ 3 _____.
| 1 | 2 | 3 |
| bronchioles
trachea |
constrict
dilate |
respiratory alkalosis
respiratory acidosis |
Respiratory Integration
With the respiratory system’s constant interaction with our external environment, it is considered a portal of entry for irritants and microorganisms. Protection of the body from these entering substances involves multiple forms of defense.
The epithelia of the upper respiratory tract contain goblet cells that produce mucus that lines the nasal cavity and most of the bronchial tree. The mucus helps to moisten the air and to trap microorganisms and particles. Mucus also contains immunoglobulin molecules which can bind pathogens and signal immune cells if needed. The cilia on respiratory epithelial cells of both the upper (above the larynx) and lower (below the larynx) respiratory tracts beat toward the pharynx creating the mucociliary elevator so that the mucus and trapped material can be swallowed. Swallowing delivers the microorganisms and particles to the stomach for destruction in stomach acid. Nerves and blood vessels underlie the epithelia in the nasal cavity. Sensory receptors can be stimulated by inhaled caustic material, resulting in the reflex called sneezing which rids these materials from the respiratory tract. At the level of the alveoli, phagocytic macrophages ‘patrol’ the lung tissues for invaders that have made it deeper into the respiratory system.
*
“Learn By Doing” and “Did I Get This?” Feedback
Did I Get This 13.1
Replace the numbers in the sentences below with a word from the numbered column.
The main function of the respiratory system is to obtain _____oxygen_____ from the air to be used to convert _____nutrients_____ to _____energy_____. The respiratory system also needs to remove _____carbon dioxide_____from the blood.
Learn By Doing 13.1
Identify the upper respiratory tract structures in the image.
1 = nasal cavity, 2 = oropharynx, 3 = epiglottis, 4 = laryngeopharnyx, 5 larynx
How would air entering the lungs be different without the nasal cavity? The nasal cavity contains structures such as hair, sebaceous glands, and mucus that aid in preventing microorganisms from entering. The conchae of the nose contain mucus glands and blood vessels to aid in humidifying and warming the air. The paranasal sinuses are hollow areas that make the skull lighter and also moisten and warm incoming air. Thus, without the nasal cavity, air entering the lungs would be more likely to contain pathogens and debris. It would also be colder and less humid. All 3 of these changes could cause lung dysfunction.
If a person has an injury to the epiglottis, what would be the physiological result?
The epiglottis is a region of the larynx that is important during the swallowing of food or drink. As a person swallows, the pharynx moves upward, and the epiglottis closes over the trachea, preventing food or drink from entering the trachea. If a person’s epiglottis were injured, this mechanism would be impaired. As a result, the person may have problems with food or drink entering the trachea and possibly, the lungs. Over time, this may cause infections such as pneumonia to set in.
Learn By Doing 13.2
Examine the image of the tree below. Replace the numbers in the paragraph below with one of the phrases in this table.
| Numbers 1, 3, 5 | Numbers 2, 4, 6 |
 |
| Trachea Bronchioles Bronchi |
Cartilage No Cartilage C-shaped rings of cartilage |
The trunk of this tree would represent the ___trachea____ which requires ___C-shaped rings of cartilage___ to remain open. The split in the tree that leads to the two primary branches would represent the ___Bronchi____ which requires ____Cartilage____ to remain open. The smallest branches of the tree would represent ____Bronchioles____ which requires _____No Cartilage____ to remain open.
Learn By Doing 13.3
Consider what occurs to cause “Smoker’s cough.” Based on this description, the function of the cilia is to move ___Mucus____ up and out of the lungs. If the cilia are paralyzed or destroyed by chemicals in cigarettes, the body must ___Cough____ to remove mucus from the lungs. If mucus is not removed from the lungs, microorganisms can grow in it. This may lead to __Pneumonia__.
Learn By Doing 13.4
In your own words, describe the function of the pleura.
Learn By Doing 13.5
Replace the numbers in the paragraph below with one of the following words:
- External respiration
- Ventilation
- Conducting zone
- Respiratory zone
- Cellular Respiration
- Internal respiration
___Ventilation__ is the movement of air into the body and the movement of air back out of the body. The channel for moving air into the lungs and back out is referred to as the ___conducting zone___. Gas exchange in the lungs is called ___external respiration___, and the location where this gas exchange occurs is called the ___respiratory zone___. After oxygen-enriched blood is transported through the body, ___internal respiration___ occurs. This process then allows ___cellular respiration___.
Decide whether each of the statements below describes the conducting zone or the respiratory zone of the respiratory tract.
- Responsible for warming and humidifying air entering the body: conducting zone
- Allows for the passage of air from inside the body to outside the body: conducting zone
- Allows for gas exchange between the lungs and the blood: respiratory zone
Which of the following is the correct order that air passes through structures in the respiratory system during inspiration?
- Lungs, bronchi, trachea, larynx, pharynx, nasal cavities
- Nasal cavities, larynx, pharynx, trachea, bronchi, lungs
- Lungs, bronchi, trachea, pharynx, larynx, nasal cavities
- Nasal cavities, pharynx, larynx, trachea, bronchi, lungs
In your own words explain why some experts recommend that you should breathe through your nose when temperatures are low.
Our Answer: Cold air holds less water vapor. The structures of the nasal cavity are able to warm and humidify incoming air. This is especially important when the air is cold. Breathing through the mouth bypasses the major mechanisms used to moisten and warm air. Gas exchange between the air inside the lungs and the bloodstream is most efficient within a certain range of temperature and humidity.
Did I Get This 13.2
Choose the correct word, either up or down, to fill in each blank:
As volume goes up, pressure goes _____down_____ , and as volume goes _____down_____, pressure goes up.
Learn By Doing 13.6
Normal inspiration is a(an) _____active_____ process that primarily relies on the _____contraction_____ of the _____diaphragm_____. By _____increasing_____ the volume of the thoracic cavity, the pressure ___decreases_____ allowing air to _____enter_____ the lungs. Normal expiration is a(an) _____ passive _____ process that primarily relies on the _____relaxation_____ of the _____diaphragm _____.
| 1 | 2 | 3 | 4 | 5 | 6 |
| Passive Active |
Contraction Relaxation |
Diaphragm Internal Intercostals |
Increasing Decreasing |
Increases Decreases |
Enter Exit |
In a situation such as screaming, the process of expiration becomes a(an) ____active_____ process that primarily relies on the _____contraction _____ of the _____ internal Intercostals _____. By _____decreasing _____ the volume of the thoracic cavity more than usual, the pressure _____increases _____ even farther, forcing air to _exit_ the lungs.
| 1 | 2 | 3 | 4 | 5 | 6 |
| Passive Active |
Contraction Relaxation |
InternalIntercostals External Intercostals |
Increasing Decreasing |
Increases Decreases |
Enter Exit |
Learn By Doing 13.7
Which of the phrases below is associated with ventilation? With internal respiration? With the molecule involved with carrying oxygen and carbon dioxide? With external respiration?
- Gas exchange with tissues: internal respiration
- Gas Transport: hemoglobin
- Movement of atmosphere into the body: ventilation
- Gas exchange with alveoli: external respiration
Learn By Doing 13.8
Air that enters the lungs from the atmosphere has a_____higher _____O2 partial pressure than the air in the alveoli of the lungs. The air in the alveoli of the lungs has a slightly lower O2partial pressure because gas exchange is occurring with the blood and tissues _____constantly _____ even between breaths. At higher altitudes, the partial pressure of oxygen _____decreases _____ which makes it more difficult for enough oxygen to diffuse into the alveoli of the lungs.
| 1 | 2 | 3 |
| higher lower |
intermittently constantly |
increases decreases |
Learn By Doing 13.9
Choose external respiration, internal respiration, or neither for each of the following:
- The partial pressure of oxygen is higher in the alveoli than the partial pressure of oxygen in the blood plasma. What is this called? external respiration, In external respiration the partial pressure difference between the alveoli and the blood plasma allows oxygen to diffuse from the area of higher pressure in the alveoli into the blood plasma.
- What is it called when the partial pressure of carbon dioxide is higher in the alveoli than the partial pressure of carbon dioxide in the blood plasma? neither, If the partial pressure of carbon dioxide remained higher in the alveoli than the partial pressure of carbon dioxide in the blood plasma carbon dioxide would diffuse into the bloodstream. One of the main functions of respiration is to remove excess carbon dioxide from the body.
- What is it when the partial pressure of oxygen is lower in metabolically active cells than in the blood plasma? internal respiration, Internal respiration relies on the partial pressure of oxygen being lower in metabolically active cells so it can diffuse from the blood into the tissues.
Learn By Doing 13.10
The presence of surfactant at the gas-liquid interphase lowers the _____surface tension _____ of the water molecules. (Surface tension occurs because of the hydrogen bonding between water molecules. Surfactant contains phospholipids which can help disrupt the hydrogen bonding.) This prevents the alveoli from collapsing during _____exhalation _____.
| 1 | 2 | 3 |
| mucins immunoglobins |
adhesion surface tension |
inhalation exhalation |
Identify the parts of hemoglobin. Choose from the following:
- heme
- globin
- iron
The protein part is globin.
The flat (planar) ring structure is heme.
The metal that binds directly to oxygen is iron.
Learn By Doing 13.11
Carbon dioxide is carried in the blood in three different forms. Which form is least common and can diffuse from the tissues into the blood?
- Converted to bicarbonate ions: Incorrect. Most of the carbon dioxide (about 70-80%) is converted to bicarbonate ions and transported in the blood plasma.
- Dissolved: About 7-10% of carbon dioxide is carried in the blood plasma as a dissolved gas. This is the form of carbon dioxide that can diffuse from the tissues into the blood.
- Attached to hemoglobin: Incorrect. Between 20%-23% of carbon dioxide is attached to hemoglobin molecules.
Learn By Doing 13.12
Hyperventilating occurs when a person is breathing too fast. This results in the release of too much carbon dioxide. The release of too much carbon dioxide would result in _____respiratory alkalosis _____. (Alkalosis occurs when the blood becomes too basic. When carbon dioxide normally reacts with water to create carbonic acid in the blood. If too much carbon dioxide is released, it can lower the acidity of the blood and increase the pH, resulting in alkalosis.)
| 1 | 2 | 3 |
| bronchioles trachea |
constrict dilate |
respiratory alkalosis respiratory acidosis |
