Chapter 11: Immune System, Infectious Diseases, and STD’s/STI’s
How does the immune system fight off disease?
What are the different kinds of organisms that cause disease?
What can you do to try to stop the spread of diseases?
How do you know if you have an STD?
Chapter Learning Outcomes
By the end of this chapter you will be able to:
- List the common types of pathogens (disease causing agents)
- Describe how the Immune system works to fight off infection
- Compare the role of the various types of immune cells
- Explain how vaccines work
- Explain the signs and symptoms of the most common STD’s/STI’s
The Immune System
Imagine a number that is ten billion times the number of stars in the universe, this is the estimated number of viruses on Earth[1]. Viruses are just one type of microorganism in our environment. Some microorganisms are detrimental to our health making us sick, others are important for our health (beneficial), and others are inconsequential. The microorganisms that cause diseases in humans are called pathogens. In total, there are about 1,400 known species of human pathogens that fall into five groups known as bacteria, virus, fungi, protozoa, and helminths (worms).
Pathogens are found in the air around us, the food we eat, what we drink, and the people and animals we are around, thus we are constantly exposed pathogens. Thankfully our immune system is in a constant battle working to identify the foreign invader (pathogen) and destroy them. This immune system battle is happening right now while you are reading this book!
The main purpose of the immune system is to protect your body from harmful substances, germs and cell changes that could make you ill. With this purpose, the immune system works to:
-
fight disease-causing germs (pathogens) like bacteria, viruses, parasites or fungi, and to remove them from the body,
-
recognize and neutralize harmful substances from the environment, and
-
fight disease-causing changes in the body, such as cancer cells.
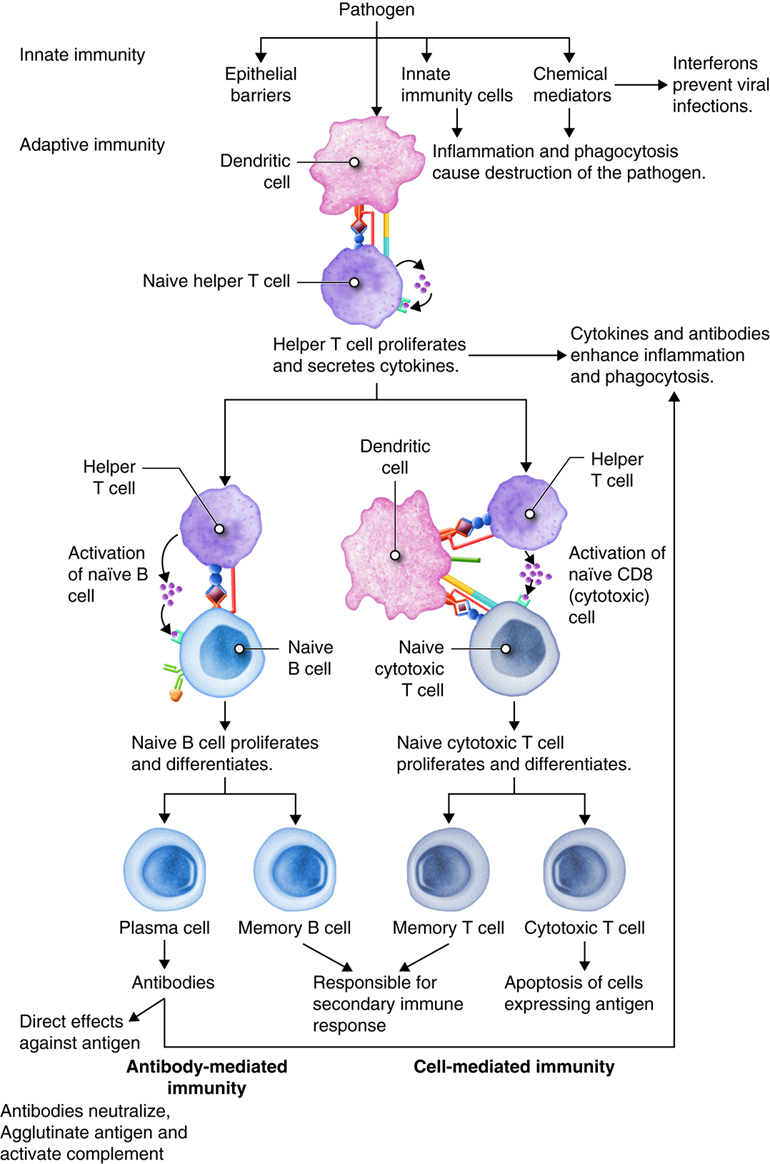
Your immune system is made up of two parts that work together to fight off disease. The innate immune system works to constantly find and destroy any foreign invaders, and the adaptive immune system works by remembering previous pathogens and infections to be able to launch a more efficient battle to destroy pathogens upon re-exposure.
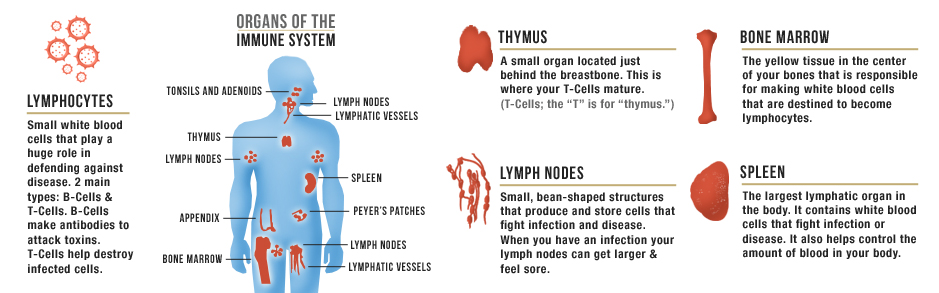
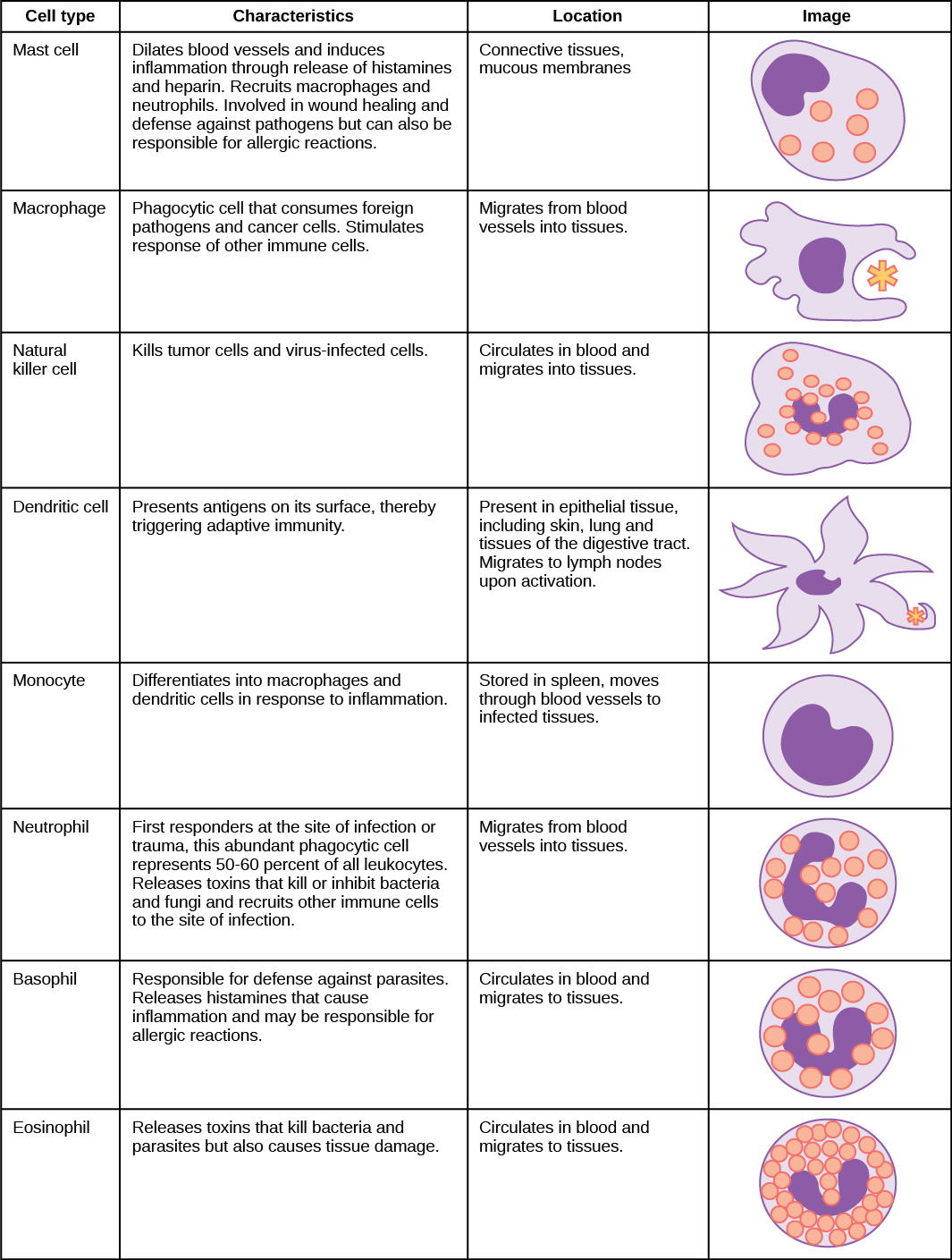
The immune system includes white blood cells, organs, and tissues of the lymph system, such as the thymus, spleen, tonsils, lymph nodes, lymph vessels, and bone marrow. The white blood cells, or immune cells, that help the body fight infections and other diseases include neutrophils, eosinophils, basophils, mast cells, monocytes, macrophages, dendritic cells, natural killer cells, and lymphocytes (B cells and T cells).
The immune system is an amazing system of protection, however sometimes it cannot destroy the pathogen and this is when infection or disease occurs, like the Flu, Strep Throat, or a Sexually Transmitted Disease (STD).
Pathogens and Infectious Diseases
The number of viruses and bacteria on earth is staggering[2] and they occupy essentially every environment. For example, a liter of surface seawater typically contains in excess of ten billion bacteria and 100 billion viruses. The vast majority of viruses and bacteria we are exposed to have no negative effect, some can even be beneficial, however a tiny fraction of these can severely affect our health. It is estimated that only about 1,400 of a trillion microbial species are human pathogens. Pathogens are too small to be seen by the naked eye and they live all around us in water, soil, and air.
The agents that cause disease, or pathogens, fall into five groups: viruses, bacteria, fungi, protozoa, and helminths (worms). Protozoa and worms are usually grouped together as parasites.
| Virus | Bacteria | Fungi | Parasites/Protozoa |
|
|
|
|
Common Viruses and Mutations
Every year warnings are shared about the annual flu season. The flu is a contagious respiratory illness caused by the influenza viruses that infect the nose, throat, and lungs. It can cause mild to severe illness, and at times can lead to death. Although the flu can be caught year round, in the U.S. it is most common in the Fall and Winter seasons. The flu virus is not the same each year due to what is known as antigenic drift and antigenic shift which essentially indicates that the influenza virus has changed and thus the body will likely react differently to the variations.
Viruses can only replicate if they are absorbed by cells in the body, thus viruses survive based on the ability to continue to infect hosts. In order to continue to infect humans, the virus has to overcome the humans immune systems. Since the immune system can remember past viral infections, viruses mutate and change over time to be able to adapt to their surroundings and more effectively move from host to host. When viruses mutate they evolve into new variants. Virus variants are similar to a family tree with multiple lineages (or closely related groups of variants) and sublineages. Each variant starts with a parent lineage followed by descendant lineages. For example, with COVID-19, the BA.1.1.529 variant is from the Omicron variant.
Pandemics
There is a difference between an endemic, outbreak, epidemic, and pandemic[3]. An endemic condition occurs at a predictable rate among a population. An outbreak corresponds to an unpredicted increase in the number of people presenting a health condition or in the occurrence of cases in a new area. An epidemic is an outbreak that spreads to larger geographic areas. A pandemic is an epidemic that spreads globally.
Pandemics have occurred throughout history impacting the entire world, some of these include:
- Three plagues during the years: 541-543, 1347-1351, and 1885-ongoing.
- Six pandemics of cholera during the years: 1817-1824, 1827-1835, 1839-1856, 1863-1875, 1881-1886, and 1899-1893.
- And numerous flu pandemics: Russian flu from 1889-1893, Spanish flu from 1918-1919, Asian flu from 1957-1959, Hong Kong flu from 1968-1970, SARS from 2002-2003, Swine flu from 2009-2010, MERS from 2015-ongoing, and more recent COVID-19 from 2019-ongoing.
The COVID-19 pandemic was caused by a virus called SARS-CoV-2. Viruses constantly change through mutation and sometimes these mutations result in a new variant of the virus. COVID variations include the Omicron variant and Delta variant, with new variants of the virus expected to occur. The COVOD-19 pandemic is the first global pandemic requiring large-scale responses since the 1918 Spanish flu. As of 2022, COVID-19 is still considered a pandemic and there is still concern of continued spread, sickness, and death.
The Chain of Infection
The way in which people become infected with a pathogen is referred to as the Chain of Infection.
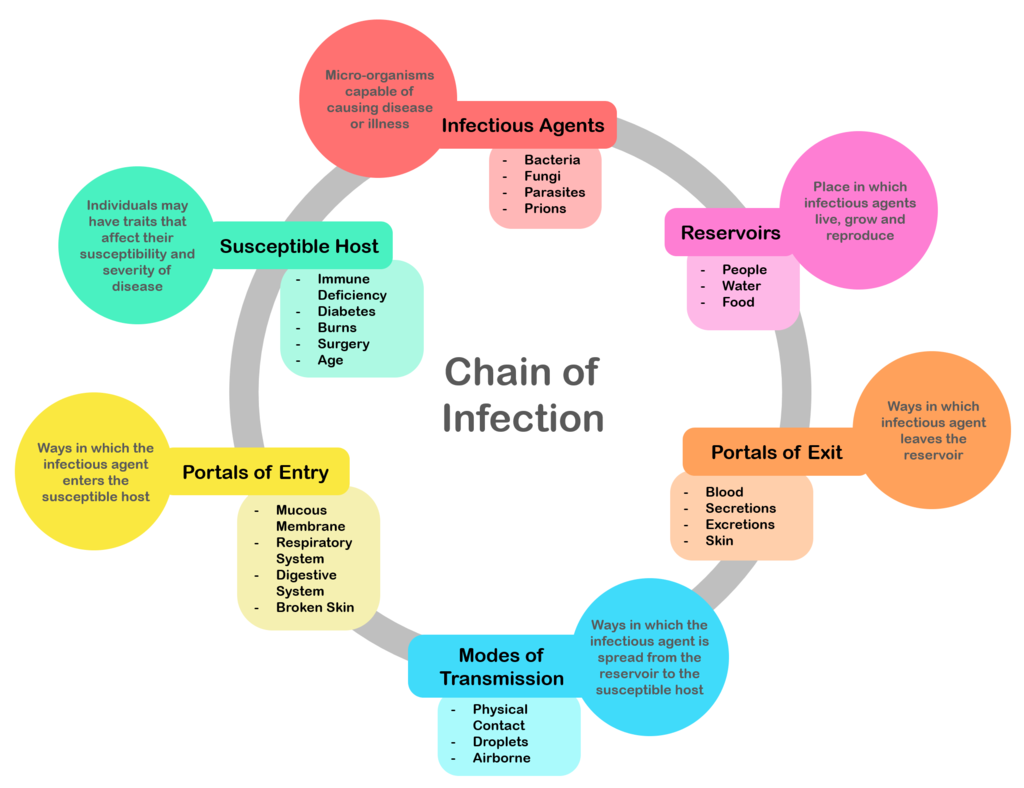
The chain of infection begins with the “Infectious Agent.” The infectious agent is a pathogen, a microorganism that is capable of causing disease. There are about 1,400 different pathogens that fall within five main categories of bacteria, virus, fungi, protozoa, and worms.
The infectious agent begins in a “Reservoir.” The reservoir could be another person, an animal, in water, or in food; it is the habitat in which the infectious agent normally lives, grows, and multiplies. The reservoir may or may not be the source from which an agent is transferred to a host. For example, the reservoir of Clostridium botulinum is soil, but the source of most botulism infections is improperly canned food containing C. botulinum spores. Human reservoirs may or may not show the effects of illness. A carrier is a person with inapparent infection who is capable of transmitting the pathogen to others. Asymptomatic or passive or healthy carriers are those who never experience symptoms despite being infected. Carriers commonly transmit disease because they do not realize they are infected, and consequently take no special precautions to prevent transmission.
The infectious agent needs a way to leave the reservoir through a “Portal of Exit.” For a person, this could include breathing out air, or a cut through the skin, touching or rubbing your nose, coughing, sexual intercourse, feces, urine, mucus, or blood.
The infectious agent then needs a “Mode of Transmission” to the new host. The mode of transmission could be direct or indirect. Direct contact and direct spreading of droplets often occur when two people are close together or touching, this could be through hugging, sexual intercourse, or droplets spreading when talking or sneezing when someone is close by. Indirect transmission could occur through the air, on a vehicle such as food or drinks, or transmitted by an insect like a mosquito, flee, or tick.
The infectious agent then needs to a “Portal of Entry” into the new susceptible new host, these are ways the infectious agent could enter the body. The portal of entry must provide access to tissues in which the pathogen can multiply. This might include inhaling the infectious agent into the respiratory system, consuming it through food or drink therefore entering the digestive system, or entering directly into blood or tissues through breaks in the skin.
The final step in the Chain of Infection is when the infectious agent has successfully entered the Susceptible Host. If a pathogen gets past a host’s defenses, it will attempt to infect the host and begin replicating itself; The pathogens must infect a host in order to grow or replicate. However, just because the pathogen has successfully entered the host does not mean they will get infected! This is where the power of the immune system steps in to fight off the infection destroying the infectious agent.
The survival of human pathogens, like viruses, bacteria, and parasites, is dependent upon quickly invading a human, replicating, and efficiently transmitting to others. Pathogens depend on the chain of infection for survival. You can take precautions to break the chain of infection at each step in the chain by doing the following:
- Recognize signs and symptoms of disease in order to get treatment and isolate when needed.
- Wash your hands and/or use hand sanitizer
- Cleaning and disinfect surfaces
- Get treatment from a doctor
- If you have a bacterial infection you need antibiotics. Antibiotics are medicines that fight bacterial infections.
- Avoid touching your face
- Do not cough into your hand, cough into your arm or elbow.
- Use pest control
- Wear personal protective equipment to put a barrier between the portal of exit or entry.
- Use air purifiers to reduce airborne pathogens.
- Properly dispose of waste.
- Drink clean drinking water.
- Follow food safety guidelines.
- Immunizations/vaccines to reduce the susceptibility of the new host.
The Immune System Battle
When an infectious agent leaves a reservoir through a portal of exit and finds a mode of transmission, it is then up to the defenses of the new host to try to reduce the chances of infection. This is when the immune system battle commences which includes two main subsystems of the immune system, called the innate immune system and the adaptive immune system. The innate immune system is what you are born with and the adaptive immune system is developed overtime as your body is exposed to pathogens. The innate immune response is always present and attempts to defend against all pathogens rather than focusing on specific ones. Conversely, the adaptive immune response stores information about past infections and mounts pathogen-specific defenses.
The innate immune system includes the bodies physical and chemical barriers along with white blood cells that are always present in the blood and tissues ready to destroy any and all invading pathogens. The adaptive immune system also includes white blood cells, but they are more specialized and ready to destroy specific pathogens.
Immune System: Physical and Chemical Barriers
The first step in the battle against pathogens is to put up a physical barrier against the portal of entry. The largest physical barrier against pathogens is our skin. Skin provides provides both a barrier of entry and a means to destroy pathogens through skin acidity and dryness. The areas of the body that are not covered with skin have alternative methods of defenses using mucus and secretions, like tears in the eyes, wax in the ears, and cilia and mucus in the nose, mouth, and lungs. Despite these barriers, pathogens may enter the body through skin abrasions or punctures, or by collecting on mucosal surfaces in large numbers that overcome the mucus or cilia. Some pathogens have evolved specific mechanisms that allow them to overcome physical and chemical barriers. When pathogens do enter the body, the innate and adaptive immune systems responds.
The Innate and Adaptive Immune System
The main job of the innate immune system is to fight harmful substances and germs that enter the body, for instance through the skin or digestive system. The innate immune system is the rapid response to any invading pathogen, the response is non-specific meaning the same response for any and all pathogens. The adaptive immune system makes antibodies and uses them to specifically fight certain germs that the body has previously come into contact with. This is also known as an “acquired” (learned) or specific immune response. Because the adaptive immune system is constantly learning and adapting, the body can also fight bacteria or viruses that change over time.
Both the innate and the adaptive immune system rely on markers that are on body cells. These markers tell the immune system whether the cell is a human cell that belongs in the body, or whether the cell is foreign. Pathogens have two markers. One marker is non-specific called a Pathogen-Associated Molecular Patterns (PAMPs), the other markers is specific called an Antigen. Many pathogens share the same PAMPs, however have unique and distinctive antigens; Every invader’s antigenic pattern is unique. The innate immune cells have receptors called Pattern Recognizing Molecules (PRMs) that recognize the PAMP. When the innate cells recognize the PAMP they begin the battle to destroy the foreign invaders. Adaptive immune system cells recognize the specific antigens on the pathogen and launch a battle specifically to destroy that pathogen.
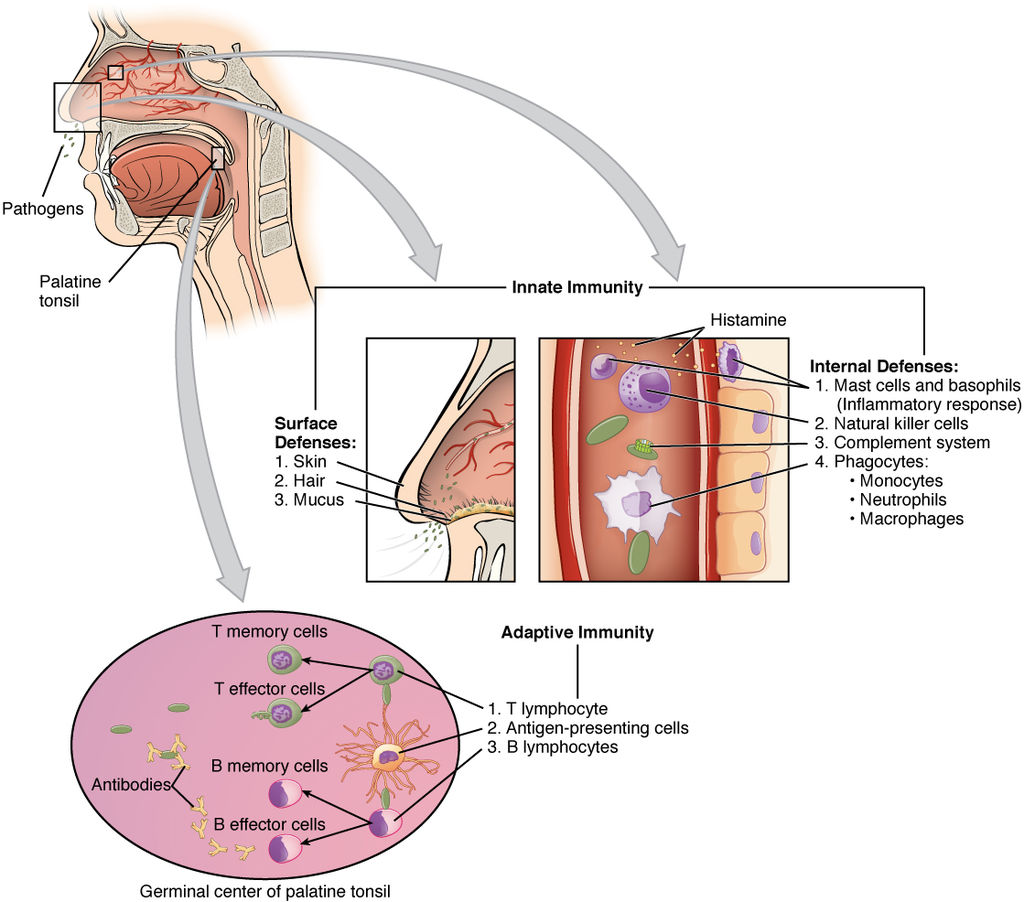
The innate immune system cells are the first to respond, these include the following types of leukocytes: mast cells, macrophages, natural killer cells, dendritic cells, monocytes, neutrophils, basophils, and eosinophils (described in Figure 11.?). Cells of the adaptive immune system are classified as lymphocytes (a type of leukocyte) and include two main types: T-cells and B-cells (the letters denote ‘thymus’ and ‘bone marrow’, the tissues where each of these leukocytes mature).
Steps to the The Immune System Battle:
- The cellular immune response begins when a pathogen gets through the bodies physical and chemical barriers.
- If a pathogen gets past the hosts defenses it will attempt to infect the host and begin replicating itself. The subsequent battle between the germs and the body’s immune system will cause the symptoms of illness.
- The first immune cells to respond to the invading pathogen are the innate immune cells: mast cells, macrophages, natural killer cells, dendritic cells, monocytes, neutrophils, basophils, and eosinophils. These cells are always ready to fight off pathogens and work hard to destroy the foreign invaders.
- Actions of the innate immune system cells
- Dendritic Cells: Ingest pathogen and help activate the adaptive immune system by presenting their antigen to Helping T-Cells and killer T-Cells.
- Neutrophils: Migrate from the bloodstream to ingest and kill bacteria and fungi and recruit more immune cells.
- Macrophages: Known as the “big eaters”, they ingest pathogens and dead cells and help activate the adaptive immune system by presenting their antigen. They also recruit more immune cells.
- Mast Cells: launch inflammatory response and recruit macrophages and neutrophils.
- Natural Killer cells: Detect and kill tumor or virus infected cells.
- Basophils: Defend against parasites and contribute to inflammatory response.
- Eosinophils: Kill bacteria and parasites.
- The innate immune cells alert the whole body that there is a problem by activating the inflammatory response and initiating the adaptive immune system.
- The inflammatory response brings swelling, pain and higher temperature, which attracts more cells to the site of infection. This means more immune cells join the fight to destroy the pathogen.
- The innate immune cells provide important information to the adaptive immune cells to “train” the adaptive immune cells how to destroy the pathogen.
- Training the adaptive immune cells is done in two ways, by releasing cytokines and displaying the pathogens antigens.
- Cytokines are signals that tell cells what to do and where to go. Your body responds to threats in different ways depending on the cytokine signal released by your immune cells.
- The antigen is displayed when the innate immune cells capture and breakdown the invader.
- Together, the cytokines and antigens train individual adaptive immune cells to recognize and destroy specific patterns of each foreign invader.
- The Adaptive Immune System Cells
- Helper and killer T-Cells are activated after the Dendritic cells engulf the pathogen.
- When the helper T-Cells create B-Cells they are initiating the adaptive immune system.
- Antibodies, B Cells, are then produced that attach to the pathogen.
- The B Cells divide to produce plasma and memory cells.
- If the same pathogen invades again, the memory cells help the immune system activate much quicker.
- When the adaptive cells are “trained” how to fight a specific antigen, they remember how to fight it, thus the next time that this pathogen tries to infect you your adaptive immune cells will remember it and destroy it quickly.
- The ability of the immune system to remember previous pathogens is commonly called adaptive or acquired immunity and is the basis for vaccines.
- However, pathogens really want to live and they can be tricky. Some pathogens, including those that cause flu, strep throat, and malaria, can mutate and change the way they look to your immune system over time by changing their antigen markers thus disguising themselves marking it harder for your immune system to recognize the mutated germs even though you’ve been exposed to them before. This is why you can get sick from flu, strep throat, or COVID multiple times.
Vaccines
It is possible to acquire adaptive immunity naturally or artificially. Natural immunity results from natural exposure to an antigen. For example, someone sneezes the influenza virus into the air and then it is breathed into another person’s nasal passageway. However, artificial immunity refers to deliberately introducing an antigen into an individual to stimulate an immune response, known as a vaccine. Whether you have been introduced to a pathogen naturally or artificially the end result is the same, to develop memory cells to acquire immunity against the pathogen.
If the immune system did not have the ability to remember pathogens then vaccines would not work; vaccines are effective because of memory cells. The mechanism underlying vaccination is that exposure of the adaptive immune system to a small dose of an antigen will produce an initial immune response. More importantly, this small dose of antigen establishes a population of memory T and B cells that will live long-term in the body. When that antigen is encountered again, the immune system is already primed. Upon a subsequent exposure, a more robust and faster response is established and the pathogen is destroyed faster. Vaccines can either prevent or decrease the severity of infections.
There are several different types of vaccines and even more types of vaccines in development. Each type is designed to teach your immune system how to fight off certain kinds of germs—and the serious diseases they cause. When scientists create vaccines, they consider how your immune system responds to the germ, who needs to be vaccinated against the germ, and the best technology or approach to create the vaccine.
| Vaccine Type | Characteristics | Vaccine Protects against |
| Inactivated vaccines |
|
|
| Live-attenuated vaccines |
|
|
| Messenger RNA (mRNA) vaccines |
|
|
| Subunit, recombinant, polysaccharide, and conjugate vaccines |
|
|
| Toxoid vaccines |
|
|
| Viral vector vaccines |
|
|
| DNA vaccines |
|
In development. No vaccines available yet. |
| Recombinant vector vaccines (platform-based vaccines) |
|
In development. No vaccines available yet. |
There is another way to get temporary immunity and that is called passive immunity, which is when antibodies are provided to the person from a donor recipient, for example from a mother to child as antibodies move across the placenta before birth. Passive immunity is not long-lasting because the individual does not produce memory cells.
Sexually Transmitted Diseases (STD’s)
There are approximately 20 different infections that are known to be transmitted through sexual contact. One in five people in the U.S. has an STD. While sexually transmitted diseases (STDs) affect individuals of all ages, STDs take a particularly heavy toll on young people. CDC estimates that youth ages 15-24 account for almost half of the 26 million new sexually transmitted infections that occurred in the United States in 2018.
Many cases of chlamydia, gonorrhea, and syphilis continue to go undiagnosed and unreported, and data on several additional STDs — such as human papillomavirus, herpes simplex virus, and trichomoniasis — are not routinely reported to CDC. Many STD’s are asymptomatic, meaning they do not show any symptoms, yet can still be spread to sexual partners. As a result, the CDC data on rates of STD’s only captures a fraction of the true burden of STDs in America. However, it provides important insights into the scope, distribution, and trends in STD diagnoses in the country.
| Year | Rate of Syphilis | Rate of Chlamydia | Rater of Gonorrhea |
| 1985 | 28.4 | 17.4 | 383 |
| 1990 | 54.3 | 160.2 | 276.4 |
| 1995 | 26 | 187.8 | 147.5 |
| 2000 | 11.2 | 251.4 | 128.7 |
| 2005 | 11.2 | 329.4 | 114.6 |
| 2010 | 14.8 | 423.6 | 100.2 |
| 2015 | 23.2 | 475 | 123 |
| 2020 | 40.8 | 481.3 | 206.5 |
It is important to understand the risk factors and symptoms of STD’s in order to protect yourself and your partners. It is also important to understand the impacts to your health if you do not get treatment.
Women who do not get treatment for STD’s can get Pelvic Inflammatory Disease (PID). PID is a serious condition which left untreated can cause scar tissue and abscesses to develop in the reproductive tract which can lead to permanent damage to the reproductive organs. PID can cause ectopic pregnancy (in which the fetus develops in abnormal places outside of the womb, a condition that can be life-threatening) and infertility.
For more detailed information, review the CDC fact sheet for Pelvic Inflammatory Disease (PID
Partners who do not get treated for an STD can be at an increased risk of contracting or spreading HIV/AIDS. If you get an STD and you have a sore or break in the skin from the STD, this may allow HIV to more easily enter your body and people who have HIV are more likely to spread HIV if they have an STD. The same behaviors and circumstances that may put you at risk for getting an STD also can put you at greater risk for getting HIV. In addition, having a sore or break in the skin from an STD may allow HIV to more easily enter your body. If you are sexually active, get tested for STDs and HIV regularly, even if you don’t have symptoms.
For more detailed information, review the CDC fact sheet for HIV/AIDS & STDs
Bacterial Vaginosis
Bacterial vaginosis (BV) is a condition that happens when there is too much of certain bacteria in the vagina. This changes the normal balance of bacteria in the vagina. BV is the most common vaginal condition in women ages 15-44.
Researchers do not know the cause of BV. However, we do know the condition most often occurs in those who are sexually active. BV is a result of an imbalance of “good” and “harmful” bacteria in a vagina. Douching, not using condoms, and having new or multiple sex partners can upset the normal balance of vaginal bacteria, increasing your risk for getting BV.
We also do not know how sex causes BV. There also is no research to show that treating a sex partner affects whether someone gets BV. Having BV can increase your chances of getting other STDs.
BV rarely affects those who have never had sex.
You cannot get BV from toilet seats, bedding, or swimming pools.
Many people with BV do not have symptoms. If you do have symptoms, you may notice:
- A thin white or gray vaginal discharge;
- Pain, itching, or burning in the vagina;
- A strong fish-like odor, especially after sex;
- Burning when peeing; and
- Itching around the outside of the vagina.
For more detailed information, review the CDC fact sheet for Bacterial Vaginosis (BV)
Chlamydia
Chlamydia is a common bacterial STD that can cause infection among both men and women. It can cause permanent damage to a woman’s reproductive system. This can make it difficult or impossible to get pregnant later. Chlamydia can also cause a potentially fatal ectopic pregnancy (pregnancy that occurs outside the womb).
You can get chlamydia by having vaginal, anal, or oral sex with someone who has chlamydia. Also, you can still get chlamydia even if your sex partner does not ejaculate (cum). A pregnant person with chlamydia can give the infection to their baby during childbirth.
Chlamydia often has no symptoms, but it can cause serious health problems, even without symptoms. If symptoms occur, they may not appear until several weeks after having sex with a partner who has chlamydia.
Even when chlamydia has no symptoms, it can damage a woman’s reproductive system.
Women with symptoms may notice:
- An abnormal vaginal discharge; and
- A burning sensation when peeing.
Symptoms in men can include:
- A discharge from their penis;
- A burning sensation when peeing; and
- Pain and swelling in one or both testicles (although this is less common).
Men and women can also get chlamydia in their rectum. This happens either by having receptive anal sex, or by spread from another infected site (such as the vagina). While these infections often cause no symptoms, they can cause
- Rectal pain;
- Discharge; and
- Bleeding.
See a healthcare provider if you notice any of these symptoms. You should also see a provider if your partner has an STD or symptoms of one. Symptoms can include
- An unusual sore;
- A smelly discharge;
- Burning when peeing; or
- Bleeding between periods.
For more detailed information, review the CDC fact sheet for Chlamydia
Gonorrhea
Gonorrhea is is a common bacterial STD that can cause infection in the genitals, rectum, and throat. It is very common, especially among young people ages 15-24 years.
You can get gonorrhea by having vaginal, anal, or oral sex with someone who has gonorrhea. A pregnant person with gonorrhea can give the infection to their baby during childbirth.
Gonorrhea often has no symptoms, but it can cause serious health problems, even without symptoms.
Most women with gonorrhea do not have any symptoms. Even when a woman has symptoms, they are often mild and can be mistaken for a bladder or vaginal infection.
Symptoms in women can include:
- Painful or burning sensation when peeing;
- Increased vaginal discharge; and
- Vaginal bleeding between periods.
Men who do have symptoms may have:
- A burning sensation when peeing;
- A white, yellow, or green discharge from the penis; and
- Painful or swollen testicles (although this is less common).
Rectal infections may either cause no symptoms or cause symptoms in both men and women that may include:
- Discharge;
- Anal itching;
- Soreness;
- Bleeding; and
- Painful bowel movements.
See your healthcare provider if you notice any of these symptoms. You should also see a provider if your partner has an STD or symptoms of one. Symptoms can include an unusual sore, a smelly discharge, burning when peeing, or bleeding between periods.
For more detailed information, review the CDC fact sheet for Gonorrhea
Genital Herpes
Genital herpes is common viral STD in the United States. In 2018, CDC estimates show there were 572,000 new genital herpes infections in the United States among people aged 14 to 49.
HSV-1 often causes oral herpes, which can result in cold sores or fever blisters on or around the mouth. HSV-1 is typically acquired during childhood, is very common, and often has no symptoms. HSV-2 is a sexually transmitted disease that causes genital herpes. Oral herpes caused by HSV-1 can spread from the mouth to the genitals through oral sex, thus Genital herpes is an STD that can be caused by two types of viruses – herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2).
You can get genital herpes by having vaginal, anal, or oral sex with someone who has the infection. You can get herpes if you have contact with:
- A herpes sore;
- Saliva from a partner with an oral herpes infection;
- Genital fluids from a partner with a genital herpes infection;
- Skin in the oral area of a partner with oral herpes; or
- Skin in the genital area of a partner with genital herpes.
You also can get genital herpes from a sex partner who does not have a visible sore or is unaware of their infection. It is also possible to get genital herpes if you receive oral sex from a partner with oral herpes.
You will not get herpes from toilet seats, bedding, or swimming pools. You also will not get it from touching objects, such as silverware, soap, or towels.
Most people with genital herpes have no symptoms or have very mild symptoms. Mild symptoms may go unnoticed or be mistaken for other skin conditions like a pimple or ingrown hair. Because of this, most people do not know they have a herpes infection.
Herpes sores usually appear as one or more blisters on or around the genitals, rectum or mouth. This is known as having an “outbreak”. The blisters break and leave painful sores that may take a week or more to heal. Flu-like symptoms (e.g., fever, body aches, or swollen glands) also may occur during the first outbreak.
For more detailed information, review the CDC fact sheet for Genital Herpes
Hepatitis
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C (there is also Hepatitis D and E).
Hepatitis A and B can be transmitted through sexual activity, it is less common to be infected with Hepatitis C through sexual intercourse.
For more detailed information, review the CDC fact sheet for Hepatitis
Human Papillomavirus Virus (HPV)- Genital Warts
HPV is a viral STD and the most common STD/STI. There were about 43 million HPV infections in 2018, many among people in their late teens and early 20s. There are many different types of HPV. Some types can cause health problems, including genital warts and cancers. But there are vaccines that can stop these health problems from happening. HPV is a different virus than HIV and HSV (herpes).
You can get HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. It also spreads through close skin-to-skin touching during sex. A person with HPV can pass the infection to someone even when they have no signs or symptoms. If you are sexually active, you can get HPV, even if you have had sex with only one person. You also can develop symptoms years after having sex with someone who has the infection. This makes it hard to know when you first got it.
HPV can cause cervical and other cancers, including cancer of the vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat (called oropharyngeal cancer). This can include the base of the tongue and tonsils. Cancer often takes years, even decades, to develop after a person gets HPV. Genital warts and cancers result from different types of HPV.
There is no test to find out a person’s “HPV status.” Also, there is no approved HPV test to find HPV in the mouth or throat. However, there are HPV tests that can screen for cervical cancer. Most people with HPV do not know they have the infection. They never develop symptoms or health problems from it. Some people find out they have HPV when they get genital warts. Women may find out they have HPV when they get an abnormal Pap test result (during cervical cancer screening). Others may only find out once they’ve developed more serious problems from HPV, such as cancers.
There is a vaccine available to prevent new HPV infections. The HPV vaccine is recommended for routine vaccination starting at age 11 or 12 years (can be started at age 9). Vaccination is not recommended for everyone older than age 26 years, however adults ages 27 through 45 years might decide to get the HPV vaccine based on discussion with their clinician, if they did not get adequately vaccinated when they were younger.
For more detailed information, review the CDC fact sheet for Human Papillomavirus (HPV
Syphilis
Syphilis is a bacterial sexually transmitted infection (STI) that can cause serious health problems without treatment. Infection develops in stages (primary, secondary, latent, and tertiary). Each stage can have different signs and symptoms.
You can get syphilis by direct contact with a syphilis sore during vaginal, anal, or oral sex. You cannot get syphilis through casual contact with objects, such as toilet seats or doorknobs.
Syphilis can spread from a mother with syphilis to her unborn baby.
There are four stages of syphilis (primary, secondary, latent, and tertiary). Each stage has different signs and symptoms. Without treatment, syphilis can spread to the brain and nervous system (neurosyphilis), the eye (ocular syphilis), or the ear (otosyphilis) during any of the four stages.
- Primary Stage
- During the first (primary) stage of syphilis, you may notice a single sore or multiple sores. The sore is the location where syphilis entered your body. These sores usually occur in, on, or around the penis, vagina, anus, rectum, or mouth.
- Sores are usually (but not always) firm, round, and painless. Because the sore is painless, you may not notice it. The sore usually lasts 3 to 6 weeks and heals regardless of whether you receive treatment.
- Even after the sore goes away, you must still receive treatment. This will stop your infection from moving to the secondary stage.
- Secondary Stage
- During the secondary stage, you may have skin rashes and/or sores in your mouth, vagina, or anus.
- This stage usually starts with a rash on one or more areas of your body. The rash can show up when your primary sore is healing or several weeks after the sore has healed. The rash usually won’t itch and can be on the palms of your hands and/or the bottoms of your feet and look rough, red, or reddish-brown.
- Other symptoms may include fever, swollen lymph nodes, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue.
- The symptoms from this stage will go not away unless you receive treatment. Without the right treatment, your infection will move to the latent and possibly tertiary stages of syphilis.
- Latent Stage
- The latent stage of syphilis is a period when there are no visible signs or symptoms. Without treatment, you can continue to have syphilis in your body for years.
- Tertiary Stage
- Most people with untreated syphilis do not develop tertiary syphilis. However, when it does happen, it can affect many different organ systems. These include the heart and blood vessels, and the brain and nervous system. Tertiary syphilis is very serious and would occur 10–30 years after your infection began. In tertiary syphilis, the disease damages your internal organs and can result in death. A healthcare provider can usually diagnose tertiary syphilis with the help of multiple tests.
For more detailed information, review the CDC fact sheet for Syphilis
Trichomoniasis
Trichomoniasis (or “trich”) is a very common STD caused by infection with Trichomonas vaginalis (a protozoan parasite). Although symptoms vary, most people who have trich cannot tell they have it.
Sexually active people can get trich by having sex without a condom with a partner who has trich.
In women, the infection is most commonly found in the lower genital tract (vulva, vagina, cervix, or urethra). In men, the infection is most commonly found inside the penis (urethra). During sex, the parasite usually spreads from a penis to a vagina, or from a vagina to a penis. It can also spread from a vagina to another vagina.
It is not common for the parasite to infect other body parts, like the hands, mouth, or anus. It is unclear why some people with the infection get symptoms while others do not. It probably depends on factors like a person’s age and overall health. People with trich can pass the infection to others, even if they do not have symptoms.
About 70% of people with the infection do not have any signs or symptoms. When trich does cause symptoms, they can range from mild irritation to severe inflammation. Some people get symptoms within 5 to 28 days after getting the infection. Others do not develop symptoms until much later. Symptoms can come and go.
Men with trich may notice:
- Itching or irritation inside the penis;
- Burning after peeing or ejaculating; and
- Discharge from the penis.
Women with trich may notice:
- Itching, burning, redness or soreness of the genitals;
- Discomfort when peeing; and
- A clear, white, yellowish, or greenish vaginal discharge (i.e., thin discharge or increased volume) with a fishy smell.
Having trich can make sex feel unpleasant. Without treatment, the infection can last for months or even years.
For more detailed information, review the CDC fact sheet for Trichomoniasis
Key Takeaways for Chapter
- The immune system is constantly working to keep you healthy.
- There are about 1,400 known pathogens that cause disease in humans.
- There are steps you can take to break the chain of infection and stop disease transmission.
- The bodies first barrier to disease are the physical and chemical barriers.
- The innate and adaptive immune system work in tandem to protect you.
- The immune system has an incredible ability to remember past infections.
- The ability to remember pathogens is the foundation for Vaccines
- There are several different types of vaccines.
- STD’s are very common
- Most STDs are asymptomatic.
Media Attributions
- Immune_system101 © AIDSgov is licensed under a Public Domain license
- Chain_of_Infection © Genieieiop, is licensed under a CC BY (Attribution) license
- Cooperation_Between_Innate_and_Immune_Responses © OpenStax College is licensed under a CC BY (Attribution) license
- Innate-Immune-System-Cells © Modification of work by NIH is licensed under a Public Domain license
- Lymph_42 © Open Learning Initiative is licensed under a CC BY (Attribution) license
- Balloux, F., van Dorp, L. Q&A: What are pathogens, and what have they done to and for us?. BMC Biol 15, 91 (2017). https://doi.org/10.1186/s12915-017-0433-z ↵
- Balloux, F., van Dorp, L. Q&A: What are pathogens, and what have they done to and for us?. BMC Biol 15, 91 (2017). https://doi.org/10.1186/s12915-017-0433-z ↵
- Piret J, Boivin G. Pandemics Throughout History. Front Microbiol. 2021 Jan 15;11:631736. doi: 10.3389/fmicb.2020.631736. PMID: 33584597; PMCID: PMC7874133. ↵
