Chapter 6: Emotional & Mental Health
Do you feel you are living up to your potential?
Do you find opportunities throughout the day to focus on happiness?
Do you feel good about yourself?
Have you ever felt sad for a prolonged amount of time?
Have you, or do you know someone who has, felt depressed or had anxiety?
Chapter 6 Learning Outcomes
By the end of this chapter you will be able to:
- Describe what mental, emotional, and psychological health entails.
- Recognize warning signs of emotional distress
- Relate Maslow’s Hierarchy of Needs to emotional health
- Recognize emotional defense mechanisms
- Describe types of anxiety disorders and treatments
- Explain incidence and signs of Depression
What is Mental Health?
Mental health is a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community. Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make choices. Mental health is important at every stage of life, from childhood and adolescence through adulthood. Mental health is fundamental to our collective and individual ability as humans to think, emote, interact with each other, earn a living and enjoy life. Although more emphasis is often placed on our physical wellness, mental and physical health are equally important components of overall health.
Although poor mental health and mental illness are terms that are often used interchangeably, poor mental health and mental illness are not the same. A person can experience poor mental health and not be diagnosed with a mental illness. Likewise, a person diagnosed with a mental illness can experience periods of physical, mental, and social well-being.
According to the World Health Organization:
- Mental health is more than the absence of mental disorders.
- Mental health is an integral part of health; indeed, there is no health without mental health.
- Mental health is determined by a range of socioeconomic, biological and environmental factors
Mental Health and Wellness
Your mental health is very important to your well-being. Just like we strive for to be physically healthy, we must also strive to be mentally, emotionally, and socially healthy.
Positive mental health allows people to:
- Cope with the stresses of life
- Be physically healthy
- Have good relationships
- Make meaningful contributions to your community
- Work productively
- Realize your full potential
Reaching Your Full Potential
What does it take to reach your full human potential, to become everything that you are capable of becoming? Is it important to have air, water, food, and shelter in order for you to strive to reach your human potential? Is it important to feel safe in order to reach your human potential?
In 1943 Abraham Maslow published one of the most cited theories of human behavior called Maslow’s Hierarchy of Needs[1]. The purpose of the Hierarchy of Needs was to explain that there are levels of human needs and we need to focus on each of the levels in order to become everything that we are capable of becoming. Maslow’s hierarchy of needs is often portrayed in the shape of a pyramid, with the most fundamental levels of needs at the bottom. Maslow developed the hierarchy with order of importance in mind, however noted that although it was observed that most people fulfilled their basic needs in the order of the hierarchy, there are some exceptions. The order of needs as categorized by Maslow from bottom to top are: physiological needs, safety, love and belonging, esteem, and self-actualization. Maslow acknowledged that many different levels of motivation are likely to be present in a human all at once. His focus in discussing the hierarchy was to identify the basic types of motivation and the order that they generally progress as lower needs are reasonably well met.
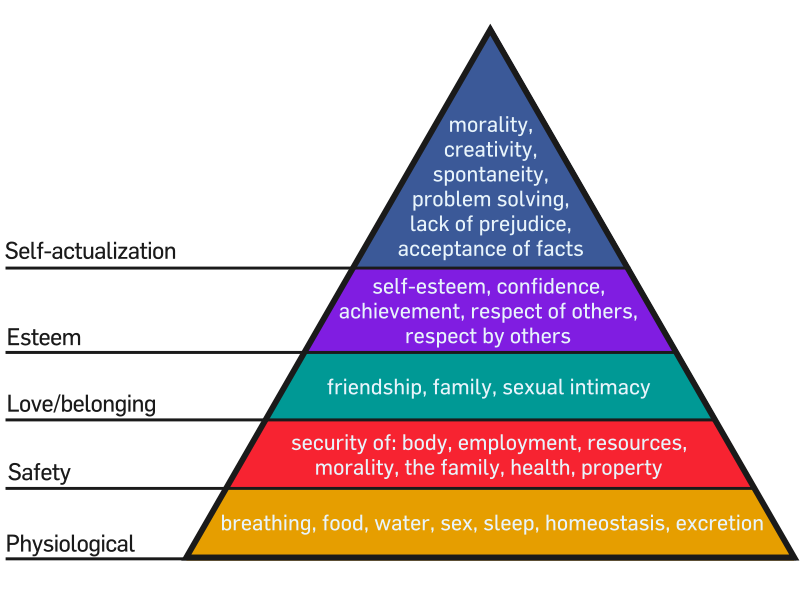
Physiological Needs
Physiological needs are generally obvious because they are required for survival. If requirements are not met, the body cannot continue to function. Air, water, food, clothing, and shelter are the basic physiological needs.
Safety Needs
Once physical needs are satisfied, individual safety takes precedence. Safety and Security needs include:
- Personal and family safety
- Financial security
- Health and well-being
Love/belonging Needs
After physiological and safety needs are fulfilled, the third layer of human needs are interpersonal. This involves feelings of belongingness. Humans need to feel a sense of belonging and acceptance, whether it comes from larger community affiliations or simply a few close friends. Without these connections, many people become susceptible to loneliness, social anxiety, and clinical depression. This need for belonging can sometimes overcome physiological and security needs. For example, an anorexic may ignore the need to eat and the security of health for a feeling of control and belonging. Deficiencies in interpersonal needs, due to neglect, shunning, ostracism, etc., can impact an individual’s ability to form and maintain emotionally significant relationships.
Esteem
Esteem represents the normal human desire to be accepted and valued by others. People need to engage themselves to gain recognition and have an activity or activities that give the person a sense of contribution, to feel self-valued, be it in a profession or hobby. Imbalances at this level can result in low self-esteem or an inferiority complex. Many people with low self-esteem will not be able to improve their view of themselves simply by receiving fame, respect, and glory externally, but must first accept themselves internally. Psychological imbalances, such as depression, can prevent one from obtaining self-esteem on both levels.
Self-actualization
This level of need refers to what a person’s full potential is and the realization of that potential. Maslow describes this level as the desire to accomplish everything that one can, to become the most that one can be. Individuals may perceive or focus on this need very specifically. For example, one individual may have the strong desire to become an ideal parent. In another, the desire may be expressed athletically. For others, it may be expressed in paintings, pictures, or inventions. Maslow believed that to acquire this level of need, the person must adequately achieve the previous needs.
Examples: The Movie Cast Away
The movie, Cast Away, demonstrates Maslow’s Hierarchy of Needs. When Tom Hanks character is marooned on a deserted island the first things he does find water and food. These actions satisfy his immediate physiological needs. Next he needs to find shelter for safety and security. To meet his love and belongingness needs he has “Wilson”.
Positive Psychology: The Science of Happiness
Why study happiness? What does happiness have to do with well-being? For your well-being, is it more important to focus on being happy as a goal or focus on bringing positivity into your life? What do Denmark, Iceland, Switzerland, Finland, and Netherlands have in common?
Happiness has been linked to health with research indicating that being happy lowers disease risk, increases the likelihood of including positive behaviors in your life, and reduced the chance of all-cause mortality[2]. The science of happiness is just one area of what is called Positive Psychology[3]. Positive psychology is a relatively new field that shifted the discussion from a specific focus on what is wrong with someone (disease or illness) to what is right, by utilizing research to understand what contributes to a persons optimal functioning and helps them to flourish. This shift in focus is one factor that led to the publication of the World Happiness Report. Since 2012, the World Happiness Report has been published annually focusing on the state of global happiness for 156 countries by measuring how happy their citizens perceive themselves to be. Denmark, Iceland, Switzerland, Finland, and Netherlands are routinely shown to be the happiest countries in the world.
Studies show that focusing on positivity in your life is associated with overall happiness, life satisfaction, and psychological well-being, whereas a focus on seeking happiness or being happy is associated with negative feelings[4]. To increase happiness in your life, focus on bringing positivity into you life, which will lead to happiness. Just focusing on wanting to be happy will likely have a negative impact on your well-being.
Focus on your mental health
Ways to maintain positive mental health include:
- Getting professional help if you need it
- Connecting with others
- Staying positive
- Getting physically active
- Helping others
- Getting enough sleep
- Developing coping skills
- Developing a sense of meaning and purpose in life.
- Relaxation Techniques (meditation)
- Practice Mindfulness
- Practice Gratitude
Challenges to our mental health
Although it is important to focus on reaching your full potential and embracing positivity, this does not mean you will not have challenges to your mental health.
Many factors contribute to mental health problems, including:
- Biological factors, such as genes or brain chemistry
- Life experiences, such as trauma or abuse
- Family history of mental health problems
- Experiences related to other ongoing (chronic) medical conditions, such as cancer or diabetes
- Use of alcohol or drugs
- Having feelings of loneliness or isolation
Mental Health Statistics
Mental illness is very common. It is so common that more than 50% of Americans will be diagnosed with a mental illness or disorder at some point in their lifetime, with 1 in 5 Americans experiencing a mental illness in any given year. Mental illness does no just effect adults, 1 in 5 children, either currently or at some point during their life, have had a seriously debilitating mental illness. Mental illness varies in degree of severity from mild to severe with about 1 in 25 Americans living with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression.
The National Institute of Mental Health categorizes mental illness into two broad categories, Any Mental Illness (AMI) and Serious Mental Illness (SMI).
- Any mental illness (AMI) is defined as a mental, behavioral, or emotional disorder. AMI can vary in impact, ranging from no impairment to mild, moderate, and even severe impairment (e.g., individuals with serious mental illness as defined below).
- In 2020, there were an estimated 52.9 million adults aged 18 or older in the United States with AMI. This number represented 21.0% of all U.S. adults.
- The prevalence of AMI was higher among females (25.8%) than males (15.8%).
- Young adults aged 18-25 years had the highest prevalence of AMI (30.6%) compared to adults aged 26-49 years (25.3%) and aged 50 and older (14.5%).
- The prevalence of AMI was highest among the adults reporting two or more races (35.8%), followed by White adults (22.6%). The prevalence of AMI was lowest among Asian adults (13.9%).
- Serious mental illness (SMI) is defined as a mental, behavioral, or emotional disorder resulting in serious functional impairment, which substantially interferes with or limits one or more major life activities. The burden of mental illnesses is particularly concentrated among those who experience disability due to SMI.
- In 2020, there were an estimated 14.2 million adults aged 18 or older in the United States with SMI. This number represented 5.6% of all U.S. adults.
- The prevalence of SMI was higher among females (7.0%) than males (4.2%).
- Young adults aged 18-25 years had the highest prevalence of SMI (9.7%) compared to adults aged 26-49 years (6.9%) and aged 50 and older (3.4%).
- The prevalence of SMI was highest among the adults reporting two or more races (9.9%), followed by American Indian / Alaskan Native (AI/AN) adults (6.6%). The prevalence of SMI was lowest among Native Hawaiian / Other Pacific Islander (NH/OPI) adults (1.2%).
Warning signs of Mental Illness
Not sure if you or someone you know is living with mental health problems? Experiencing one or more of the following feelings or behaviors can be an early warning sign of a problem:
- Eating or sleeping too much or too little
- Pulling away from people and usual activities
- Having low or no energy
- Feeling numb or like nothing matters
- Having unexplained aches and pains
- Feeling helpless or hopeless
- Smoking, drinking, or using drugs more than usual
- Feeling unusually confused, forgetful, on edge, angry, upset, worried, or scared
- Yelling or fighting with family and friends
- Experiencing severe mood swings that cause problems in relationships
- Having persistent thoughts and memories you can’t get out of your head
- Hearing voices or believing things that are not true
- Thinking of harming yourself or others
- Inability to perform daily tasks like taking care of your kids or getting to work or school
Coping Mechanisms and defense mechanisms
When confronted with something that is challenging to our mental health or stress, many people respond with coping mechanisms[5] or defense mechanisms[6]. The main difference between coping mechanisms and defense mechanisms is that coping is something you consciously do and a defense mechanism is often employed unconsciously. Both actions are intended to manage a situation that is creating a problem for the person.
When confronted with a challenge, people might consciously employ problem-focused, emotion-focused, meaning-focused, or social-focused coping mechanisms. Many of these coping mechanisms can be helpful, however people might employe maladaptive coping mechanisms which could lead to poor mental health such as using drugs or alcohol to avoid a problem.
| Coping Mechanism Category | Description | Example |
| Problem-focused | An individual focuses on solving the problem | Active coping, problem-solving, planning, restraint coping, and suppression of competing activities. |
| Emotion-focused | An individual aims to reduce the negative emotions associated with the problem | Positive reframing, acceptance, and humor |
| Meaning-focused | An individual uses cognitive strategies to derive and manage the meaning of the situation | Focus on beliefs and values to support well-being |
| Social-focused | An individual reduces stress by seeking emotional or instrumental support from their community | Reach out to people |
Good coping skills include:
- Practicing meditation and relaxation techniques
- Having time to yourself
- Engaging in physical activity or exercise
- Reading
- Spending time with friends
- Finding humor
- Spending time on your hobbies
- Engaging in spirituality
- Spending quality time with your pets
- Getting a good night’s sleep
- Eating healthy.
Negative coping skills include:
- Using drugs
- Drinking alcohol excessively
- Engaging in self-mutilation
- Ignoring or bottling up feelings
- Taking sedatives
- Taking stimulants
- Working too much
- Avoiding your problems
- Being in denial.
Of the negative coping skills listed above, two of them are considered defense mechanisms, avoidance and denial. Defense mechanisms are psychological mechanisms aimed at reducing anxiety. They were first discussed by Sigmund Freud as part of his psychoanalytic theory and further developed by his daughter, Anna Freud. Often unconscious, defense mechanisms are used to protect an individual from psychological pain or anxiety.
Defense mechanisms include avoidance, repressions, regression, dispalcement, sublimation, reaction formation, projections, and rationalization as shown in the following Table.
| Defense Mechanism | Description | Example |
| Avoidance | Any behavior used to escape, distract, or avoid difficult thoughts, feelings, or situations. | Utilizing drugs or alcohol to numb feelings or making up excused to avoid attending social gatherings. |
| Repression | Unknowingly placing an unpleasant memory or thought in the conscious | Not remembering a traumatic event such as being sexually abused as a child. |
| Regression | Reverting back to an immature behavior from an earlier stage of development | Throwing temper tantrums as an adult when you don’t get your way |
| Displacement | Redirecting feelings or actions from the intended source to a safer, substitute target | Taking your anger towards your boss out on family members by yelling at them in place of your boss. |
| Sublimation | Replacing socially unacceptable impulses with socially acceptable behavior | Channeling aggressiveness into playing football |
| Reaction formation | Overacting in the opposite way to one’s true feelings. | Being overly protective of an unwanted child. |
| Projection | Attributing one’s own unacceptable feelings and thoughts to others and not yourself | Accusing your boy/girlfriend of cheating on you because you have thoughts about cheating on him/her |
| Rationalization | Justifying actions, thoughts, or unwanted outcomes with excuses or faulty logic | Blaming the teaching style of a professor for why you failed an exam. |
Mental Health Disorders
Mental illness or disorders are often categorized into Mood Disorders, Anxiety Disorders, Psychotic Disorders, and Eating Disorders.
Mood disorders, also called affective disorders, affect your emotional state focusing on how you feel from extreme sadness to extreme happiness. Anxiety disorders occur when a person responds to something with fear or dread and has a severe stress response that may include physical reactions such as rapid heart rate, overwhelming worry, muscle tension, trouble sleeping, nausea, and diarrhea. Psychotic Disorders, also called thought disorders, involve distorted awareness or thinking.
Mood Disorders include:
- Depression
- Bipolar disorders
- Seasonal affective disorder
Anxiety Disorders include:
- General anxiety
- Specific phobias and Agoraphobia
- Post-traumatic stress disorder
- Panic disorder
- Social anxiety disorder
Psychotic Disorders include:
- Schizophrenia
Eating Disorders include
- Anorexia Nervosa
- Bulimia Nervosa
- Binge Eating
Depression
Depression (major depressive disorder or clinical depression) is the most common mood disorder characterized by severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. Depression is more than just feeling down or having a bad day. When a sad mood lasts for a long time and interferes with normal, everyday functioning, you may be clinically depressed.
It is estimated that about 1 out of every 6 adults will have depression at some time in their life. There are varying levels of depression and causes of depression. A person with persistent depressive disorder (also called dysthymia) means they have suffered from depressed mood that lasts for at least two years. A woman with perinatal depression has experienced full-blown major depression during pregnancy or after delivery (postpartum depression).
Symptoms of depression include:
- Feeling sad or anxious often or all the time
- Not wanting to do activities that used to be fun
- Feeling irritable‚ easily frustrated‚ or restless
- Having trouble falling asleep or staying asleep
- Waking up too early or sleeping too much
- Eating more or less than usual or having no appetite
- Experiencing aches, pains, headaches, or stomach problems that do not improve with treatment
- Having trouble concentrating, remembering details, or making decisions
- Feeling tired‚ even after sleeping well
- Feeling guilty, worthless, or helpless
- Thinking about suicide or hurting yourself
Not everyone who is depressed experiences every symptom. Some people experience only a few symptoms while others may experience many. Several persistent symptoms in addition to low mood are required for a diagnosis of major depression, but people with only a few – but distressing – symptoms may benefit from treatment of their “subsyndromal” depression. The severity and frequency of symptoms and how long they last will vary depending on the individual and his or her particular illness. Symptoms may also vary depending on the stage of the illness.
Bipolar Disorder
Bipolar disorder is a mood disorder characterized by intense mood swings. Sometimes you may feel extremely “up,” elated, irritable, or energized. This is called a manic episode. Other times you may feel “down,” sad, indifferent, or hopeless. This is called a depressive episode. You may have both manic and depressive symptoms together. This is called a mixed episode.
Symptoms of Bipolar include:
- The symptoms of a manic episode can include
- Feeling very up, high, or elated
- Feeling jumpy or wired, more active than usual
- Having a very short temper or seeming extremely irritable
- Having racing thoughts and talking very fast
- Needing less sleep
- Feeling like you are unusually important, talented, or powerful
- Do risky things that show poor judgment, such as eating and drinking too much, spending or giving away a lot of money, or having reckless sex
- The symptoms of a depressive episode can include
- Feeling very sad, hopeless, or worthless
- Feeling lonely or isolating yourself from others
- Talking very slowly, feeling like you have nothing to say, or forgetting a lot
- Having little energySleeping too much
- Eating too much or too little
- Lack of interest in your usual activities and being unable to do even simple things
- Thinking about death or suicide
- The symptoms of a mixed episode include both manic and depressive symptoms together. For example, you may feel very sad, empty, or hopeless, while at the same time feeling extremely energized.
Seasonal Affective Disorder (SAD)
SAD is a specific type of Depression (a mood disorder) that comes and goes with the seasons.
Seasonal affective disorder is characterized by the onset of depression during the winter months, when there is less natural sunlight. This depression generally lifts during spring and summer. Winter depression, typically accompanied by social withdrawal, increased sleep, and weight gain, predictably returns every year in seasonal affective disorder.
Symptoms of SAD include:
- Sadness
- Gloomy outlook
- Feeling hopeless, worthless, and irritable
- Loss of interest or pleasure in activities you used to enjoy
- Low energy
- Difficulty sleeping or oversleeping
- Carbohydrate cravings and weight gain
- Thoughts of death or suicide
General Anxiety
Generalized Anxiety Disorder is an anxiety disorder characterized by excessive worrying. People with GAD excessively worry about ordinary daily issues such as health, money, work, and family on most days for at least 6 months.
Symptoms of GAD include:
- Feeling restless, wound-up, or on-edge
- Being easily fatigued
- Having difficulty concentrating; mind going blank
- Being irritable
- Having muscle tension
- Difficulty controlling feelings of worry
- Having sleep problems, such as difficulty falling or staying asleep, restlessness, or unsatisfying sleep
Panic Disorder
Panic disorder is an anxiety disorder characterized by recurrent unexpected panic attacks, which are sudden periods of intense fear that may include palpitations, pounding heart, or accelerated heart rate; sweating; trembling or shaking; sensations of shortness of breath, smothering, or choking; and feeling of impending doom.
Symptoms of panic disorder include:
- Heart palpitations, a pounding heartbeat, or an accelerated heartrate
- Sweating
- Trembling or shaking
- Sensations of shortness of breath, smothering, or choking
- Feelings of impending doom
- Feelings of being out of control
People with panic disorder often worry about when the next attack will happen and actively try to prevent future attacks by avoiding places, situations, or behaviors they associate with panic attacks. Worry about panic attacks, and the effort spent trying to avoid attacks, cause significant problems in various areas of the person’s life, including the development of agoraphobia.
Specific Phobias and Agoraphobia
A phobia is an anxiety disorder characterized by a strong, irrational fear of something that poses little or no real danger. There are many specific phobias such as the fear of heights which is called Acrophobia, or the fear of spiders termed Arachnophobia. A person who has a fear of public spaces is termed Agoraphobia. If you become anxious and extremely self-conscious in everyday social situations, you could have a social phobia, also referred to as a social anxiety disorder.
Symptoms of specific phobias include:
- May have an irrational or excessive worry about encountering the feared object or situation
- Take active steps to avoid the feared object or situation
- Experience immediate intense anxiety upon encountering the feared object or situation
- Endure unavoidable objects and situations with intense anxiety
Agoraphobia: People with agoraphobia have an intense fear of two or more of the following situations:
- Using public transportation
- Being in open spaces
- Being in enclosed spaces
- Standing in line or being in a crowd
- Being outside of the home alone
People with agoraphobia often avoid these situations, in part, because they think being able to leave might be difficult or impossible in the event they have panic-like reactions or other embarrassing symptoms. In the most severe form of agoraphobia, an individual can become housebound.
Social Anxiety Disorder (social phobia)
Social anxiety disorder is an anxiety disorder characterized by a general intense fear of, or anxiety toward, social or performance situations. They worry that actions or behaviors associated with their anxiety will be negatively evaluated by others, leading them to feel embarrassed.
Symptoms of Social Anxiety Disorder include:
- Feeling highly anxious about being with other people and having a hard time talking to them
- Feeling very self-conscious in front of other people and worried about feeling humiliated, embarrassed, or rejected, or fearful of offending others
- Being very afraid that other people will judge them
- Worrying for days or weeks before an event where other people will be
- Staying away from places where there are other people
- Having a hard time making friends and keeping friends
- Blushing, sweating, or trembling around other people
- Feeling nauseous or sick to your stomach when other people are around
Post-traumatic stress disorder
PTSD is an anxiety disorder that develops in some people who have experienced a shocking, scary, or dangerous event. The “fight of flight” reaction is a natural process meant to keep a person from harm when in traumatic experiences, however for those with PTSD the reaction continues for a long period of time or they experience the reaction even when they are not in danger.
Symptoms include:
- To be diagnosed with PTSD, an adult must have all of the following for at least 1 month:
- At least one re-experiencing symptom
- At least one avoidance symptom
- At least two arousal and reactivity symptoms
- At least two cognition and mood symptoms
- Re-experiencing symptoms include:
- Flashbacks—reliving the trauma over and over, including physical symptoms like a racing heart or sweating
- Bad dreams
- Frightening thoughts
Schizophrenia
Schizophrenia is a psychotic disorder that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality, which causes significant distress for the individual, their family members, and friends. Schizophrenia is typically diagnosed in the late teen years to the early thirties and tends to emerge earlier in males (late adolescence – early twenties) than females (early twenties – early thirties).
Symptoms of Schizophrenia include:
- Psychotic Symptoms
- Hallucinations, such as hearing voices or seeing things that aren’t there
- Delusions, which are firmly held beliefs not supported by objective facts (e.g., paranoia – irrational fears that others are “out to get you” or believing that the television, radio, or internet are broadcasting special messages that require some response)
- Negative Symptoms
- Reduced motivation and difficulty planning, beginning, and sustaining activities
- Diminished feelings of pleasure in everyday life
- “Flat affect,” or reduced expression of emotions via facial expression or voice tone
- Reduced speaking
- Cognitive Symptoms
- Difficulty processing information to make decisions
- Problems using information immediately after learning it
- Trouble focusing or paying attention
Eating Disorders and Mental Health
Eating disorders are not a choice, rather they are serious and often fatal illnesses that are associated with severe disturbances in people’s eating behaviors and related thoughts and emotions. Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors.
Review chapter 4 for more in-depth explanations of common eating disorders.
Suicide
Suicide is a major public health concern. In 2020, an estimated 12.2 million American adults seriously thought about suicide, 3.2 million planned a suicide attempt, 1.2 million attempted suicide, and 45,979 died by suicide. In 2020, suicide was among the top 9 leading causes of death for people ages 10-64 and the second leading cause of death for people ages 10-14 and 25-34. Depression, substance use disorders, and psychosis are the most relevant risk factors for suicide, with anxiety, personality, eating, and trauma-related disorders also contributing to risk of suicide. Most people, could be at least 90%, who have died by suicide have suffered from mental disorders[7]. Suicide is complicated and tragic but it is often preventable. Knowing the warning signs for suicide and how to get help can help save lives.
Suicidal thoughts or actions are a sign of extreme distress and should not be ignored.
Warning signs that someone may be at immediate risk for attempting suicide include:
- Talking about wanting to die or wanting to kill themselves
- Talking about feeling empty or hopeless or having no reason to live
- Talking about feeling trapped or feeling that there are no solutions
- Feeling unbearable emotional or physical pain
- Talking about being a burden to others
- Withdrawing from family and friends
- Giving away important possessions
- Saying goodbye to friends and family
- Putting affairs in order, such as making a will
- Taking great risks that could lead to death, such as driving extremely fast
- Talking or thinking about death often
Other serious warning signs that someone may be at risk for attempting suicide include:
- Displaying extreme mood swings, suddenly changing from very sad to very calm or happy
- Making a plan or looking for ways to kill themselves, such as searching for lethal methods online, stockpiling pills, or buying a gun
- Talking about feeling great guilt or shame
- Using alcohol or drugs more often
- Acting anxious or agitated
- Changing eating or sleeping habits
- Showing rage or talking about seeking revenge
Risk Factors for suicide
- Depression, other mental disorders, or substance use disorder
- Chronic pain
- A history of suicide attempts
- Family history of a mental disorder or substance use
- Family history of suicide
- Exposure to family violence, including physical or sexual abuse
- Presence of guns or other firearms in the home
- Having recently been released from prison or jail
- Exposure, either directly or indirectly, to others’ suicidal behavior, such as that of family members, peers, or celebrities
How can you help? 5 Action Steps for Helping Someone in Emotional Pain
- Ask: “Are you thinking about killing yourself?” It’s not an easy question but studies show that asking at-risk individuals if they are suicidal does not increase suicides or suicidal thoughts.
- Keep them safe: Reducing a suicidal person’s access to highly lethal items or places is an important part of suicide prevention. While this is not always easy, asking if the at-risk person has a plan and removing or disabling the lethal means can make a difference.
- Be there: Listen carefully and learn what the individual is thinking and feeling. Findings suggest acknowledging and talking about suicide may in fact reduce rather than increase suicidal thoughts.
- Help them connect with help
- Call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255), 24 hours a day, 7 days a week. The service is available to everyone.
- You can also connect 24/7 to a crisis counselor by texting the Crisis Text Line.Text HOME to 741741.
- The deaf and hard of hearing can contact the Lifeline via TTY at 1-800-799-4889.
- You can also help make a connection with a trusted individual like a family member, friend, spiritual advisor, or mental health professional.
- Stay Connected: Staying in touch after a crisis or after being discharged from care can make a difference. Studies have shown the number of suicide deaths goes down when someone follows up with the at-risk person.
Mental Health: Risks, Causes, and Treatments
Mental illnesses, in general, are thought to be caused by a variety of genetic and environmental factors, these include:
- Inherited traits. Mental illness is more common in people whose blood relatives also have a mental illness. Certain genes may increase your risk of developing a mental illness, and your life situation may trigger it.
- Environmental exposures before birth. Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When the neural networks involving these chemicals are impaired, the function of nerve receptors and nerve systems change, leading to depression and other emotional disorders.
Certain factors may increase your risk of developing a mental illness, including:
- A history of mental illness in a blood relative, such as a parent or sibling
- Stressful life situations, such as financial problems, a loved one’s death or a divorce
- An ongoing (chronic) medical condition, such as diabetes
- Brain damage as a result of a serious injury (traumatic brain injury), such as a violent blow to the head
- Traumatic experiences, such as military combat or assault
- Use of alcohol or recreational drugs
- A childhood history of abuse or neglect
- Few friends or few healthy relationships
- A previous mental illness
Treatment begins with getting a medical diagnosis to understand which mental illness may be causing your symptoms. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association, is used for diagnosis. Treatment depends on the type of mental disorder and may include medications, physicians, psychotherapist, psychiatrists, and social workers or family members.
- Psychotherapy
- Psychotherapy or “talk therapy” can help people with anxiety disorders. To be effective, psychotherapy must be directed at the person’s specific anxieties and tailored to his or her needs. A typical “side effect” of psychotherapy is temporary discomfort involved with thinking about confronting feared situations.
- Cognitive Behavioral Therapy (CBT)
- CBT is a type of psychotherapy that can help people with anxiety disorders. It teaches a person different ways of thinking, behaving, and reacting to anxiety-producing and fearful situations. CBT can also help people learn and practice social skills, which is vital for treating social anxiety disorder.
- Two specific stand-alone components of CBT used to treat social anxiety disorder are cognitive therapy and exposure therapy. Cognitive therapy focuses on identifying, challenging, and then neutralizing unhelpful thoughts underlying anxiety disorders. Exposure therapy focuses on confronting the fears underlying an anxiety disorder in order to help people engage in activities they have been avoiding.
- Stress-Management Techniques
- Stress management techniques and meditation can help people with anxiety disorders calm themselves and may enhance the effects of therapy. While there is evidence that aerobic exercise has a calming effect, the quality of the studies is not strong enough to support its use as treatment. Since caffeine, certain illicit drugs, and even some over-the-counter cold medications can aggravate the symptoms of anxiety disorders, avoiding them should be considered. Check with your physician or pharmacist before taking any additional medications.
- The family can be important in the recovery of a person with an anxiety disorder. Ideally, the family should be supportive but not help perpetuate their loved one’s symptoms. Talking with a trusted friend or member of the clergy can also provide support, but it is not necessarily a sufficient alternative to care from an expert clinician.
- Medication
- Medication does not cure anxiety disorders but often relieves symptoms. Medication can only be prescribed by a medical doctor (such as a psychiatrist or a primary care provider), but a few states allow psychologists to prescribe psychiatric medications.
- Medications are sometimes used as the initial treatment of an anxiety disorder, or are used only if there is insufficient response to a course of psychotherapy. In research studies, it is common for patients treated with a combination of psychotherapy and medication to have better outcomes than those treated with only one or the other.
- The most common classes of medications used to combat anxiety disorders are antidepressants, anti-anxiety drugs, and beta-blockers. Be aware that some medications are effective only if they are taken regularly and that symptoms may recur if the medication is stopped.
Key Takeaways for Chapter 6
- Mental health is just as important as physical health.
- Meeting our physiological needs is a necessary foundation to reaching our human potential.
- Focusing on happiness and positivity increases our overall health and wellness.
- Mental illness is very common.
- Understanding warning signs of mental illness can help yourself and others.
Media Attributions
- Maslow’s_Hierarchy_of_Needs © User:Factoryjoe, CC BY-SA 3.0 , via Wikimedia Commons is licensed under a CC BY-SA (Attribution ShareAlike) license
- Maslow, A. H. (1943). A theory of human motivation. Psychological Review, 50(4), 370–396. https://doi.org/10.1037/h0054346 ↵
- Steptoe, A. (2019). Happiness and Health. Annual Review of Public Health, 40(1), 339–359. https://doi.org/10.1146/annurev-publhealth-040218-044150 ↵
- Ackerman, C. E., MA. (2022, February 14). What is Positive Psychology & Why is It Important? PositivePsychology.Com. https://positivepsychology.com/what-is-positive-psychology-definition/ ↵
- Hansenne M. (2021). Valuing Happiness is Not a Good Way of Pursuing Happiness, but Prioritizing Positivity is: A Replication Study. Psychologica Belgica, 61(1), 306–314. https://doi.org/10.5334/pb.1036 ↵
- Algorani EB, Gupta V. Coping Mechanisms. [Updated 2021 May 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559031/ ↵
- Bailey R, Pico J. Defense Mechanisms. [Updated 2021 Jun 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559106/ ↵
- Brådvik L. (2018). Suicide Risk and Mental Disorders. International journal of environmental research and public health, 15(9), 2028. https://doi.org/10.3390/ijerph15092028 ↵
