Chapter 12: Cardiovascular Disease
How does the heart work?
What happens when a person has a heart attack or a brain attack (stroke)?
What can you do to reduce your risk of cardiovascular disease?
Can you feel it if you have high blood pressure or high cholesterol?
Chapter 12 Learning Outcomes
By the end of this chapter you will be able to:
- Describe how the cardiovascular system works
- Compare the risk and prevalence of cardiovascular disease
- Describe the common types of cardiovascular disease
- Identify risk factors for cardiovascular disease
- Interpret blood pressure and cholesterol readings
One person dies every 36 seconds in the United States from cardiovascular disease.
About 659,000 people in the United States die from heart disease each year—that’s 1 in every 4 deaths.
Heart disease is the leading cause of death in the United States, and stroke is the fifth leading cause of death.
Heart disease costs the United States about $363 billion each year from 2016 to 2017.
It is important for everyone to understand how their cardiovascular system works and the common types of diseases of the cardiovascular system.
The Cardiovascular System
Activity: Your Heart and Breath
Before you begin this chapter, take a moment to feel your heart and your breathing.
- Take your pulse.
- Count how many times your heart beats in one minute.
- In your wrist:
- hold out one of your hands, with your palm facing upwards
- press the first (index) finger and middle finger of your other hand on the inside of your wrist, at the base of your thumb – don’t use your thumb as it has its own pulse
- press your skin lightly until you can feel your pulse – if you can’t find it, try pressing a little harder or move your fingers around
-
In your neck:
- press your first finger and middle finger to the side of your neck, just under your jaw and beside your windpipe – don’t use your thumb
- press your skin lightly to feel your pulse – if you can’t find it, try pressing a bit harder or move your fingers around
- Measure your respiratory rate
- Count how many times you inhale and exhale in one minute.
- Multiple your one minute pulse and your one minute count of breaths by 1,440 to see how many times your heart beats and how many times you inhale/exhale in one day.
If your heart beats 75 times per minute, it would contract approximately 108,000 times in one day, more than 39 million times in one year, and nearly 3 billion times during a 75-year lifespan. Your heart is an amazing organ that works all day, everyday, to ensure all of the cells, tissues, and organs in your body get the oxygen and nutrients needed to survive, while also removing carbon dioxide and waste by pumping about 2,000 gallons of blood around your body. This is a lot of work for an organ about the size of your fist that weighs less than a pound.
The heart is the power, or the pumping force, behind the circulation of blood through the body. Every time your heart beats it is contracting in order to push blood, much like you would squeeze a plastic ketchup bottle and push out ketchup. The heart is just one part of the cardiovascular system, the other part are the vessels through which blood travels through the body. The heart and blood vessels are a closed-loop system, where blood moves in one direction to and from your heart.
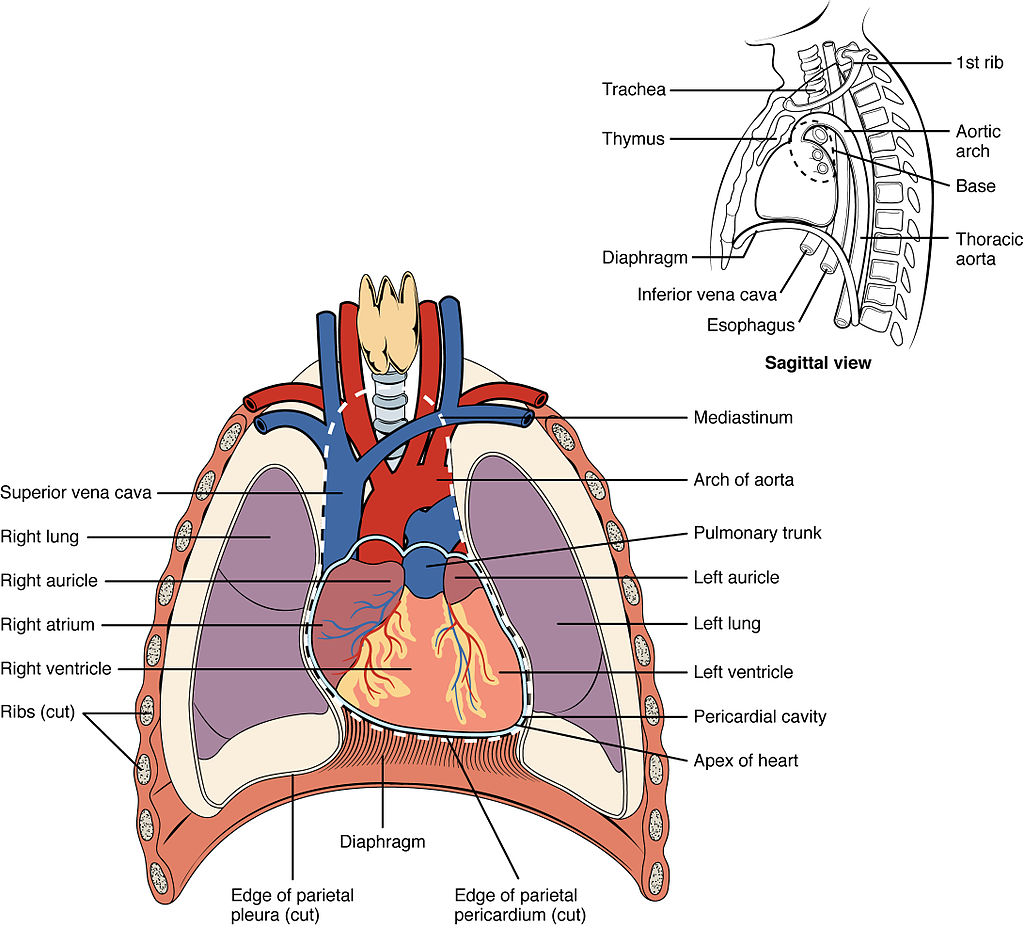
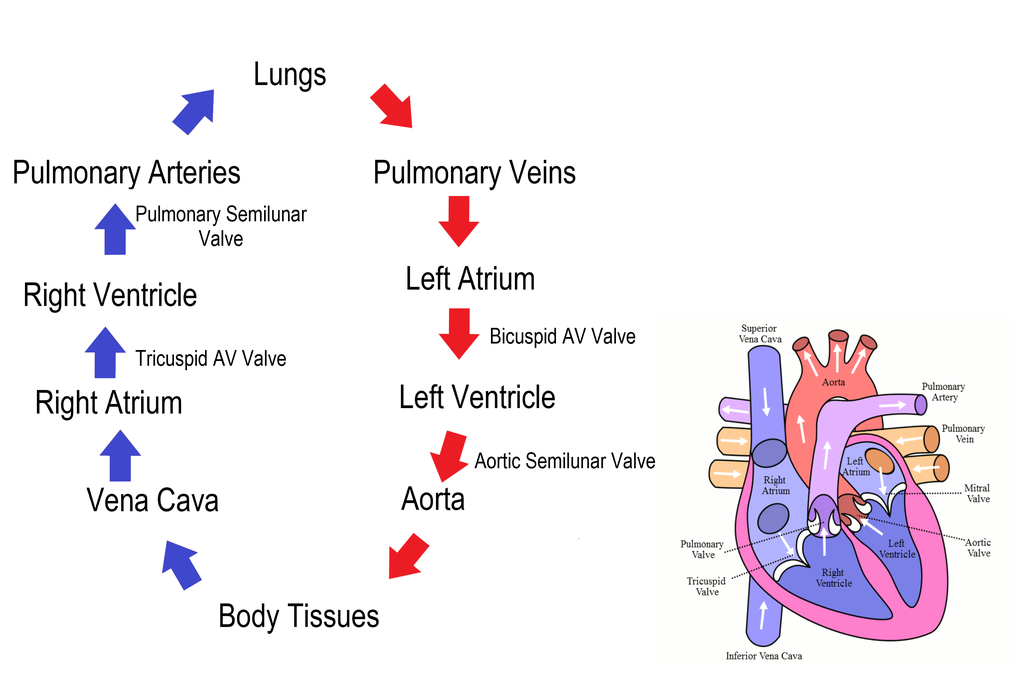
The heart has two halves, each with atria and ventricles known as the right atrium, right ventricle, left atrium, and left ventricle. As a closed-loop system, blood moves through the heart in a precise pattern.
- Deoxygenated blood enters the heart through the largest vein of the body called the superior vena cava
- The deoxygenated blood first enter the heart through the right atrium.
- The blood is then pushed down into the right ventricle.
- The deoxygenated blood now leaves the heart to go to the lungs and pick up oxygen.
- Oxygenated blood then returns to the heart through the left atrium.
- The blood is pushed into the left ventricle.
- Lastly the oxygenated blood leaves the heart to go to the body through the largest artery of the body called the aorta.
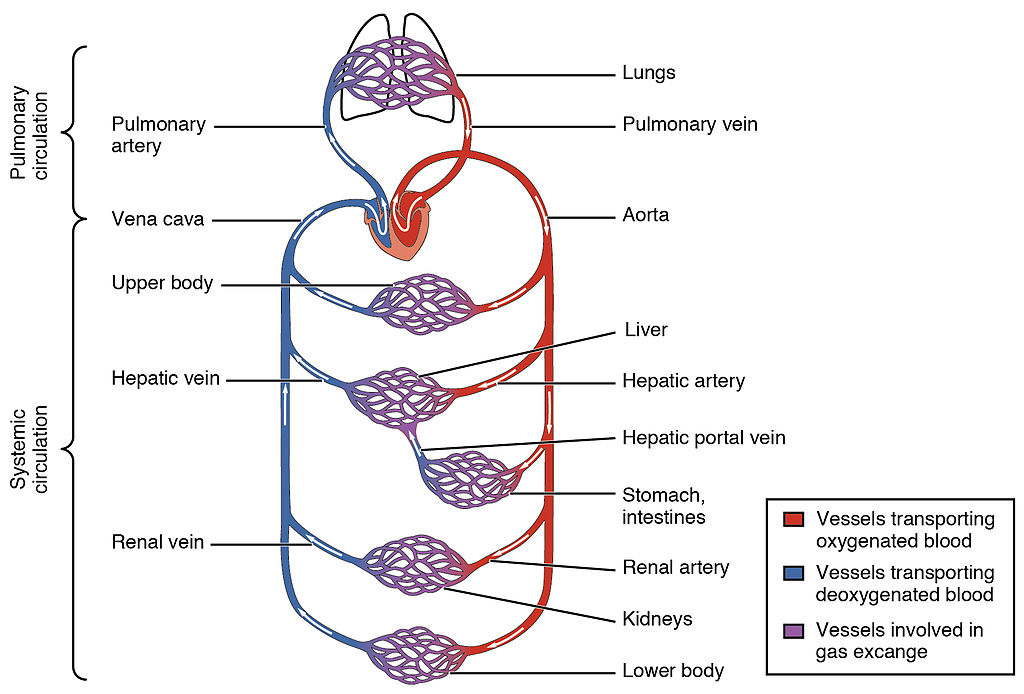
Each side of the heart plays an important role in the circulation of blood. The right side of the heart is responsible for circulating the deoxygenated blood to the lungs to pick up oxygen, called pulmonary circulation, and the left side of the heart is responsible for circulating the blood to the rest of the body, called systemic circulation.
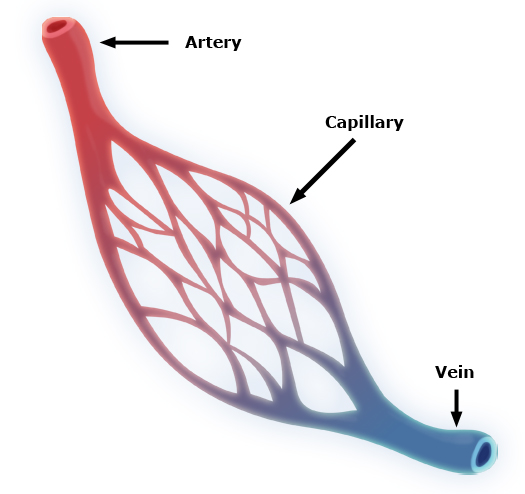
The three main types of blood vessels that transport blood throughout the body are the arteries, veins, and capillaries. In short, arteries are large blood vessels that carry blood away from the heart, veins are large blood vessels that carry blood to the heart, and capillaries are the small blood vessels that delivery oxygenated blood to organs and tissues and pick up deoxygenated blood from organs and tissues for the veins to take back to the heart. You might think of arteries and veins as big freeways or highways and the capillaries as the neighborhood streets, both working to provide a pathway to deliver food and take away waste.
In pictures of the circulatory system, arteries are typically represented by red blood vessels and veins are typically represented as blue blood vessels. Red is used for arteries because most arteries carry oxygenated blood, or red blood. Veins typically carry deoxygenated blood, or blue blood. The faster the heart beats, the more oxygen and nutrients are transported throughout the body.
Each beat of the heart helps to keep the blood moving within the closed system, however the heart has an additional feature that helps to keep the blood moving in one direction and these are called heart valves. Heart valves ensure unidirectional blood flow through the heart. Valves operate link french doors that open when the heart contracts and close when the heart is at rest. The four valves in the heart are the tricuspid valve, pulmonary valve, bicuspid valve, and aortic valve.
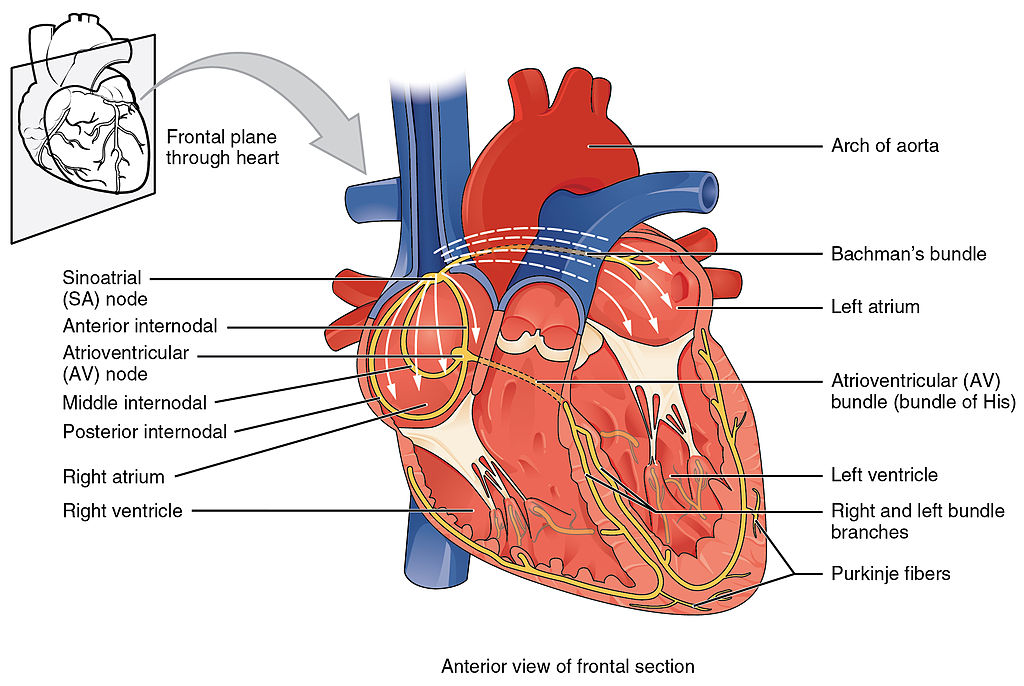
You do not tell you heart to beat, rather your heart beats automatically. For example, when your body needs more oxygen, such as when exercising, your bodies autonomic nervous system tells your heart to speed up to pump more blood throughout your body. The Autonomic nervous system specifically sends messages to a specialized group of cells located high in the right atrium, called the Sinoatrial Node, or SA node. The SA node is commonly referred to as the pacemaker of the heart and is responsible for normal cardiac rhythm by sending an electrical signal that makes the heart contract.
The contraction of the heart is called systole and the relaxation of the heart is called diastole. Imagine clenching and relaxing your fist, when it is clenched that is representing systole and when it is relaxed that is diastole. When the heart contracts (systole) and pushes blood from the heart into the blood vessel (artery) it puts pressure on the blood vessel walls. When the heart relaxes (diastole) the pressure on the blood vessel walls lowers. By measuring the pressure in the blood vessel we can better understand the health of the heart and blood vessels. Measuring the pressure created in the blood vessel is known as your blood pressure. When you get your blood pressure tested they give you two numbers, the top number is the pressure created during systole and the bottom number is the pressure created during diastole. Thus, blood pressure readings are read as systolic over diastolic pressure. Average blood pressure is considered to be 120/80 (systolic/diastolic). If the pressure increases to 140/90 you are considered to have high blood pressure.
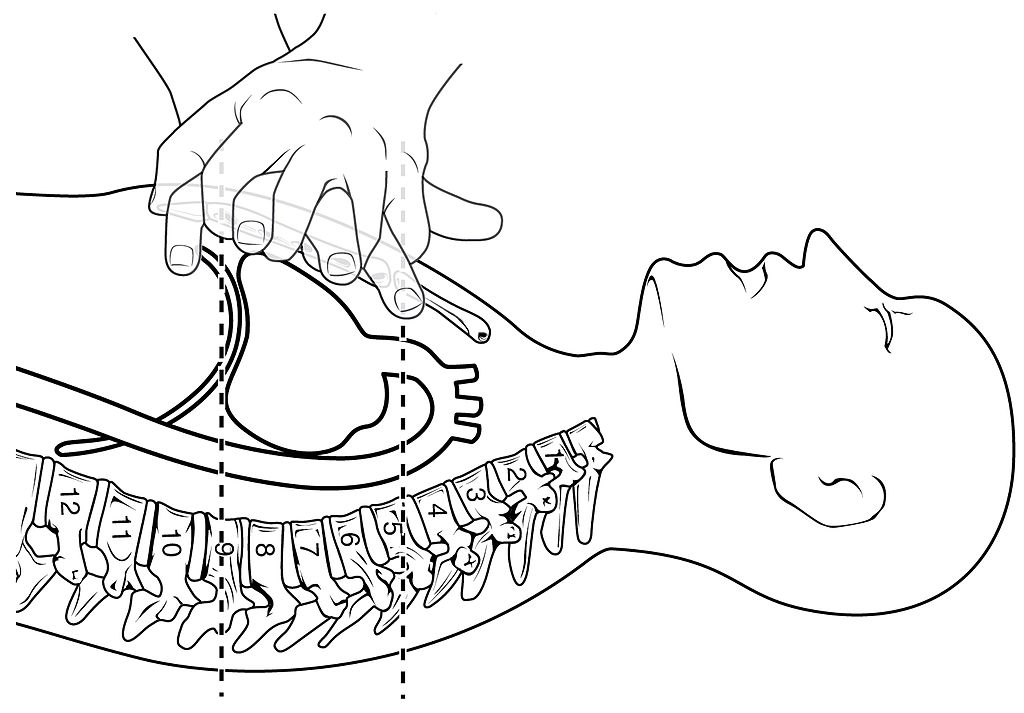
Manually Pumping Blood: CPR
If the heart stops beating, the blood can be manually pumped by using an emergency technique known as cardiopulmonary resuscitation (CPR). When performing CPR, repeated pressure is placed on the heart to push the blood through both the pulmonary and systemic circuits. This is particularly critical for the brain, as irreversible damage and death of neurons occur within minutes of loss of blood flow.
Trained first responders will perform both chest compressions and mouth-to-mouth breathing. However, bystanders should perform compression-only CPR.
- Call 9-1-1 (or send someone to do that)
- Push hard and fast in the center of the chest
Current standards call for compression of the chest at least 5 cm deep and at a rate of 100-120 compressions per minute, a rate equal to the beat in “Staying Alive,” recorded in 1977 by the Bee Gees.
Cardiovascular Disease
The cardiovascular system is an intricate system and each part of the system plays an important role in ensuring your body receives the oxygen and nutrients it needs. Diseases of the cardiovascular includes diseases effecting the various elements of the heart and diseases impacting the ability of blood to move through the blood vessels.
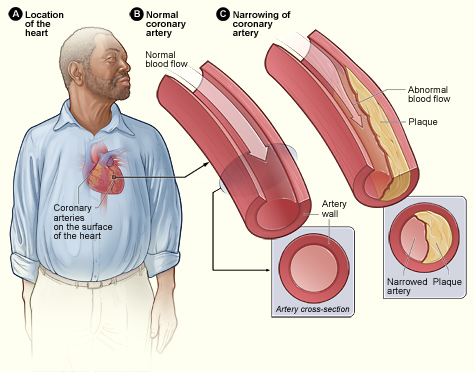
The term “heart disease” refers to several types of heart conditions. The most common type of heart disease in the United States is coronary artery disease (CAD). The coronary artery is the artery that feeds oxygenated blood to the heart muscle itself. If the coronary artery is partially or fully blocked it affects the blood flow to the heart. When the heart muscle does not get oxygenated blood this is called a heart attack.
Sometimes heart disease may be “silent” and not diagnosed until a person experiences signs or symptoms of a heart attack, heart failure, or an arrhythmia. When these events happen, symptoms may include:
- Heart attack: Chest pain or discomfort, upper back or neck pain, indigestion, heartburn, nausea or vomiting, extreme fatigue, upper body discomfort, dizziness, and shortness of breath.
- Arrhythmia: Fluttering feelings in the chest (palpitations).
- Heart failure: Shortness of breath, fatigue, or swelling of the feet, ankles, legs, abdomen, or neck veins.
The risk factors for the majority of cardiovascular diseases are high blood pressure, high blood cholesterol, and smoking. About half of people in the United States (47%) have at least one of these three risk factors. Several other medical conditions and lifestyle choices can also put people at a higher risk for heart disease, including:
- Diabetes
- Overweight and obesity
- Unhealthy diet
- Physical inactivity
- Excessive alcohol use
Coronary Artery Disease
Coronary artery disease (CAD) is the leading cause of death worldwide and the most common type of heart disease in the United States. It is sometimes called coronary heart disease or ischemic heart disease. CAD is caused by plaque buildup in the walls of the arteries that supply blood to the heart and other parts of the body, this build up is called Atherosclerosis. As the coronary blood vessels become occluded, the flow of blood to the tissues will be restricted, a condition called ischemia that causes the cells to receive insufficient amounts of oxygen, called hypoxia. Angina, or chest pain and discomfort, is the most common symptom of CAD. Although angina is the most common symptom of CAD, for some people, the first sign of CAD is when they have a heart attack.
Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way it should.
Arteriosclerosis and Atherosclerosis
Both atherosclerosis and arteriosclerosis negatively impact the ability of blood to flow freely throughout the body. Arteriosclerosis is known as the hardening of the artery and atherosclerosis is known as the thickening of the artery. Aging is a common factor in the hardening of the artery where the artery is losing elasticity and flexibility over time, however, lifestyle choices are a common factor in the thickening of the artery where plaques are building up in the artery.
Atherosclerosis is caused by an accumulation of plaque deposits of cholesterol and other substances in the artery. Plaque buildup causes the inside of the arteries to narrow over time, which can partially or totally block the blood flow. Atherosclerosis progresses slowly and often beginning in childhood and gradually progressing throughout life.
Well-documented risk factors include smoking, family history, hypertension, obesity, diabetes, high alcohol consumption, lack of exercise, stress, and hyperlipidemia or high circulating levels of lipids in the blood.
Have you ever used a plunger?
Take a moment to think about how the plumbing in a house or building works. When it works well, water comes into the house freely and waste from flushing the toilet or washing dishes flows out of the house. However, if the plumbing of a house get blocked by debris, then a backup occurs. Just like in a house, debris that blocks flow causes problems.
Angina
Angina, or chest pain and discomfort, is the most common symptom of CAD. Angina can happen when too much plaque builds up inside arteries, causing them to narrow. Narrowed arteries can cause chest pain because they can block blood flow to your heart muscle and the rest of your body.
Myocardial Infarction or “heart attack”
Myocardial infarction (MI) is the formal term for what is commonly referred to as a heart attack. It normally results from a lack of blood flow (ischemia) and oxygen (hypoxia) to a region of the heart, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque. It can also occur when a portion of an unstable atherosclerotic plaque travels through the coronary arterial system and lodges in one of the smaller vessels. The resulting blockage restricts the flow of blood and oxygen to the myocardium and causes death of the tissue. MIs may be triggered by excessive exercise, in which the partially occluded artery is no longer able to pump sufficient quantities of blood, or severe stress, which may induce spasm of the smooth muscle in the walls of the vessel.
For many people, the first clue that they have CAD is a heart attack. Symptoms of heart attack include
- Chest pain or discomfort (angina)
- Weakness, light-headedness, nausea (feeling sick to your stomach), or a cold sweat
- Pain or discomfort in the arms or shoulder
- Shortness of breath
MIs may trigger cardiac arrest, but the two are not synonymous.
Cardiac Arrest and Arrhythmia
Cardiac arrest occurs when the heart suddenly and unexpectedly stops pumping. If this happens, blood stops flowing to the brain and other vital organs. The main cause of cardiac arrest is having an arrhythmia. An arrhythmia, or irregular heartbeat, is a problem with the rate or rhythm of your heartbeat. When a person suffers from cardiac arrest, there are a number of things that could potentially be happening to their heart: they could have a rapid heart rhythm (tachycardia), a disorganized electrical rhythm that doesn’t allow heart muscles to contract (fibrillation), or they could have no electrical current passing through their heart (asystole).
Nine out of 10 people who have a cardiac arrest outside of a hospital die — often within minutes.
Important risk factors include prior cardiac arrest, coronary heart disease, heart valve disease, congenital heart defects, and arrhythmias caused by faulty gene. However, half of cardiac arrests happen to people who did not know they had a heart problem.
“Clear”
Have you watched medical shows where a doctor grabs paddles, rubs them together, yells “clear,” and then shocks or zaps the patient? They are using a machine called a defibrillator that sends an electrical shock to the heart to try to get the electrical signals in the heart to contract in their regular rhythm. Although you might believe the defibrillator is restarting the heart, it is actually stopping the heart in order to try to get the hearts electrical signal to reset and resumes beating in a normal rhythmic way.
Congenital Heart Defects
Congenital heart defects are problems with the heart that are present at birth. They are the most common type of major birth defect. Examples include abnormal heart valves or holes in the heart’s walls that divide the heart’s chambers. Congenital heart defects range from minor to severe.
Heart Valve Defects
Heart valves prevent the backward flow of blood. They are located between the chambers of the heart and where the blood leaves and returns to the heart. Healthy heart valves can fully open and close the valve during the heartbeat, but diseased valves might not fully open and close. If the heart valves are diseased, the heart can’t effectively pump blood throughout the body and must work harder to pump, either while the blood is leaking back into the chamber or against a narrowed opening. This can lead to heart failure, sudden cardiac arrest (when the heart stops beating), heart palpitations (rapid, fluttering, or pounding), shortness of breath, or swelling in your legs and feet.
Valvular disorders are often caused by carditis, or inflammation of the heart. One common trigger for this inflammation is rheumatic fever, or scarlet fever, an autoimmune response to the presence of a bacterium, Streptococcus pyogenes, normally a disease of childhood.
Congestive Heart Failure
Heart failure is often called congestive heart failure because of fluid buildup in the lungs, liver, legs, and feet. Heart failure is a serious condition that occurs when the heart can’t pump enough blood to meet the body’s needs. It does not mean that the heart has stopped but that muscle is too weak to pump enough blood. Most of heart failure cases are chronic, or long-term heart failures.
The only cure for heart failure is a heart transplant. However, heart failure can be managed with medications or medical procedures.
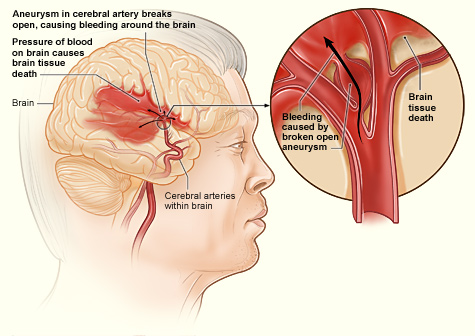
Stroke or “brain attack”
A stroke is sometimes called a “brain attack” and is formally known as a Cerebrovascular Accident (CVA). Like a heart attack, a brain attack (stroke) occurs because oxygen cannot get to the brain. With a stroke, the oxygen may not be getting to the brain because of a blockage in the blood vessel (likely due to atherosclerosis) or due to a rupture of the blood vessel. In either case, parts of the brain become damaged or die. To work properly, your brain needs oxygen. Your arteries deliver oxygen-rich blood to all parts of your brain. If something happens to block the flow of blood, brain cells start to die within minutes, because they can’t get oxygen. This causes a stroke.
Time lost is brain lost. Every minute counts.
The brain controls our movements, stores our memories, and is the source of our thoughts, emotions, and language. The brain also controls many functions of the body, like breathing and digestion. The impact of a stroke is dependent on the part of the brain that is not getting the oxygen it needs. A stroke can cause lasting brain damage, long-term disability, or even death.
There are two types of stroke:
- Ischemic stroke
- Most strokes are ischemic strokes. An ischemic stroke occurs when blood clots or other particles block the blood vessels to the brain. Fatty deposits called plaque can also cause blockages by building up in the blood vessels.
- Hemorrhagic stroke
- A hemorrhagic stroke happens when an artery in the brain leaks blood or ruptures (breaks open). The leaked blood puts too much pressure on brain cells, which damages them. High blood pressure and aneurysms are examples of conditions that can cause a hemorrhagic stroke. Aneurysms are balloon-like bulges in an artery that can cause the artery to stretch and burst.
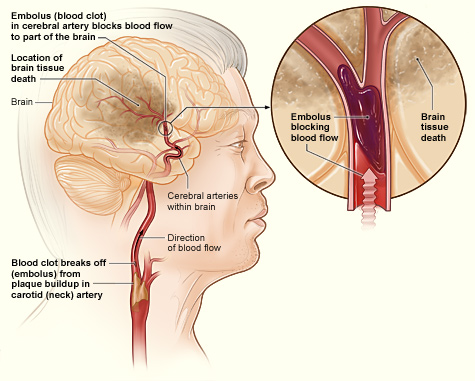
A transient ischemic attack (TIA) is sometimes called a “mini-stroke” or a “warning stroke.” It is different from the major types of stroke, because blood flow to the brain is blocked for only a short time—usually no more than 5 minutes.
- A TIA is a warning sign of a future stroke.
- A TIA is a medical emergency, just like a major stroke.
- Strokes and TIAs require emergency care. Call 9-1-1 right away if you feel signs of a stroke or see symptoms in someone around you.
- There is no way to know in the beginning whether symptoms are from a TIA or from a major type of stroke.
- Like ischemic strokes, blood clots often cause TIAs.
- More than a third of people who have a TIA and don’t get treatment have a major stroke within 1 year. As many as 10% to 15% of people will have a major stroke within 3 months of a TIA.
Treatment for Cardiovascular Diseases
The best treatment for cardiovascular diseases is prevention. By living a healthy lifestyle, you can help keep your blood pressure, cholesterol, and blood sugar levels normal and lower your risk for heart disease and heart attack.
Choose healthy habits:
- Choose healthy foods
- Maintain a healthy weight
- Exercise regularly
- Don’t smoke
Understand your own health
- Have your Cholesterol levels checked regularly
- Measure your blood pressure regularly
- Manage your blood sugar levels and control diabetes
- Go to the doctor regularly. Many of the diseases of the cardiovascular system, like blood pressure, have no symptoms, so you will not know you have it without being tested.
If you suffer from cardiovascular diseases, there are several surgeries or procedures that me be required.
Medications
There are many types and combinations of drugs used to treat coronary artery disease (CAD), and your doctor or other health care provider will decide the best treatment combination for your situation. Some of the medications available include:
- Anticoagulants: Decrease the clotting (coagulating) ability of the blood. Sometimes called “blood thinners”
- Antiplatelet agents: Keep blood clots from forming by preventing blood platelets from sticking together.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: Expand blood vessels and decreases resistance thus allowing blood to flow more easily and makes the heart’s work easier or more efficient.
- Beta blockers: Decrease the heart rate and force of contraction, which lowers blood pressure and makes the heart beat more slowly and with less force.
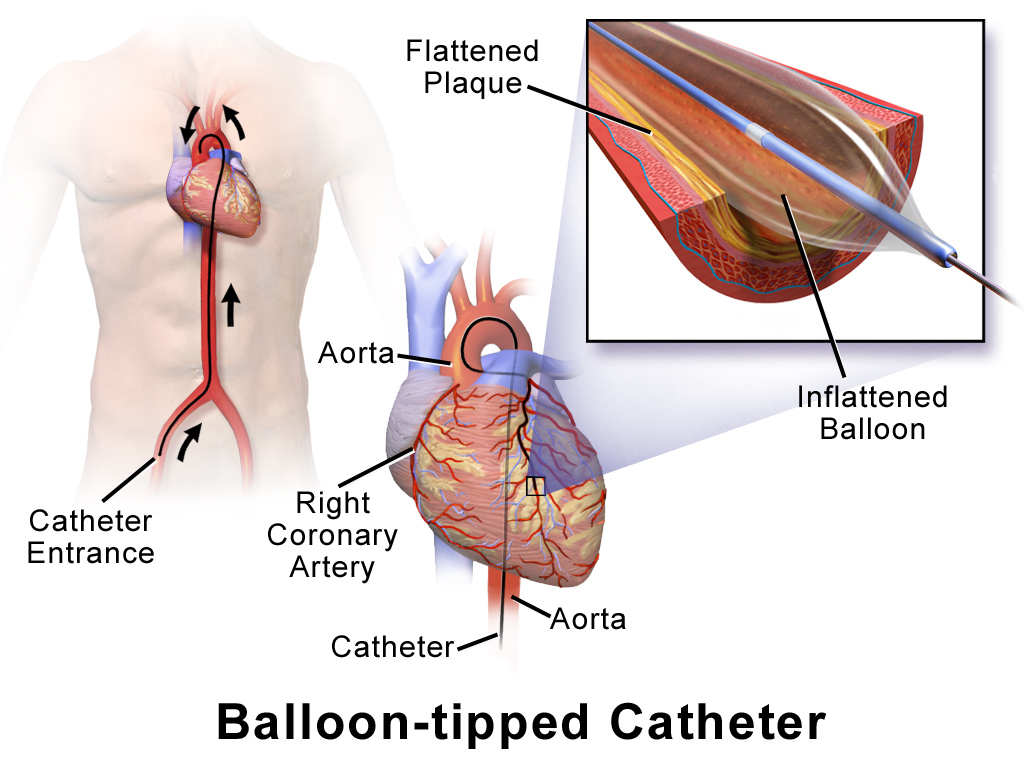
Balloon Angioplasty
Angioplasty is a procedure to improve blood flow in coronary arteries that have become narrow or blocked by mechanically widening the artery with a balloon. A specialized catheter with an expandable tip is inserted into the blocked blood vessel. The balloon is inflated to compress the plaque material and to open the vessel to increase blood flow. Then, the balloon is deflated and retracted. A stent consisting of a specialized mesh is typically inserted at the site of occlusion to reinforce the weakened and damaged walls. Stent insertions have been routine in cardiology for more than 40 years.
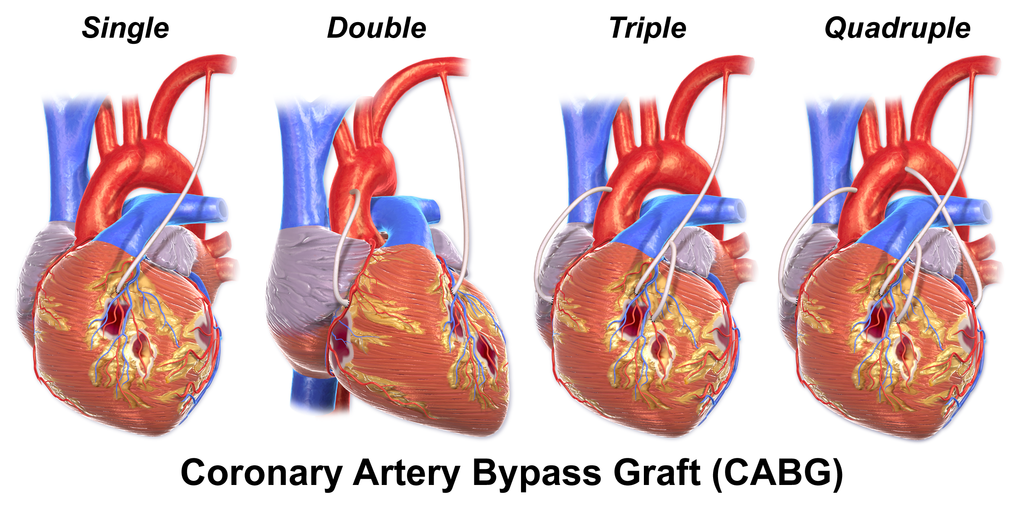
Coronary Bypass Surgery
Sometimes arteries become so damaged that they cannot be healed or fixed. When this occurs, the only option is to create a new artery and bypass the damaged one, this is known as coronary bypass surgery. You might have heard of someone having a “quadruple bypass,” what they are saying is that the surgeon had to create four new blood vessels to replace four coronary arteries that were blocked.
The surgery creates a new path for blood to flow to the heart. The surgeon takes a healthy piece of vein from the leg or artery from the chest or wrist. Then the surgeon attaches it to the coronary artery, just above and below the narrowed area or blockage. This allows blood to bypass (get around) the blockage.
Risk Factors for Cardiovascular Disease
Metabolic syndrome is a group of conditions that together raise your risk of coronary heart disease, diabetes, stroke, and other serious health problems. Metabolic syndrome is common in the United States; About 1 in 3 adults have metabolic syndrome. The good news is that it is largely preventable.
You might have metabolic syndrome if you have three or more of the following conditions:
- A large waistline: This is also called abdominal obesity or “having an apple shape.” Extra fat in your stomach area is a bigger risk factor for heart disease than extra fat in other parts of your body.
- High blood pressure: If your blood pressure rises and stays high for a long time, it can damage your heart and blood vessels. High blood pressure can also cause plaque, a waxy substance, to build up in your arteries. Plaque can cause heart and blood vessel diseases such as heart attack or stroke.
- High blood sugar levels: This can damage your blood vessels and raise your risk of getting blood clots. Blood clots can cause heart and blood vessel diseases.
- High blood triglycerides: Triglycerides are a type of fat found in your blood. High levels of triglycerides can raise your levels of LDL cholesterol, sometimes called bad cholesterol. This raises your risk of heart disease.
- Low HDL cholesterol, sometimes called good cholesterol: Blood cholesterol levels are important for heart health. “Good” HDL cholesterol can help remove “bad” LDL cholesterol from your blood vessels. “Bad” LDL cholesterol can cause plaque buildup in your blood vessels.
Risk factors you can control include:
- Lifestyle habits:
- Being inactive
- Eating an unhealthy diet and large portion sizes
- Not getting enough good quality sleep, which helps control how your body absorbs nutrients from the food you eat
- Smoking and drinking a lot of alcohol
- Occupation: Shift workers have a higher risk of metabolic syndrome because they often have circadian clocks that are not aligned with the environment. This can cause problems with how your body absorbs nutrients from food.
Risk factors you cannot control include:
- Age: Your risk of metabolic syndrome increases as you get older.
- Environment: Low socioeconomic status can lead to an unhealthy diet and an inactive lifestyle, and can cause you not to get enough sleep (sleep deprivation).
- Family history and genetics: Your genes can affect your weight or how your body responds to insulin. You have a higher risk of metabolic syndrome if others in your family have had diabetes, metabolic syndrome, or any of its risk factors.
- Other medical conditions: The following medical conditions can raise your risk of metabolic syndrome.
- Overweight and obesity are the main risk factors for metabolic syndrome because they can raise “bad” LDL cholesterol, blood triglycerides, and blood pressure, and lower “good” HDL cholesterol. Overweight and obesity during pregnancy can raise your child’s risk of metabolic syndrome. In infants, a low birth weight and rapid weight gain after birth can raise the risk of metabolic syndrome later in life.
- Polycystic ovary syndrome (PCOS) is a condition that causes fluid-filled sacs called cysts to grow on the ovaries. The hormone changes that cause PCOS can also cause you to have a large waistline, high blood sugar levels, high triglyceride levels, and low levels of “good” HDL cholesterol.
- Problems with your immune system can cause some skin diseases such as psoriasis, which raise your risk. Certain cancer treatments that affect your immune system also can raise your risk.
- Sleep problems, including not getting enough sleep (sleep deprivation), circadian rhythm disorders, and sleep apnea, can raise your risk.
- Some medicines used to treat allergies, bipolar disorder, depression, HIV, and schizophrenia also raise your risk.
- Sex: In older adults, women have a higher risk of metabolic syndrome than men. This is because changes in hormone levels after menopause can raise the risk of a large waistline, high blood sugar levels, and low levels of “good” HDL cholesterol.
Key Takeaways for Chapter
- Cardiovascular disease is the leading cause of death.
- Cardiovascular disease includes diseases of the heart and blood vessels.
- The heart is the “pumping” force behind your blood flow.
- Arteries carry blood away from the heart to your organs and tissues
- Veins carry blood back to your heart from your organs and tissues.
- Blood pressure readings show your systolic pressure over your diastolic pressure, or the pressure during contraction over your pressure during relaxation.
- Both arteriosclerosis and atherosclerosis impact the ability of blood to flow freely in your blood vessels.
- A heart attack is the blockage in a coronary artery.
- A “brain attack” or stroke is the blockage or rupture of the artery that brings oxygenated blood to the brain.
- Everyone should know how to do CPR compressions to keep blood circulating when a person heart has stopped beating.
- Risks for cardiovascular disease are highly lifestyle dependent.
Media Attributions
- Heart_Position_in_ThoraxN © OpenStax College is licensed under a CC BY (Attribution) license
- Capillary_system_CERT © Community Emergency Response Team,
- Blood_Flow_Through_the_Heart © OpenStax College is licensed under a CC BY (Attribution) license
- Circulation_of_blood_through_the_heart © Christinelmiller is licensed under a CC BY-SA (Attribution ShareAlike) license
- 2018_Conduction_System_of_Heart © OpenStax College is licensed under a CC BY (Attribution) license
- 2002_CPR_Technique © OpenStax College is licensed under a CC BY (Attribution) license
- Atherosclerosis_2011 © National Heart Lung and Blood Insitute (NIH) is licensed under a Public Domain license
- Stroke_ischemic © National Heart Lung and Blood Insitute (NIH) is licensed under a Public Domain license
- Stroke_hemorrhagic © National Heart Lung and Blood Insitute (NIH) is licensed under a Public Domain license
- 1024px-Balloon-Tipped_Catheter © BruceBlaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- Blausen_0152_CABG_All © BruceBlaus. When using this image in external sources it can be cited as:Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0 , via Wikimedia Commons is licensed under a CC BY (Attribution) license
