3.5 Implantology
The basis of dentistry is the prevention of oral disease. Wear and tear, and trauma can cause tooth loss regardless of prevention practices. These healthy patients are perfect candidates for tooth replacement by dental implants.
A dental implant is an implantable medical device that replaces single teeth, multiple teeth or entire arches.
Once it’s determined that the patient is a good candidate for dental implants and the treatment plan has been elected, the next aspect of implantology to consider is system. System is usually determined by the referring dentist or lab that a dentist is using to fabricate the prosthetic portion of the implant (crown, bridge, or denture).
KEEP IT STERILE: There is a high risk of bone infection (osteomyelitis), and specifically peri-implantitis when placing dental implants because the surgery involves drilling into bone. Osteomyelitis and peri-implantitis can be disastrous to successful dental implants because it is difficult to rid the bone of infection, and maintaining asepsis and sterile surgical procedures are the best method of prevention. Implant placement is an invasive procedures that can introduce bacteria into bone.
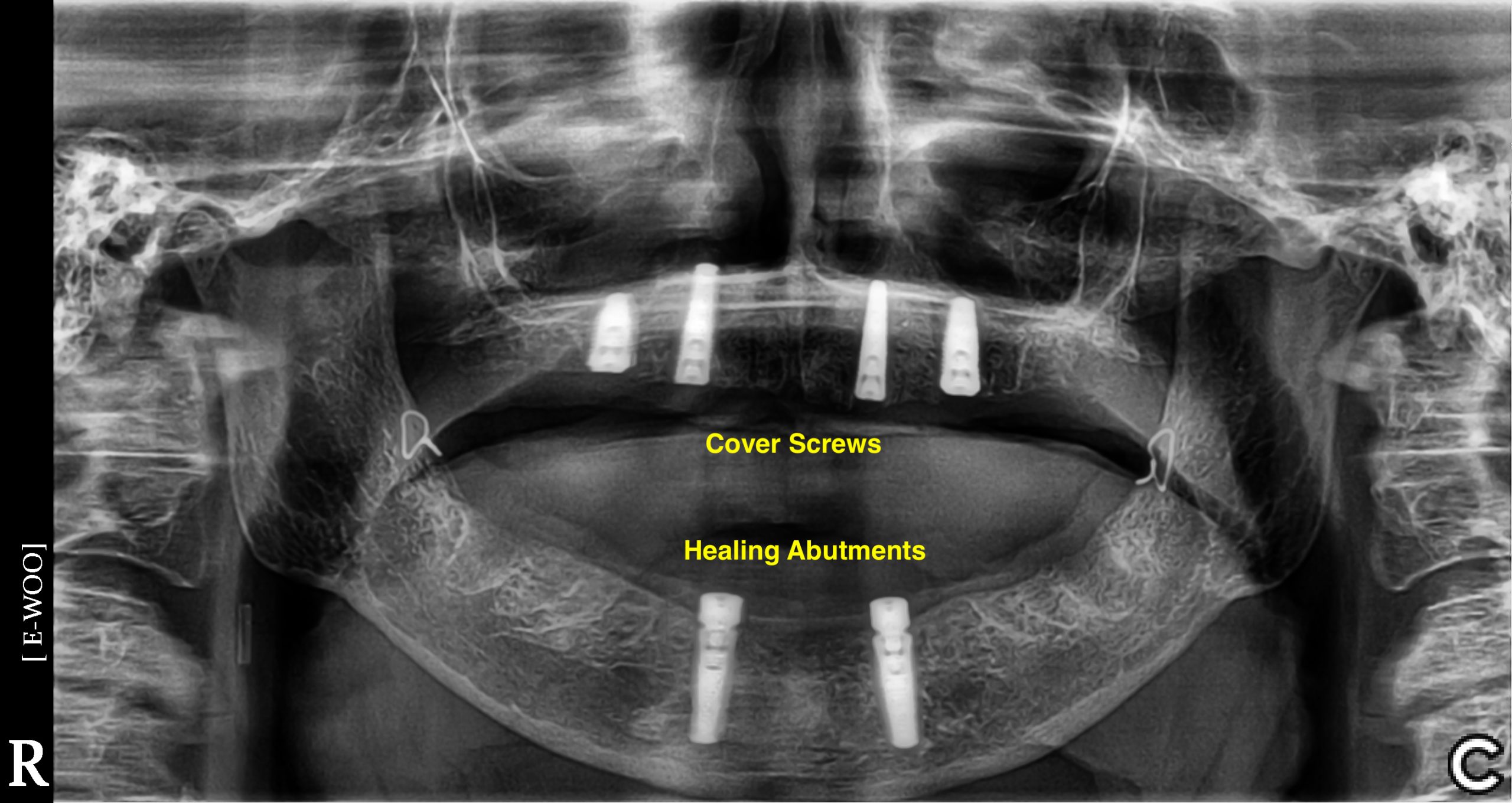
- Implant with Cover Screw
- Implant with Healing Abutment
- Multiple Implants
- All-on-4 Max & Mand
Categories:
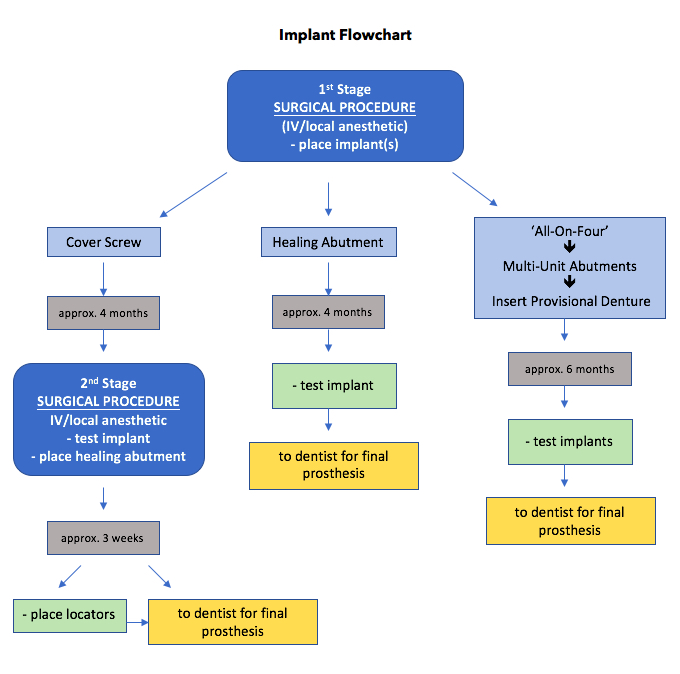
- First Stage Surgery with Cover Screw: a flap is elevated and the implant is placed using a specialized console, handpiece, and a system specific surgical kit containing osteotomy drills, and attachments. A cover screw is placed and the flap is sutured. The patient returns in approximately 4 months for Second Stage Surgery – a flap is elevated, the cover screw is removed and an osseointegration check is performed. A healing abutment is placed, and the flap is closed around the healing abutment leaving it exposed above the tissues – the tissues heal around the abutment. The tissues are allowed to heal for approximately 2 weeks before an impression or digital scan is obtained for the new implant crown (or bridge, etc.). The healing abutment is replaced to hold the tissues in place while the crown is being fabricated.
- First Stage with Healing Abutment: a flap is elevated and the implant is placed using a specialized console, handpiece, and a system specific surgical kit containing osteotomy drills, and attachments. A healing abutment is placed and the flap is closed around the healing abutment leaving it exposed above the tissues – the tissues heal around the abutment. The patient returns in approximately 4 months, the healing abutment is removed, an osseointegration check is performed, and an impression or digital scan is obtained. The healing abutment is replaced to hold the tissues in place while the crown is being fabricated. NOTE: sometimes a temporary crown is placed instead of a healing abutment – this occurs in the esthetic zone (the anteriors) to provide superior gingival contour in preparation for the final crown.
- First Stage with Provisional Denture Conversion: the implant is placed and instead of a cover screw or healing abutment, the implant is loaded with a provisional crown or denture. The patient returns in approximately 6 months for an osseointegration check. A final denture is fabricated.
REMEMBER: The First Stage of implant placement requires the Sterile Technique and is performed with or without Sedation.
Armamentarium FIRST STAGE:
• REMOVE FORCEPS and ELEVATORS from Surgical Tray
PROCEDURE SPECIFIC CHECKLIST (here is a customizable template: Surgical Procedure Checklist)
Italics = OPEN ONLY AS DIRECTED
• #12 scalpel blade
• #15 scalpel blade
• Barriers (sterile): light handles, unit handle, hose covers
• Bite Block: edentulous
• Bone Mill
• Bone Trap with suction tips
• Cautery
• Chlorhexidine & Bowl: for provisional appliance
• Discoid/Cleoid carver
• Face Prep Sponge
• Gauze: sterile 2×2’s & 4×4’s
• Graft Bin: allograft, bone scraper, membranes
• Handpiece and Hose
• Implant Console
• Implant Handpiece
• Implant Surgical Kit
• Implants
• Implant Healing Abutments/Cover Screws
• Kidney Basin
• Magnetic Drape
• Patient Drape: sterile (large)
• Personal Protection Equipment: Sterile Gowns, Sterile Gloves, Bonnets, Masks
• Retractors: Right Angle
• Saline: sterile
• Sterile back counter drape, implant cart drape
• Sinus Instruments: maxilla (include osteotomes and mallet)
• Suction Tubing
• Sutures: 3.0 or 4.0 chromic gut (surgeon’s preference)
• Towel Clamps
• Sutures: silk
• Sutures: vicryl
• Tissue Glue
Denture Conversion (ADD)
• Curing Light
• Implant Multi-Unit Abutments (MUA’s)
• Impression Putty (standard set) & Tray
• Prosthetic Kit: for MUA’s
• Tackle-box: impression copings, replicas, temporary abutments, comfort caps
• Triad
• Teflon Tape and Fermit
The Second Stage of implant placement requires the Aseptic Technique.
Armamentarium SECOND STAGE:
• REMOVE FORCEPS and TOOTH ELEVATORS from BASIC OMS TRAY WITH SUCTION
• Implant system specific prosthodontic/processing kit
• Healing or locator abutments
Preoperative Considerations:
• Follow written Pre Op Instructions (sedation).
• Check if a denture will be converted following surgery: ensure that denturist or dentist has coordinated fabrication.
Intraoperative Considerations:
• Grafting often occurs during surgery: ensure that grafting materials are in the operatory.
• Excessive bleeding during surgery may require the use of cauterization. Ensure that the cautery unit is at hand.
• Effective assisting is required: do not desiccate surgical site with suction, and be mindful of the mental foramen and the inferior alveolar nerve.
Postoperative Considerations:
• Follow written Post Op Implant Instructions.
• There is a risk of peri-implantitis which is a latent inflammation of the periodontium (it’s not caused by the surgery itself, rather it is caused by other risk factors such as poor oral hygiene, and smoking: POST-OP CONSIDERATIONS!!
• Care of provisional: healing abutment, temporary crown or denture.
• No chewing on provisional until integration is confirmed.
REMEMBER: All implant components must be recorded for warranty purposes. This can be done online AND a backup copy is recommended. Each item comes with a discrete Lot and Reference number on stickers that must be placed in the patient’s chart and a practice wide filing system (sorted by date).
NOTE: No implant system is endorsed or promoted in this publication