Chapter 4: Human Digestion
“Life comes through food.”
-Turkish proverb
Your body requires dozens of nutrients in order to function properly. We eat foods that contain these nutrients, and our bodies digest, absorb, transport, and store them for use by the multiple organ systems that make up the human body. Understanding nutrition requires an understanding of how these organ systems function and work together to make us who we are. In this chapter we will explore how the body is organized, the digestive process, and problems that can occur in digestion that affect other organ systems.
Learning Objectives
- Differentiate between mechanical and chemical digestion and describe digestive activities in each category.
- Identify the anatomy of the digestive system and its secretions that aid digestion.
- Explain the functional physiology of the digestive system organs and their secretions.
- Describe how foods and nutrients are digested, absorbed, and transported, and stored.
- Describe digestive disorders that can compromise health including risk factors, symptoms, treatment, and prevention.
4.1 The Building Blocks of the Human Body
In order to understand the human body, we have to understand a little bit about chemistry. We are made from chemicals, food is made from chemicals, and so the interplay between food and the body is a chemical process. Fundamentally, everything in and around us is made from atoms which are the basic units of matter. Some atoms have a positive charge, some have a negative charge, and some have no charge (neutral). Charged atoms (either + or – ) are called ions. Many of the essential minerals we must consume in our diets like calcium (Ca+2), sodium (Na+), potassium (K+), and chloride (Cl–) are ions. When ions with opposite charges combine together it’s called a chemical bond which “glues” the atoms together. For example, when sodium (Na+) combines with chloride (Cl–), sodium chloride (NaCl) is formed. NaCl is the chemical formula for table salt. Another example is when we combine hydrogen (H+) with oxygen (O-2) to get H2O or water. This combination of two or more atoms is called a molecule, and often they can be very large. Even larger, more diverse molecules are called macromolecules. Common macromolecules in nutrition are carbohydrates, proteins, and lipids. Molecules and macromolecules can combine to form functional units that are called cells.
The Cell
A cell is the smallest and most basic form of life. Robert Hooke, one of the first scientists to use a light microscope, discovered the cell in 1665. In all life forms, including bacteria, plants, animals, and humans, the cell was defined as the most basic structural and functional unit. Based on scientific observations over the next 150 years, scientists formulated the cell theory, which is used for all living organisms no matter how simple or complex.
The cell theory incorporates three principles:
- Cells are the most basic building units of life. All living things are composed of cells. New cells are made from preexisting cells, which divide in two. Who you are has been determined because of two cells that came together inside your mother’s womb. The two cells containing all of your genetic information (DNA) united to begin making new life. Cells divided and differentiated into other cells with specific roles that led to the formation of the body’s numerous body organs, systems, blood, blood vessels, bone, tissue, and skin. As an adult, you are comprised of trillions of cells. Each of your individual cells is a compact and efficient form of life—self-sufficient, yet interdependent upon the other cells within your body to supply its needs.
- Independent single-celled organisms must conduct all the basic processes of life. The single-celled organism must take in nutrients (energy capture), excrete waste, detect and respond to its environment, move, breathe, grow, and reproduce. Even a one-celled organism must be organized to perform these essential processes. All cells are organized from the atomic level to all its larger forms. Oxygen and hydrogen atoms combine to make the molecule water (H2O). Molecules bond together to make bigger macromolecules. The carbon atom is often referred to as the backbone of life because it can readily bond with four other elements to form long chains and more complex macromolecules. As we discussed previously, we call any molecule that contains the carbon atom an organic molecule. Four macromolecules—carbohydrates, lipids, proteins, and nucleic acids—make up all of the structural and functional units of cells.
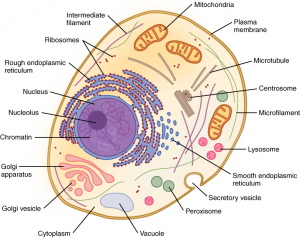
- Although we defined the cell as the “most basic” unit of life, it is structurally and functionally complex (see Figure 4.1.1). A cell can be thought of as a mini-organism consisting of tiny organs called organelles. The organelles are structural and functional units constructed from several macromolecules bonded together. A typical animal cell contains the following organelles:
-
- Nucleus: Houses the genetic material DNA
- Mitochondria: Generates energy (“powerhouse” of a cell)
- Ribosomes: Protein manufacturing facility
- Endoplasmic reticulum: Modifies proteins and manufactures lipids
- Golgi body: Sorts and tags protein and lipids so that they end up in the right places
- Lysosomes and peroxisomes: Little “digestive pouches” which break down macromolecules and destroy foreign invaders
All of the organelles are anchored in the cell’s cytoplasm via a cytoskeleton. The cell’s organelles are isolated from the surrounding environment by a plasma membrane.
Tissues, Organs, Organ Systems, and Organisms
While unicellular (single-celled) organisms can function independently, cells must combine to form more complex multicellular organisms. The cells of multicellular organisms are dependent upon each other and are organized into five different levels in order to coordinate their specific functions and carry out all of life’s biological processes.
- Cells: Basic structural and functional unit of all life. Examples include red blood cells and nerve cells.
- Tissues: Groups of cells that share a common structure and function and work together. There are four types of human tissues:
- Connective, which connects tissues;
- Epithelial, which lines and protects organs;
- Muscle, which contracts for movement and support; and
- Nerve, which responds and reacts to signals in the environment.
- Organs: Group of tissues arranged in a specific manner to support a common physiological function. Examples include the brain, liver, and heart.
- Organ systems: Two or more organs that support a specific physiological function. Examples include the digestive system and central nervous system. There are 11 organ systems in the human body (Table 4.1.1)
- Organism: Complete living system capable of conducting all of life’s biological processes.
Table 4.1.1 Overview of Organ Systems
Organ System Components Main Functions Cardiovascular Heart, blood, blood vessels Transport of substances to body tissues Digestive Gastrointestinal tract and accessory organs Ingest and digest food, absorb nutrients, and excrete wastes Endocrine Glands and hormones Regulates body processes such as nutrient use, metabolism, and reproduction Immune Lymphatic vessels, lymph containing white blood cells, mucus, bone marrow Protects against foreign invaders such as bacteria and viruses Integumentary Skin, hair, nails, sweat glands Barrier to pathogens; helps regulate body temperature Muscular Muscles (skeletal, smooth, cardiac) Voluntary and involuntary movement Nervous Brain, spinal cord, sensory and motor nerves Sense environmental changes and create appropriate reactions Reproductive Gonads (testes and ovaries), genitals, mammary glands (breasts) Reproductive functions Respiratory Lungs, nose, mouth, throat, trachea Gas exchange between lungs and air Skeletal Bones, cartilage, joints Support and structure; storage site for some minerals Urinary Kidneys, bladder, ureters Removal of metabolic waste products; water balance
Food For Thought
Think about how the body is organized. If the body becomes disorganized by a disease or disorder what happens to its function? One example is a leg fracture and movement. Can you think of any other examples?
An Organism Requires Energy and Nutrient Input
All of the organ systems must work together so that the entire organism will survive and thrive. Energy is required in order to build molecules into larger macromolecules, and to turn macromolecules into organelles and cells, and then turn those into tissues, organs, and organ systems, and finally into an organism. Proper nutrition provides the necessary nutrients to make the energy that supports life’s processes. Your body builds new macromolecules from the nutrients in food.
Nutrient and Energy Flow
Energy is stored in a nutrient’s chemical bonds. Energy comes from sunlight, which plants then capture and via photosynthesis, use to transform carbon dioxide (CO2) in the air into the molecule glucose. When the glucose bonds are broken, energy is released. Bacteria, plants, and animals (including humans) harvest the energy in glucose via a biological process called cellular respiration. In this process the chemical energy of glucose is transformed into cellular energy in the form of the molecule adenosine triphosphate (ATP). Cellular respiration requires oxygen (aerobic) which is a waste product of photosynthesis. The waste products of cellular respiration are CO2 and water, which plants use to conduct photosynthesis again. Thus, energy is constantly cycling between plants and animals. As energy is consumed nutrients are recycled within it. All life is composed of cells capable of transforming small organic molecules into energy. How do complex organisms such as humans convert the large macromolecules in the foods that we eat into molecules that can be used by cells to make cellular energy? In the next section, we will discuss the physiological process of digestion to help to answer this question.
4.2 The Digestive Process
The process of digestion begins even before you put food into your mouth. Sights and smells influence your body’s preparedness for food. Smelling food sends a message to your brain. Your brain then tells the mouth to get ready, and you start to salivate in preparation for a meal.
Once you have eaten, your digestive system starts the process that breaks down the components of food into smaller components that can be absorbed and taken into the body. Another word for the breakdown of complex molecules into smaller, simpler molecules is catabolism or a “catabolic reaction.” To do this, catabolism functions on two levels, mechanically to move and mix ingested food and chemically to break down large macromolecules into smaller molecules. This chemical break down of macromolecules is done by the addition of water, a process called hydrolysis (“hydro” = water, “lysis” = to break apart). Once the smaller particles have been broken down into their nutrient components, they will be absorbed into the blood and delivered to cells throughout the body to be used for energy or as building blocks, creating new molecules needed for cell function. When nutrients combine to form new molecules such as protein, storage fat, or glycogen, they do so in a process called dehydration synthesis or condensation which is the opposite of hydrolysis. Water (H2O) is removed (an -OH from one molecule and -H from another), and the two molecules combine to form one larger molecule. Single units can be added in this way until macromolecules are formed.
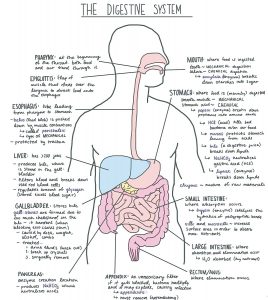
The digestive system is composed of several hollow tube shaped organs including the mouth, pharynx, esophagus, stomach, small intestine, large intestine, and rectum. It is lined with mucosal tissue that secretes digestive juices which aid in the breakdown of food and mucus which makes the walls “slippery” and aids the propulsion of food through the digestive tract. Smooth muscle tissue surrounds the digestive organs and its contraction produces waves, known as peristalsis, that propel food down the tract.
There are four steps in the digestive process:
- Ingestion is the collection of food into the digestive tract. It may seem like a simple process, but ingestion involves smelling food, thinking about food, and the involuntary release of saliva in the mouth to prepare for food entry.
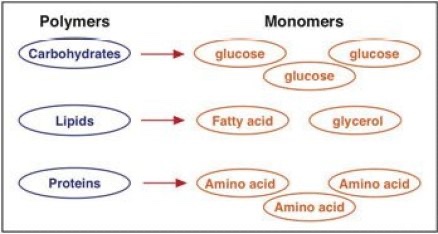
Figure 4.2.1 The Digestive Process - Digestion is the mechanical and chemical breakdown of food to its smallest particles, which will be processed into energy or used as building blocks for body tissues.
- Absorption is the process of moving the smallest particles from food into the blood for transportation throughout the body.
- Excretion is the process of eliminating any substances in food that were not absorbed.
Although it varies widely from person to person and from meal to meal, it can take anywhere from 24 to 72 hours for a meal to travel completely through the digestive tract and the steps listed above.
Throughout our discussion of the digestive system, both the mechanical and chemical breakdown of food will be addressed. Each of these forms of digestive activity play essential roles in helping us gain the required nutrients from the foods we eat.
The mechanical form of digestion is the physical “breaking apart” of food particles into physically smaller forms. There are several different forms of mechanical breakdown including:
- Mastication (chewing, crushing, and grinding with teeth)
- Moistening and softening (saliva and mucus)
- Peristalsis and segmentation (muscle contractions of the digestive tract that mix and propel foods downward and through the digestive organs)
The chemical form of digestion involves enzymes, which break apart the components in food by splitting chemical bonds that held the macromolecules (carbohydrates, protein, lipids) together. These enzymes are secreted by the salivary glands, stomach, pancreas, and small intestine.
4.3 General Anatomy and Physiology of the Digestive Tract
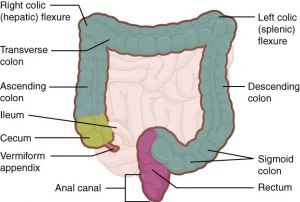
The digestive tract (also called the gastrointestinal or GI tract or the alimentary canal) consists of all of the organs that contribute to the digestive process where food moves through. The entrance to the GI tract is the mouth, the exit is the anus or anal sphincter. Food moves through the mouth, esophagus, stomach, small intestine, and large intestine—muscular tube-like organs that extend 26 to 30 feet. The organs of the GI tract are separated by muscular rings called sphincters. These sphincters relax and contract, opening and closing to allow food to move from organ to organ in an organized manner.
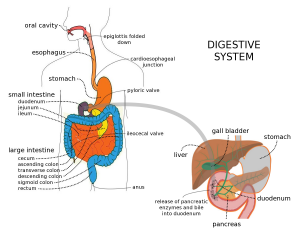
The digestive system also contains accessory organs that secrete a variety of chemical agents like enzymes, hormones, and acid that aid the chemical digestion process. These accessory organs are the salivary glands, liver, gallbladder, and pancreas.
From the Mouth to the Stomach
The digestive process begins in the mouth where ingestion of food occurs, and digestion begins with the mechanical and chemical breakdown of foods. Mechanical breakdown starts with mastication (chewing). Teeth crush and grind large food particles, while saliva from the salivary glands contributes to the mechanical breakdown by softening and moistening food which enables its movement downward. Salivary glands also begin the chemical breakdown of macronutrients with the secretion of the first chemical enzymes, salivary amylase and lingual lipase.
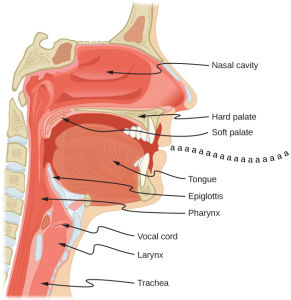
The mass of partially broken down food is called a bolus, which moves down the digestive tract as you swallow. Swallowing may seem voluntary at first because it requires conscious effort to push the food with the tongue back toward the throat, but after this, swallowing proceeds involuntarily, meaning it cannot be stopped once it begins. As you swallow, the bolus is pushed from the mouth through the pharynx which is the area at the back of the throat. In the pharynx, two “tubes” sit side by side. One, the trachea, transports air from the nose and mouth into the lungs. The other, the esophagus, is a muscular tube that connects the mouth to the stomach. As the bolus is swallowed it travels through the pharynx, and a small flap called the epiglottis closes off the trachea to prevent choking by keeping food from going into the lungs. It is impossible to breathe and swallow at the same time, and your mother was right when she said “don’t talk with your mouth full.” Problems with swallowing are called dysphagia, which will be discussed in greater detail in Chapter 18.
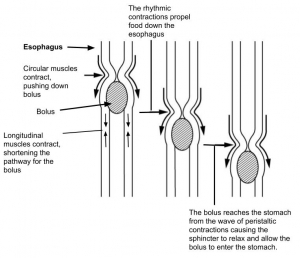
Two different types of muscular contractions, called peristalsis and segmentation, move and mix the food in various stages of digestion through the GI tract. Peristalsis is circular waves of smooth muscle contraction that propel food forward. With segmentation, the smooth muscle contractions push the food from the sides, dividing the bolus into “segments.” Another way to think about peristalsis and segmentation is to consider how toothpaste leaves a tube. Sometimes it’s pushed from the end of the tube (like peristalsis), and sometimes it leaves by squeezing the sides of the tube (like segmentation). These contractions begin at the start of the esophagus and propel the food downward to the stomach.
At the junction between the esophagus and stomach there is a sphincter muscle that remains closed until the food bolus approaches. The pressure of the food bolus stimulates the lower esophageal sphincter (also called the gastroesophageal sphincter) to relax and open allowing the bolus to move from the esophagus into the stomach. Solid food takes between four and eight seconds to travel down the esophagus, and liquids take about one second.
From the Stomach to the Small Intestine
The stomach is the most muscular of all of the digestive organs, having three layers of muscle—a longitudinal layer, a circular layer, and an oblique layer (Figure 4.3.4). When food enters the stomach, these muscle layers contract causing powerful peristaltic contractions which help mash, pulverize, and churn food into chyme. Chyme is a semi-liquid mass of partially digested food that also contains gastric juices secreted by cells in the stomach. Gastric juices contain mucus, hydrochloric (HCl) acid and the enzyme pepsin, that chemically break down proteins into smaller molecules. The stomach has three basic tasks:
- To briefly store food
- To mechanically and chemically break down food
- To empty partially broken down food (chyme) into the small intestine
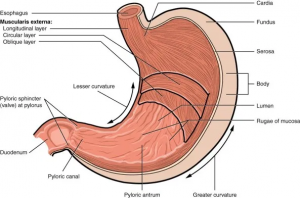
The length of time food spends in the stomach varies by the macronutrient composition of the meal. A high fat or high protein meal takes longer to break down than one rich in carbohydrates. It usually takes a few hours after a meal to empty the stomach contents completely.
Chyme is secreted through the pyloric sphincter between the stomach and the small intestine about a tablespoon (about the size of the first part of your thumb) at a time. The small intestine (also called the small bowel) is a hollow tube that folds and coils. It is 1-1.5 inches in diameter and is the longest organ of the digestive system, measuring 12 to more than 20 feet in adults. It is structurally divided into three sections: the duodenum (8-10 inches long), the jejunum (7-10 feet long), and the ileum (10-12 feet long).
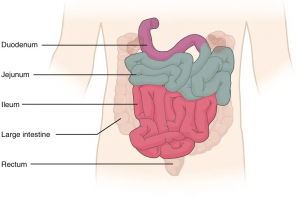
The small intestine is the site of most chemical digestion and absorption of nutrients from the foods we eat. When the chyme enters the duodenum (the first segment of the small intestine), the pancreas and gallbladder are stimulated and release juices that aid in chemical digestion. The pancreas secretes up to 1.5 liters (about 0.4 gallons) of pancreatic juice through a duct into the duodenum per day. This fluid consists mostly of water, but it also contains bicarbonate ions that neutralize the hydrochloric acid of the stomach-derived chyme and enzymes that further breakdown carbohydrates, protein, and lipids. The gallbladder secretes a much smaller amount of fluid, called bile, to help digest fats, through the same duct that leads to the duodenum. Bile is made in the liver and stored in the gallbladder. Its components act like detergents by surrounding fats similar to the way dish soap removes grease from a frying pan. This process is called emulsification and it allows for the movement of fats in the watery environment of the small intestine.
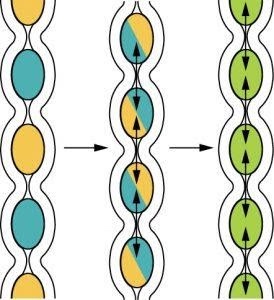
Peristalsis continues to propel food through the entirety of the small intestine, and segmentation from circular muscle contraction slows movement in the small intestine by forming temporary “sausage link” type of segments that allows chyme to slosh food back and forth in both directions to promote mixing of the chyme with digestive juices to enhance nutrient absorption.
Almost all of the components of food are completely broken down to their simplest unit within the duodenum of the small intestine. Instead of carbohydrates, protein, and lipids, the chyme now consists of their nutrient building blocks: monosaccharides, amino acids, emulsified fatty acids, vitamins, minerals, and water.
From the Small Intestine to the Large Intestine
The process of digestion is fairly efficient. Any food that is still incompletely broken down (usually less than 10% of food consumed) and the food’s indigestible fiber content moves from the small intestine through the ileocecal sphincter to the large intestine which also has three sections: the cecum, the colon (the largest portion), and the rectum. (Please note however, that colloquially the entire large intestine is referred to as the colon.) The ileocecal sphincter connects the last part of the small intestine (ileum) with the first part of the large intestine (cecum). The main task of the large intestine is to reabsorb water. Remember, water is present not only in solid foods, but the stomach releases a few hundred milliliters (ml) of gastric juice and the pancreas adds approximately another 500 ml (or nearly 17 fluid oz; a little more than a pint) of fluid during the digestion of the meal. For the body to conserve water, it is important that the water be reabsorbed. It is also important for compacting the body’s waste, making the last function of the digestive system, excretion, easier.
In the large intestine, no further chemical or mechanical breakdown of food takes place, unless it is accomplished by the bacteria that inhabit this portion of the digestive tract. There are billions of microorganisms living in and on the human body, but the largest population resides in the intestines, especially the large intestine. The great majority of bacteria in the large intestine are harmless and many are beneficial. This population of microorganisms includes not only bacteria but also viruses, fungi, and parasites, and is called the microbiome. Over the last 20 years the study of these microorganisms has expanded dramatically and scientists are finding that these organisms help us digest our food, produce some vitamins, improve our immune system, and protect us from harmful disease causing bacteria. They may also play a role in our weight.
From the Large Intestine to the Anus
After a few hours in the stomach, plus three to six hours in the small intestine, and about 16 hours in the large intestine, the digestion process enters step four, which is excretion, the elimination of indigestible food as feces. Fecal matter contains indigestible food and gut bacteria (almost 50% of content). It is stored in the rectum until it is expelled through the anus (anal sphincter) via defecation.
Sphincter Review
There are four sphincters within the GI tract that are located between digestive organs. These sphincters are rings of muscle that open and close to allow food to pass from one organ to another, helping to control the flow of food.
- Gastroesophageal Sphincter (lower esophageal sphincter): between the esophagus and stomach
- Pyloric Sphincter: between stomach and duodenum of the small intestine
- Ileocecal Sphincter: between the ileum of the small intestine and the cecum of the large intestine
- Anal Sphincter (anus): at the end of the large intestine
The Gut Microbiome
Lately you may have heard about how important fermented foods may be for health. Regular consumption of yogurt, kombucha, kefir, sauerkraut, tempeh, tofu can improve gut health by diversifying the microorganisms that reside there – the gut microbiome. This collection of microorganisms is currently an intense area of research, and it seems that the more diverse the population, the better it is for health. A typical Western diet high in processed foods and sugar, red meats, and low in fiber reduces microbiome diversity, and may contribute to conditions such as irritable bowel syndrome and inflammatory bowel diseases such as Crohn’s or ulcerative colitis. Other chronic conditions such as obesity and type 2 diabetes may also be linked to a lack of microbiome diversity. The good news is that you can diversify your gut microbiome by consuming not only the fermented foods listed above, but also by consuming whole, non-processed plant foods that are high in fiber and micronutrients.
4.4 Absorption and Distribution of Nutrients
The third step of the digestive process, nutrient absorption, takes place in the remaining length of the small intestine, the jejunum and ileum. The way the small intestine is structured gives it a huge surface area to maximize nutrient absorption. The surface area is increased by folds and finger-like projections called villi which are covered in even smaller finger-like projections called microvilli. This surface resembles a hair brush, and is often called the “brush border.”
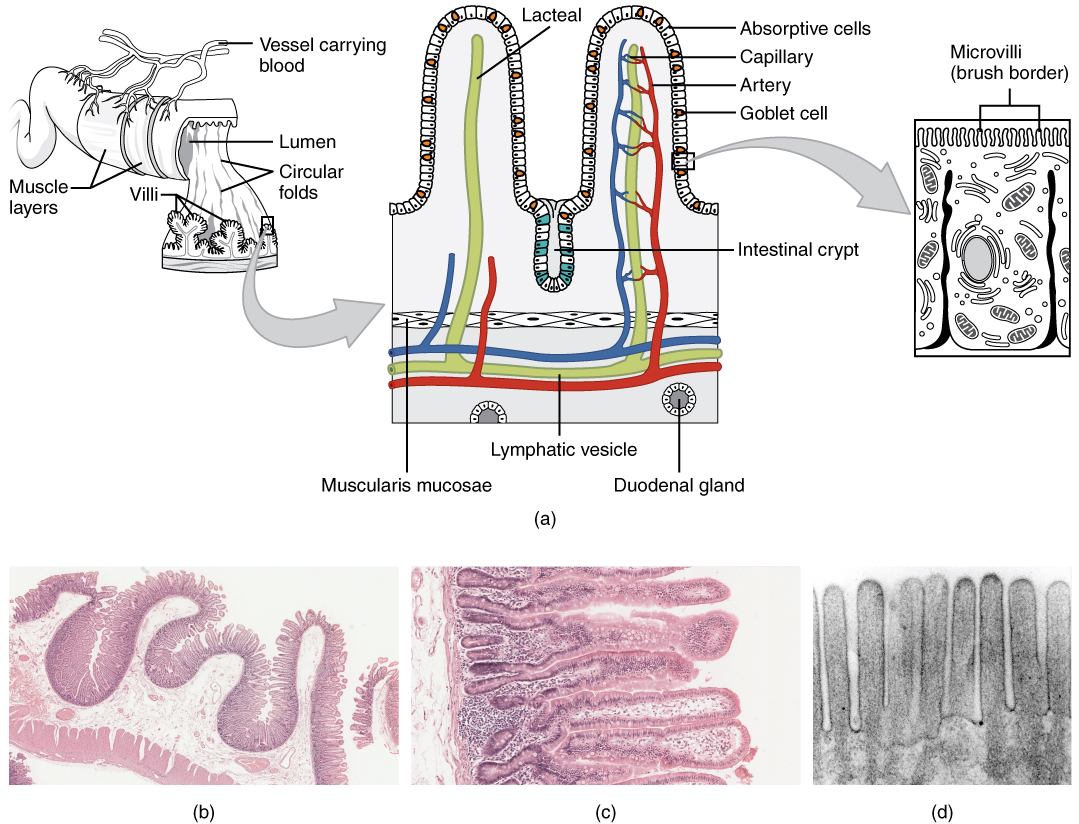
The small intestine is perfectly structured for maximizing nutrient absorption. Its surface area is greater than 200 square meters, which is about the size of a tennis court. Each microvilli contains two types of vessels: a capillary containing blood and a lymphatic vessel containing lymph. The digested nutrients pass through the absorptive cells of the intestine via simple diffusion, facilitated diffusion, or active transport (see Table 4.4.1).
Table 4.4.1 Absorptive Processes
| Process | Mechanism | Nutrients |
| Simple Diffusion | Passive: nutrients move across a concentration gradient from a region of higher concentration within the lumen (interior) of the small intestine into the capillaries (or lymphatic vessel in the case of large lipids and fat-soluble vitamins) of the villi which have a lower concentration of the nutrient | Water; lipids; fat-soluble vitamins |
| Facilitated Diffusion | Passive: nutrients require a protein “carrier” to move across a concentration gradient from higher to lower concentration | Fructose; water-soluble vitamins |
| Active Transport | Active: requires both a protein carrier and energy in the form of ATP which can move nutrients against a concentration gradient from a region of lower concentration to higher concentration | Glucose; some amino acids, di- and tripeptides |
Digested nutrients are absorbed into either capillaries or lymphatic vessels contained within each microvilli, depending on their size. Amino acids, monosaccharides (glucose, fructose, galactose), water-soluble vitamins, and minerals are transported from the intestinal cells into the blood in capillaries, but the much larger emulsified fatty acids, and fat-soluble vitamins are transported first through lymphatic vessels (lacteals), which soon meet up with blood vessels.
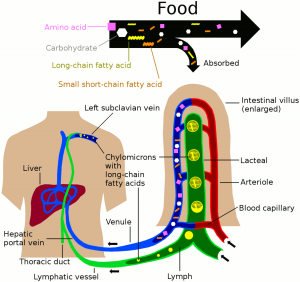
Nutrient Distribution
When the digestive system has broken down food to its nutrient components the body eagerly awaits delivery. The first stop of most absorbed nutrients is the liver. One of the liver’s primary functions is to regulate metabolic homeostasis. Metabolic homeostasis is when the nutrients consumed and absorbed match the energy required to carry out life’s biological processes. Simply put, nutrient energy intake equals energy output. If this homeostasis is disturbed by disordered eating or disease, bodily functions suffer.
Through the body’s network of blood vessels, glucose, amino acids, minerals, and water-soluble vitamins are directly transported from the small intestine to the liver via the hepatic portal vein. Lipids are transported to the liver by a more circuitous route involving the lymphatic system, which contains vessels similar to the circulatory system that transport white blood cells called lymph. The liver is the checkpoint for metabolic activity, and serves as the sorting site for nutrients. From the liver, nutrients travel upward through the inferior vena cava blood vessel to the heart. The heart forcefully pumps the nutrient-rich blood first to the lungs to pick up some oxygen and then to all other cells in the body. Arteries become smaller and smaller on their way to cells, so that by the time blood reaches a cell, the artery’s diameter is extremely small and the vessel is now called a capillary. The reduced diameter of the blood vessel substantially slows the speed of blood flow. This dramatic reduction in blood flow gives cells time to harvest the nutrients in blood and exchange metabolic wastes.
The liver is the only organ in the human body that is capable of exporting nutrients for energy production to other tissues. Therefore, when a person is in between meals (fasted state) the liver exports nutrients and when a person has just eaten (fed state) the liver stores nutrients. Nutrient levels and the hormones that respond to their levels in the blood provide the input so that the liver can distinguish between the fasted and fed states and distribute nutrients appropriately.
4.5 Digestive Disorders That Can Compromise Health
When nutrients and energy are in short supply, cells, tissues, organs, and organ systems do not function properly. Unbalanced diets can cause diseases and, conversely, certain illnesses and diseases can cause an inadequate intake and absorption of nutrients, simulating the health consequences of an unbalanced diet. Overeating energy dense foods and nutrient poor foods can lead to obesity and exacerbate the symptoms of gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS). Many diseases and illnesses, such as celiac disease, interfere with the body getting its nutritional requirements. A host of other conditions and illnesses such as stomach ulcers, Crohn’s disease, diverticulitis, and more can also impair the process of digestion and/or negatively affect nutrient balance and decrease overall health.
Gastroesophageal Reflux Disease
Gastroesophageal reflux, also commonly called “heartburn,” occurs when the acidic contents of the stomach leak backward into the esophagus and cause irritation. Gastroesphageal Reflux Disease (GERD) is a chronic, more serious form of gastroesophageal reflux. This reflux occurs when the lower esophageal sphincter is weakened or relaxes when it should not. Risk factors include increased pressure on your abdomen from excess weight or pregnancy, certain medications, and smoking. GERD is estimated to affect approximately 20% of the US population.
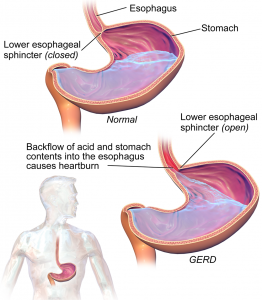
The main symptom is the painful burning sensation in the middle of the chest at the lower esophageal sphincter. Because of the location it is called “heartburn,” although the heart is not involved. Other symptoms include nausea, problems swallowing, and bad breath. More serious consequences of GERD include scarring or stricture of the esophagus, and Barrett’s esophagus which increases risk of esophageal cancer.
GERD is often diagnosed by a history of the frequency of recurring symptoms. A more precise diagnosis requires an upper endoscopy. This procedure involves a gastroenterologist inserting a long, flexible tube with a camera at the end into the mouth and down the upper GI system. Treatment of GERD includes1:
- eating smaller meals
- avoiding spicy foods, chocolate, garlic, fried foods, and tomato based foods
- avoiding alcohol and caffeine
- remaining upright at least 2-3 hours after eating
- losing weight (if overweight or obese)
- avoiding smoke
When lifestyle modifications are not enough, many medications are available to treat GERD, including antacids, histamine-2 blockers, and proton-pump inhibitors. Some evidence from scientific studies indicates that medications used to treat GERD may accentuate certain nutrient deficiencies, namely zinc and magnesium. When these treatment approaches do not work surgery is an option. The most common surgery involves reinforcing the weakened lower esophageal sphincter between the stomach and esophagus.
Gastrointestinal Ulcers
Gastrointestinal ulcers are sores that occur in the lining of the GI tract. These are most common in the lining of the stomach (peptic or gastric ulcer), although they can also occur in the duodenum (duodenal) or esophagus (esophageal). Risk factors include chronic use of non-steroidal anti-inflammatory (NSAIDs), corticosteroid use, being female, drinking alcohol, smoking, older age, and infection with Helicobacter pylori (H. pylori) bacteria.
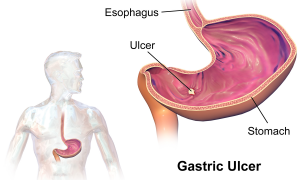
Symptoms include a dull or burning pain in your stomach that lasts for minutes to hours that comes and goes for several days or weeks, bloating, burping, nausea, vomiting, poor appetite, and/or weight loss. Diagnosis of H. pylori is often made via stool testing. However, the most common test to diagnose peptic ulcers is an upper endoscopy. Several medications can be used to treat a peptic ulcer including histamine-2 blockers and proton-pump inhibitors that are also used in GERD. Antibiotics are necessary in the case of peptic ulcer caused by H. pylori.2
Hurry, Curry, and Worry: The Story of H. pylori.
The cure for gastrointestinal ulcers took some time for scientists to figure out. If your grandfather complained to his doctor of symptoms of peptic ulcer, he was probably told to avoid spicy foods, alcohol, and coffee, and to manage his stress. In the early 20th century, the medical community thought peptic ulcers were caused by what you ate and drank, and by stress. In 1915, Dr. Bertram W. Sippy devised the “Sippy diet” for treating peptic ulcers. Dr. Sippy advised patients to drink small amounts of cream and milk every hour in order to neutralize stomach acid. And then, increasingly, introduce soft bland foods with frequent meal times. For a while this diet sometimes worked, fooling both doctors and patients. However, the disappearance of peptic ulcer symptoms was likely the result of having a full stomach all the time, as the symptoms more often occur when the stomach is empty. Ultimately, the Sippy diet did not cure peptic ulcers and in the latter 1960s scientists discovered the diet was associated with a significant increase in heart disease due to its high saturated fat content.
In the 1980s, Australian physicians Barry Marshall and Robin Warren proposed a radical hypothesis—that the cause of ulcers was bacteria that could survive in the acidic environment of the stomach and small intestine. They met with significant opposition to their hypothesis but they persisted with their research. Their research led to an understanding that the spiral shape of the bacterium H. pylori allows it to penetrate the stomach’s mucus lining, where it secretes an enzyme that generates substances to neutralize the stomach’s acidity. This weakens the stomach’s protective mucus, making the tissue more susceptible to the damaging effects of acid, leading to the development of sores and ulcers. H. pylori also prompts the stomach to produce even more acid, further damaging the stomach lining. Marshall actually drank a dish of H. pylori hoping to give himself an ulcer to prove his point. A few days later he was vomiting and had inflamed tissue in his stomach. The presence of H. pylori was confirmed. He then took an antibiotic and the symptoms of H. pylori infection dissipated. Experimental success? It still took years for the medical community to be entirely convinced of the link between peptic ulcers and H. pylori.3
In 1994, the National Institutes of Health held a conference on the cause of peptic ulcers. There was scientific consensus that H. pylori causes most peptic ulcers and that patients should be treated with antibiotics. In 1996, the FDA approved the first antibiotic that could be used to treat patients with peptic ulcers. Nevertheless, the link between H. pylori and peptic ulcers was not sufficiently communicated to healthcare providers. In fact, 75% of patients with peptic ulcers in the late 1990s were still being prescribed antacid medications and advised to change their diet and reduce their stress. In 1997, the Centers for Disease Control and Prevention (CDC), alongside other public health organizations, began an intensive educational campaign to convince the public and healthcare providers that peptic ulcers are a curable condition requiring treatment with antibiotics. Today, if you go to your primary physician you will be given the option of taking an antibiotic to eradicate H. pylori from your gut. Scientists have progressed even further and mapped the entire genome of H. pylori, which will hopefully aid in the discovery of even better drugs to treat peptic ulcers.
The H. pylori discovery was made relatively recently, through the use of the scientific method, overturning a theory applied in our own time. The demystification of disease requires the continuous forward march of science, overturning old, traditional theories and discovering new, more effective ways to treat disease and promote health. In 2005, Marshall and Warren were awarded the prestigious Nobel Prize in medicine for their discovery that many stomach ulcers are caused by H. pylori—not by hurry, curry, and worry.4
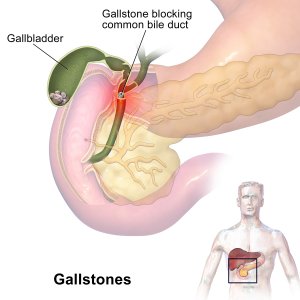
Gallstones
Gallstones are hard, pebble-like substances often made of cholesterol or bilirubin that form in the gallbladder. They can range in size from a grain of sand to a golf ball. The gallbladder can make one or several stones of varying sizes.

People can have one or more gallstones without realizing it as they are painless and do not require medical treatment. That is unless a gallstone blocks the bile duct, causing sudden pain in the upper right of the abdomen. Risk factors for developing gallstones include being female, older age, family history, other medical conditions (liver cirrhosis, Crohn’s disease, elevated triglyceride levels), obesity, losing weight rapidly, and/or a diet high in refined carbohydrates and low in fiber. Gallstones affect approximately 10-15% of the US population. Nearly 250,000 people require surgical intervention annually.
As stated previously, gallstones do not cause symptoms until a stone blocks the duct. In addition to sharp pain in the upper right of the abdomen, one may experience nausea, vomiting, or jaundice (yellowing of the eyes or skin). Diagnosis can be made via blood lab tests, ultrasound or other imaging tests. Treatment consists of surgery to remove the gallbladder. This is one of the most common surgical procedures performed on adults in the US. The gallbladder is not an essential organ. As an accessory organ of digestion, it stores bile that is created by the liver. Once the gallbladder is removed, the liver can take over this role. However, a low fat diet is recommended for the first few weeks post gallbladder removal.5
Diarrhea and Constipation
Both diarrhea and constipation can occur if the normal function and rhythm of the GI tract is disrupted. If waste matter moves too quickly through the large intestine, not enough water is absorbed resulting in loose, watery stools more than three times per day are characteristics of diarrhea. Acute diarrhea is most commonly caused by ingesting food or water contaminated with bacteria (e.g., E. coli, Salmonella), viruses (e.g., norovirus, rotavirus), or parasites (e.g., Cryptosporidium enteritis, Giardia lambdia). Persistent or chronic diarrhea can be caused by dietary allergies and intolerances, or other GI tract conditions such as irritable bowel syndrome or Crohn’s disease. Complications of diarrhea include dehydration and malabsorption of nutrients.6
On the other end of the spectrum is constipation, characterized by infrequent bowel movements (less than 3 times per week) with stools that are hard, dry, or lumpy, and often painful to pass. Sometimes constipation is caused by holding stool and delaying defecation. That gives the colon and rectum additional time to absorb water, making the feces too hard and dry. Delaying defecation is common in children or others who may fear that it will hurt to pass a stool, but of course, holding it only worsens the problem. Constipation can also occur due to other disruptions in daily rhythms, such as changing what or how much you eat, travel, or certain medications. Constipation is common in pregnancy due to hormonal changes. It also becomes more common with age, which may be due to decreased physical activity, medication use, or weakness of the smooth muscle of the intestine. Constipation can be a sign of other medical problems, so chronic constipation should be checked out by a doctor.7
Constipation can often be addressed by dietary changes, including eating more high fiber foods (whole grains, legumes, fruits, vegetables, nuts, etc.) and drinking more water. It can also be helpful to attempt a bowel movement after meals, when the intestine is more active, and to make that a habit to try to establish more regularity. A caffeinated beverage with breakfast can help, as can increasing physical activity. Fiber supplements can be helpful for increasing fiber intake and addressing constipation, at least in the short term. However, it is preferable to transition to dietary sources of fiber as they come packaged with many other valuable nutrients.7
Laxatives may also be helpful to address constipation in the short term but are usually not a good long term solution. It is possible to become dependent on some types of laxatives for bowel movements, meaning that the colon does not contract normally on its own. In these cases, a doctor can help make a plan to gradually reduce laxative use and find other ways to improve bowel regularity.7
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is characterized by muscle spasms in the colon that result in abdominal pain, bloating, constipation, and/or diarrhea. Interestingly, IBS produces no permanent structural damage to the large intestine which makes it difficult to diagnose. Two primary factors that contribute to IBS are diet and stress. It is estimated that 1 in 5 Americans displays symptoms of IBS. The disorder is more prevalent in women than men.
Symptoms of IBS significantly decrease a person’s quality of life as they are present for at least 12 consecutive or nonconsecutive weeks in a year. Large meals and foods high in fat and added sugars, or those that contain wheat, rye, barley, peppermint, and/or chocolate often intensify or bring about symptoms of IBS. Additionally, beverages containing caffeine or alcohol often worsen IBS.
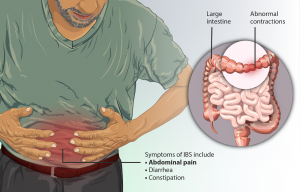
There is no specific test to diagnose IBS, but other conditions that have similar symptoms (such as celiac disease) must be ruled out. This involves stool tests, blood tests, and having a colonoscopy, which involves a gastroenterologist inserting a long flexible tube with a camera on the end through the anus to see the colon tissues.
As with GERD, the first treatment approaches for IBS are diet and lifestyle modifications. People with IBS are often told to keep a daily food journal to help identify and eliminate the food(s) that cause(s) the most problems. Other recommendations are to eat slower, add more fiber to the diet, drink more water, and to exercise. There are also over-the-counter and prescription medications available to treat IBS and the resulting diarrhea or constipation.
Celiac Disease
Celiac disease is an autoimmune disorder caused by an abnormal immune reaction of small intestine cells to a type of protein, called gluten. Gluten forms in the presence of water and is composed of two protein parts, glutenin and gliadin. Glutenin and gliadin are found in grains that are commonly used to make bread such as wheat, rye, and barley.
Celiac disease is most common in people of European descent and is rare in people of African, Japanese, and/or Chinese descent. It is much more prevalent in women and in people with type 1 diabetes, autoimmune thyroid disease (Hashimoto’s disease), and Down or Turner syndromes. It affects between 0.5-1.0% Americans or 1 in every 100 to 200 people.
Symptoms include abdominal pain, weight loss and, in children, a failure to grow and thrive. The symptoms can appear in infancy or much later in life, even by age seventy. Celiac disease is not always diagnosed because the symptoms may be mild.
Diagnosis requires a blood test and a biopsy of the small intestine. Because celiac disease is an autoimmune disease, antibodies produced by white blood cells circulate in the body and can be detected in the blood. When gluten-containing foods are consumed the antibodies attack cells lining the small intestine leading to a destruction of the small villi projections. This tissue damage can be detected with a biopsy, a procedure that removes a portion of tissue from the damaged organ. Villi destruction is what causes many of the symptoms of celiac disease. The destruction of the absorptive surface of the small intestine also results in the malabsorption of nutrients, so that while people with this disease may eat enough, nutrients do not make it to the bloodstream because absorption is reduced. The effects of nutrient malabsorption are most apparent in children and the elderly as they are especially susceptible to nutrient deficiencies. Over time these nutrient deficiencies can cause health problems like anemia and osteoporosis.
Treatment requires following a gluten free diet for life. Many foods like fruits, vegetables, meat, and dairy are naturally gluten free. However, grains like wheat, rye, and barley are not and gluten is often added to processed foods. This condition requires some detective work to seek out foods with hidden gluten, but many stores carry gluten free foods. Corn, millet, buckwheat and oats do not contain the proteins that make gluten, however, there is the potential for cross-contamination of grains during harvest, storage, packing, and processing. After eliminating gluten from the diet, the tissues of the small intestine rapidly repair themselves and should heal in less than six months.
Irritable Bowel Diseases
Unlike IBS, irritable bowel diseases (IBD) are characterized by chronic inflammation of the GI tract that results in damage to the GI tract and increases one’s risk of colon cancer.
Crohn’s Disease
Crohn’s is a chronic disease that causes inflammation and irritation anywhere in the GI tract, although it most commonly affects the small and large intestines. Crohn’s disease is most commonly diagnosed in people aged 20 to 29, smokers, and those with a family member with IBD. It is estimated that more than half a million people in the US have Crohn’s disease.
Symptoms include diarrhea, cramping and abdominal pain, weight loss, anemia, fatigue, and joint pain. Crohn’s disease often begins gradually and worsens over time. However, periods of remission (when symptoms disappear) can last for weeks or months at a time. Blood tests, endoscopy and/or colonoscopy are the most common tools for diagnosis. There are numerous types of medications used to treat Crohn’s disease. During severe episodes (or flare ups), bowel rest may be required, which often consists of intravenous (IV) nutrition. Even with medications, many people with Crohn’s may require surgical intervention such as removal of parts of the small or large intestine, a process called resection.8
Ulcerative Colitis
Ulcerative colitis, another form of IBD, causes irritation, inflammation, and ulcers in the lining of the large intestine. Ulcerative colitis can occur at any age but is more common in those aged 15 to 30 or older than 60, those with a family member with IBD, and those of Jewish descent.
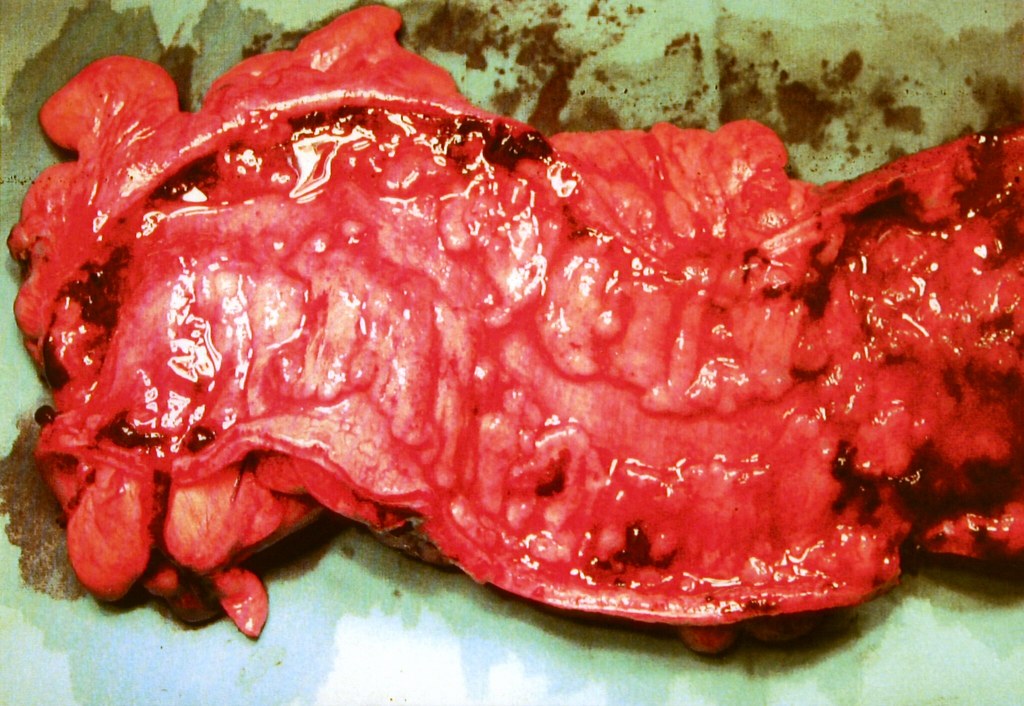
Symptoms include diarrhea with blood or pus, abdominal pain, fatigue, nausea, loss of appetite, weight loss, and anemia. Additional symptoms include irritated and red eyes, fever, mouth ulcers, recurring diarrhea, rectal bleeding or mucus, and painful or swollen joints and skin. Like Crohn’s disease, ulcerative colitis often begins gradually and worsens over time. Periods of remission are also common. Diagnosis typically requires a colonoscopy. There are several medications that can be used to treat ulcerative colitis. And similar to Crohn’s, surgery may also be required.9
Diverticular Disease
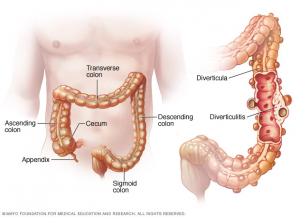
Diverticulosis occurs when small pouches push outward through weak spots in the colon, most commonly in the sigmoid colon. Most people with diverticulosis are unaware they have it and do not experience any symptoms. Diverticulitis occurs when one or more of these pouches becomes inflamed and/or infected. Diverticulitis can be incredibly painful. Risk factors include use of certain medications (such as NSAIDs), physical inactivity, obesity, smoking, genetic predisposition, and older age. Approximately 35% of US adults younger than 50 have diverticulosis, while approximately 58% of US adults older than 60 have diverticulosis. It is thought that approximately 20% of those with diverticulosis will experience diverticulitis at some point in their lives.
Symptoms of diverticulitis can include pain in the lower left side of the abdomen, constipation or diarrhea, fever, nausea, vomiting, and blood in stool. Diagnosis most commonly occurs via colonoscopy. Treatment includes increasing fiber, use of prescription medicine, and probiotics. More severe cases of diverticulitis may require surgical resection of the colon to remove the affected part of the colon.10
Hemorrhoids
Hemorrhoids are swollen, inflamed veins around the anus or in the lower rectum. Risk factors for hemorrhoids include straining during bowel movements, sitting on the toilet for long periods of time, chronic constipation or diarrhea, a low fiber diet, pregnancy, and/or lifting heavy objects. Approximately 1 in 20 US adults has hemorrhoids, with men and women being affected equally. Nearly half of those older than 50 have hemorrhoids.
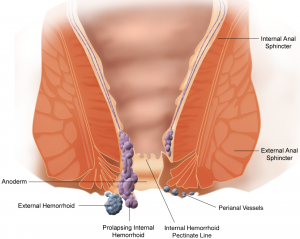
Symptoms include anal itching, hard or tender lumps near your anus, anal pain (especially when sitting), and possibly bright red blood spots in the toilet after bowel movement. Complications include blood clots within a hemorrhoid, or a strangulated hemorrhoid (where blood flow to it is cut off). Treatment includes eating a high fiber diet, taking a stool softener, drinking more water, and over-the-counter medications. However, if symptoms have not improved within a week or have worsened, you should see a physician.11
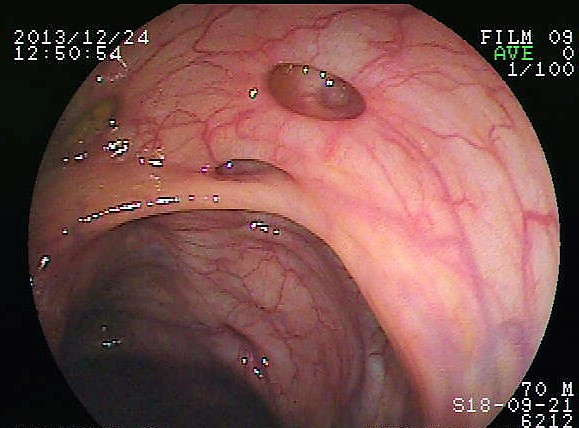
Colorectal Cancer
Colorectal cancer often begins as a growth, called a polyp, on the inner lining of the colon or rectum. Sometimes these polyps are benign or harmless, while others can turn into cancer and grow into the wall of the colon. Risk factors include:
- being overweight or obese
- being physically inactive
- consuming a diet high in red and/or processed meats
- smoking
- alcohol use
- being 50 or older
- having IBD
- a family history of colorectal cancer
In the US, colorectal cancer is the third leading cause of cancer-related deaths in men and in women. Lifetime risk of developing colorectal cancer is approximately 1 in 23 for men and 1 in 25 for women.
There are often minimal to no symptoms of colorectal cancer, particularly in the early stages, however, some symptoms may include diarrhea, constipation, rectal bleeding with bright red blood, abdominal pain, weakness, fatigue, and/or unintended weight loss. It is recommended that adults with average risk of developing colorectal start screening at 45 years old. Colorectal cancer is primarily diagnosed via colonoscopy. These are important as polyps can be removed during the colonoscopy before they have a chance to become cancerous. Treatment for colorectal cancer includes chemotherapy, radiation, surgery, and/or immunotherapy medications.12
Key Takeaways
- The cell is the basic structural and functional unit of life. Cells are independent, single-celled organisms that take in nutrients, excrete wastes, detect and respond to their environment, move, breathe, grow, and reproduce.
- There are 11 organ systems in the human body that work together to support life; all of which require nutrients.
- The breakdown of complex macromolecules in foods to simple absorbable components is accomplished by the digestive system. These components are processed by cells throughout the body into energy or are used as building blocks.
- The digestive system is composed of the mouth, pharynx, esophagus, stomach, small intestine, large intestine (or colon), rectum, and anus. There are four steps in the digestion process: ingestion, the mechanical and chemical breakdown of food, nutrient absorption, and elimination of indigestible food.
- The digestive system also has accessory organs that provide secretions such as enzymes, hydrochloric acid, bile, saliva, and hormones to aid the digestive process.
- The mechanical breakdown of food occurs via muscular contractions called peristalsis and segmentation. Enzymes secreted by the salivary glands, stomach, pancreas, and small intestine accomplish the chemical breakdown of food. Additionally, bile emulsifies fats.
- Four sphincters help to control the flow of food through the digestive tract.
- After digestion, nutrients are absorbed into the circulatory or lymphatic system via three processes: simple diffusion, facilitated diffusion, or active transport.
- After digestion, nutrients are taken to the liver where they are sorted and stored or sent back into circulation to body cells for their use.
- Other important body systems for nutrient distribution include circulatory, nervous, endocrine.
- Several digestive disorders can compromise health including gastroesophageal reflux disease (GERD), ulcers, gallstones, diarrhea, constipation, irritable bowel syndrome (IBS), celiac disease, irritable bowel diseases (IBD) like Crohn’s disease and ulcerative colitis, diverticular disease, hemorrhoids, and colorectal cancer.
Portions of this chapter were taken from OER Sources listed below:
Callahan, A., Leonard, H., Powell, T. (2020). Nutrition: Science and Everyday Application. https://openoregon.pressbooks.pub/nutritionscience
Tharalson, J. (2019). Nutri300:Nutrition. https://med.libretexts.org/Courses/Sacremento_City_College/SSC%3A_Nutri_300_(Tharalson)
Titchenal, A., Calabrese, A., Gibby, C., Revilla, M.K.F., & Meinke, W. (2018). Human Nutrition. University of Hawai’i at Manoa Food Science and Human Nutrition Program Open Textbook. https://pressbooks.oer.hawaii.edu
Zimmerman, M., & Snow, B. (2012). An Introduction to Nutrition, v. 1.0. https://2012books.lardbucket.org/books/an-introduction-to-nutrition/
Additional References:
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Acid reflux (GER & GERD) in adults. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Peptic ulcers (stomach ulcers). National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers
- Kyle, R. A., Steensma, D. P., & Shampo, M. A. (2016). Barry James Marshall – Discovery of Helicobacter pylori as a cause of peptic ulcer. Mayo Clinic Proceedings, 91(5), e67-e68. https://doi.org/10.1016/j.mayocp.2016.01.025
- Konturek, S. J., Konturek, P. C., Konturek, J. W., Plonka, M., Czesnikiewicz-Guzik, M., Brzozowski, T., & Bielanski, W. (2006). Helicobacter pylori and its involvement in gastritis and peptic ulcer formation. Journal of Physiology and Pharmacology: An Official Journal of the Polish Physiological Society, 57(Suppl 3), 29-50.
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Gallstones. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/gallstones
- National Institutes of Diabetes and Digestive and Kidney Diseases (n.d.). Diarrhea. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea
- National Institutes of Diabetes and Digestive and Kidney Diseases (n.d.). Constipation. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/constipation
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Crohn’s disease. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Ulcerative colitis. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Diverticular disease. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis
- National Institutes of Diabetes and Digestive and Kidney Diseases. (n.d.). Hemorrhoids. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids
- American Cancer Society. (2018, February 21). What is colorectal cancer? https://www.cancer.org/cancer/colon-rectal-cancer/about/what-is-colorectal-cancer.html
Media Attributions
- B5A34C84-DB15-46BE-AE3E-5A8F905BB87F
- 5F842728-B086-4FC5-916C-4F32369C6592-300×225-1
- Mineral Classification
a charged atom
term used in chemistry to denote that a molecule contains the carbon atom
chemical energy obtained from the breakdown of food molecules and released to fuel cellular processes
breakdown of molecules into smaller units
The process of chemically splitting macromolecules by the addition of water. It is used in many places in the body, including digestion where large carbohydrates, lipids, and proteins are split into smaller molecules.
Process of combining molecules by removing a water molecule. This occurs in many instances in the body including the building of macromolecules such as glycogen, storage fat, and protein.
hormone released by fat cells; signals to the hypothalamus that eating is not required, often called the satiety hormone; helps regulate long term food intake
muscular rings separating digestive organs that open and close to allow food to move through the digestive tract in a more orderly fashion
Digestive organs that add secretions to the process of digestion, but the food itself does not enter these organs.
food that has been partially broken down that leaves the mouth and enters the pharynx and esophagus - the amount you swallow each time
Anatomical description of the throat area containing the epiglottis and opening of the trachea
Tube that carries air from the mouth and nose into the lungs
muscular digestive tube that connects the mouth to the stomach
Small flap that covers the entrance of the trachea when you swallow to stop the bolus of food from entering the trachea instead of the esophagus
muscle contractions of the digestive tract, squeezing from top to bottom
muscular contractions of the digestive tract squeezing from the sides
sphincter between the esophagus and the stomach
partially digested food that is a semiliquid mass that leaves the stomach about a tablespoon at a time and enters the duodenum of the small intestine
sphincter between the stomach and the small intestine
Substance made in the liver, stored in the gallbladder. It emulsifies fats, allowing them to mix more readily with water-based enzymes for digestion
finger-like projections that line the small intestine
very small finger-like projections on the tips of the villi of the small intestine
State where nutrients absorbed match energy required to carry out biological processes
blood vessels that carry blood away from the heart and to the lungs for gas exchange and to the body cells to deliver oxygen and nutrients and to pick up wastes
tiniest blood vessels
