Chapter 8: Alcohol
“It is the wine that leads me on, the wild wine that sets the wisest man to sing at the top of his lungs, laugh like a fool – it drives the man to dancing. . .it even tempts him to blurt out stories better never told.”
-Homer, The Odyssey
Alcohol is both a beverage providing some sustenance and a drug. For thousands of years, alcohol has been consumed in a medicinal, celebratory, and ritualistic manner. It is drunk in just about every country and often in excessive amounts. In this chapter we will discuss how alcohol is absorbed and metabolized, and how alcohol and health are related.
Learning Objectives
- Discuss how alcohol is made and consumed.
- Describe the absorption and metabolism of alcohol in the body.
- List the symptoms of intoxication and how blood alcohol content can be influenced.
- Describe the health consequences of alcohol use and abuse.
- List symptoms of Alcohol Use Disorder.
8.1 Alcohol Consumption, Absorption, and Metabolism
Alcohol can be made from a variety of different starchy foods through a process called fermentation. Fermentation of a starchy food such as barley or wheat can produce ethanol and carbon dioxide (CO2) which makes up what is commonly known as beer. Fermentation of fruit produces wine. Liquor is produced through a process called distilling which takes fermented plants (usually fruit or grains) and heats them so that the alcohol is distributed as a gas (spirit). This gas is collected, cooled, and condensed back into a liquid. Then water is added, and the liquor is stored for various amounts of time. Common distilled spirits include rum, gin, whiskey, brandy, tequila, and vodka.1
Alcohol is a legal, controlled, psychoactive drug. A psychoactive drug is any substance that crosses the blood-brain barrier primarily affecting the functioning of the brain, be it altering mood, thinking, memory, motor control, or behavior. Alcohols in chemistry refer to a group of similar organic compounds, but in beverages the only alcohol consumed is ethanol.
Research suggests that more than half of the adult US population drank alcohol in the past thirty days, and 25% of adults over 18 reported at least one heavy drinking day (more than 4 drinks) in the past year. Of the total population who drank alcohol, approximately 5% drank heavily (15 or more drinks per average week for men, 8 or more for women), while 15% participated in binge drinking.2
Binge drinking occurs when men consume 5 or more drinks, and when women consume 4 or more drinks within 2-3 hours. According to the Centers for Disease Control and Prevention (CDC), “it is the most common, costly, and deadly pattern of excessive alcohol use in the United States.”4 In the US, 1 in 6 adults binge drink 4 times per month, drinking 7 drinks per binge. Men are twice as likely to binge drink as women. Those under 21 years of age report that when they drink alcohol, it is a binge.3 In 2010, binge drinking cost the US economy $249 billion—about $2.00 per drink. About 40% of those dollars are paid by federal, state, and local governments, costing each taxpayer between $592 and $1526 per year.4
Underage drinking is also a public health problem in the US. Alcohol is the most commonly used and abused drug by youth, contributing to 4,300 deaths per year. In 2017, the Youth Behavior Risk Survey reported that among high school students in the last 30 days, 30% had consumed some alcohol, 14% binge drank, 6% drove after drinking alcohol, and 17% rode with a driver who had been drinking alcohol. Other national surveys show similar results. Consequences of underage drinking include problems in school and home life, increased risk of suicide, sexual assault, unprotected sexual activity leading to unplanned pregnancy, and long-term issues such as memory problems, and reduction in growth and development.5 Adults who first used alcohol before they turned 15 are 7 times more likely to develop alcoholism than adults who first used alcohol at the age of 21. Additionally, 40% of all drug-related emergency room visits of people under age 20 were caused by alcohol abuse.6
Alcohol Absorption
As a person starts drinking alcohol, up to 5% of the ingested ethanol is directly absorbed and metabolized by some cells of the gastrointestinal tract (the mouth, tongue, esophagus). About 20% of alcohol is absorbed into the blood from the stomach, the remaining 75-80% is absorbed through the small intestine.
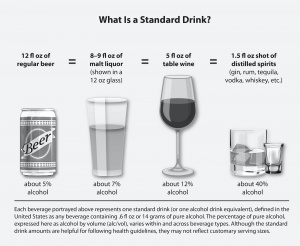
Blood alcohol concentration (BAC) is measured in milligrams percent (mg%) comparing units of alcohol to units of blood and is the most accurate measure of alcohol in the body. BAC is a measurement used legally to assess intoxication and the impairment and ability to perform certain activities, such as driving a car. Once absorbed, more than 90% of ingested alcohol is metabolized in the liver. As a general rule, the liver can metabolize one standard drink (defined as 12 oz of beer, 5 oz of wine, or 1.5 oz of hard liquor) per hour. Drinking more than this, or more quickly, will cause BAC to rise to potentially unsafe levels. Intoxication results when the level of alcohol in the blood exceeds the rate at which the liver can metabolize it. While awaiting metabolism by the liver, the remaining alcohol stays in the blood and is eventually excreted through the breath, urine, saliva, and sweat. Alcohol is a volatile (flammable) organic substance and can be converted to a gas. The lungs exhale alcohol as a gas. The more alcohol consumed, the stronger the smell of alcohol in a person’s breath. Breathalyzer tests measure the exhaled alcohol levels in the lungs to determine the state of inebriation.
Table 8.1.1 Mental and Physical Effects of Different BAC Levels7
| BAC | Effects |
| 0.0-0.05% | Begin to perceive some effects like relaxation; mild memory, attention, coordination, and balance impairment; sleepiness can begin |
| 0.06-0.08% | Perceived beneficial effects such as relaxation; increased risk of aggression in some people; speech, memory, attention, and judgment impaired; muscle coordination, reaction time and balance impaired; reduced driving skills |
| 0.09-0.15% | Clear deterioration of reaction time and control; balance and movement increasingly impaired; increased risk of injury to self or others; vomiting can occur |
| 0.16-0.30% | Speech, memory, coordination, reaction time, balance and all driving skills significantly impaired; judgment and decision making dangerously impaired; vomiting and other signs of alcohol poisoning occur; blackouts and/or loss of consciousness common |
| 0.31-0.45% | Loss of consciousness; significant risk of death due to loss of vital functions |
In addition to the one drink per hour guideline, the rate at which an individual’s BAC rises is affected by the following factors:
- Sex (a woman’s BAC will rise more quickly than a man’s)
- Weight (BAC will rise more slowly for heavier people)
- Genetics
- Length of time as a heavy drinker (tolerance)
- Type of alcohol consumed
- Amount of alcohol consumed
- Consumption rate
- Consumption before or after a meal (food in the stomach slows absorption)
- Mixture (carbonated mixers speed absorption)
- Medications may increase the bioavailability of alcohol
Giving the liver enough time to fully metabolize the ingested alcohol is the only effective way to avoid alcohol toxicity. Drinking coffee or taking a shower will not help. The legal limit for intoxication is a BAC of 0.08% in the US. Taking into account the rate at which the liver metabolizes alcohol after drinking stops, and the alcohol excretion rate, it takes at least 5 hours for a legally intoxicated person to achieve sobriety.
Following intoxication, a common occurrence is the development of a “hangover.” Susceptibility to a hangover varies widely, but common symptoms include thirst, tiredness, headache, nausea, altered mood, and impaired cognitive function. Why these symptoms occur is not well understood. However, research suggests the cause could be multi-faceted. Possibilities include changes in production of hormone-like molecules like cytokines that affect levels of inflammation, decline of blood glucose which may contribute to tiredness and changes in mood, and poor sleep patterns may also play a role. If you are feeling the effects of a hangover, and feel the need to take an over-the-counter pain reliever, be cautious. Taking acetaminophen (TylenolTM) could be problematic. Alcohol metabolism activates an enzyme that transforms acetaminophen into a toxic metabolite that causes liver inflammation and damage. Liver damage may not be reversible. Aspirin and ibuprofen (AdvilTM) can increase acid release in the stomach, irritating the stomach lining.8
Alcohol Metabolism
The liver metabolizes 85-98% of the circulatory ethanol. The liver uses two metabolic processes to get rid of this circulating ethanol as quickly and safely as possible.
- Alcohol dehydrogenase system
- Microsomal ethanol oxidizing system (MEOS)
Alcohol Dehydrogenase System
About 80-90% of the total hepatic (liver) ethanol uptake is processed via the alcohol dehydrogenase system. The degradation of ethanol begins in the liver. The enzyme that catalyzes this reaction is called alcohol dehydrogenase. The products from this reaction are acetaldehyde, NADH (a reduced coenzyme that carries electrons from one reaction to another), and a hydrogen (H+) ion. Acetaldehyde is very toxic to the liver and the body’s cells. The moment acetaldehyde is produced, it must be degraded to protect the liver cells. The enzyme that will carry this type of degradation reaction is acetaldehyde dehydrogenase (ALDH). Acetaldehyde dehydrogenase converts acetaldehyde into acetate, a non-toxic molecule. A small amount (up to 10%) of the liver acetaldehyde may accumulate inside the liver cells.
Microsomal Ethanol Oxidizing System (MEOS)
In a moderate drinker, only about 10-20% of the total liver ethanol uptake is processed via the microsomal ethanol oxidizing system (MEOS). During periods of heavy drinking, however, the alcohol dehydrogenase system cannot keep up, and the MEOS system will metabolize most of the excess ethanol ingested. Heavy drinking stimulates the human body to include the MEOS system enzymes in order to clear ethanol faster from the body.
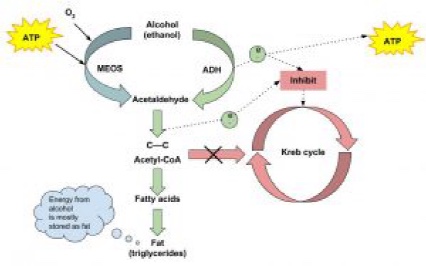
The MEOS system is also located in the liver. Similar to the alcohol dehydrogenase system, acetaldehyde dehydrogenase will immediately convert acetaldehyde into acetate, a non-toxic molecule. Other products from this reaction are NADH and H+ ion.
As more alcohol is ingested, the production of acetaldehyde by both the alcohol dehydrogenase and MEOS systems is stimulated. As the levels of acetaldehyde increase inside the liver cells with heavy consumption of alcohol, some of the acetaldehyde diffuses into the blood circulation. In circulation, high levels of acetaldehyde cause nausea and vomiting. Vomiting causes more body dehydration and loss of electrolytes. If the dehydration becomes severe enough, this can impair brain function and a person may lose consciousness.
Fate of Acetate
The acetate produced (from the alcohol dehydrogenase system and MEOS) is either released into circulation or retained inside the liver cells. In the liver cells, acetate is converted to acetyl CoA where it is used to produce other molecules like CO2 or used in the synthesis of fatty acids and cholesterol.
8.2 Health Consequences of Alcohol Use
Alcohol in excess is detrimental to health; however since its beginnings it has been suspected and promoted as a benefit to the body and mind when consumed in moderation. In the US, the Dietary Guidelines define moderate alcohol intake as no more than one drink per day for women and no more than two drinks per day for men.9 Although drunkenness has pervaded many cultures, drinking in moderation has long been a mantra of multiple cultures with access to alcohol.
Health Consequences of Alcohol Abuse
Excessive alcohol use or recurrent binge drinking can lead to both short term and long term disability and death. Almost 90,000 people had alcohol-related deaths every year between 2006-2010. Incredibly, 1 in 10 adults between ages 20-64 died from excessive alcohol consumption. They died from injuries sustained in motor vehicle crashes, falls, drownings, burns, homicides, suicides, sexual assaults, and alcohol poisoning. Chronic, regular consumption of alcohol can damage almost every organ system in the body.10
Alcohol and the Liver
Alcohol stimulates the release of epinephrine (or adrenaline) from the adrenal glands located on top of the kidneys. Epinephrine binds to receptors in the liver cells to stimulate the release of glucagon from the pancreas. Glucagon and epinephrine stimulate glycogenolysis (breakdown of glycogen to glucose) in the liver cells. Epinephrine also stimulates the breakdown of triglycerides and glycerol into free fatty acids in adipose tissue and are released into the bloodstream and travel to the liver. A portion of these triglycerides are stored in the liver cells; while, the remainder of these triglycerides are converted to very low density lipoprotein (VLDL). The increased accumulation of both stored triglycerides and VLDL particles inside the liver cells causes a condition called fatty liver or hepatic steatosis. This can impair normal liver function. The more alcohol consumed, the more lipids produced and stored inside the liver cells. These effects are cumulative over time.
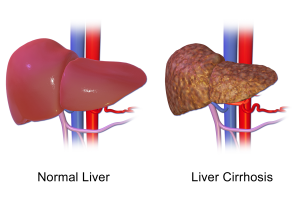
According to the CDC, 22,456 Americans died from alcohol-related liver diseases in 2017, up from about 15,000 in 2007, and there were almost 36,000 total deaths related to alcohol (excluding accidents and homicides).10 Although not every alcoholic or heavy drinker will die from liver problems, the liver is one of the body’s main filtering organs and is severely stressed by alcohol abuse. The term Alcoholic Liver Disease (ALD) is used to describe liver problems linked to excessive alcohol intake. ALD can be progressive, with individuals first suffering from a fatty liver and going on to develop cirrhosis. It is also possible to have different forms of ALD at the same time. Excessive alcohol consumption causes the destruction of liver cells. In an attempt to repair itself, the liver initiates an inflammatory and repair process causing scar tissue to form. In the liver’s attempt to replace the dead cells, surviving liver cells multiply. The result is clusters of newly formed liver cells, also called regenerative nodules, within the scar tissue. This state is called cirrhosis of the liver.11
Non-Alcoholic Fatty Liver Disease (NAFLD) & NASH
In recent years because of the increase in obesity and type 2 diabetes there has been a stark increase in the diagnosis of liver disease that looks similar to that caused by chronic alcohol consumption. However, this damage occurs in people who do not excessively consume alcohol so is called Non-Alcoholic Fatty Liver Disease (NAFLD). Non-Alcoholic Steatohepatitis (NASH) is a subset of NAFLD where the liver becomes inflamed and damaged, with fatty deposits (cirrhosis).12 About 25% of adults have NAFLD making it the most common chronic liver condition in the US. It is estimated that by 2030 NASH will be the most frequent reason for liver transplant.13 Unfortunately most people with this condition do not have any symptoms so diagnosis usually occurs in late stages of the disease. Although the cause is unknown, researchers have identified some conditions that are risk factors. These include being overweight or obese (especially with excess weight at the waist), having insulin resistance, hypercholesterolemia, high triglycerides, hypertension, and/or hyperglycemia. Certain genes may also make you more likely to develop NAFLD, and it is more common in women.12 There is currently no treatment for NAFLD or NASH. You may be able to reverse or slow its progression by losing weight, exercising regularly, eliminating alcohol, reducing intake of refined carbohydrates and added sugars, consuming vitamin E (a powerful antioxidant), and if you’re diabetic, keeping blood glucose tightly controlled.13
Alcohol and the Cardiovascular System
When alcohol is consumed it causes a temporary increase in heart rate, blood pressure, and irregular heartbeats. Chronic consumption can cause these temporary increases to persist, causing hypertension and weakening the heart muscle (cardiomyopathy), leading to heart failure, heart attack, or stroke. Because excessive alcohol intake affects the liver, it can also cause hyperlipidemia and increasing LDL or “bad cholesterol” leading to increased deposits of plaque on the blood vessel walls. This diminishes blood flow to the heart, causing further damage.
Alcohol and the Brain
Alcohol can adversely affect nearly every area of the brain. When BAC rises, the central nervous system is depressed. Alcohol disrupts the way nerve cells communicate with each other by interfering with receptors on certain cells. The immediate impact of alcohol on the brain can be seen in the awkwardly displayed symptoms of confusion, blurred vision, slurred speech, and other signs of intoxication. These symptoms will go away once drinking stops, but abusive alcohol consumption over time can lead to long-lasting damage to the brain and nervous system including dementia, depression, anxiety, learning problems, or other mental health issues.10
Alcohol, Weight, and Nutrition
Alcoholic drinks in excess may contribute to weight gain by substantially increasing caloric intake. Recall that 1 gram of alcohol provides 7 kcal; these are considered “empty calories” because they have no nutritional value. Distilled spirits have exceptionally few nutrients, but some beer and wines do provide a few nutrients (vitamins and/or minerals) and phytochemicals along with calories. A typical beer is 150 kcal, a 5 oz glass of wine contains 90-240 kcal, and an ounce of hard liquor (without mixer) is around 100 kcal. These excess calories are easily stored as body fat, contributing to obesity.
Chronic malnutrition is common among alcoholics. Consuming alcohol may reduce nutrient intake by displacing more nutrient dense foods. Those with severe alcoholism sometimes get 50% or more of their daily caloric intake from alcoholic beverages. Excessive alcohol intake also reduces the secretion of pancreatic juice and damages the lining of the gastrointestinal system, impairing nutrient digestion and absorption. This impaired digestion and absorption of nutrients in alcoholics contributes to their characteristic “skinniness” and multiple associated micronutrient deficiencies. The most common macronutrient deficiency among alcoholics is water, as it is excreted in excess. Commonly associated micronutrient deficiencies include the water-soluble B vitamins (thiamin, niacin, B6, folate) and vitamin C; fat-soluble vitamins (A, D, E, K), and minerals such as magnesium, calcium, selenium, and zinc. These deficiencies can lead to mild to moderate cognitive impairment including problems with memory/learning, spatial skills, and problem solving.14
Other Health Effects of Alcohol Consumption
Alcohol can reduce the effectiveness of your immune system, making you more susceptible to infection. This may also increase your chances of developing cancer, especially of the oral cavity, throat, esophagus, liver, breast, and colon. It can cause inflammation of the stomach (gastritis) or pancreas (pancreatitis), and cause reproductive issues including erectile dysfunction in men.10 Pregnant women should avoid alcohol use. Fetal Alcohol Spectrum Disorders (FASDs) can occur in people whose mother drank alcohol during her pregnancy. These disorders can range in severity, and can include physical, behavioral, or learning difficulties.15

Is Drinking Moderately Beneficial?
Although past studies have hinted that there may be health benefits to moderate alcohol intake (no more than 1 standard drink per day for women and 2 standard drinks per day for men), more recent studies indicate that this may not be true. Improved health outcomes for moderate drinkers may not be related to their alcohol intake at all, instead being attributed to other health behaviors such as not smoking, eating a healthful diet, or exercising regularly.16 It is also clear that excess alcohol consumption is harmful, and some groups including pregnant women, those taking medications that interact with alcohol, and those who are unable to drink in moderation should abstain completely.
Alcohol Addiction
Alcohol is a legal, controlled substance that is a central nervous system depressant, lowering anxiety and inhibitions. Because it is legal and widely accepted, it is sometimes difficult to tell the difference between casual use and abuse. Not everyone who drinks is an alcoholic, but anyone whose life is consistently negatively affected by alcohol is considered to have Alcohol Use Disorder. Some of these negative consequences include physical harm, illness, strained relationships, problems at work or school, and financial difficulty. Alcohol use can become an addiction, called alcoholism.6
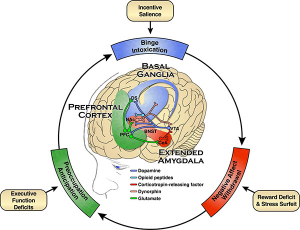
The three stages of Alcohol Use Disorder describe the cycle of alcohol addiction. Many parts of the brain are influenced by alcohol ingestion. During the binge/intoxication stage, neurotransmitters like dopamine are released, affecting the basal ganglia of the brain. This is the reward/pleasure system. The cells in this area help with habit formation. With repeated bouts of alcohol consumption, the cells in this area change and the drinker begins to compulsively seek out alcohol. The drinker also begins to associate drinking with other social stimuli like the presence of others, locations, etc.
Over time, the brain changes and exposure to these stimuli can activate the reward system—even without alcohol. The absence of alcohol stimulates the withdrawal/negative affect stage. There is a decrease of the neurotransmitters that stimulate the reward system, and instead other neurotransmitters are secreted activating stress. This causes increased anxiety and irritability. The third stage, the preoccupation/anticipation stage, is the point at which the drinker will seek out alcohol to combat the negative, stressful effects of the previous stage. The prefrontal cortex of the brain is engaged. This is the area of the brain where executive decisions are made—the “go” or “no-go” systems. An imbalance in these systems can lead to binge drinking and the cycle begins again.17
Do You or Someone You Love have Alcohol Use Disorder?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) provides a list of symptoms of Alcohol Use Disorder. If you recognize any of these symptoms in yourself or in others, alcohol may already be a cause for concern. The more symptoms you have, the more urgent the need for change. Talk to your doctor or other health professional, or even a friend, to help you decide the best course of action.18 Symptoms of Alcohol Use Disorder
Key Takeaways
- Alcohol provides some sustenance but is also a psychoactive drug made from fermentation of plants like grains or fruit.
- More than half of US adults drink alcohol, but there are issues with excess including binge drinking, underage drinking, and driving while intoxicated causing social, physical, and economic hardship to individuals and communities.
- Alcohol is absorbed primarily from the small intestine and travels in the blood until it reaches the liver for metabolism. Some losses occur through breath, urine, saliva, and sweat.
- Blood alcohol content (BAC) rises based on several factors in addition to the amount and rate of alcohol consumed.
- The liver breaks down (metabolizes) alcohol at a rate of about 1 oz per hour through two systems: the alcohol dehydrogenase system which metabolizes 80-90%, and the microsomal ethanol oxidizing system (MEOS) which metabolizes 10-20%.
- Alcohol has negative health consequences on the brain, liver, cardiovascular system, immune system, and gastrointestinal organs.
- NAFLD and NASH are liver disorders that occur in people who do not abuse alcohol, but the liver damage is similar to that caused by chronic alcohol consumption.
- Chronic excessive alcohol consumption can lead to malnutrition.
- The Alcohol Use Disorder cycle describes the brain and body’s adaptations to chronic alcohol use and the development of alcohol addiction.
Portions of this chapter were taken from OER Sources listed below:
Titchenal, A., Calabrese, A., Gibby, C., Revilla, M.K.F., & Meinke, W. (2018). Human Nutrition. University of Hawai’i at Manoa Food Science and Human Nutrition Program Open Textbook. https://pressbooks.oer.hawaii.edu
Additional References:
- Shipman, F. M., & Thomas, A. T. (2020, January 14). Distilled spirit. Encyclopaedia Britannica. https://www.britannica.com/topic/distilled-spirit
- Centers for Disease Control and Prevention. (2017, January 20). Alcohol use. National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/alcohol.htm
- Centers for Disease Control and Prevention. (2019, December 30). Binge drinking. https://www.cdc.gov/alcohol/fact-sheets/binge-drinking.htm
- Centers for Disease Control and Prevention. (2019, December 30). Excessive drinking is draining the U.S. economy. https://www.cdc.gov/alcohol/features/excessive-drinking.html
- Centers for Disease Control and Prevention. (2020, January 3). Underage drinking. https://www.cdc.gov/alcohol/fact-sheets/underage-drinking.htm
- Addiction Center. (2020, June 18). Understanding alcohol. http://addictioncenter.com/alcohol
- Aware Awake Alive. (n.d.) Blood alcohol concentration and calculator. https://awareawakealive.org/educate/blood-alcohol-content
- National Institute of Alcohol Abuse and Alcoholism. (2019, March). Hangovers. National Institutes of Health. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/hangovers
- United States Department of Agriculture and United States Department of Health and Human Services. (2020). Dietary Guidelines for Americans, 2020-2025. (9th ed.). https://www.dietaryguidelines.gov
- Centers for Disease Control and Prevention. (2019, December 30). Alcohol use and your health. https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm
- Osna, N. A., Donohue, T. M., Jr, & Kharbanda, K. K. (2017). Alcoholic liver disease: Pathogenesis and current management. Alcohol Research: Current Reviews, 38(2), 147-161.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2016, November). Symptoms & causes of NAFLD & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/symptoms-causes
- American Liver Foundation. (n.d.). NASH definition & prevalence. https://liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/nonalcoholic-steatohepatitis-information-center/nash-definition-prevalence/
- Ham, B. J., & Choi, I-G. (2005). Psychiatric implications of nutritional deficiencies in alcoholism. Psychiatry Investigation, 2(2), 44-59. https://www.psychiatryinvestigation.org/m/journal/view.php?number=744
- Centers for Disease Control and Prevention. (2020, March 30). Fetal alcohol spectrum disorders (FASDs). https://www.cdc.gov/ncbddd/fasd/
- Centers for Disease Control and Prevention. (2019, December 30). Dietary guidelines for alcohol. https://www.cdc.gov/alcohol/fact-sheets/moderate-drinking.htm
- National Institute of Alcohol Abuse and Alcoholism. (n.d.). NIAAA Strategic Plan 2017-2021. National Institutes of Health. https://www.niaaa.nih.gov/strategic-plan/basic-science
- National Institute of Alcohol Abuse and Alcoholism. (n.d.). Alcohol use disorder. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-use-disorders
any substance that crosses the blood-brain barrier that affects brain function
consuming 5 or more alcoholic drinks per day for men, 4 or more for women
legal measurement used to assess intoxication and the impairment and ability to perform certain activities such as driving a car
When blood alcohol level exceeds the rate at which the liver can metabolize it; leading to physical and mental impairment
Enzyme used to breakdown alcohol (ethanol) in the liver.
fight-or-flight hormone released from the adrenal gland
The breakdown of glycogen to glucose for use as energy
The inability to control drinking due to both a physical and emotional dependence on alcohol.
Characteristics describing the cycle of alcohol addiction: binge/intoxication stage, withdrawal/negative stage, and the preoccupation/anticipation stage.
Stage 1 of Alcohol Use Disorder, alcohol consumption initiates the reward/pleasure system of the brain.
Stage 2 of Alcohol Use Disorder. In this stage the body experiences withdrawal symptoms when alcohol is not consumed.
Stage 3 of Alcohol Use Disorder. The drinker seeks out alcohol to combat the negative and stressful withdrawal, leading to additional and continued consumption of alcohol.
