Chapter 7: Lipids
“The food you eat can be either the safest and most powerful form of medicine or the slowest form of poison.”
-Ann Wigmore, Natural Health Advocate, Founder of the Ann Wigmore Natural Health Institute
Lipids are important macromolecules that serve various roles in the human body including being part of cell membranes and acting as our most abundant source of energy. The term lipid describes a broad group of biomolecules, and fat is one of them. However, in the study of nutrition, the terms lipid and fat are used interchangeably. We also use the term fat to describe both fats in foods and stored fats on the body. Although often maligned, body fat is probably the reason we are all here. Throughout history, there have been many instances when food was scarce. Our ability to store excess caloric energy as fat for future use allowed us to continue as a species during times of famine. So normal fat reserves are a signal that metabolic processes are efficient and a person is healthy. In this chapter we will look at lipid structure, functions, how they are digested and absorbed, and how they relate to overall health.
Learning Objectives
- Explain the structures of lipids (triglycerides, phospholipids, sterols) and how structure impacts its function as it relates to health and disease.
- Compare and contrast the structure of the following types of fats: triglycerides (saturated, monounsaturated, polyunsaturated, omega-3, and omega-6), phospholipids, and sterols.
- Summarize the steps in lipid digestion, absorption, and transport through the body.
- Explain how lipids are used for energy and stored in the body.
- Discuss health issues related to lipids, including risk factors and signs/symptoms.
7.1 Defining Lipids
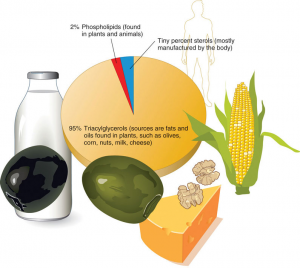
Lipids are a family of organic compounds that are mostly insoluble in water. Composed of fats and oils, lipids are molecules that yield high energy (9 kcal/g) and, like carbohydrates, are composed of carbon, hydrogen, and oxygen. The three main types of lipids are triglycerides (or triacylglycerols), phospholipids, and sterols. Fatty acids are considered “building blocks” and are the main component of triglycerides and phospholipids.
What Are Fatty Acids?
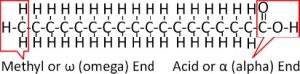
Fatty acids consist of a carboxylic acid (-COOH) group on one end of a carbon chain and a methyl group (-CH3) on the other end. The acid end is called “alpha,” the methyl end is “omega.” Between the ends is a line of carbon atoms which can each make four chemical bonds with other atoms. There are dozens of fatty acids that make up both foods we eat and body tissues. Fatty acids can differ from one another in several ways.
Chain Length
Fatty acids have different chain lengths and compositions. Most fatty acids have a chain length between 4 and 24 carbons and they always contain an even number of carbons in the chain. When the carbon chain length is shorter, the melting point of the fatty acid becomes lower and the fatty acid becomes more liquid. Chain length also affects how a fatty acid is absorbed after digestion. Short chain fatty acids have fewer than 8 carbons in their chain, medium chain fatty acids have 8-12 carbons, and long chain fatty acids have greater than 12 carbons.
Degrees of Saturation
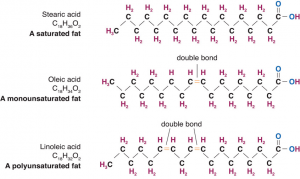
Fatty acid chains are held together by carbon atoms that attach to each other and to hydrogen atoms. The carbon atoms must remain attached to one another. The term saturation refers to whether or not the available carbon atoms that are not attached to other carbons are “filled” (or saturated) to capacity with hydrogen atoms. If each available carbon bond holds a hydrogen atom we call this a saturated fatty acid chain (SFA). All carbon atoms in such a fatty acid chain are bonded with a single bond making them very stable molecules.
Sometimes the chain has a place where hydrogen atoms are missing. When this occurs, the bonds between carbon atoms must double (C=C) to maintain the four bond requirement for carbon atoms. This refers to a point of unsaturation. When one or more bonds between carbon atoms are a double bond, that fatty acid is an unsaturated fatty acid. When a fatty acid has only one double bond it is a monounsaturated fatty acid (MUFA). An example of a food containing MUFA is olive oil (75% of its fat is monounsaturated). These fats help regulate blood cholesterol levels, thereby reducing the risk of heart disease and stroke. A polyunsaturated fatty acid (PUFA) has two or more double bonds (two or more points of unsaturation). Soybean oil contains high amounts of PUFA that provide nutrition that is essential for normal cell development and healthy skin. The more double bonds there are in a fatty acid the less stable it is because the second bond of a double bond will readily break and singly bond with another atom if available.
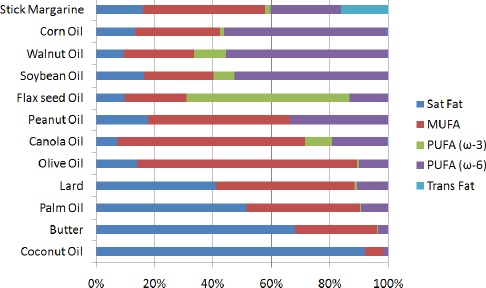
Knowing the connection between chain length, degree of saturation, and the state of the fatty acid (solid or liquid) is important for making food choices. If you decide to limit or redirect your intake of fat products, then choosing those containing high amounts of unsaturated fatty acids is more beneficial than choosing those high in saturated fatty acids. This choice is easy enough to make because unsaturated fats tend to be liquid at room temperature, like olive oil which contains oleic acid, an 18-carbon (18-C) MUFA, whereas saturated fats tend to be solid at room temperature. Examples of fats made up of high levels of saturated fatty acids include butter, the fats found in chocolate, and those in meat (stearic acid, an 18-C SFA is a primary component in meat). Avocados are rich in unsaturated fats. Most vegetables and fish oils contain high quantities of PUFA. Olive and canola oils are also rich in MUFA. Conversely, tropical oils are an exception to this rule in that they are liquid at room temperature yet high in saturated fats. Palm oil (often used in food processing) is highly saturated and has been proven to raise blood cholesterol. Shortening, margarine, and commercially prepared products (in general) report to use only vegetable-derived fats in their processing. But even so, much of the fat they use may be in the saturated and trans fat categories.
Cis or Trans Fatty Acids?
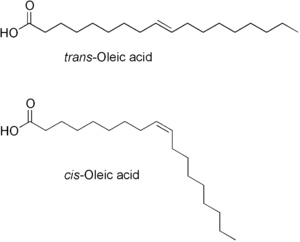
The introduction of a carbon double bond in a carbon chain, as in an unsaturated fatty acid, can result in different structures for the same fatty acid composition. When the hydrogen atoms are bonded to the same side of the carbon chain, it is called a cis fatty acid. Because the hydrogen atoms are on the same side, the carbon chain has a bent structure (Figure 7.1.3). Naturally occurring fatty acids usually have a cis configuration. In a trans fatty acid, the hydrogen atoms are attached on opposite sides of the carbon chain which changes the shape of the fatty acid to be more linear.
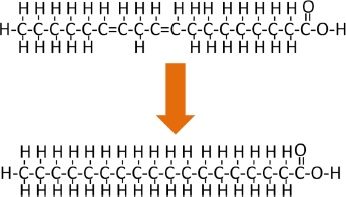
Unlike cis fatty acids, most trans fatty acids are not found naturally in foods, but as a result of a process called hydrogenation. We mentioned above that the second bond of a double bond is not as strong and will singly bond with available atoms. Hydrogenation is the process of adding hydrogen, making the hydrogen atoms available to bond with the second bond of the double bond. This removes double bonds, making the fatty acid more saturated. This hydrogenation process can remove all of the double bonds, or just some of them (partial hydrogenation). To visualize the difference in the amount of hydrogenation consider the difference between tub margarine and stick margarine. Stick margarine is more fully hydrogenated giving it a more solid texture. This is one of the two reasons to hydrogenate, to get a more solid texture. The second reason is that it makes it more shelf stable, because the double bonds of unsaturated fatty acids are susceptible to oxidation, which causes them to become rancid more quickly. More information about trans fats can be found later in this chapter.
Essential Fatty Acids: Omega-3 and Omega-6
Fatty acids are vital for the normal operation of all body systems. The circulatory, respiratory, integumentary, immune systems, brain, and other organs require fatty acids to properly function. The body is adept at synthesizing the majority of required fatty acids from fat, protein, and carbohydrate. However, when we say essential fatty acid we are referring to the two families of fatty acids that the body cannot create on its own, so they must be consumed in the diet, namely, alpha-linolenic acid (omega-3) and linoleic acid (omega-6). The 3 and 6 refer to the position of the first carbon-carbon double bond from the omega (or methyl) end of the fatty acid chain.
- Omega-3 Fatty Acids. At the helm of the omega-3 fatty acid family is alpha-linolenic acid (ALA). From this fatty acid, the body can make eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Alpha-linolenic acid is found in nuts, especially walnuts, flax and chia seeds, hemp, legumes, and vegetable oils such as soybean, canola, and flaxseed. EPA and DHA are found abundantly in marine sources such as cold-water fatty fish (e.g., salmon, herring, albacore tuna, lake trout) and algae. ALA, DHA, and EPA can also be found in dietary supplements. Eating seafood containing DHA/EPA at least once per week has shown to have moderate benefits for heart health, fetal growth and development, and reducing symptoms of rheumatoid arthritis. However, the benefits of dietary supplements are less certain.1 Omega-3 fatty acids may also play important roles in cognition, mood, circulation, and skin.2
- Omega-6 Fatty Acids. At the helm of the omega-6 fatty acid family is linoleic acid. Like ALA, the body uses linoleic acid to make other important substances such as arachidonic acid (ARA) that is used to make eicosanoids. Eicosanoids perform critical roles in the body as they affect a broad spectrum of functions. The word eicosanoid originates from the Greek word eicosa, meaning “twenty,” because this hormone is derived from ARA that is 20 carbon atoms in length. Eicosanoids affect the synthesis of all other body hormones and control all body systems, such as the central nervous system and the immune system. Among the many functions eicosanoids serve in the body, their primary function is to regulate inflammation. Without these hormones the body would not be able to heal wounds, fight infections, or fight off illness each time a foreign germ presented itself. Eicosanoids work together with the body’s immune and inflammation processes to play a major role in several important body functions, such as circulation, respiration, growth and development. Omega-6 fatty acids are found in vegetable oils, nuts, and some animal products.2
Balancing Omega-3 and Omega-6 in the Diet
To achieve optimal health benefits, a proper dietary balance between omega-3 and omega-6 fatty acids must be achieved. As our food choices evolve, the sources of omega-6 fatty acids in our diets are increasing at a much faster rate than sources of omega-3 fatty acids. Omega-3s are plentiful in diets of unprocessed foods where grazing animals and foraging chickens roam free, eating grass, clover, alfalfa, and grass dwelling insects. In contrast, today’s Western diets are bombarded with sources of omega-6. For example, we have oils derived from seeds and nuts and from the meat of animals that are fed grain. Vegetable oils used in fast food preparations, most snack foods, cookies, crackers, and sweet treats are also loaded with omega-6 fatty acids. While we need a small amount of eicosanoids that our body synthesizes from omega-6 fatty acids, too much of these are pro-inflammatory, meaning they promote inflammation, blood clotting, and cell proliferation. In contrast, omega-3 fatty acids are anti-inflammatory.
While omega-6 fatty acids are essential, they can be harmful when they are out of balance with omega-3 fatty acids. Both omega-6 fats and omega-3 fats are required only in small quantities. Researchers believe that when omega-6 fats greatly outnumber omega-3 fats in the diet they diminish the beneficial effects of omega-3 fats. This imbalance may elevate the risks for allergies, arthritis, asthma, coronary heart disease, type 2 diabetes, many types of cancer, autoimmune and neurodegenerative diseases, all of which are believed to originate from some form of inflammation in the body.
What does this mean for you? If your diet is low in omega-3 fats to begin with, then most of your essential fatty acids are from omega-6. Stop and think about your dietary intake. Do not create a pro-inflammatory environment in your body. Attaining proper balance between omega-3 fatty acids and omega-6 fatty acids means learning to make healthy choices, choosing more foods like fatty fish, nuts, and seeds in place of processed, industrialized foods.
Food for Thought
Think about your favorite restaurant and the food you like to order there. What type of fatty acids does a typical meal that you eat there have? Consider the health benefits and possible drawbacks. What foods would you add to enhance your meal? What foods should you consider avoiding?
Types of Lipids
Like amino acids are the building blocks of proteins, fatty acids are the main building blocks of fats. There are three forms of fats in the body: triglycerides, phospholipids, and sterols.
Triglycerides
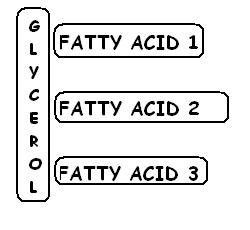
Triglycerides make up 90% of the lipids found in the body and more than 95% of the lipids in the diet. They are commonly found in fried foods, vegetable oil, butter, whole milk, cheese, cream cheese, and some meats. Avocados, olives, corn, and nuts are also sources of naturally occurring triglycerides. The process that forms triglycerides from glycerol and fatty acids is called lipogenesis. To form a triglyceride, a glycerol molecule attaches to three fatty acid chains resembling the capital letter “E.” The fatty acids on each triglyceride can have the same characteristics or each can be different. Remember that fatty acids can differ in their chain length, degree of saturation, and location of their double bonds.
Phospholipids
Phospholipids make up only about 2% of dietary lipids. They are both water-soluble (-phosphate group attached to the glycerol) and insoluble (-two fatty acids) and are found in both plants and animals. Phospholipids are crucial for building the protective barrier, or membrane, around your body’s cells. In fact, phospholipids are synthesized in the body to form cell and organelle membranes. In blood and body fluids, phospholipids form structures, called lipoproteins (to be covered later in the chapter) in which fat is enclosed and transported throughout the bloodstream.
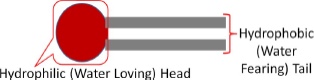
Like triglycerides, phospholipids have a glycerol backbone, but unlike triglycerides, phospholipids are diglycerides (two fatty acids attached to the glycerol head) with a phosphate group coupled with a nitrogen-containing group. As stated previously, phospholipids are unique because they are amphipathic—which means it has one section containing the fatty acids that are hydrophobic (water fearing) and another section, the phosphate group, that is hydrophilic (water loving).
In the body, phospholipids bind together to form cell membranes. The hydrophilic nature of the phosphate group of phospholipids governs their function as components of cell membranes. The phospholipids form a double layer in cell membranes thus effectively protecting the inside of the cell from the outside environment while at the same time allowing for transport of fat and water through the membrane.
Because it is amphipathic, phospholipids are ideal emulsifiers that can keep emulsions like oil and water mixed. Emulsions are mixtures of two liquids that do not want to mix. Without emulsifiers, the fat and water content could separate within food. Lecithin (phosphatidylcholine) found in egg yolk, honey, and mustard, is a popular food emulsifier. The egg yolk in mayonnaise contains lecithin and demonstrates lecithin’s ability to blend vinegar and oil to create this spreadable condiment. Food emulsifiers also play an important role in making the appearance of food appetizing. Adding emulsifiers to sauces and creams not only enhances their appearance but also increases their freshness. In the digestive process, bile secreted from the gallbladder, serves as an emulsifier and aids in lipid digestion.
Sterols
Sterols have a very different structure from triglycerides and phospholipids. Most sterols do not contain any fatty acids but rather are multi-ring structures. They are complex molecules that contain interlinking rings of carbon atoms, with side chains of carbon, hydrogen, and oxygen attached. Cholesterol is the most well known sterol. We consume cholesterol in our diets if we consume animal foods like meat, poultry, fish, eggs, and dairy. Plant foods do not contain cholesterol. However, most of the cholesterol used in the body is actually produced in our liver.
Cholesterol plays some important roles in the body. Like phospholipids, cholesterol is present in all body cells as it is an important substance in cell membrane structure. Approximately 25% of cholesterol in the body is localized in brain tissue. Cholesterol is required for the synthesis of sex hormones (testosterone, estrogen, progesterone), vitamin D, and bile salts. However, cholesterol is often vilified because it is also a component of the plaque that narrows the arteries in atherosclerosis and heart disease. Although cholesterol is found exclusively in animal foods, there are other sterols in other food sources. The sterols found in plants resemble cholesterol in structure. However, plant sterols (also called phytosterols) inhibit cholesterol absorption in the human body, which can contribute to lowering blood cholesterol levels and a reduced risk for arterial plaque formation.
7.2 Lipid Digestion and Absorption
Lipids are large molecules and generally not water-soluble. You can see that this is the case if you pour oil into a glass of water. The oil and water do not mix, and the oil floats to the top. Like carbohydrates and protein, during digestion lipids are broken into smaller components for absorption. Since most of our digestive enzymes are water based, how does the body break down lipid and make it available for the various functions it must perform in the human body?
From the Mouth to the Stomach
The digestion of lipids is really the digestion of triglycerides since these are by far the most abundant form of fat in the diet. Saliva contains an enzyme, lingual lipase, and a small amount of phospholipid as an emulsifier. While lingual lipase is an important enzyme for infants as it begins digestion of milk fats, adults produce very little. Therefore, in adults, no chemical digestion of lipids occurs in the mouth. However, mechanical digestion occurs with saliva softening the food in the mouth to create a bolus and peristaltic contractions of the esophagus deliver the bolus to the stomach.
From the Stomach to the Small Intestine
In the stomach, gastric lipase, secreted from cells in the stomach walls, begins the chemical break down of triglycerides by removing a fatty acid and turning triglycerides into diglycerides (two fatty acids attached to a glycerol). Within two to four hours after eating a meal, roughly 30% of the triglycerides are converted to diglycerides and free fatty acids. The stomach’s churning and contractions help to disperse the fat molecules, while the diglycerides derived in this process act as further emulsifiers. However, even amid all of this activity, very little fat digestion has occurred thus far in the body.
As stomach contents enter the small intestine, the digestive system sets out to manage a small hurdle, namely, to combine the separated fats with its own watery fluids. The solution to this hurdle is bile. Bile is made in the liver and is stored in the gallbladder. As chyme enters the duodenum a hormone, cholecystokinin (CCK), is released. This hormone tells the gallbladder to release bile into the duodenum. Bile contains bile salts, lecithin, and substances derived from cholesterol so it acts as an emulsifier. It attracts and holds onto fat while it is simultaneously attracted to and held on to by water, forming a bridge. Emulsification increases the surface area of lipids over a thousand-fold, making them more accessible to the water-based enzyme lipase.
Another hormone mentioned in previous chapters, secretin, is also released as chyme enters the duodenum. Its function is to signal the pancreas to release digestive juice containing bicarbonate to neutralize stomach acidity and lipid digesting enzymes including lipase. Once the stomach contents have been emulsified, pancreatic lipase works on the triglycerides and diglycerides to cleave fatty acids from their glycerol foundations into free fatty acids and monoglycerides.
Table 7.2.1 Summary of Secretions and their Functions in Lipid Digestion
| Organ | Secretion | Function |
| Salivary Glands | Saliva | Moisten and soften food |
| Lingual Lipase (enzyme) | Begins breakdown of large lipids—primarily in infants | |
| Stomach | Gastric Lipase (enzyme) | Removes fatty acid from triglycerides to form diglycerides |
| Small Intestine | Secretin (hormone) | Signals pancreas to release secretions |
| Cholecystokinin (hormone) | Signals gallbladder to release bile | |
| Gallbladder | Bile | Emulsifies triglycerides, increasing their surface area so that they are more accessible to water-based lipase |
| Pancreas | Bicarbonate | Neutralizes hydrochloric acid in chyme |
| Pancreatic Lipase (enzyme) | Continues breakdown of tri- and diglycerides into monoglycerides and free fatty acids |
Lipid Absorption
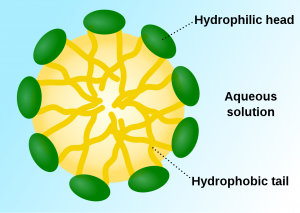
Once fats are digested, another hurdle presents itself. How will the fatty acids pass through the watery layer of mucus that coats the absorptive lining of the digestive tract? As before, the answer is bile. Bile salts envelop the fatty acids and monoglycerides to form micelles. Micelles have a fatty acid core with an exterior that is water-soluble. This allows efficient transportation through the watery mucus and into the intestinal microvilli. The fat components are then released and disseminated into the cells of the digestive tract lining.
Recall from Chapter 4 that in each intestinal villus there are two vessels: a capillary carrying blood, and a lymphatic vessel (lacteal) carrying lymph. Just as lipids require special handling in the digestive tract to move within a water based environment, they require similar handling to travel in the bloodstream. Inside the intestinal cells, short and medium chain fatty acids are easily transported through the intestinal walls and absorbed directly into the bloodstream, but long chain fatty acids and monoglycerides need help because they’re too large to enter the small capillaries. Instead, they reassemble themselves into triglycerides. Then triglycerides, cholesterol, and phospholipids form lipoproteins (lipid + protein) which have an inner core that is primarily made up of triglycerides and cholesterol esters (a cholesterol linked to a fatty acid), and an outer envelope or shell made of protein, phospholipids, and cholesterol. Together they form a chylomicron, which is a large lipoprotein that now enters the lacteal. The lymphatic vessel has a larger diameter to accommodate the larger size of the chylomicron as opposed to the much smaller capillary. These chylomicrons travel through the vessels of the lymphatic system, in a route that passes the heart. The lymphatic vessels connect with the bloodstream via the jugular vein in the neck, and the chylomicrons continue through the bloodstream to their final destinations—primarily the liver. Chylomicrons are the perfect transport vessel for delivery of food fats through the body’s water-based blood to the liver and other body tissues.
Dietary cholesterol molecules are poorly absorbed when compared to phospholipids and triglycerides. Cholesterol absorption is aided by an increase in dietary fat and is hindered by high fiber content. This is the reason that a high intake of fiber is recommended to decrease blood cholesterol. Foods high in fiber such as fresh fruits, vegetables, and oats can bind bile salts and cholesterol, preventing their absorption and carrying them out of the small intestine and into the large intestine for removal from the body.
Almost all dietary fats are digested and absorbed in the small intestine. However, if fats are not absorbed properly as is seen in some medical conditions, they will continue into the large intestine, and a person’s stool will contain high amounts of fat. If fat malabsorption persists the condition is known as steatorrhea. Steatorrhea can result from diseases affecting absorption such as Crohn’s disease, ulcerative colitis, and cystic fibrosis.
Lipid Transport – from Liver to the Body
Recall that chylomicrons are transporters of fats through the watery environment within the blood. After about ten hours of circulating throughout the body, chylomicrons arrive at the liver, carrying dietary fats from the small intestine. The chylomicrons are dismantled and used as raw materials by the liver to formulate additional lipoproteins. Why? Because cells in the body require fats for many functions. These fats must be delivered through the watery bloodstream, and just like their journey from the small intestine, fats require a protein-covered delivery system—lipoproteins. The following is a list of the various lipoproteins and their functions:
- VLDLs. Very low-density lipoproteins are made in the liver from remnants of chylomicrons and transport triglycerides from the liver to various tissues in the body. VLDLs have a core made of cholesterol, surrounded by a ring of triglycerides, and a protein coating of phospholipids. They are considered “very low density” because they are primarily triglycerides which are less dense and lighter than the watery blood. As the VLDLs travel through the circulatory system, an enzyme called lipoprotein lipase strips the VLDL of triglycerides so that they can be used in body cells. As triglyceride removal continues, the VLDLs begin to shrink and become intermediate-density lipoproteins.
- IDLs. Intermediate-density lipoproteins continue to transport a variety of fats and cholesterol in the bloodstream and contain about half of the triglycerides of the VLDL. While traveling in the bloodstream, cholesterol is gained from other lipoproteins while circulating enzymes remove its phospholipid component. When IDLs return to the liver, they are transformed into low-density lipoprotein.
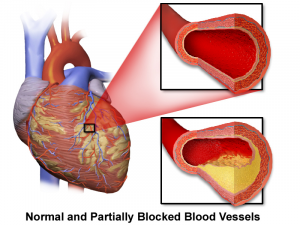
- LDLs. Low-density lipoproteins are commonly known as “bad cholesterol.” It is imperative that we understand their function in the body so as to make healthy dietary and lifestyle choices. When VLDLs and IDLs lose their triglycerides to body cells, what remains is the cholesterol core. What happens to it? Remember from the previous section that cholesterol participates in many cellular functions in the body. As the LDLs deliver cholesterol and other lipids to the cells, each cell’s surface has receptor systems specifically designed to bind with LDLs. Circulating LDLs in the bloodstream bind to these LDL receptors and are consumed. Once inside the cell, the LDL is taken apart and its cholesterol is released. Diets rich in saturated fats will inhibit the LDL receptors, leaving LDLs to continue to circulate in the blood. When this occurs, some of the LDLs may deposit their cholesterol on artery walls, leading to atherosclerosis. Thus, LDL receptors are critical for regulating blood cholesterol levels.
- HDLs. High-density lipoproteins are also made in and released from the liver. They are responsible for escorting circulating LDLs out of the bloodstream and back to the liver, removing LDLs from circulation. In the liver the components of the LDL are either reused or removed from the body as a component of bile. HDLs have a very large protein shell coupled with a low cholesterol content (20-30%) compared to the other lipoproteins. This makes them dense when compared to other lipoproteins so are called high density. These HDLs rid the bloodstream of excess LDLs and are commonly called “good cholesterol.”
Table 7.2.2 Summary of Lipid Absorption and Transport
| Component | Function |
| Micelle | Transporter of lipid from lumen (interior) of small intestine, through the mucus layer and into the microvilli |
| Lipoproteins | |
| Chylomicron | Transport long chain fatty acids*, triglycerides, phospholipids, cholesterol into lymphatic system; lymphatic system merges with bloodstream and chylomicrons eventually travel to the liver |
| VLDL | Made in the liver; contain cholesterol, triglycerides in protein shell; transport lipids to the body cells—lipoprotein lipase removes triglycerides from VLDL/IDL for cell use |
| LDL | After triglycerides removed from VLDL/IDL, cholesterol remains; can deposit excess cholesterol on arterial walls forming plaque and carries lipids that are pro-inflammatory; called “bad” cholesterol |
| HDL | Made in liver; primarily a protein shell; travels through bloodstream removing LDL and cholesterol from cells, tissue, and blood and returning it to the liver; anti-inflammatory; called “good” cholesterol |
| *Short and medium chain fatty acids are absorbed directly into the blood and are taken to the liver | |
7.3 Functions of Lipids
In the Body
Lipids have major roles in the body. They are part of cell membranes (phospholipids), they are an abundant source of energy, they function as important signaling molecules, and they provide protection and insulation.
Energy Source
The excess energy from the food we eat is digested and incorporated into adipose (or fat) tissue. Most of the energy required by the human body is provided by carbohydrates and lipids. While glycogen provides a ready source of energy, adipose tissue functions as an energy reserve and provides the majority of the energy fueling body functions. Fats are packed together tightly without water and store far greater amounts of energy in a reduced space compared to glycogen. A fat gram is densely concentrated with energy—it contains more than double the amount of energy than a gram of carbohydrate: 9 kcal/g for fat, 4 kcal/g for carbohydrate.
Similarly to carbohydrate, the breakdown of fatty acids for energy occurs in most body cells through cellular respiration. Unlike glucose, fatty acids can only be broken down for energy in the mitochondria and only under aerobic conditions. Fatty acids must first be activated by combining with coenzyme A, an enzymatic process which requires energy. They are then transported into the mitochondria of cells and are oxidized in a process called beta-oxidation where carbons of the fatty acid are cleaved off two at a time and combined with coenzyme A to form acetyl CoA. The acetyl CoA then enters the Kreb’s Cycle which generates a few ATP and electron carriers NADH2 and FADH2 that are processed through the electron transport chain (ETC), generating many ATP.
As discussed previously, triglycerides are the most common form of lipid in the diet and in our bodies. They are made up of a glycerol backbone and three fatty acids. They are large molecules! Each fatty acid contains between 4 and 24 carbons. During breakdown, these carbons are cleaved off in pairs to create Acetyl CoA. So during beta oxidation, a single fatty acid containing 18 carbons, for example, would become 9 Acetyl CoA molecules. The ATP generated from these 9 acetyl CoA molecules from a single 18-carbon fatty acid in the Kreb’s cycle and ETC is 120 ATP! It is easy to see why fatty acids are our body’s greatest source of energy.
The glycerol “backbone” of triglycerides can also be catabolized for energy. It must be activated by phosphorylation. Then it can be converted into pyruvate or glucose, and catabolized. Glycerol provides about 5% of the energy provided by the breakdown of triglycerides.
Regulating and Signaling
Triglycerides control the body’s internal climate, helping to maintain constant temperature. Those who don’t have enough fat in their bodies tend to feel cold sooner, are often fatigued, and may develop pressure sores on their skin from fatty acid deficiency. Triglycerides also help the body produce and regulate hormones. For example, adipose tissue secretes the hormone leptin, which helps to regulate appetite. In the reproductive system, fatty acids are required for proper reproductive health; women who lack proper amounts may stop menstruating. Omega-3 and omega-6 essential fatty acids help regulate cholesterol, blood clotting, and control inflammation in the joints, tissues, and bloodstream. Fats also play important functional roles in the brain sustaining memory storage and tissue structure. They help form nerve cell membranes, insulate neurons, and facilitate the signaling of electrical impulses throughout the brain.
Insulating and protecting
The composition of the brain is amazingly 60% fat, demonstrating the major structural role that fat serves within the body. Some of our body fat, called visceral fat, is specifically located around our heart, kidneys and liver and acts to cushion and protect them. You may be more familiar with subcutaneous fat, or fat located just underneath the skin. This blanket layer of tissue insulates the body from extreme temperatures and helps keep the internal climate under control. It pads our hands and buttocks and prevents friction, as these areas frequently come in contact with hard surfaces.
Increasing Bioavailability
Fats increase the bioavailability of compounds known as phytochemicals, which are plant constituents such as lycopene (found in tomatoes) and beta-carotene (found in carrots and other red, yellow, and orange vegetables). Phytochemicals are believed to promote health and well-being. As a result, eating tomatoes with olive oil or salad dressing will facilitate lycopene absorption. Other essential nutrients, such as essential fatty acids, are constituents of the fats themselves and serve as building blocks of a cell.
Roles of Lipids In Food
Fats tend to make foods smell good, taste good, and give food a pleasing, creamy texture.
High Energy Source
Fat-rich foods naturally have a high kccal density. (Remember that fat contains 9 kcal/g as opposed to carbohydrate and protein which contain 4 kcal/g). High fat foods are calorie dense and a convenient source of energy. Depending on the level of physical activity and nutritional needs, fat requirements can vary greatly from person to person, and the AMDR for fat is 20-35% of total kcal. When energy needs are high, the body welcomes the high energy density of fats. For instance, infants and growing children require proper amounts of fat to support normal growth and development. If an infant or child is given a low fat diet for an extended period, growth and development will not progress normally. Other individuals with high energy needs are athletes, people who have physically demanding jobs, and those recuperating from illness.
Dietary Fats: Athletes vs. Average
When the body has used most of its energy from carbohydrates (this can occur after just 15-20 minutes of high intensity exercise), it turns to stored fat as its energy source. A long distance elite swimmer must consume large amounts of food energy to meet the demands of their sport, so eating fat-rich foods makes sense. In contrast, if a person who leads a sedentary lifestyle eats the same energy dense fatty foods, they will intake more fat calories than their body requires within just a few bites. The body stores these excess calories as adipose tissue. So use caution, consumption of kcal beyond energy requirements is a contributing factor to obesity.
Smell, Taste, Mouthfeel
Fat contains dissolved compounds that contribute to mouth watering aromas and flavors. Fat also adds texture to food, contributing to improved mouthfeel (the physical sensation of food in the mouth). Baked foods are supple and moist. Frying foods locks in flavor and lessens cooking time. How long does it take you to recall the smell of your favorite food cooking? What would a meal be without that savory aroma to delight your senses and heighten your preparedness for eating a meal? You can thank fats in foods for these sensations.
Satiety/appetite
Fat plays another valuable role in nutrition. Fat contributes to satiety, or the sensation of fullness. When fatty foods are swallowed the body responds by enabling the processes controlling digestion to slow the movement of food along the digestive tract, thus promoting an overall sense of fullness. Often before the feeling of fullness arrives, people overindulge in fat-rich foods, finding the delectable taste irresistible. This is part of appetite (the psychological desire for food) and another reason to encourage savoring a meal slowly. Indeed, the very things that make fat-rich foods attractive can also make their over-consumption a hindrance to maintaining a healthful diet.
7.4 Lipids, Diet, and Personal Choices
In this chapter, you have learned about the different types of lipids and the role they play in the body and in our food. You may reason that if some fats are healthier than other fats, why not consume as much healthy fat as desired? Remember, everything in moderation. All fats are energy dense, containing 9 kcal per gram. As we review the established guidelines for daily fat intake, the importance of balancing fat consumption with proper fat sources will be explained.
How Much Do You Need?
Most health groups provide similar recommendations for lipid intake. The Dietary Reference Intake (DRI) Committee, American Heart Association (AHA), and the 2020-2025 Dietary Guidelines all recommend:
- Fat kcal should be limited to 20-35% of total kcals (AMDR) with most fats coming from MUFA and PUFA, such as those found in fish, nuts, lean meats, vegetable oils, low-fat dairy, and plant-based alternatives.
- Consume fewer than 10% of kcal from saturated fats. Remember that saturated fats are solid fats. Some studies suggest that lowering the saturated fat content to less than 7% can further reduce your risk of heart disease, particularly if one has a genetic predisposition to it.
- Avoid trans fats (any food label that reads hydrogenated or partially hydrogenated oil) completely. There is no safe amount of trans fat.
- Consume fatty fish for omega-3 fatty acids at least twice per week or at least 8 oz weekly
Food for Thought
Are you getting the recommended amount of lipids in your diet? Would you say that your intake consists of more saturated fats (solid fats) or more oils (liquid fats)?
Table 7.4.1 Evaluating Sources of Fat in Overall Dietary Pattern
| Type of Fat/Characteristics | Choose/Limit/Avoid | Foods |
Monounsaturated fats
|
Choose – often called “good fat” | Plant oils, nuts (almonds, cashews, pecans, peanuts, walnuts), nut products, avocados, extra virgin olive oil, sesame oil, high oleic safflower oil, sunflower oil, canola oil |
Polyunsaturated fats
|
Choose | Plant-based food, oils, fish, nuts (walnuts, hazelnuts, pecans, almonds, peanuts), soybean oil, corn oil, safflower oil, flaxseed oil, canola oil, fish
Fatty fish (tuna, herring, mackerel, trout, salmon), seeds (chia, hemp, flax), cod liver oil Eggs, poultry, most vegetable oils, wheat germ oil, whole grains, cereals, nuts, seeds (sunflower, sesame, watermelon) |
Saturated fats
|
Limit to less than 10% total kcal from fat | Animal foods, dairy (cheese), palm and coconut oils, butter |
| Trans fats | Avoid – there is no safe level of consumption
Read food labels carefully |
Processed foods, stick margarines, fast foods, commercial baked goods, some snack foods |
More About Trans Fats
Trans fatty acids occur in tiny amounts in nature. However, the trans fats that are used by the food industry are produced via the hydrogenation process. As discussed previously, trans fats are a result of the partial hydrogenation of unsaturated fatty acids, which cause them to have a trans configuration, rather than the naturally occurring cis configuration. Because trans fats can behave like saturated fats, the body processes them similarly. Consuming large amounts of trans fats has been associated with tissue inflammation throughout the body, insulin resistance in some people, weight gain, digestive issues, and coronary heart disease. In addition, the hydrogenation process robs the person of the benefits of consuming the original oil because hydrogenation destroys omega-3 and omega-6 fatty acids.
The World Health Organization (WHO) estimates that industrially produced trans fats contributes to nearly 500,000 deaths per year from coronary heart disease. Nearly 60 countries worldwide, including the US, have introduced limits or bans on trans fatty acids in their food supplies.3 Since 2006 it has been required that food manufacturers in the US list the amount of trans fat in their products on the Nutrition Facts Label (NFL) although they are allowed to put zero grams of trans fat on the NFL if the product contains less than 0.5 grams per serving.4 More recently, the FDA revoked Generally Recognized as Safe (GRAS) status of partially hydrogenated vegetable oil and required its use to be phased out by January 2021.5 The AHA states that, like saturated fats, trans fats raise LDL and trans fats lower HDL cholesterol and advises avoiding trans fat.6
What should I choose—butter or margarine?
Originally margarine was an inexpensive substitute for butter, made from combining emulsified fats or oils with water or milk to make it spreadable with less saturated fat. In the creation of margarine using partial hydrogenation, trans fat is a byproduct. When saturated fats were linked with heart disease, margarine use was recommended as the alternative. However, it turns out that the trans fat byproducts are actually worse than saturated fat in altering biomarkers associated with cardiovascular disease. Trans fat increases LDL (bad cholesterol) and decreases HDL (good cholesterol) levels, while saturated fat increases LDL without altering HDL levels. With the ban on trans fats, will margarine disappear? The answer is no. Margarine can be made using complete hydrogenation of vegetable oils instead of partial. This reduces the saturated fat content but does not result in the trans fat byproducts. It is too soon to tell if these new margarines will be a healthier option. Whether you choose to use butter or margarine, remember that both contain the same number of kcals per gram and are energy dense, so use in moderation.
Dietary Fat Replacers
In response to the rising awareness and concern over the consumption of trans fat and saturated fats, various fat replacers have been developed. Fat substitutes aim to mimic the richness, taste, and smooth feel of fat without the same kcal content as fat. There are three main types of fat replacers: carbohydrate-based, protein-based, and fat-based. The carbohydrate-based replacers tend to bind water and thus dilute kcal. They are usually made from starchy carbs, and make up the bulk of the fat replacers used in foods today. Examples include dextrin, cellulose, gums, and modified dietary fibers. Fat substitutes can also be made from proteins (for example, egg whites and milk whey). However, these are not very stable and are affected by changes in temperature, hence their usefulness is somewhat limited. Fat-based replacers are made by replacing the triglycerides in vegetable oils. Examples of these include olestra which is non-caloric (marketed as Olean), and salatrim (marketed as Benefat). Because fat replacers do not have to be listed on labels with their brand name, it may be difficult for consumers to identify them.
Are fat replacers safe to consume? Currently there is no evidence that carbohydrate-based or protein-based replacers affect health negatively. Lipid-based olestra may interfere with absorption of fat-soluble vitamins, carotenoids, and antioxidants. Some consumers of olestra may also experience cramping, bloating, and loose stools.7 Another alternative is to replace high fat foods with lower kcal, lower fat alternatives. There are many lists on the internet that provide lower fat substitutions for high fat food items, such as this one from the National Heart, Lung, and Blood Institute (NHLBI), a division of the National Institutes of Health (NIH).8
7.5 Diseases and Conditions Involving Lipids
Chronic diseases are ongoing, life-altering, and often life-threatening health challenges. They are the leading cause of death worldwide. Chronic conditions are increasing in frequency. They cause significant physical and emotional suffering and are an impediment to economic growth and vitality. Several chronic diseases are related to dietary lipids including cardiovascular disease, hypertension, and stroke.
Risk Factors
You may recall from Chapter 1 that a risk factor is a signal that your chances for acquiring a chronic disease may be increased. You might liken a risk factor to the flags that lifeguards sometimes set up at beaches. When you see these flags, you know immediately that swimming within the marked areas could be hazardous, and that if you choose to swim within these parameters anyway, you are doing so at your own risk. But if you heed the warnings, you are taking the necessary step to protect your safety and health. Similarly, risk factors are warning signs that coincide with the development and progression of disease. However, risk factors are not a 100% guarantee that a person will develop a chronic disease, only that the conditions are right. For example, if a person gets sick with the flu, we can say with certainty that the illness was caused by a virus. However, we cannot say definitively that a sedentary lifestyle caused the onset of cardiovascular disease in a patient, because a risk factor indicates a correlation (or link) not a causation. Chronic disease development usually includes a combination of risk factors.
Risk factors such as genetics and age cannot be changed and are therefore described as non-modifiable. For example, being a woman over age 65 is a risk factor for developing osteoporosis. A person cannot change their genetic information or family history. However, some risk factors can be modified to promote health and wellness (such as diet). For example, a person who continuously eats a diet high in sugars, saturated fats, and red meat is at risk for becoming obese and developing type 2 diabetes, cardiovascular disease, and/or several other conditions. Making more healthy dietary choices can greatly reduce that risk. People without a genetic predisposition for a particular chronic illness can still develop it. Not having a genetic predisposition for a chronic disease is not a guarantee of immunity.
Identifying Your Risk Factors
To estimate your own risk factors for developing certain chronic diseases, search through your family’s medical history. What diseases do you note showing up among close blood relatives? These may be of concern to you. At your next physical, pay attention to your blood tests and ask the doctor if any results are out of normal range. It is also helpful to note your vital signs, particularly your blood pressure and resting heart rate. In addition, you may wish to keep a food diary to make a note of the dietary choices that you make on a regular basis and be aware of foods that are high in saturated or trans fat, among other unhealthy options. As a general rule, it is important to look for risk factors that you can modify to promote your health. For example, if you discover that your grandmother, aunt, and uncle all suffered from high blood pressure, then you may want to avoid a high sodium diet. Identifying your risk factors can arm you with the information you need to help ward off disease.
Cardiovascular Disease (CVD)
Cardiovascular or heart disease is the leading cause of death in the US for both men and women and for people of most ethnicities. For American Indians or Alaska Natives and Asians or Pacific Islanders, heart disease is second only to cancer. Approximately 610,000 Americans die of heart disease each year. That’s one in every four deaths in this country from heart disease.9
The term “heart disease” is a general term for any cardiovascular issues. The most common type is coronary artery disease (CAD), which can cause a heart attack. Other kinds of heart disease may involve the valves in the heart, or the heart may not pump well and cause heart failure. Some people are born with heart problems that lead to heart attack. Anyone can develop heart disease. About half of all Americans have at least one of the three key risk factors for heart disease: smoking, high blood pressure, or high cholesterol.10
Table 7.5.1 Risk Factors for Cardiovascular Disease9
| Non-Modifiable Risk Factors | Modifiable Risk Factors |
| Age: Risk increases as age increases; for men at 45 years and for women at 55 years | Blood Pressure: High blood pressure often has no symptoms, but added pressure on the walls of the blood vessels can cause vessel damage and damage other organs including the heart |
| Sex: Men have a higher risk than women until after menopause, then the risk for women greatly increases | Unhealthy Cholesterol Levels: High levels of blood cholesterol can increase risk. A high level of LDL, and/or low levels of HDL can promote atherosclerosis and increase risk |
| Family History: The more family members who have heart disease the greater the risk | Diabetes: Uncontrolled blood glucose increases risk of cardiovascular diseases |
| Race and Ethnicity: High risk groups include African Americans, whites, American Indians, and Alaskan Natives. | Obesity: Excess weight worsens other risk factors |
| Others: Excessive alcohol consumption; physical inactivity; eating a diet high in saturated and trans fats; tobacco use |
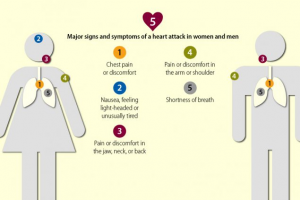
For many, the first clue that they have an issue with their heart is when they have a heart attack (myocardial infarction). When plaque builds up in the arteries, the arteries narrow over time. This narrowing reduces blood flow to the heart, eventually causing a heart attack. Cells in the heart muscle that do not receive enough oxygenated blood begin to die and the more time that passes without restored blood flow, the greater the damage to the heart. According to the Centers for Disease Control and Prevention (CDC), someone in the US has a heart attack every 40 seconds.11 Symptoms of a heart attack vary depending on the type of heart disease. For many suffering a heart attack, the first sign is chest pain or discomfort (angina). Some heart attack sufferers may experience several symptoms. The 5 major symptoms of a heart attack are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that lasts for more than a few minutes or that goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain.
- Feeling weak, light-headed, or faint. You may also break out into a cold sweat.
- Pain or discomfort in the jaw, neck, or back.
- Pain or discomfort in one or both arms or shoulders.
- Shortness of breath. This often comes along with chest discomfort, but shortness of breath can also happen before chest discomfort.
Other symptoms of a heart attack could include unusual or unexplained tiredness, and nausea or vomiting. Women are more likely to have these other symptoms.11 If you think that you or someone you know is having a heart attack, call 911 immediately.
Hypertension (High Blood Pressure)
Another form of CVD is hypertension or high blood pressure. Blood pressure is the force of blood pushing against the walls of your arteries, which carry blood from your heart to other parts of your body, and back to the heart. Blood pressure normally rises and falls throughout the day. But if it stays high for a long time, it can damage your heart and lead to other health problems. Hypertension is a common and dangerous condition, putting you at risk for heart disease and stroke, two of the leading causes of death in the US.
Blood pressure readings consist of two numbers. The top number measures systolic pressure (the pressure against the walls of the arteries immediately after the heart contracts) and the bottom number measures diastolic pressure (when the heart is at rest between beats). What should blood pressure be?
Table 7.5.2 Blood Pressure Numbers12
| Systolic (mmHg) | Diastolic (mmHg) | |
| Ideal | < 120 | < 80 |
| Prehypertension | 120-139 | 80-89 |
| Hypertension | ≥ 140 | ≥ 90 |
About one of every three American adults (or about 75 million people) has hypertension. Only about half (54%) of these people have their high blood pressure under control. Hypertension is often called the “silent killer” because it often has no warning signs or symptoms, and many people do not know they have it.13
Table 7.5.3 Risk Factors for Hypertension
| Non-modifiable | Modifiable |
| Age. After age 55, hypertension risk is 90% | Weight. Approximately 60% of those with hypertension are overweight |
| Race. African Americans are more likely to develop hypertension and manifest it at a younger age | Sodium Consumption. The more salt in a person’s diet, the more likely they are to have high blood pressure |
| Family History. There is a strong genetic component to high blood pressure and an individual’s risk increases with the number of family members who have hypertension | Alcohol. Drinking more than two drinks per day for men and one drink for women increases the likelihood of hypertension |
Take a quiz to test your basic knowledge about blood pressure: Blood Pressure 101: Know the Basics
One of the reasons for hypertension is the accumulation of plaque which narrows and hardens arteries. This elevates blood pressure because the vessels cannot expand effectively to accommodate the pulses of blood coming from the heart. Chronically high blood pressure strains the heart and can cause additional damage, leading to a stroke.
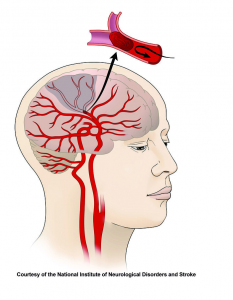
Stroke is the fifth leading cause of death in the US. Someone has a stroke every 40 seconds; almost 800,000 people per year.14 Strokes can occur when arterial walls become so weakened that they balloon and form what is known as an aneurysm. If the aneurysm bursts, it is a life-threatening event because blood rushes out of the hole in the artery wall. Strokes can also occur when the plaques that have formed on the artery walls rupture. The body responds to this perceived “injury” by forming blood clots. These clots may stay stationary (a thrombus) or move through the circulatory system (an embolus). If it stays stationary it can slowly kill off surrounding tissue, or grow so big that it blocks blood circulation, causing thrombosis. If it moves through the circulatory system, it can get stuck in a smaller artery, cutting off blood flow and causing cell death. This is referred to as an embolism. Blood clots in the heart or brain arteries can cause heart attacks or strokes, respectively. The most important thing is to take action immediately if you think someone is having a stroke. Many treatments work best within three hours of the onset of first symptoms. The sooner the victim gets medical help the more likely they are to survive. Signs and symptoms of a stroke include:
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body
- Sudden confusion, trouble speaking, or difficulty understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination
- Sudden severe headache with no known cause

The CDC recommends that you act F.A.S.T. if you suspect a stroke14:
F –Face: Ask the person to smile. Does one side of the face droop?
A –Arms: Ask the person to raise both arms. Does one arm drift downward?
S –Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
T –Time: If you see any of these signs, call 9-1-1 right away.
It is also helpful to note the time when any symptoms first appear. This information can help health care providers determine the best treatment for each person. If you think you are having a stroke, do not drive yourself to the hospital. Let someone else drive you or call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
Transient Ischemic Attacks (TIA)
TIAs are often called “mini-strokes.” They share the symptoms of a stroke, but symptoms do not persist. Don’t ignore these. They are signs that there is an issue that needs to be addressed.
In most cases, the damage done by hypertension takes place over time. Left undetected (or uncontrolled), it can lead to15:
- Congestive Heart Failure (CHF). The increased workload from hypertension can cause the heart to enlarge and fail to supply blood to the body.
- Chronic Kidney Disease (CKD) or even renal failure. Hypertension can damage the arteries around the kidneys and interfere with their ability to filter blood effectively.
- Vision loss. Hypertension can strain or damage blood vessels in the eyes.
- Sexual dysfunction. Hypertension can lead to erectile dysfunction in men or lower libido in women.
- Angina. Over time, hypertension can lead to heart disease. Angina, or chest pain, is a common symptom.
- Peripheral artery disease (PAD). Atherosclerosis caused by hypertension can cause a narrowing of arteries in the legs, arms, stomach and head, causing pain, fatigue, or ischemia (inadequate of blood flow).
Hypercholesterolemia (High Blood Cholesterol)
As discussed previously, high blood cholesterol (hypercholesterolemia) is a risk factor for CVD. We know that it is best to have relatively low LDL cholesterol and relatively high HDL circulating in the bloodstream. You can find out the level of blood cholesterol and the levels of various lipoprotein components by having a blood cholesterol test, also called a lipid panel or lipid profile. According to the National Heart, Lung and Blood Institute of the National Institutes of Health (NIH), current guidelines recommend testing for young adults every 5 years, every 1-2 years for adults 45-65 years, and every year for people over age 65.16 If there is a family history of high cholesterol, your healthcare provider may suggest a test sooner or more often than this. Testing calls for a blood sample to be drawn after 9 to 12 hours of fasting for an accurate reading. By this time, most of the fats ingested from the previous meal have circulated through the body and the concentration of lipoproteins in the blood will have stabilized.
Blood Cholesterol Recommendations
According to the NIH, the following recommended values are used to measure an overall lipid profile:
- Total cholesterol: < 200 milligrams/deciliter (mg/dL)
- LDL: < 129 mg/dL
- HDL: 40-60 mg/dL
- Triglycerides: < 150 mg/dL
- VLDL: < 30 mg/dL
Metabolic Syndrome, Syndrome X, or Insulin Resistance Syndrome
Metabolic syndrome is a cluster of factors that make a person more likely to suffer from CVD, type 2 diabetes, and/or a stroke. About 1 in 3 adults in the US have it.17 Doctors assess five areas to determine whether or not a patient has metabolic syndrome, and a person with three or more of the following conditions would be diagnosed with this condition:
- having a large waist circumference (> 35 in for women, > 40 in for men; apple-shaped)
- hypertension (≥ 130/85 mm Hg)
- high levels of blood triglycerides (≥ 150 mg/dL fasted)
- low levels of “good” cholesterol levels (< 50 mg/dL HDL for women, < 40 mg/dL HDL for men )
- high blood glucose levels (≥ 100 mg/dL)
The underlying causes of metabolic syndrome include being overweight or obese, having insulin resistance, and being physically inactive. High levels of body fat, especially in the abdomen, can modify hormones that help the body digest and use carbohydrates. This leads to insulin resistance, which leads to modification of blood triglycerides and HDL, and it can also raise blood pressure. In addition, extra body fat leads to inflammation which contributes to plaque formation in blood vessels.17
Reducing the Risk of Cardiovascular Diseases
Diet and nutrition can play a significant role in reducing the risk of CVD and metabolic syndrome. It is helpful to lower sodium intake to less than 2,400 mg per day, increase consumption of dietary fiber, especially soluble fiber that reduces cholesterol absorption into the bloodstream, and limit consumption of saturated fat, which promotes plaque formation. In addition, it is important to replace refined starches and added sugar (which can boost triglycerides) with whole grains, vegetables, and fruits. Eating foods rich in omega-3 fatty acids, especially fatty fish, using alcohol in moderation, and opting for low or no-fat dairy products can all help reduce your CVD risk. Emphasizing vegetable-based sources of protein, such as nuts, beans, seeds, and legumes, can be beneficial, as well as consuming more soy products and minimally processed vegetable oils like extra virgin olive oil. Regular exercise is also essential for reducing CVD risk, and please don’t smoke or use tobacco products of any kind. If you find it difficult to remember the list of recommendations, just remember the three most important ways to reduce risk of all chronic disease: don’t smoke, eat more plants (especially whole plants), and exercise regularly.
Dietary Approaches to Stop Hypertension (DASH)
7.6 Choosing Dietary Fats
Fat is an important part of a healthy diet, but it is easy to overindulge because of its energy density. Making healthier choices for your fat kcal budget is key. When grocery shopping, read all food labels carefully and seriously consider everything that goes into your shopping cart. At restaurants, learn to look for clues on the menu which can help you choose wisely. As you refine your understanding of dietary fat, here are key points to bear in mind:
- The NFL provides information about total fat, saturated fat, and trans fat. It may also include information about specific unsaturated fats. Check the %DV for each of these categories. Remember that total fat, saturated fat, or trans fat with a %DV of <5% would most likely be a healthy choice. For a review of how to read food labels, see Chapter 2.
- When selecting prepared foods (frozen or fresh), opt for those without creamy high-fat sauces or gravies. For snacks and daily eating, gravitate toward foods that are lowest in or absent of saturated fats. If selecting precooked meats, avoid those that are fried, coated, or prepared in high-fat sauces. A popular and healthier precooked meat choice is the rotisserie chicken that most supermarkets carry.
- When selecting meats be aware of the need to compare different cuts—notice their fat content, color, and marbling. Higher fat meats tend to have white fat marbled throughout. Choose lean cuts (like loin or round) and white meat as these are lower in saturated fat.
- Minimize your intake of saturated fat by avoiding foods containing fats that are solid at room temperature (think bacon or the fat on a steak). It’s also recommended to reduce your consumption of red meat, processed meats (sausage, bacon, hot dogs, beef jerky, etc.), and full-fat dairy products. When consuming dairy products, choose low-fat or non-fat options such as mozzarella cheese instead of cheddar, or yogurt instead of ice cream.
- Maximize your intake of mono- and polyunsaturated fat. These unsaturated fats tend to be more liquid at room temperature, and monounsaturated fats are especially beneficial to overall health. Foods containing monounsaturated fat include fish, nuts and nut butters, avocados, olives and olive oil, and canola oil. Make sure to get your omega-3 fatty acids, a type of polyunsaturated fat by consuming a moderate serving of fish, walnuts, ground flaxseeds, flaxseed oil, or soybean oil in your diet every day. To derive the most benefit from including these foods, do not add them to an existing diet full of fat. Use these to replace the saturated fats that are being removed from the diet.
- Always choose plenty of fresh fruits, vegetables, nuts, and seeds, as their phytosterols are a good competitor for cholesterol. Keep a collection of nuts in your fridge or freezer that can be added to your salads, stir-fry, one-dish meals, soups, desserts, and yogurts.
- When cooking at home use cooking sprays or non-stick pans that don’t require any fat for cooking instead of solid fats. Grill, bake, stir-fry, or roast your foods. Never fry in solid fats such as shortening. Marinate foods to be grilled in fruit juices and herbs. Instead of relying upon commercial salad dressings, learn to make your own top-quality dressing from cold-pressed olive oil, flaxseed oil, or sesame oil to reduce sodium content. Use herbs and spices to add flavor. Avoid using high-fat meat gravies, cheese, and cream sauces. Limit adding extras to foods such as butter or bacon bits on a baked potato. Use non-fat sour cream or a flavorful pile of other roasted vegetables on top instead.
- Remember that fat adds flavor. Choose a flavorful unsaturated oil like sesame oil, peanut oil, or a nut butter to add flavor to foods. Because of the stronger flavors, less is required. This is also true for cheese; choose Romano, Parmesan, or Asiago in place of American, Swiss, or Cheddar.
- At restaurants, avoid ordering items with descriptive terms like white sauce (Alfredo), breaded, crispy, smothered, gooey, rich, velvety, or au gratin as these imply the use of ingredients like cheese or cream. If you are ordering something with a sauce, ask for it “on the side” so that you can control how much you actually put on your entree. Be careful with the “free” items served prior to the meal like chips and salsa, garlic sticks, or bread and butter. All of these can add significant fat kcal to the meal.
Finally, a low-fat or fat-free label does not provide you with a license to consume all the calories you desire. There will be consequences to your weight and your overall health. Common replacements for fat in many fat-free foods are refined carbohydrates and sugar. Too much of these ingredients can also cause health problems. Choose and consume wisely.
Key Takeaways
- Lipids include triglycerides, phospholipids, and sterols.
- Triglycerides, the most common lipid, comprise most body fat and are most fats and oils in food. They are made from fatty acids and glycerol.
- Fatty acids can vary based on the length of the carbon chain (short, medium, long), the number and location of double bonds (SFA, MUFA, PUFA, omega-3, omega-6), and the location of hydrogens around double bonds (cis or trans).
- The structure and length of a fatty acid determines whether it is solid or liquid at room temperature.
- Essential fatty acids cannot be synthesized by the body and must be included in the diet. Omega-3 and omega-6 fatty acids have opposing functions and must be consumed in proper balance to promote health.
- Hydrogenation is the process of stabilizing a polyunsaturated fatty acid by adding hydrogen ions. This provides a more stable molecule and increases stability and shelf life of foods. However, it also creates trans fats which are harmful to human health.
- Lipid digestion occurs primarily in the small intestine with enzymes called lipases. Lipids must be emulsified by bile from the liver and gallbladder prior to enzymatic breakdown. Several hormones are involved in the process including secretin and CCK.
- Short and medium chain fatty acids are absorbed directly into the blood, but long chain fatty acids must be absorbed into the larger lymphatic vessels.
- Lipids must be packaged as lipoproteins in order to be transported in the bloodstream. There are several different forms of lipoproteins. Chylomicrons transport lipids from the small intestine to the liver, VLDL/IDL transport lipids to body cells, LDL transports cholesterol in blood, and HDL clears LDL and brings it back to the liver.
- The primary role of fat is to provide a source of energy. It is the most energy dense of the macronutrients, containing 9 kcals/g. It promotes satiety, and adds smell, taste, and mouthfeel to foods.
- Excess energy from food is stored as adipose tissue (body fat). Body fat is critical for maintaining body temperature, cushioning vital organs, regulating hormones, transmitting nerve impulses, and storing memory. Lipids transport fat-soluble nutrients and phytochemicals and promote bioavailability of these compounds.
- The AMDR for adults is 20–35% of your total caloric intake. Saturated fat must be less than 10% of your total caloric intake, and lowering this to 7% may further reduce the risk of heart disease. Trans fat should be avoided.
- CVD are related to dietary fat consumption and obesity. To reduce risk factors associated with these diseases, eat more plants, don’t smoke, and exercise regularly.
- Dietary recommendations include consuming MUFA and PUFA that are liquid at room temperature and avoiding SFA and trans fats. Choose nuts, seeds, whole grains, legumes, and vegetables and fruits, fatty fish, lean meats and poultry, and low-fat dairy.
Portions of this chapter were taken from OER Sources listed below:
Jellum, L., Hitzeman, J., Krauss, M., Henderson, S., Harnden, T., Elsberry, C., & Ford, G. (2018). Principles of Nutrition Textbook, Second Edition. Nursing and Health Sciences Open Textbooks. 5. https://oer.galileo.usg.edu/health-textbooks/5
Tharalson, J. (2019). Nutri300:Nutrition. https://med.libretexts.org/Courses/Sacremento_City_College/SSC%3A_Nutri_300_(Tharalson)
Titchenal, A., Calabrese, A., Gibby, C., Revilla, M.K.F., & Meinke, W. (2018). Human Nutrition. University of Hawai’i at Manoa Food Science and Human Nutrition Program Open Textbook. https://pressbooks.oer.hawaii.edu
Zimmerman, M., & Snow, B. (2012). An Introduction to Nutrition, v. 1.0. https://2012books.lardbucket.org/books/an-introduction-to-nutrition/
Additional References:
- National Center for Complementary and Integrative Health. (2020, June 10). 7 things to know about omega-3 fatty acids. National Institutes of Health. https://www.nccih.nih.gov/health/tips/things-to-know-about-omega-fatty-acids
- Jacob, A. (2013). Balancing act. Today’s Dietitian, 15(4), 38. https://www.todaysdietitian.com/newarchives/040113p38.shtml
- World Health Organization. (2020). Countdown to 2023: WHO Report on Global Trans Fat Elimination 2020. https://apps.who.int/iris/bitstream/handle/10665/334170/9789240010178-eng.pdf
- United States Federal Drug Administration. (2018, September 9). Small entity compliance guide: Trans fatty acids in nutrition labeling, nutrient content claims, and health claims. Center for Food Safety and Applied Nutrition. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/small-entity-compliance-guide-trans-fatty-acids-nutrition-labeling-nutrient-content-claims-and#:~:text=Trans%20fatty%20acids%20should%20be,nearest%20gram%20above%205%20grams
- United States Federal Drug Administration. (2018, May 18). Final determination regarding partially hydrogenated oils (Removing trans fat). https://www.fda.gov/food/food-additives-petitions/final-determination-regarding-partially-hydrogenated-oils-removing-trans-fat)
- American Heart Association. (2017, March 23). Trans fats. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/trans-fat
- University of Wisconsin Health. (2019, August 22). Fat replacers in food. https://www.uwhealth.org/health/topic/special/fat-replacers-in-food/uq1419.html
- National Heart, Lung, and Blood Institute. (n.d.). Low-calorie, lower-fat alternative foods. National Institutes of Health. https://www.nhlbi.nih.gov/health/educational/lose_wt/eat/shop_lcal_fat.htm
- Murphy, S. L., Xu, J., Kochanek, K. D., & Arias, E. (2018, November). Mortality in the United States, 2017. NCHS Data Brief No. 328. Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db328.htm
- Centers for Disease Control and Prevention. (2019, December 9). Know your risk for heart disease. https://www.cdc.gov/heartdisease/risk_factors.htm
- Centers for Disease Control and Prevention. (2020, May 19). Heart attack symptoms, risk, and recovery. https://www.cdc.gov/heartdisease/heart_attack.htm
- American Heart Association. (2016, October 31). How high blood pressure is diagnosed. https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/how-high-blood-pressure-is-diagnosed
- Centers for Disease Control and Prevention. (2020, May 19). High blood pressure symptoms and causes. https://www.cdc.gov/bloodpressure/about.htm
- Centers for Disease Control and Prevention. (2020, April 7). Stroke. https://www.cdc.gov/stroke/
- American Heart Association. (2016). Health threats from high blood pressure. https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure
- National Heart, Lung, and Blood Institute. (n.d.). Blood cholesterol. National Institutes of Health. https://www.nhlbi.nih.gov/health-topics/blood-cholesterol
- National Heart, Lung, and Blood Institute. (n.d.) Metabolic Syndrome. National Institutes of Health. https://www.nhlbi.nih.gov/health/metabolic-syndrome
- National Heart, Lung, and Blood Institute. (n.d.). DASH Eating Plan. https://www.nhlbi.nih.gov/health-topics/dash-eating-plan
a fatty acid with no double bonds
a fatty acids with one C=C double bond in the carbon chain
a fatty acid with 2 or more C=C double bonds in the fatty acid chain
Adding hydrogen atoms to an unsaturated fatty acid which allows the double bonds to break and become single bonds. Used in food processing to extend shelf life and harden fats.
fatty acids that cannot be synthesized in adequate amounts by the body and must be consumed in the diet
Type of lipid made up of a glycerol backbone attached to three fatty acids; the most common form of lipid in the body and in food
The process that forms triglycerides from glycerol and fatty acids.
Form of lipid made up of two fatty acids attached to a hydrophilic head. Often used in cell membranes and emulsifiers
Substances that allow the mixing of water-based substances and oils
Form of lipid made up of several ringed structures.
Most well known sterol in the body important for cell membrane structure and the formation of substances like hormones and bile. Found only in animal foods in the diet.
digestive enzymes released from salivary glands that begins the digestion of lipids in infants
Digestive enzyme released from the stomach that begins the digestion of lipids in adults
Substance made in the liver, stored in the gallbladder. It emulsifies fats, allowing them to mix more readily with water-based enzymes for digestion
hormone released from the duodenum that initiates bile release from the gallbladder
hormone released from the duodenum that initiates release of pancreatic juices containing macronutrient-digesting enzymes and bicarbonate for neutralizing hydrochloric acid from the stomach
Lipid digesting enzyme released from the pancreas
Lipid transport molecule surrounded by bile salts allowing dietary lipids to be absorbed into the walls of the small intestine
Group of lipid transport molecules
lipoprotein that transports lipid from the small intestine into the lymph vessel for transport to the liver
lipoproteins made in the liver that transport fat from liver to the body cells
remains of VLDL after transport in the blood; contains cholesterol; will become LDL
Made in the liver from IDLs, transport cholesterol to the body from the liver
Lipoprotein made and secreted from the liver that travels through the blood, picks up LDL, and returns it to the liver. Often called "good" cholesterol
body fat
hormone released by fat cells; signals to the hypothalamus that eating is not required, often called the satiety hormone; helps regulate long term food intake
body fat centrally located around abdominal organs
body fat found under the skin
The amount of a substance that is absorbed, transported, and subsequently used in the body
non-nutritive chemical compounds found in the edible parts of plants that provide characteristics to the plant like color, taste, smell. They may also provide health benefits beyond the traditional nutrients
The recommended proprotion of a person's daily calories that should come from protein (10-35%), fat (20-35%), and carbohydrates (45-65%).
the sensation of being full
the psychological desire for food
characteristic that increases the risk of developing a disease
