Local Anesthesia
Step 1: Health history and physical assessment
Focus on past operative experiences with LA, wound management, suturing, etc., and allergies.
Physical assessment:
• circulation, sensation and movement distal and proximal to the wound
• 2-point discrimination
• sharp/soft discrimination
• pulses
• capillary refill
• range of motion and strength against resistance of all body parts surrounding the wound site
• pain
Step 2: Set up equipment, wash hands, don gloves
Step 3: Cleanse skin around operative site with chlorhexidine
Wound irrigation and debridement can be painful for the patient and may be better tolerated after the wound is anesthetized. Wound cleansing reduces the risk of sepsis to the wound site. Cleanse a wide area around the wound to prevent contamination of suture material and surgical instruments during the procedure.
Note that some antiseptics (i.e., chlorhexidine, iodine) are cytotoxic and damage fibroblasts essential to wound healing. Do not introduce antiseptic solution directly into the wound. The wound itself should be cleansed or debrided with sterile normal saline only. Alternative methods for wound debridement are below.
(a) Irrigation: Use an 18-gauge catheter attached to a 30 mL syringe. 10 PSI of irrigating pressure is needed to dislodge contaminants and bacteria, yet not damage tissue.
(b) Scrubbing: Use a sponge or a brush to remove embedded debris. Avoid soaps or detergents.
(c) Debridement: Remove retained debris and devitalized tissue by surgical excision to improve wound healing time and prevent disfigurement.
Step 4: Drape the wound
Step 5: Choose appropriate LA
(a) Xylocaine 1% or 2%
The maximum dose of Xylocaine 1% is 4.5 mg/kg (max 30 mL). Xylocaine is the most frequently used LA agent as side effects or allergies tend to be rare.
Xylocaine has an immediate onset of action and a duration of action of approximately three hours.
It is important to keep note of the total LA dose used if a large area must be anesthetized.
(b) Xylocaine 1% or 2% with Epinephrine
Only Xylocaine 1% with epinephrine should be used for scalp lacerations. Xylocaine with epinephrine must be avoided in areas where blood flow is minimized by the size and space; such as the nose, penis, fingers, ear, toes and skin flaps with minimal or compromised blood flow. The vasoconstriction effects of epinephrine can reduce blood flow to the area, which makes for easier visualization of the wound and also allows for a larger dose of Xylocaine to be used since systemic absorption is reduced.
Xylocaine with epinephrine is an alternative choice for scalp lacerations or other highly-vascular areas as the epinephrine can help reduce bleeding at the site.
Xylocaine with epinephrine should be avoided in grossly contaminated wounds because the vasoconstriction and reduced blood flow caused by the epinephrine could increase the risk of infection.
Step 6: Determine technique to be used
(a) Topical anesthesia
Topical anesthesia can provide sufficient anesthesia for wound cleansing and ease discomfort associated with local infiltration of anesthesia prior to suturing, and reduce distortion of the wound caused by infiltration of LA.
Use of topical LA in children can reduce pain and anxiety prior to infiltration of LA (if required).
(i) Apply a gauze pad soaked in a facility approved LA (e.g. 2% Xylocaine) to the wound or operative site and leave in place for 30 minutes.
(ii) Loosely cover the pad with an occlusive dressing or plastic wrap to prevent spread to other tissues or accidental dislodgment of the pad.
(b) Infiltration Anesthesia
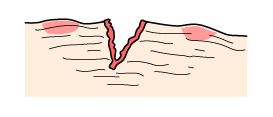
This technique should be avoided when the wound is grossly contaminated due to the risk of infection. Local infiltration involves the injection of the LA at the wound margins and/or directly into the line of incision. Injection through the edges of the wound can be less painful than injection through adjacent intact epidermis.
(i) Instill a few drops of anesthetic agent directly into the wound
(i) Place the needle directly into the exposed subcutaneous tissue
Start at one end of the laceration. Introduce the needle quickly through the wound margin rather than intact skin. The face of the bevel should be facing down and the needle parallel to the surface of the skin. Fully insert the needle to the hub. Injection of the anesthetic into the plane between the dermis and the subcutaneous tissue is less painful than direct dermal infiltration and offers less resistance.
Image retrieved from https://cosmotruth.wordpress.com/2013/07/08/skin-anatomy-101/
(ii) Aspirate for blood
(iii) Inject the LA
Inject a small amount of local anesthetic as you withdraw the needle.
Slow injection causes less discomfort as there is less distention of the surrounding tissue. Keeping the solution at slightly above body temperature (40° C) will also reduce discomfort.
(iv) Continue to anesthetize adjacent areas
(c) Field Block
(i) Draw an imaginary diamond around the lesion or laceration to be sutured
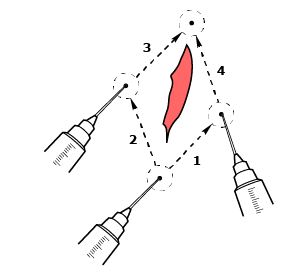
(ii) Insert the needle into the subcutaneous tissue through intact, clean skin and 1cm away from the margin of the lesion or wound site
Insertion of the needle 1 cm away allows for deep introduction of LA adjacent to the wound.
The needle should be inserted to approximately 2/3 of its length and along the “walls” as described above.
Injection of the anesthetic into the plane between the dermis and the subcutaneous tissue is less painful than direct dermal infiltration and offers less resistance.
Image retrieved from https://cosmotruth.wordpress.com/2013/07/08/skin-anatomy-101/
(iii) Aspirate for blood
(iv) Inject the LA
Slowly inject a small amount of local anesthetic as you withdraw the needle.
Slow injection causes less discomfort as there is less distention of the surrounding tissue. Keeping the solution at slightly above body temperature (40° C) will also reduce discomfort.
(iv) Repeat previous step until LA has been injected along all sides of the diamond around the lesion or wound site.
Step 7: Test sensation