Chapter Objectives
This chapter will enable you to:
-
- Discuss and identify the forms of epithelium found from the trachea to the alveoli
- Identify each subdivision of the respiratory tree from the trachea to the alveoli
- Identify pneumocyte type I cells, pneumocyte type II cells, and alveolar macrophages within the alveoli of the lung
Characteristics of the Conducting and Exchange Portions of the Respiratory System
The respiratory system is subdivided into conducting and exchange pathways. These pathways demonstrate structural specializations that facilitate (1) the conditioning of the air (warming, moistening, and cleaning) within the conducting pathway and (2) gas exchange with the cardiovascular system within the exchange pathway.
The conducting pathways of the respiratory system are those areas that are not anatomically designed for gas exchange. These pathways consist of the nasal cavities, pharynx, larynx, trachea, bronchi, and terminal bronchioles. (Only the histology of the conducting pathway from the trachea to the terminal bronchioles is discussed in this chapter.) The ability of these pathways to condition the air is accomplished by distinct histological characteristics:
- Hyaline cartilage is present, in varying forms, in all conducting pathways except bronchioles. Hyaline cartilage helps to maintain the patency of the conducting pathways.
- Seromucous glands are found in all conducting pathways except terminal bronchioles. These glands help to moisten and lubricate the conducting pathways and trap foreign particles.
- Mucous cells are found in all conducting pathways except terminal bronchioles. These cells produce mucus, which helps to moisten and lubricate the conducting pathways and trap foreign particles.
- Cilia are found within the conducting pathways wherever mucous cells are present. Cilia help to remove mucus produced by mucous cells.
- Elastic fibers are found in the subepithelial connective tissue of all conducting pathways except the nose. Elastic fibers help to maintain the patency of the conducting pathways.
- The conducting pathways demonstrate the classic respiratory epithelium (ciliated pseudostratified columnar) at every level except the bronchioles.
- All conducting pathways possess a high degree of vascularity.
The exchange portion of the respiratory system starts at the level of the respiratory bronchioles—the level at which alveoli make their first appearance. Alveoli are specialized for gas exchange. The shape of the squamous epithelium provides a large surface area and a thin diffusion barrier. The exchange portion of the respiratory system is marked by a high degree of vascularity. Three cell types are found within the exchange portion of the respiratory system:
- Pneumocyte Type I cells (also termed squamous alveolar cells or septal cells):
- Are squamous in shape and form a simple squamous epithelium, thereby providing a minimal diffusion barrier between the alveolus and surrounding capillaries
- Occupy approximately 95% of the alveolar surface
- Pneumocyte Type II cells (also termed great alveolar cells):
- Demonstrate an irregular cuboidal shape
- Occupy approximately 5% of the alveolar surface
- Produce surfactant
- Alveolar macrophages (dust cells):
- Are freely wandering phagocytic cells that are not part of the alveolar wall but are often found sitting on the alveolar surface
- Are derived from circulating monocytes
Trachea
Some histological slides of the trachea also contain a cross section of the esophagus. Scan the section at low power first and then proceed to a higher magnification after you have distinguished the trachea from the esophagus.
Figures 10-1 and 10-2 clearly demonstrate that the epithelium of the trachea is a ciliated, pseudostratified, columnar epithelium with mucous cells. (See sections on the Pseudostratified Ciliated Columnar Epithelium and Unicellular Exocrine Glands in Chapter 2.) The epithelium rests on a prominent connective tissue layer termed the lamina propria. This epithelium possesses three distinctively different cell types (not all of which are visible in this photomicrograph): mucous cells, tall ciliated cells, and short (stem) cells.
The lamina propria contains numerous elastic fibers that cannot be seen in standard hematoxylin and eosin (H & E) preparations. The submucosa is loose, irregular (areolar) connective tissue containing mixed tubuloacinar seromucous glands and adipose cells (see sections on Loose, Irregular [Areolar] Connective Tissue and Adipose Tissue in Chapter 3).
The framework and chief support of the trachea is composed of C-shaped hyaline cartilage (see section on Hyaline Cartilage in Chapter 4). Depending on the plane of section, the cartilage may not be in a complete C-shape. The posterior, open portions of the cartilage are joined by fibroelastic connective tissue and smooth muscle (see section on Smooth Muscle in Chapter 6).
Table 10-1: Histological Characteristics of the Respiratory System
| Region | Epithelium | Mucous Cells | Glands | Cartilage | Smooth Muscle | Elastic Fibers |
| Nasal cavity | Pseudostratified columnar* | Large number | Large number | Hyaline | None | None |
| Larynx | Pseudostratified columnar† |
Large number | Large number | Complex: hyaline and elastic | None | Yes |
| Trachea | Pseudostratified columnar |
Large number | Yes | C-shaped hyaline cartilage | Yes | Yes |
| Small bronchi | Pseudostratified columnar |
Few | Few | Plates and islands | Cross-spiral layers | Yes |
| Terminal bronchioles |
Simple low columnar or cuboidal; ciliated | None | None | None | Cross-spiral layers | Yes |
| Respiratory bronchioles |
Simple cuboidal, ciliated proximally, not distally | None | None | None | Cross-spiral layers | Yes |
| Alveolar ducts | Simple squamous, nonciliated | None | None | None | Yes‡ | Yes |
| Alveoli | Simple squamous (type I) or simple cuboidal (type II) | None | None | None | Yes‡ | Yes |
*Stratified squamous epithelium in regions of direct airflow or abrasion.
† Vestibule shows transition from stratified squamous epithelium with keratin to characteristic epithelium of the respiratory system.
‡ Concentrated at alveolar openings.
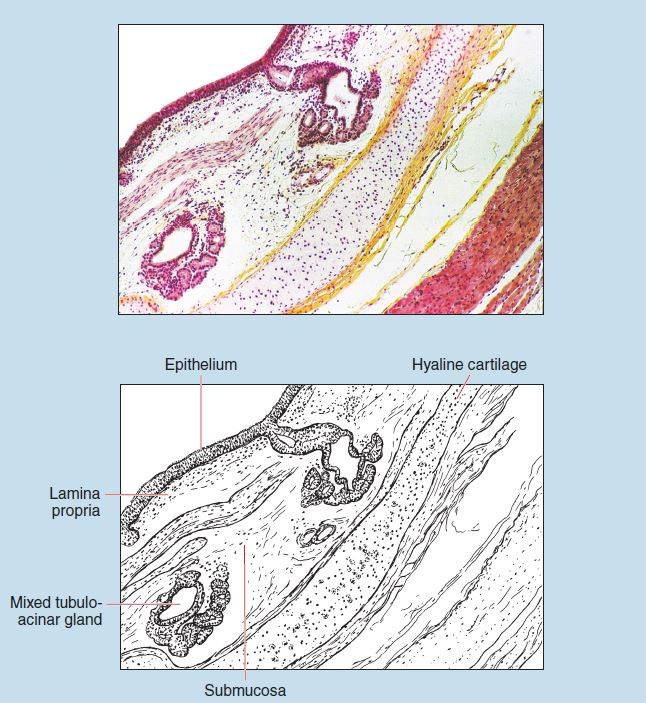
Figure 10-1 (25X): Trachea.
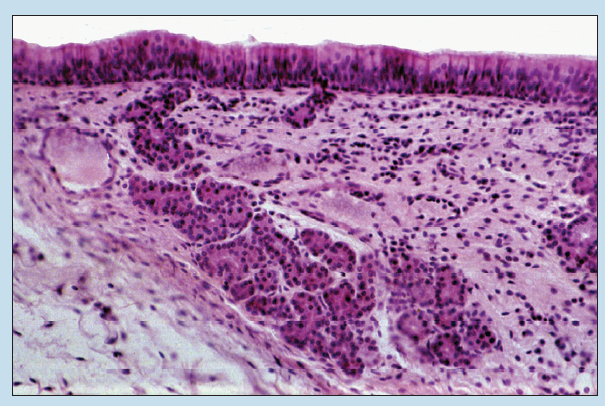
Figure 10-2 (50X): Trachea.
Lung
Bronchi
Figures 10-3 and 10-4 show a bronchus within a human lung. The surfaces of the lungs are covered with a serous membrane called the visceral pleura, which is continuous with the parietal pleura at the hilus. The visceral pleura may or may not be visible on your sections. It is not visible on either of these figures.
The main bronchus will divide into secondary bronchi after entering the lung. The hyaline cartilage of the larger bronchi will form complete rings as compared with the C-shaped cartilage seen in the trachea. In smaller bronchi, the rings give way to irregular plates and islands of hyaline cartilage.
The wall of a bronchus is continuous, and its epithelium is a typical respiratory epithelium: pseudostratified, columnar epithelium with cilia and mucous cells. Large bundles of smooth muscle will be seen intertwined with elastic fibers within the wall of the bronchus. Bronchial glands are present in the bronchial walls in numbers equal to or greater than those seen in the trachea. These bronchial glands may be serous, mucous, or seromucous in nature (see section on Epithelial Glands in Chapter 2).
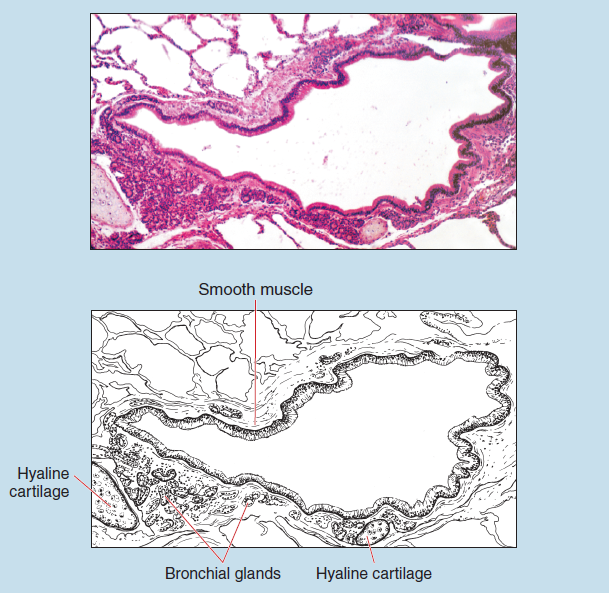
Figure 10-3 (25X): Bronchus.

Figure 10-4 (50X): Bronchus.
Terminal and Respiratory Bronchioles
Figure 10-5 illustrates the transition from a terminal bronchiole to a respiratory bronchiole. Terminal bronchioles are characterized by their continuous walls. The epithelium will change from a typical respiratory epithelium proximally to a simple columnar epithelium in the more distal segments, followed by a simple cuboidal epithelium in the most distal portions (see section on Simple Cuboidal Epithelia in Chapter 2). All of these epithelial variations possess cilia. The epithelium lacks mucous cells.
The lamina propria in a terminal bronchiole is rather thick, as is the amount of smooth muscle. Elastic fibers, which are not visible in H & E preparations, are found in higher proportions in terminal bronchioles than in bronchi. Cartilage and seromucous glands are absent from the walls of a terminal bronchiole.
The walls of respiratory bronchioles are discontinuous because of the presence of pulmonary alveoli in their walls. Between the alveoli, this subdivision of the respiratory system is lined by a simple cuboidal epithelium. This epithelium of a respiratory bronchiole is rather tall at the more proximal regions and considerably lower in height in the more distal portions. Cilia are present in the more proximal portions but will be absent in the distal portions.
Smooth muscle and elastic fibers are prominent in the walls of the respiratory bronchioles.
As was seen in terminal bronchioles, cartilage and seromucous glands are absent within the walls of a respiratory bronchiole.
A question to consider: What is the anatomical and physiological rationale for the presence of cilia in regions of the respiratory tree lacking in mucous cells and glands?
Alveoli
Figure 10-6 shows a respiratory bronchiole terminating at an alveolar duct, which in turn terminates in alveoli. The walls of an alveolar duct are formed by pulmonary sacs and alveoli. Only a few simple squamous to low cuboidal cells (see section on Simple Squamous Epithelia in Chapter 2) may be found in the walls between the alveoli. Smooth muscle cells are concentrated around the alveolar openings but are not visible in these sections. Reticular, elastic, and delicate collagenous fibers are also present but not visible.
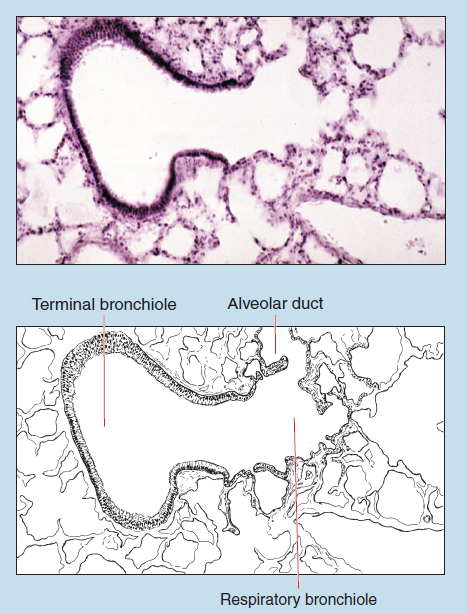
Figure 10-5 (50X): Transition from a terminal bronchiole to a respiratory bronchiole.
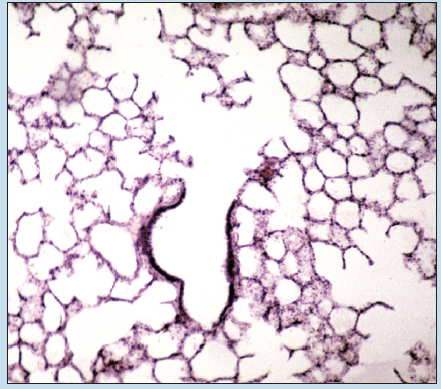
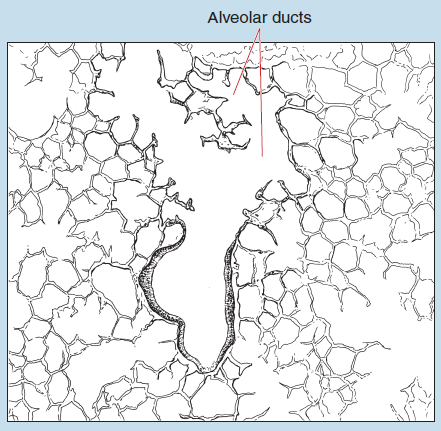
Figure 10-6 (25X): Alveolar duct.
The alveoli (Figure 10-7) are lined by pneumocyte type I cells (also termed squamous alveolar cells), pneumocyte type II cells (also termed great alveolar cells or septal cells), and alveolar macrophages (also termed dust cells). Alveolar macrophages are difficult to identify with the light microscope unless they have ingested foreign particles.
The rich capillary networks of the lungs are fed by pulmonary arteries, the larger of which are usually seen in close proximity to bronchi and bronchioles. The capillaries drain into small pulmonary veins that course through the connective tissue septa between lung lobules. The larger pulmonary arteries run along the bronchioles opposite the corresponding pulmonary veins. Bronchiolar arteries may also be seen in some of your slide preparations. They are typically smaller in diameter than pulmonary arteries. What is the function of each of these types of vessels?
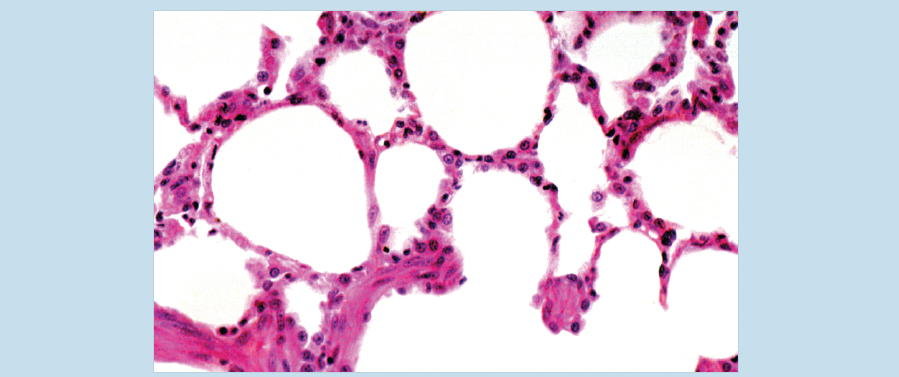
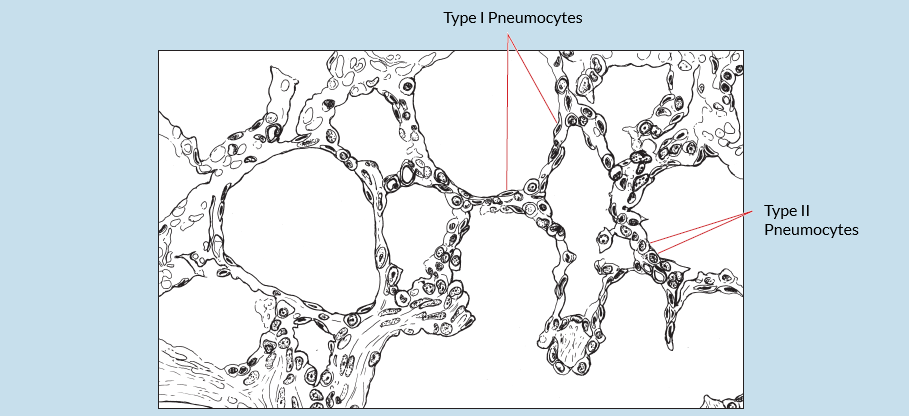
Figure 10-7 (100X): Pulmonary alveoll.
Commonly Misidentified Tissues
Artery and Small Bronchiole
At low or medium power a beginning student in histology may confuse a small bronchiole and a blood vessel, usually an artery. Therefore it is important to keep the following differences in mind:
Artery (Review Figures 8-6 to 8-8 in section on Muscular Arteries in Chapter 8)
-
- Presence of Red Blood Cells (RBCs) in lumen.
- Thin, convoluted layer of tissue lining lumen; simple squamous epithelium on connective tissue upon close examination
- Prominent outer layer (adventitia) composed of connective tissue
- Thick layer of smooth muscle
Small Bronchiole (Review Figure 10-5 in section on Terminal and Respiratory Bronchioles)
-
- Clear lumen
- Prominent folds in the thick epithelium lining wall of tubule; epithelium pseudostratified columnar with cilia and mucous cells upon close examination
- Thin layer of smooth muscle