Chapter Objectives
This chapter will enable you to identify the:
-
- Cell types of the adenohypophysis (anterior pituitary or pars distalis) and neurohypophysis (posterior pituitary or pars nervosa)
- Components and cell types of the thyroid and parathyroid glands
- Regions and cell types of the suprarenal cortex and suprarenal medulla
- Pancreatic islets (Islets of Langerhans) within the pancreas
- Components and cell types of the pineal gland
Characteristics of Endocrine Glands
An endocrine gland is defined as a ductless gland that releases its secretions directly onto the surface of the cell or directly into the lymphoid system, interstitial fluids, or bloodstream. Whether the endocrine gland constitutes only a small portion of the gland (as in the pancreas) or makes up the majority of the gland, all endocrine glands share several characteristics:
- The cells secreting the hormones possess either neural, epithelial, or epithelioid characteristics.
- All endocrine glands are richly vascularized.
- The glands either lack ducts or the ducts do not communicate with the endocrine portion of the organ.
Endocrine glands produce three major types of hormones: (1) steroids, (2) proteins or polypeptides, and (3) neurotransmitter substances. The ultrastructure of these cells will mirror the type of hormone produced. Although the ultrastructure of endocrine cells is not visible with the light microscope, it will affect the histological characteristics of the cells.
Steroid hormones are produced by endocrine cells that:
- Have an abundant smooth endoplasmic reticulum (SER), thereby causing the cytoplasm of the cells to stain acidophilically
- Have numerous mitochondria with tubular cristae, again causing the cytoplasm to stain acidophilically
- Contain lipid droplets within the cytoplasm. These droplets are dissolved during the fixation process, thereby making the cytoplasm of the cells stain lightly.
Protein and polypeptide hormones are produced by endocrine cells that:
- Have an abundant rough endoplasmic reticulum (RER) and Golgi apparatus. If these cells are actively synthesizing hormones, the cytoplasm will stain predominantly basophilic, owing to the large amounts of tRNA, mRNA, and ribosomal RNA within the cytoplasm.
- Frequently possess membrane-bound secretory granules, thereby giving the cytoplasm a slightly granular appearance.
Neurotransmitter substances are produced by endocrine cells that:
- Are derived from embryonic central nervous system tissues and therefore typically retain many of the histological characteristics seen in nervous tissue.
Pituitary Gland (Hypophysis)
The pituitary gland (hypophysis) is divided into an adenohypophysis (anterior lobe) and the neurohypophysis (posterior lobe). The adenohypophysis is further subdivided into the pars distalis (also termed the pars anterior), pars intermedia, and pars tuberalis, and the neurohypophysis is subdivided into the infundibulum and the neural lobe (posterior lobe). We will confine our histological examination of the pituitary gland to the pars distalis of the adenohypophysis and the neural lobe of the neurohypophysis.
Pars Distalis of the Adenohypophysis
The pars distalis (anterior lobe) of the adenohypophysis of the pituitary gland possesses a parenchyma of anastomosing cords of cells separated from sinusoidal capillaries by a small amount of irregular connective tissue (Figures 13-1 and 13-2). The parenchymal cells of the adenohypophysis are separated into two categories: chromophils and chromophobes (Figure 13-2). The granules within the cytoplasm of chromophils will stain with either eosin or hematoxylin, whereas those within chromophobes will not react with either stain or will do so very poorly.
Chromophils are further subdivided into acidophils (alpha cells) and basophils (beta cells) (Figure 13-2). Cytoplasmic granules determine the staining properties of the chromophils. Eosin will stain the granules of the acidophils; the granules of the basophils will stain poorly, or not at all, with hematoxylin. They will, however, stain quite well with aniline blue or Masson’s trichrome stains. Basophils on these photomicrographs stain lightly basophilic.
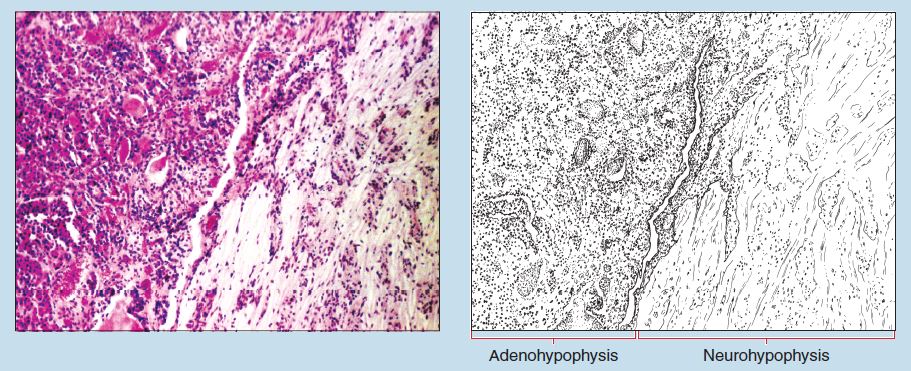
Figure 13-1 (25X): Pars distalis of the adenohypophysis (anterior lobe) of the pituitary.
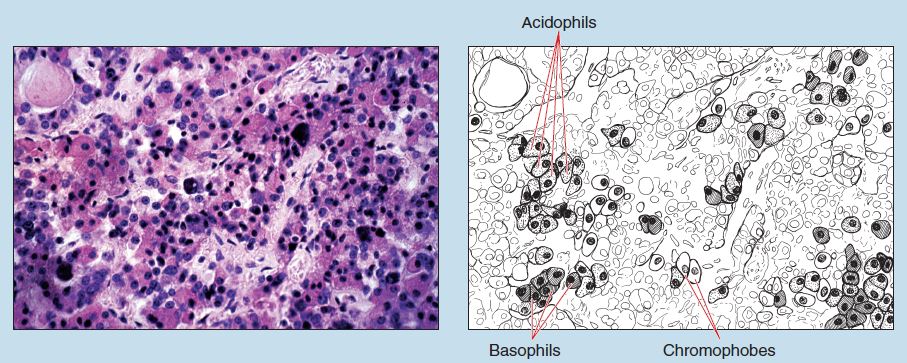 Figure 13-2 (100X): Pars distalis of the adenohypophysis (anterior lobe) of the pituitary.
Figure 13-2 (100X): Pars distalis of the adenohypophysis (anterior lobe) of the pituitary.
Neural Lobe of the Neurohypophysis
The neural lobe (pars nervosa) contains unmyelinated axons from the hypothalamo-hypophysial tract, blood vasculature, and pituicytes. In routine hematoxylin and eosin sections (Figure 13-3), the neural lobe is quite bland in that the individual axons cannot be easily distinguished, and the pituicytes resemble neuroglial cells in many ways (see sections on the Spinal Cord and Cerebral Cortex in Chapter 7).
Pituicytes (Figures 13-3 and 13-4) are small cells with ramifying processes that cannot be observed with the light microscope. Their nuclei are either round or oval and possess fine chromatin. In routine histological preparations, the cytoplasm of these cells is faintly visible.
Within the neural lobe, neurosecretory bodies (also termed Herring Bodies) may also be seen (Figure 13-4). These are large accumulations of neurosecretory material and degradative products within individual axons and nerve endings. Neurosecretory bodies appear as brown or reddish-brown granules between the pituicytes of the posterior pituitary.
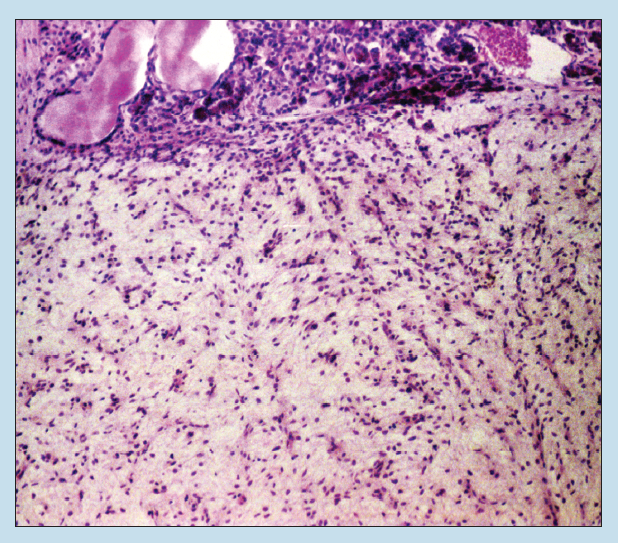
Figure 13-3 (25X): Neural lobe (pars nervosa) of the neurohypophysis (posterior lobe) of the pituitary.
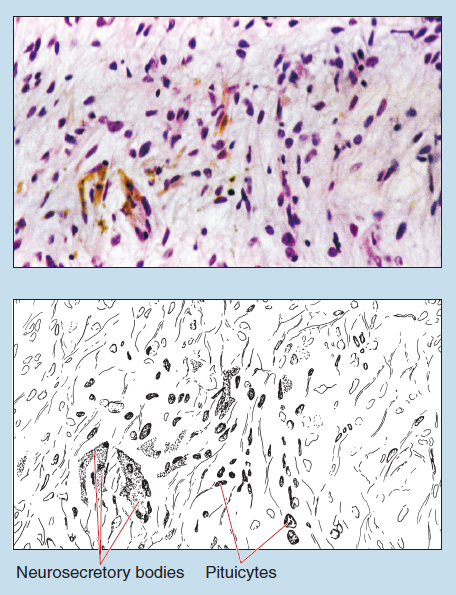
Figure 13-4 (100X): Neural lobe (pars nervosa) of the neurohypophysis (posterior lobe) of the pituitary.
Thyroid and Parathyroid Glands
Thyroid Gland
A true connective tissue capsule composed of fibroelastic connective tissue surrounds the thyroid gland (Figure 13-5). Delicate trabeculae and septa (which are not visible on this photomicrograph) radiate inward from the capsule.
The structural unit of the thyroid, the follicle, has an irregular spherical shape (Figures 13-5 and 13-6). The follicle contains an internal follicular cavity filled with a gel-like material termed colloid. The T thyrocytes of the follicular epithelium are simple cuboidal epithelial cells (see section on Simple Cuboidal Epithelia in Chapter 2), and their height will vary slightly, depending on their synthetic activity.
In this photomicrograph, the intercellular boundaries between the T thyrocytes are distinct. The cells possess a rounded nucleus within a lightly basophilic cytoplasm (Figure 13-6). The staining properties of the follicular epithelium will range from lightly basophilic for inactive squamous or cuboidal cells to deeply basophilic for cuboidal to columnar follicular epithelium with a high synthetic activity. The apical ends of the cells possess microvilli that may be visible under oil immersion.
C thyrocytes (parafollicular cells, “C” cells, clear cells, or calcitonin cells) should be visible on your section (Figure 13-6). These cells may be found either singly or in groups and may be found in the wall of the follicle or in the interfollicular space. Generally, they are larger than the T thyrocytes and stain very lightly. They are relatively sparse in humans. Why?
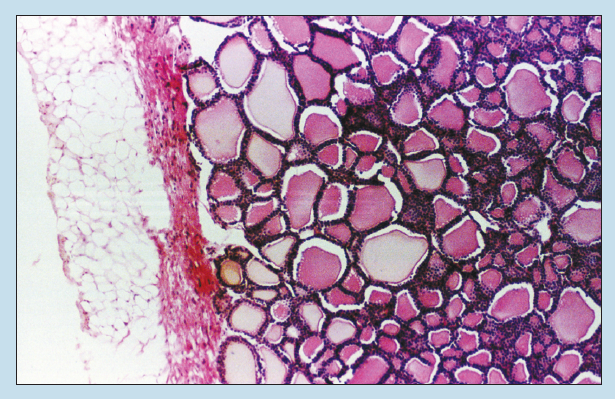
Figure 13-5 (25X): Thyroid gland.
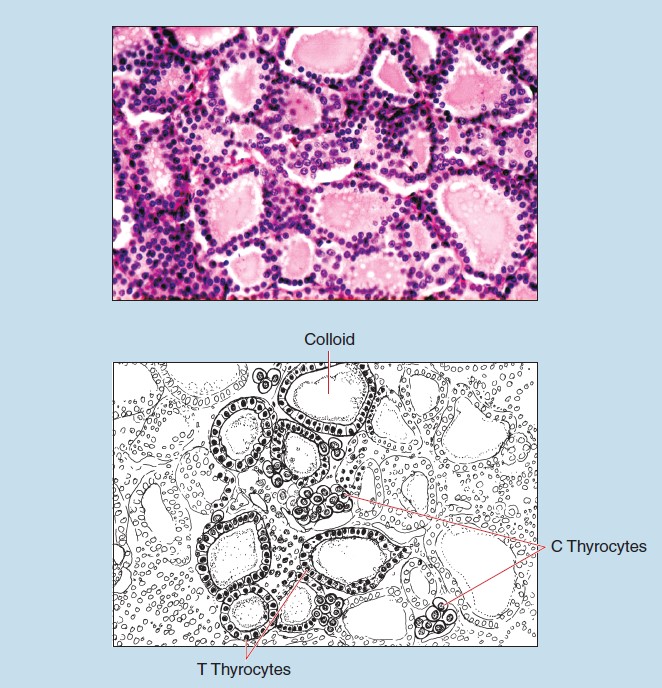
Figure 13-6 (100X): Thyroid gland.
Parathyroid Gland
The parathyroid gland possesses a delicate connective tissue capsule with slight septa radiating inward. These septa separate the parenchyma into anastomosing cords, a feature that becomes more obvious in the adult because of the increase amount of adipose tissue within the gland (Figure 13-7) (see section on White [unilocular] Adipose Tissue in Chapter 3).
The parenchyma of the parathyroid gland is composed of three cell types: parathyroid cells (also called chief cells or principle cells), oxyphil cells, and transition cells (Figure 13-8).
Parathyroid cells are constant in number and occurrence. They are polyhedral in shape, possess sparse cytoplasm, and have a rounded nucleus with loosely arranged chromatin. They possess a pale, slightly eosinophilic cytoplasm.
Oxyphil cells do not appear until after the first decade of life and are not abundant until puberty. They may be found scattered throughout the gland and occur either singly or in clumps. They are larger than parathyroid cells, with smaller yet darkerstaining nuclei. The cytoplasm stains deeply with eosin.
Transitional cells possess cytological characteristics intermediate between those of the parathyroid and oxyphil cells and cannot be easily distinguished with the light microscope.
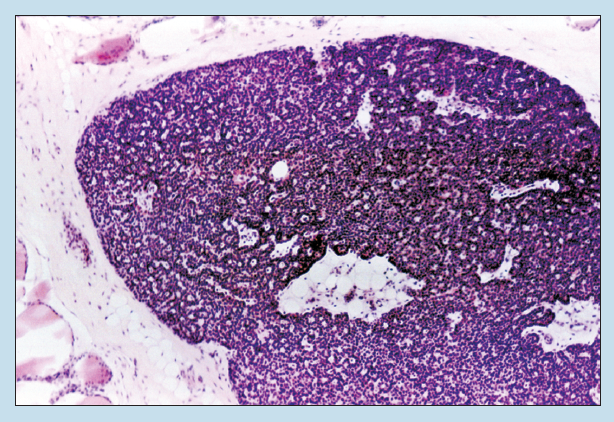
Figure 13-7 (25X): Parathyroid gland.
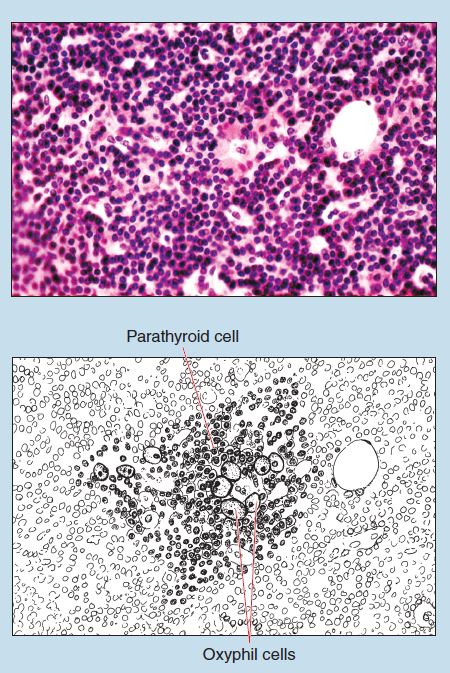
Figure 13-8 (100X): Parathyroid gland.
Suprarenal (Adrenal) Gland
Suprarenal Cortex
The suprarenal glands (Figure 13-9) (also called the adrenal glands) are actually composite glands, being composed of a cortex and a medulla, each of which has a different embryonic origin and produces different secretions. The cortex originates from mesodermal cells of the nephrogenic ridge and produces steroids; the medulla has its embryonic origin in the neural crest and produces epinephrine and norepinephrine. Therefore the appearance and staining qualities of these two sections will be quite different.
The suprarenal gland is covered with a thick capsule, composed chiefly of collagen (Figure 13-9). Delicate trabeculae extend inward from the capsule. The arrangement into cortex and medulla is not uniform in human suprarenal glands but is quite distinct in the suprarenal glands of many animals.
Figure 13-10 shows the outer portion of the suprarenal cortex, which is divided into three zones. The outermost zone is relatively thin and is termed the zona glomerulosa; the cells of this zone are arranged into ovoid groups. Their cytoplasm contains lipid droplets that are dissolved during the fixation process, and therefore they may appear as vacuoles. The nuclei stain darkly.
The zona fasciculata is the largest of the three zones, and the cells are arranged into long, parallel cords that are one to two cells thick and course perpendicular to the capsule. The cells are cuboidal or polyhedral in shape and may possess two nuclei. Because of a high concentration of lipid droplets within the cytoplasm, these cells stain lightly and have a vacuolated (spongy) appearance. These cells are sometimes referred to as spongiocytes.
The innermost zone is the zona reticularis and is composed of a network of cords (Figure 13-11). These cells are considerably smaller than those of the zona fasciculata, stain more acidophilic (Figure 13-10), and frequently have nuclei that stain more deeply. Lipofuscin granules may be evident within the cytoplasm of these cells when viewed with the oil-immersion lens.
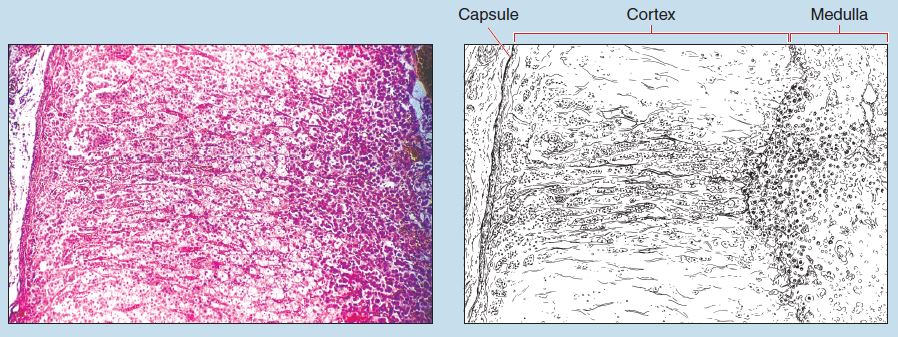
Figure 13-9 (25X): Suprarenal gland.
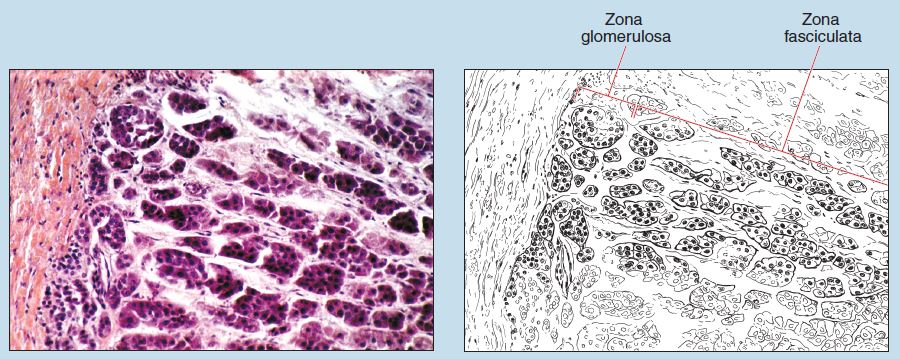
Figure 13-10 (50X): Suprarenal gland.
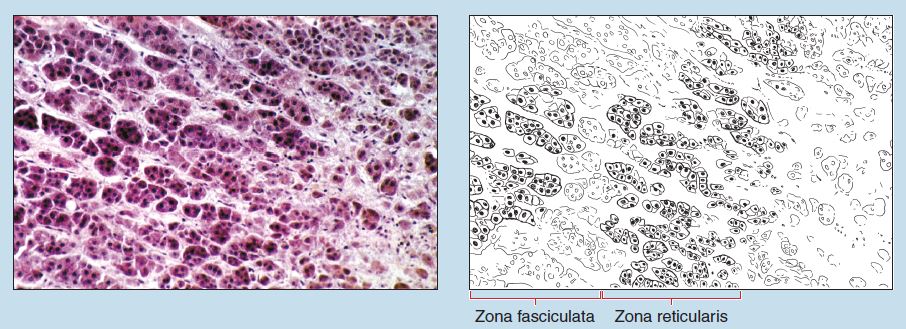
Figure 13-11 (50X): Suprarenal gland.
Suprarenal Medulla
The cells of the medulla are arranged into anastomosing cords and are termed chromaffin cells (Figure 13-12). They are polygonal to columnar in shape and contain fine cytoplasmic granules that may be seen when viewed with the oil-immersion lens.
Endocrine Pancreas/Pancreatic Islets
The pancreas is a composite gland with both exocrine and endocrine functions. The endocrine pancreas is composed of the pancreatic islets (also termed Islets of Langerhans). These cells are in the form of a spherical mass of pale staining cells arranged into irregularly anastomosing cords (Figure 13-13). Numerous capillaries (see section on Capillaries in Chapter 8) are found between the cells.
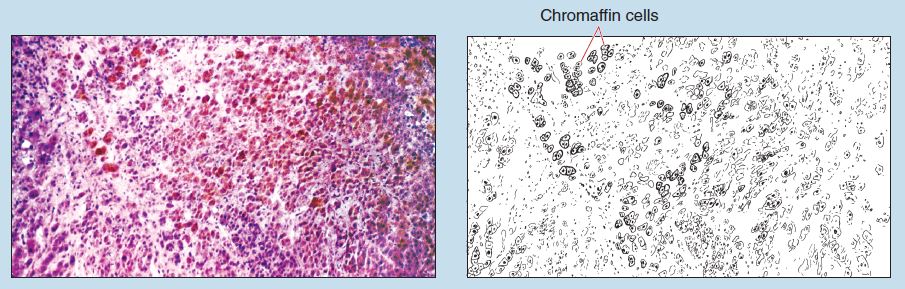
Figure 13-12 (50X): Suprarenal gland.
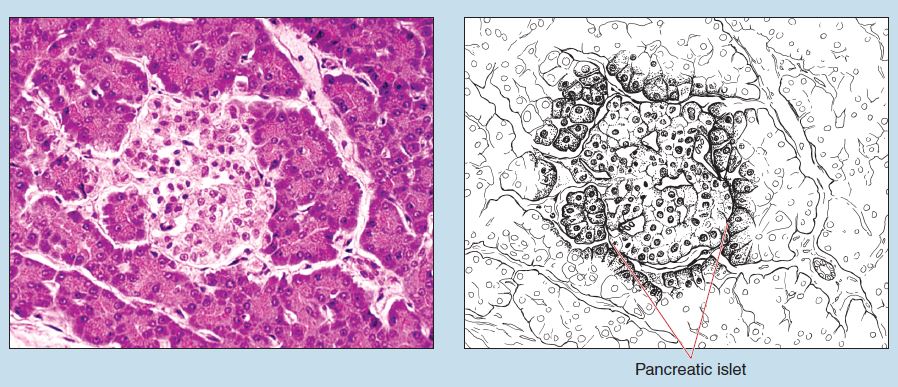
Figure 13-13 (100X): Pancreatic islet (Islet of Langerhans) of the pancreas.
Pineal Gland
The pineal gland (pineal body) is an endocrine or neuroendocrine gland attached to the roof of the diencephalon at the posterior wall of the third ventricle, near the center of the brain. The pia mater may be seen on the right side of Figure 13-14. Acervulus (also termed corpora arenacea or brain sand), which is a major identification feature of the pineal gland, may be seen in this photomicrograph. The number of corpora arenacea within the pineal gland increases with age. These structures appear to be calcium phosphate and calcium carbonate precipitates found on carrier proteins that have been released by exocytosis.
The pineal gland contains two cell types: pinealocytes and astrocytes of the pineal gland (also termed interstitial glial cells) (Figure 13-15). Pinealocytes are arranged into cords or clumps that extend deep into the gland. They have a prominent nucleus that often appears infolded. One or two prominent nucleoli may be evident within the nucleus.
Astrocytes of the pineal gland make up approximately 5% of the cells within the pineal gland. These cells have cytological and staining characteristics similar to other glial cells within the central nervous system.
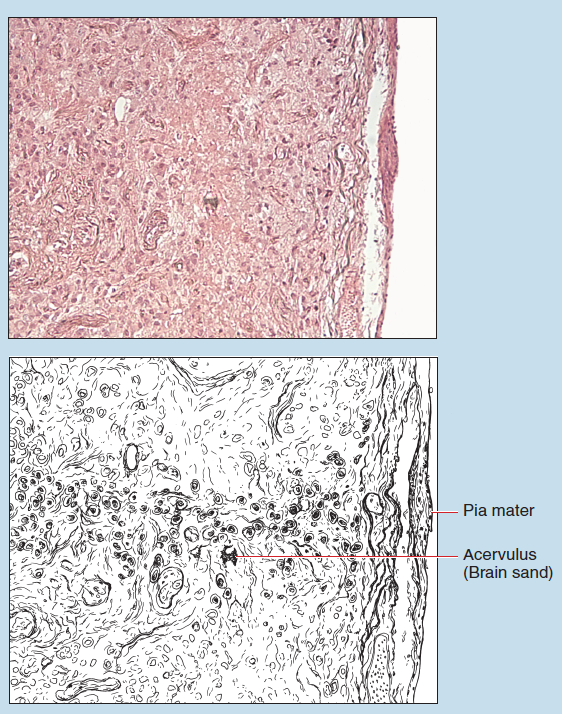
Figure 13-14 (35X): Pineal gland.
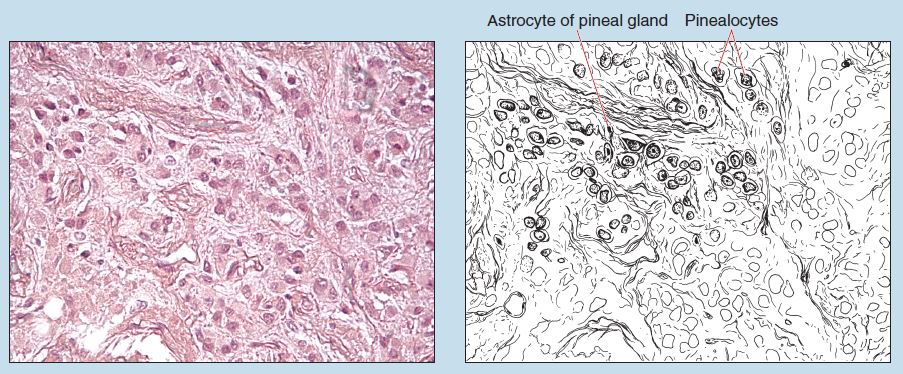
Figure 13-15 (70X): Pineal gland.
Commonly Misidentified Tissues
Parathyroid, Thymus, Lymph Node, and Spleen
Although the various endocrine glands are easy to differentiate, you may encounter difficulty distinguishing between the parathyroid gland and various glands of the lymphoid system. Therefore, keep the following histological characteristics in mind in order to differentiate between these organs.
Parathyroid Gland (Review Figures 13-7 and 13-8 in section on the Parathyroid Gland)
-
- Differential staining of the cells within the gland, owing to the presence of oxyphil and parathyroid cells
- Cells arranged into cords
- Prominent capillary bed without sinuses
- Very thin capsule
Thymus Gland (Review Figures 11-10 to 11-13 in section on the Thymus in Chapter 11)
-
- Arrangement into cortex and medulla
- Thymic (Hassal’s) corpuscles present within the medulla
- Cells within gland possess uniform staining qualities.
- Very thin capsule
Lymph Node (Review Figure 11-6 to 11-9 in section on the Lymph Nodes in Chapter 11)
-
- Lymphoid nodules with germinal centers are present.
- Medullary sinuses are prominent.
- Cells of the cortex are not arranged into cords.
- Capsule is thicker than that of endocrine glands but thinner than that of spleen.
- There are definitive subcapsular and paratrabecular spaces.
Spleen (Review Figures 11-14 to 11-18 in section on the Spleen in Chapter 11)
-
- Lymphoid nodules with germinal centers present
- Central arteries present within germinal centers
- Capsule thicker than that of lymph node
- Differentiation into red and white pulp
- No cortex or medulla
