Chapter Objectives:
This chapter will enable you to:
1. Differentiate among the various cell shapes seen in epithelial tissue.
2. Differentiate among simple, stratified, pseudostratified, and transitional epithelia.
3. Understand the composition of a basal lamina.
4. Be able to identify goblet cells and mucous cells.
5. Understand the various types of glands formed by epithelial tissue.
Characteristics of Epithelial Tissue
Epithelial tissue is one of the four basic tissues of the body. The others are connective, muscular, and nervous tissue. Epithelial tissue lines all internal cavities and passageways of the human body and covers all exposed surfaces.
All epithelial tissues share the following common and important characteristics:
- Free surface: Epithelial tissue always has an apical surface or a free edge.
- Arranged into sheets or layers: All epithelial tissue is composed of a sheet of cells one or more layers thick.
- Cellularity: Epithelial tissue is composed almost entirely of cells bound closely together by specialized junctions. As a result, epithelial tissue has little or no intercellular space.
- Polarity: Because many epithelial tissues are involved in some form of cellular transport, epithelial tissue has polarity. In other words, epithelial cells have a distinct top and bottom, with cellular specializations and intracellular organelles arranged accordingly.
- Avascularity: Epithelial tissue lacks blood vessels. As a result, all cellular nutrients must be delivered and all cellular
wastes must be removed via diffusion. - Attachment: All epithelial tissues are firmly anchored to an underlying fibrous basal lamina that has been secreted by
the overlying epithelium. - Regeneration: Epithelial tissue is continually damaged or lost at the exposed internal and external surfaces of the body. These cells are continually replaced through mitosis of stem cells found within the epithelium.
Classification of Epithelial Tissues
Epithelial tissue is classified according to (1) the number of layers making up the epithelial sheet or gland, and (2) the shape of the most superficial layer of these cells. Epithelial cells are categorized into one of the following three shapes:
- Squamous: When viewed from above, squamosal epithelial cells are described as appearing “scale-like” or like “sunny-side up” fried eggs. The thickness of the cytoplasm of these cells is usually too thin to be seen when viewed from the side with a light microscope. However, when the lateral cytoplasm can be seen, the nucleus of this cell type is often observed to bulge outward from the thin outline of the cell.
- Cuboidal: These cells are approximately equal in height and width. The nucleus of this cell type typically is positioned centrally within the cell.
- Columnar: This type of epithelial cell is taller than it is wide. The nucleus is usually located in the basal one third of the cell. However, some specialized columnar cells have an apically located nucleus.
As you examine the shapes of epithelial cells, note that the shape of the nucleus parallels that of the cell. In other words, the nuclei of squamous epithelial cells will often be attenuated and flattened, while those of cuboidal or columnar cells tend to be rounder.
In addition to cell shape, epithelial tissue is classified according to the number of layers present. Epithelial tissue may be:
- Simple: A single layer of epithelial cells in which all cells reach the underlying connective tissue (termed the basal lamina).
- Stratified: An epithelium composed of multiple layers of epithelial cells. In a stratified epithelium, only the cells of the basal layer reach the basal lamina, and only the most superficial layer of cells has a free surface.
- Pseudostratified: A single layer of epithelial cells in which the height of the cells varies considerably. In this type of epithelium, all cells reach the basal lamina, but not all cells reach the free surface. Because of the varying height of the cells and corresponding nucleus placement, the epithelium gives the appearance of being stratified.
- Transitional: This epithelium is characteristic of the urinary system. As the urinary tract organ stretches or relaxes, the cells of this epithelium will change shape, thereby giving the impression that the epithelium has changed from a multiple-layer to a single-layer arrangement.
Functions of Epithelial Tissue
Epithelial tissue serves a variety of functions, including secretion, absorption, and transport. In order to accomplish these functions, epithelial tissue will be found in the form of either sheets or glands. In addition, these sheets and glands will be composed of varying types of epithelial cells. In order to identify epithelial tissue, you must become familiar with the individual characteristics and components of the various types of epithelia. In this chapter, we will progress from identifying the varying cell shapes to identifying the layering of epithelial tissue. Finally, we will look at the processes used in the identification of the different types of epithelial cells.
Epithelial Sheets
Epithelial sheets are continuous sheets of cells that are joined by specialized intercellular junctions that cannot be seen with the light microscope. These sheets vary in thickness, ranging from one layer to multiple layers. The epithelial cells are attached to the underlying connective tissue by a basal lamina. A basal lamina is composed of two layers. (Neither of these sub-layers of the basal lamina can be identified with the light microscope.) The most superficial layer of the basal lamina is called the clear layer (lamina lucida) and is secreted by the epithelial tissue. The deeper layer is the dense layer (lamina densa), secreted by the underlying connective tissue. The structural organization of the clear layer is dominated by large, coarse collagenous fibers, microfilaments, and glycoproteins; it serves as a diffusion barrier to proteins and other large macromolecules and contributes to the strength of the basal lamina.
Often the term basement membrane will be encountered in histological studies. In some multilayered epithelia, such as the stratified squamous epithelium of the skin, the basal lamina is anchored to underlying connective tissue by a series of anchoring collagenous fibrils. The proper use of the term basement membrane pertains only to the basal lamina and this layer of anchoring collagen fibers associated with some forms of multilayered epithelia.
Simple Epithelia
Simple Columnar Epithelium (Duodenum)
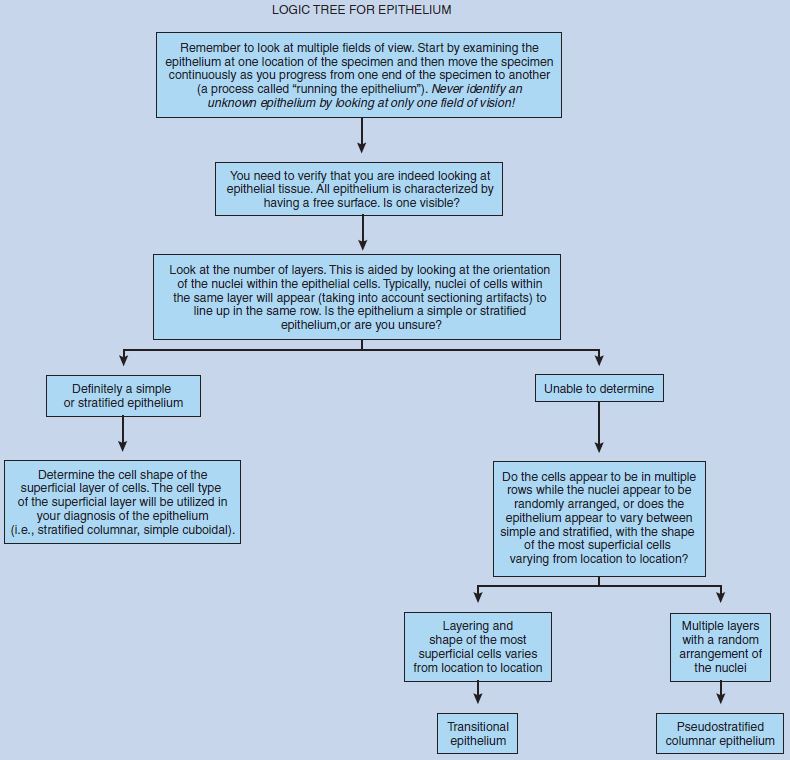
These photomicrographs are of a transverse section of the duodenum of the small intestine. First examine the specimen at low power (Figure 2-1) and then progress to higher magnifications.
The innermost layer of the small intestine is the mucosa, which is thrown into finger-like projections termed villi. These structures increase the absorptive and secretory surface area of the duodenum. The lumen of the organ is at the right of the figure. Note that the lumen appears to be filled with circular segments of villi. This is an excellent example of a sectioning artifact. As the intestinal villi twist and turn, the plane of section will vary from longitudinal sections to cross sections—hence the varied appearance of the villi seen in this section.
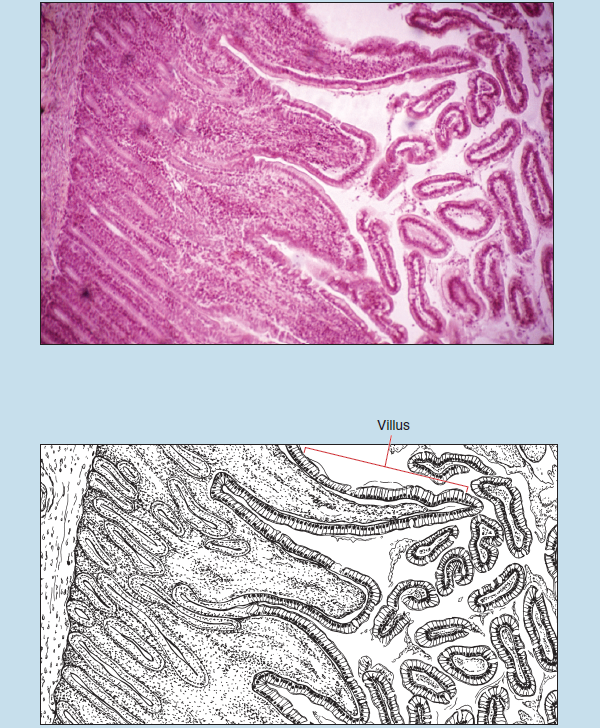
Figure 2-1 (25X): Villi of the duodenum of the small intestine.
As you progress from low to medium (Figure 2-2) to high-dry (Figure 2-3), note that the epithelial layer on the villi is a simple columnar epithelium. The tissue beneath the epithelium contains a variety of cell types, the nuclei of which give the region a granular appearance at low power.
As you examine the simple columnar epithelium, note the following:
- These cells are taller than wide, and all of the basal surfaces of the cells contact the basal lamina.
- The nucleus of this type of epithelium is typically found in the basal one third of the cell. In addition, the nuclei of a simple columnar epithelium are arranged in such a way that they are all at approximately the same level.
Note the presence of a fixation artifact in these two photomicrographs. This artifact is due to shrinkage of the specimen during fixation and gives the appearance that the epithelium is pulled away from the underlying connective tissue.
Figure 2-3 is a photomicrograph taken using the high-dry objective. Note the dark line at the free surface of the epithelium. This represents a cellular modification, termed the microvillus border, which serves to increase the surface area of the cell’s apical surface.
The basal lamina, although difficult to see, is visible as a thin, fibrous line at the base of the cells. Do not confuse it with the elongated cells in the tissue deep to the epithelium.
Throughout the epithelium you see small spherical or flask-shaped “holes.” These spaces are actually unicellular glands, termed goblet cells. Goblet cells secrete a substance termed mucinogen. Goblet cells have a clear or hollow appearance as a result of the dissolution of mucinogen during the histological processing.
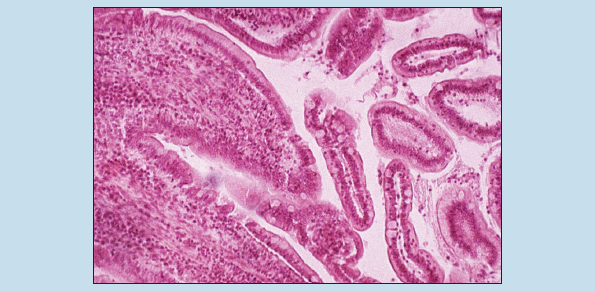 Figure 2-2 (50X): Simple columnar epithelium of duodenal villi.
Figure 2-2 (50X): Simple columnar epithelium of duodenal villi.
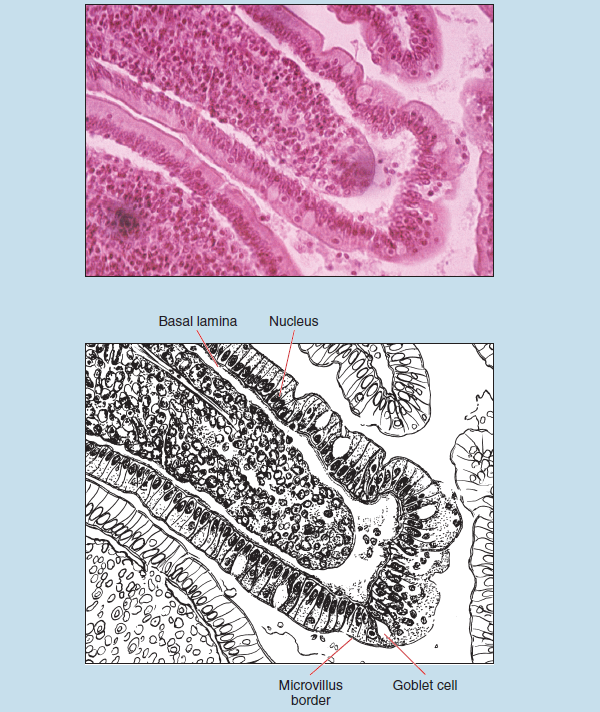 Figure 2-3 (100X): Simple columnar epithelium of duodenal villi.
Figure 2-3 (100X): Simple columnar epithelium of duodenal villi.
Simple Cuboidal and Simple Squamous Epithelia (Renal Medulla)
Figures 2-4 and 2-5 were taken from the medulla of the kidney. The medullary region of the kidney is composed of a large number of tubules: descending limbs of the proximal convoluted tubule, nephron loops (loops of Henle), and the ascending limbs of the distal convoluted tubules. The vasa recta of the renal vasculature is also present within the medulla. All of these structures have a simple epithelium, ranging from simple squamous to simple cuboidal. As discussed earlier (see Classification of Epithelial Tissues), simple cuboidal epithelial cells are approximately equal in height and width. A simple squamous epithelium, in contrast, is composed of attenuated cells, the nucleus of which often bulges outward from the thin outline of the cell.
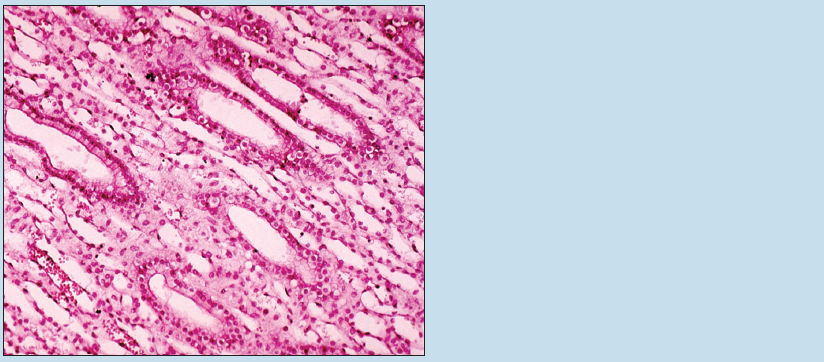 Figure 2-4 (50X): Simple cuboidal and simple squamous epithelium of the renal medulla.
Figure 2-4 (50X): Simple cuboidal and simple squamous epithelium of the renal medulla.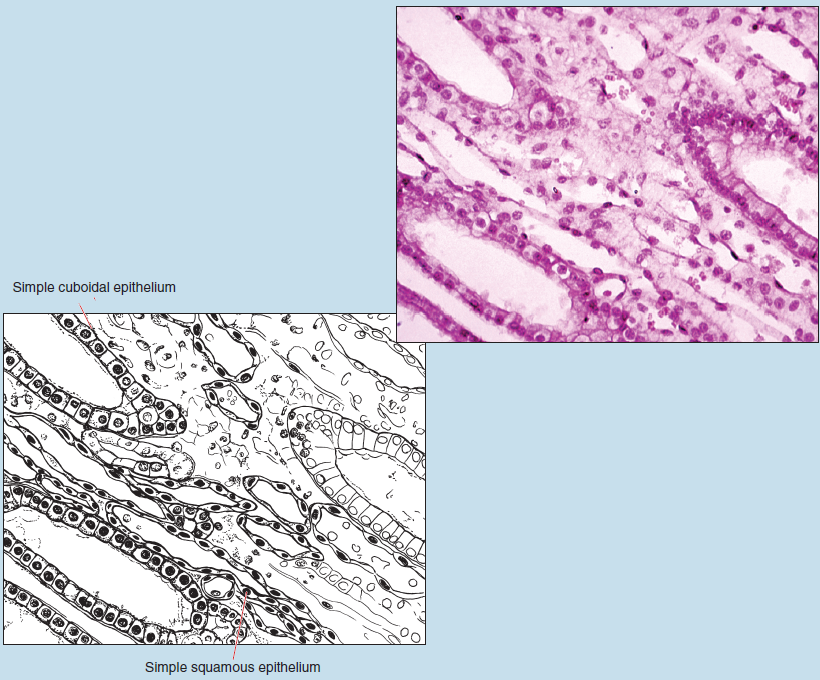 Figure 2-5 (100X): Simple cuboidal and simple squamous epithelium of the renal medulla.
Figure 2-5 (100X): Simple cuboidal and simple squamous epithelium of the renal medulla.
Stratified Epithelia
A stratified epithelium is composed of two or more layers of epithelial cells. The cells of the uppermost layer of a stratified epithelium do not reach the basal lamina but do reach the luminal surface. In contrast, those of the lowest layer do not reach the surface but do contact the underlying basal lamina. The classification of a stratified epithelium is based only on the appearance of the most superficial layer of cells.
Stratified Squamous Epithelium (Mucosal Type) (Esophagus)
Nonkeratinized, stratified squamous epithelium (mucosal type) is found on structures of the body that are moist and subjected to significant abrasion, such as those found in the esophagus and vaginal cavity. These photomicrographs demonstrate the non-keratinized, stratified squamous epithelium (mucosal type) found in the esophagus.
As you progress from low power (Figure 2-6), to medium power (Figure 2-7), and finally to high-dry (Figure 2-8), you will note the following in these photomicrographs:
- The epithelium is composed of multiple layers, thereby making it a stratified epithelium.
- The nuclei of the cells in this epithelium appear to be “regularly arranged;” that is, they appear to be arranged into distinct layers.
- Although the cells of the deepest layers of the epithelium are cuboidal in shape, the superficial layer of cells is composed of squamous cells, thereby classifying this epithelium as stratified squamous.
Deep to the epithelium are the basal lamina and a loose layer of connective tissue, termed the lamina propria, which may or may not be visible in your preparation.
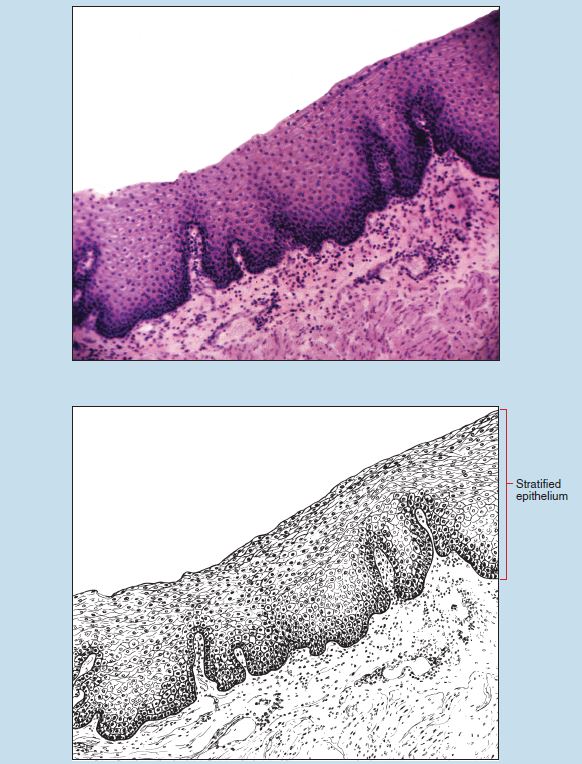 Figure 2-6 (25X): Stratified squamous epithelium of the esophagus.
Figure 2-6 (25X): Stratified squamous epithelium of the esophagus.
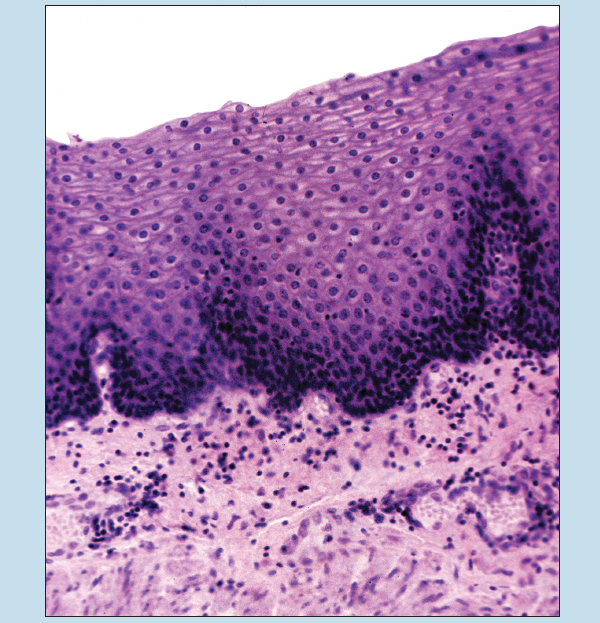 Figure 2-7 (50X): Stratified squamous epithelium of the esophagus.
Figure 2-7 (50X): Stratified squamous epithelium of the esophagus.
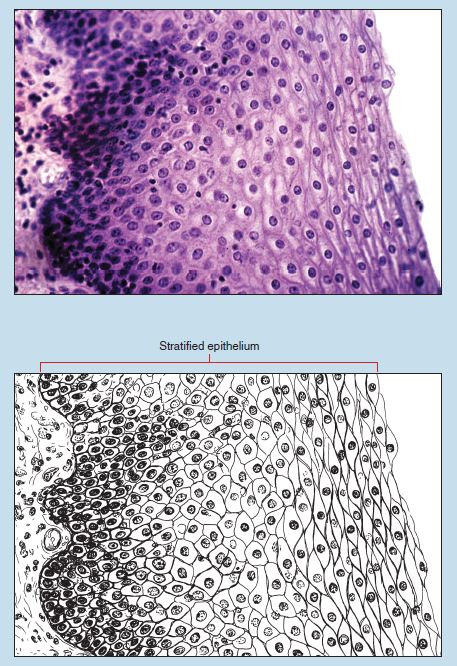
Figure 2-8 (100X): Stratified squamous epithelium of the esophagus.
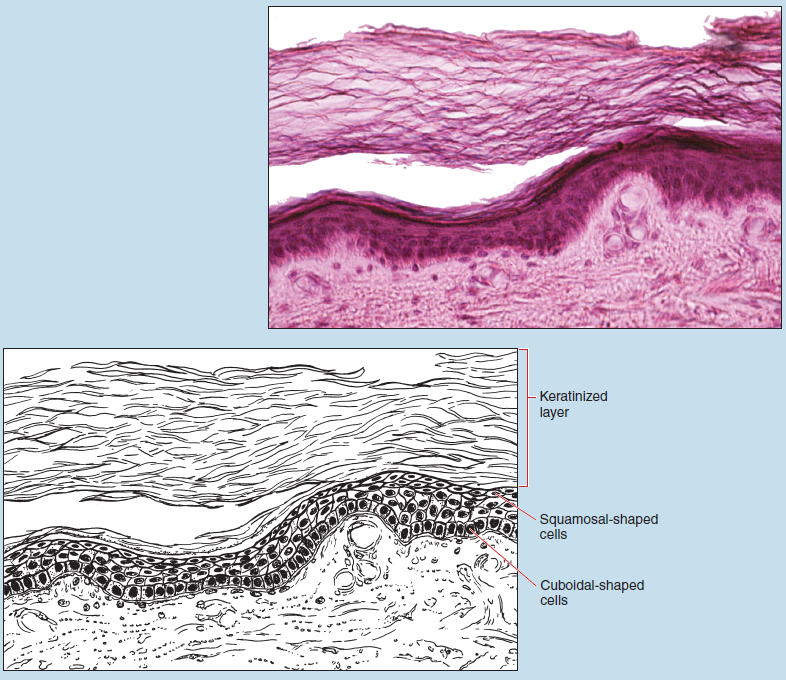
Stratified Squamous Epithelium (Keratinized) (Thin Skin/Caucasian)
Figures 2-9 and 2-10 were obtained from thin Caucasian skin. This type of epithelium is found on surfaces of the body that are subjected to significant abrasion. Note the sectioning and preparation artifacts in this slide.
As you compare Figures 2-9 and 2-10 with those examined previously (see Figures 2-6 to 2-8), you will note some subtle similarities and differences between these two examples of stratified squamous epithelium:
- The epithelium in all of the figures is composed of multiple layers, thereby making it a stratified epithelium.
- The nuclei of the cells in this epithelium appear to be “regularly arranged;” that is, they appear to be arranged into distinct layers. However, this is significantly more apparent in Figures 2-6 through 2-8 than in Figures 2-9 and 2-10.
- Although the basal cells are cuboidal in shape, the superficial layer of cells in both of these epithelia is composed of squamosal cells.
Examination of Figures 2-9 and 2-10 demonstrates that the most superficial layer of this epithelium is composed of a keratinized layer. This layer is composed of dead, anucleated squamous cells that are continuously being sloughed off. These cells give the protective characteristics to the skin.
Again, remember that the classification of a stratified epithelium is based on the shape of the most superficial layer of cells—hence this epithelium is classified as a stratified squamous epithelium.
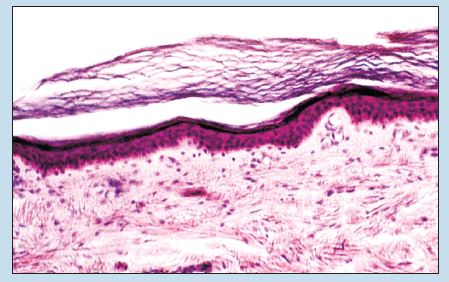
Figure 2-9 (50X): Stratified squamous epithelium (thin skin/Caucasian).
Stratified Columnar Epithelium (Spongy Urethra)
Figure 2-11 is of the spongy (cavernous or penile) portion of the male urethra and shows an epithelium composed of several layers. The most superficial layer of this epithelium is composed of columnar epithelial cells.
Note the following:
- This is an epithelium composed of more than one layer, and therefore it is classified as a stratified epithelium.
- The nuclei of the epithelial cells appear to be arranged into rows, again suggesting a stratified epithelium.
- The cells in the superficial layer are taller than they are wide, indicating a columnar epithelium.
Each of the cells in the superficial layer has its nucleus in the basal portion of the cell, again indicating a columnar epithelium. All of these are important histological characteristics of a stratified columnar epithelium.
Finally, note how the depth of the epithelium, as well as the overall focus of the structure, varies within the specimen. This is an excellent example of how the appearance of an epithelium may vary from place to place because of a sectioning artifact. The appearance of a sectioning artifact in this photomicrograph, and the way in which the image fades from in focus to out of focus, clearly indicates the need to look at the entire specimen before categorizing the epithelium.
Stratified Cuboidal Epithelium (Sweat Gland Duct)
A stratified cuboidal epithelium (Figure 2-12) is characterized by two or more layers of cells, with a superficial layer of cuboidal-shaped cells.
Although the lateral borders of the superficial cells are not clearly evident, several characteristics indicate that these cells are indeed cuboidal:
- The nucleus is located within the central portion of the cell.
- The apical cells are approximately equal in height and width.
These characteristics, when taken together, indicate that this epithelium is stratified cuboidal.
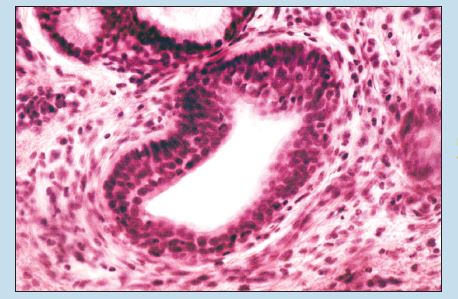
Figure 2-11 (100X): Stratified columnar epithelium (cavernous urethra).
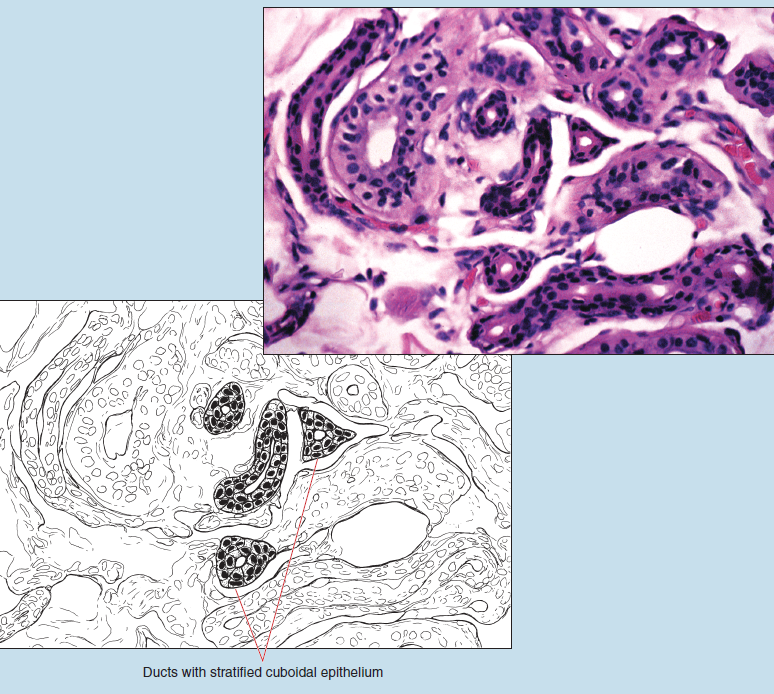 Figure 2-12 (100X): Stratified cuboidal epithelium (sweat gland duct).
Figure 2-12 (100X): Stratified cuboidal epithelium (sweat gland duct).
Pseudostratified Epithelia
Pseudostratified Ciliated Columnar Epithelium (Trachea)
These photomicrographs were taken from the trachea. As you look at Figure 2-13, note the epithelium and its characteristics. Note that the epithelial nuclei are at varying levels, thereby giving the appearance of an epithelium composed of several layers.
Now proceed to Figure 2-14. Note that the nuclei appear to be randomly arranged within the epithelium; this is a key characteristic of a pseudostratified epithelium. Continued examination demonstrates that the cells, even though they may be of different heights, are all considerably taller than they are wide, a feature that is characteristic of a columnar epithelium.
Although it cannot be demonstrated with the light microscope, all of the cells of this epithelium do indeed reach the basal lamina but vary considerably in height. Because all of the cells reach the underlying basal lamina, this epithelium cannot be classified as stratified. In addition, because of the variation in the height of the cells, not all of the cells reach the luminal surface. This variation in cell height and the corresponding nucleus location contribute to the appearance of a stratified epithelium—hence the designation of a pseudostratified epithelium; that is, an epithelium that has the appearance of being stratified but is not.
The apical surface of the cells in Figure 2-14 demonstrates a surface modification commonly seen in epithelial cells—cilia.
Also visible in Figure 2-14 are a few mucous cells, which are commonly seen in the pseudostratified columnar epithelium of the trachea.
Finally, this epithelium sits on an unusually thick basal lamina. The gap seen between the epithelium and the underlying basal lamina in this photomicrograph is a fixation artifact.
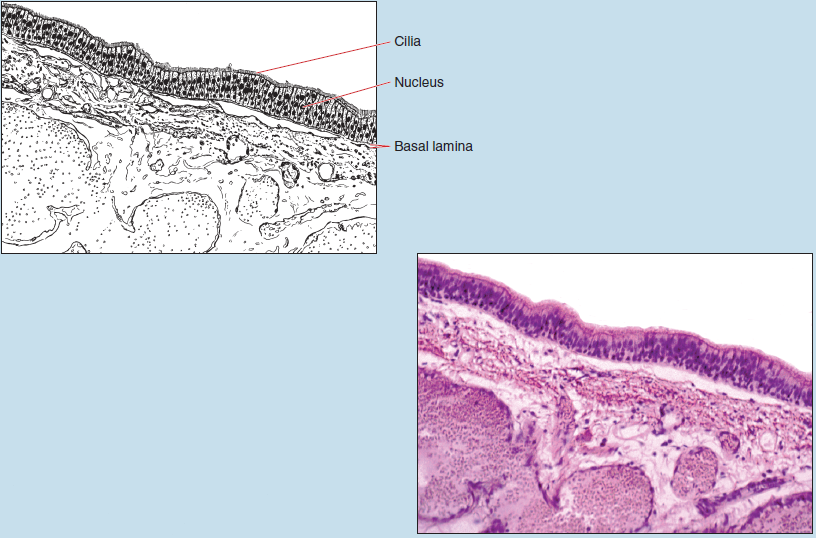 Figure 2-13 (50X): Pseudostratified ciliated columnar epithelium (trachea).
Figure 2-13 (50X): Pseudostratified ciliated columnar epithelium (trachea).
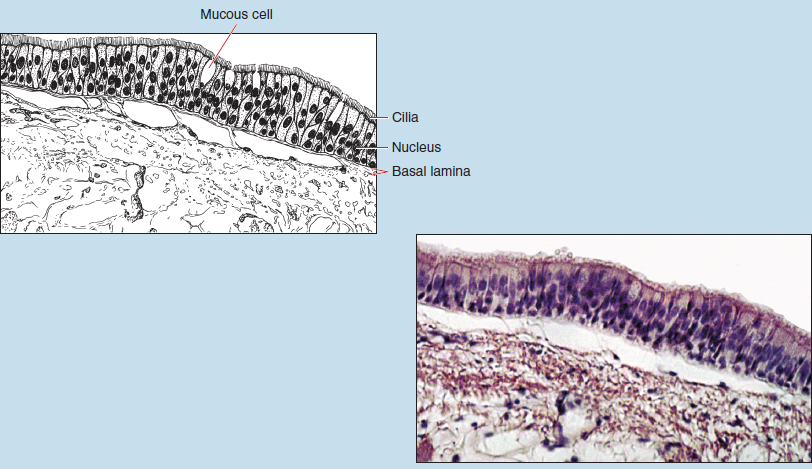 Figure 2-14 (100X): Pseudostratified ciliated columnar epithelium (trachea).
Figure 2-14 (100X): Pseudostratified ciliated columnar epithelium (trachea).
Transitional Epithelia
Transitional Epithelium (Relaxed Urinary Bladder)
The distribution of this epithelium is limited to the urinary tract. The appearance of the cells that comprise this type of epithelium will vary depending on the state of stretch of the organ at the time of fixation; hence the name transitional. Because of this inherent variability, transitional epithelium is one of the most difficult epithelia to identify correctly.
The cells at the free surface of a transitional epithelium are described as dome shaped, or balloon shaped, broadly cuboidal, or somewhat flattened (approaching squamous), depending on the state of stretch of the organ. Examination of Figure 2-15 will show the following:
- An epithelium composed of more than one layer
- A “regular” arrangement of the nuclei, in that the nuclei appear to be arranged in rows (as seen in Figures 2-7 through 2-12, but not in Figure 2-13)
- A variation in cell shape when you compare the deepest layer with the most superficial layer
- Cells at the free surface that typically are large and rounded (characteristic of a relaxed organ) or flattened, almost squamous in shape (characteristic of a stretched and distended organ)
- If the surface layer is squamous in shape, an abrupt change will be seen in cell shape from the superficial layer to deeper layers, where the cells will be larger and more rounded
These characteristics might lead you to incorrectly identify this epithelium as a stratified epithelium—possibly a stratified cuboidal or stratified columnar epithelium, or even a stratified squamous epithelium. However, further examination will lead you to a correct identification of this epithelium.
A correct identification of all epithelia, particularly transitional epithelia, requires you to examine the entire epithelial surface—a process often termed running the epithelium. In order to correctly identify transitional epithelium, you must slowly run the epithelium. This is accomplished by slowly scanning the entire epithelium from one end of the specimen to the other. Start at the end of the epithelium in the lower right side of the photomicrograph (see Figure 2-15). Now proceed toward the middle of the photomicrograph and then continue until you complete your examination at the other end of the epithelium. As you run the epithelium, additional characteristics of a relaxed transitional epithelium come to light:
- The shape of the most superficial cells on this specimen changes from region to region. If you run the epithelium from the lower right of Figure 2-15, you will note that the most superficial layer of cells ranges from almost squamous to something approaching cuboidal, and finally to a series of rounded or dome-shaped cells. As you approach the upper left corner of the epithelium, the cell shape again approaches squamous. This variation in the shape of the most superficial layer of cells is an important identification feature of a relaxed transitional epithelium.
- The number of layers in the epithelium appears to vary from region to region. This, too, is an important identification feature of a relaxed transitional epithelium.
- When transitional epithelium is obtained from a relaxed organ, the surface cells often bulge into the lumen (often referred to as dome- or balloon-shaped cells), another important identification feature of transitional epithelium.
- This photomicrograph also demonstrates that transitional epithelia may have binuclear cells on the apical surface.
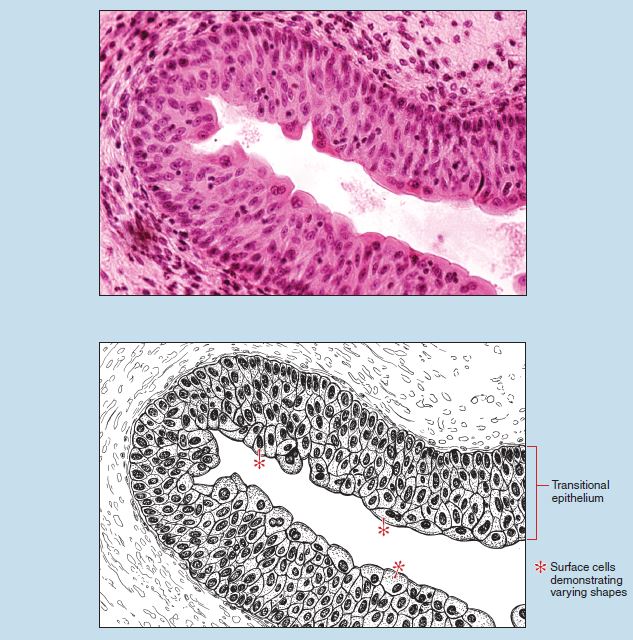
Figure 2-15 (100X): Transitional epithelium (relaxed urinary bladder).
Epithelial Glands
Epithelial glands are the second main form of epithelial tissue. Epithelial glands are classified as either endocrine glands or exocrine glands.
Endocrine glands are ductless glands that release their secretions directly onto the cell’s surface or directly into the lymphoid system, interstitial fluids, or bloodstream.
Exocrine glands are those that possess ducts or that deliver their secretion to an apical or luminal surface. These glands may be either unicellular (e.g., goblet cells and mucous cells) or multicellular. Multicellular exocrine glands are composed of two parts: a secretory portion and a duct that conveys the secretion to the epithelial surface. Multicellular exocrine glands are typically subdivided by the structure of their ducts. Simple exocrine glands possess an unbranched duct, whereas a compound exocrine gland possesses a duct that branches repeatedly.
Compound exocrine glands may be further subdivided based on the shape of the secretory portion of the gland. An acinar gland is a compound exocrine gland, the secretory portion of which is flask shaped; the secretory portion of a tubular gland is shaped like a tube. Some glands (e.g., mammary glands and the pancreas) may be a combination of a tubular and acinar gland. Such glands would then be classified as tubuloacinar glands.
Exocrine Glands
Unicellular Exocrine Glands
Figures 2-3 and 2-14 demonstrate unicellular exocrine glands. Goblet cells (see Figure 2-3) are commonly found within many regions of the digestive tract, whereas mucous cells (see Figure 2-14) are found within portions of the respiratory tree. Goblet and mucous cells often give the appearance of being clear or empty. They have this appearance as a result of the dissolution of the mucinogen during histological processing.
Simple Glands (Sweat Glands)
Sweat glands are multicellular glands that possess a distal secretory portion in which the epithelial cells produce the secretion, and an epithelial duct that carries the secretion to the exterior of the gland. Although the distal secretory portion is not visible in this section, Figure 2-16 demonstrates how the duct is repeatedly sectioned into circular segments because of the convoluted shape of the tubular portion of the gland. Note that the duct does not appear to go to the surface. This is the result of the plane of section and illustrates how you must keep the three-dimensional organization of a structure in mind when viewing histological preparations.

Figure 2-16 (100X): Simple epithelial glands (sweat glands).
Simple Glands (Intestinal Crypts)
Figure 2-17 demonstrates unbranched, simple tubular exocrine glands of the duodenum of the small intestine (called intestinal crypts). These simple glands are formed by the surface epithelium extending deep into the mucosal layer of the duodenum, thereby forming a straight tubule that opens directly onto the epithelial surface via a simple, unbranched duct.
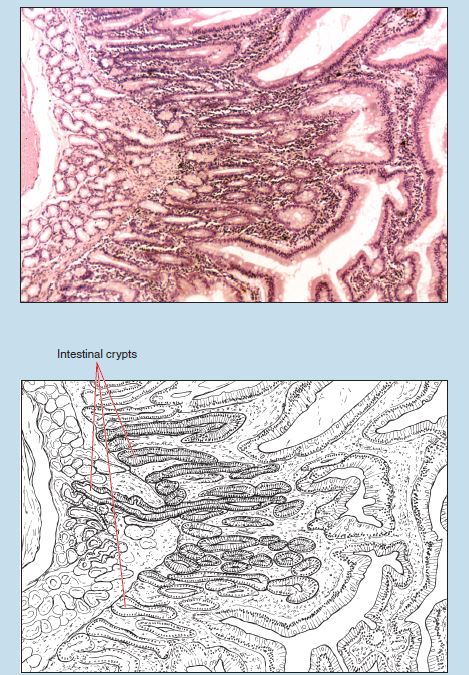 Figure 2-17 (50X): Simple glands (duodenum).
Figure 2-17 (50X): Simple glands (duodenum).
Compound Tubuloacinar Glands
Mammary Gland
The mammary gland (Figure 2-18) is composed of secretory acini and excretory ducts and is therefore a compound tubuloacinar gland.
Parotid Salivary Gland
The parotid salivary gland (Figure 2-19) is another excellent example of a compound tubuloacinar gland. For this slide, concentrate on the shape and composition of an acinar gland. Later (see Chapter 16) you will learn about the histological characteristics that will enable you to correctly identify the different types of salivary glands.
Acinar glands are epithelial glands that contain circular or flask-shaped secretory segments. In this slide, note both the secretory acini and ducts of the salivary gland. One way to visualize an acinus is to imagine an orange or grapefruit that has been cut into a cross section (see Figure 1-6). Each wedge of the fruit represents a columnar acinar cell. This cell shape is termed columnar because the cell is taller than it is wide. The central portion of the fruit section is the centroacinar duct of the gland, and the skin of the fruit represents the basal lamina of the glandular acinus.
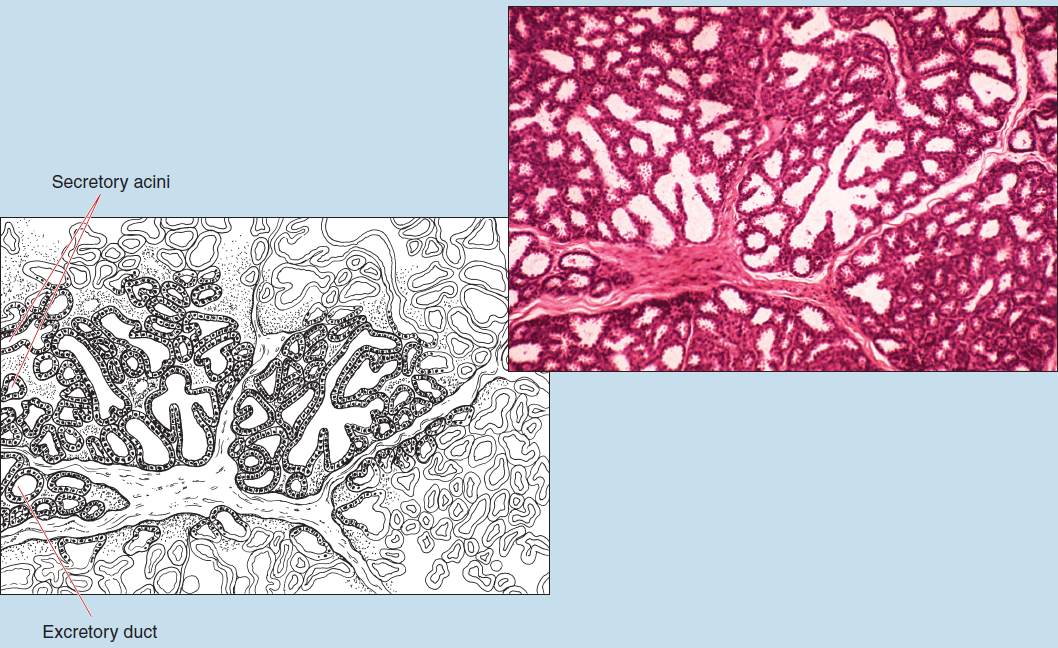 Figure 2-18 (100X): Compound tubuloacinar epithelial glands (mammary gland).
Figure 2-18 (100X): Compound tubuloacinar epithelial glands (mammary gland).
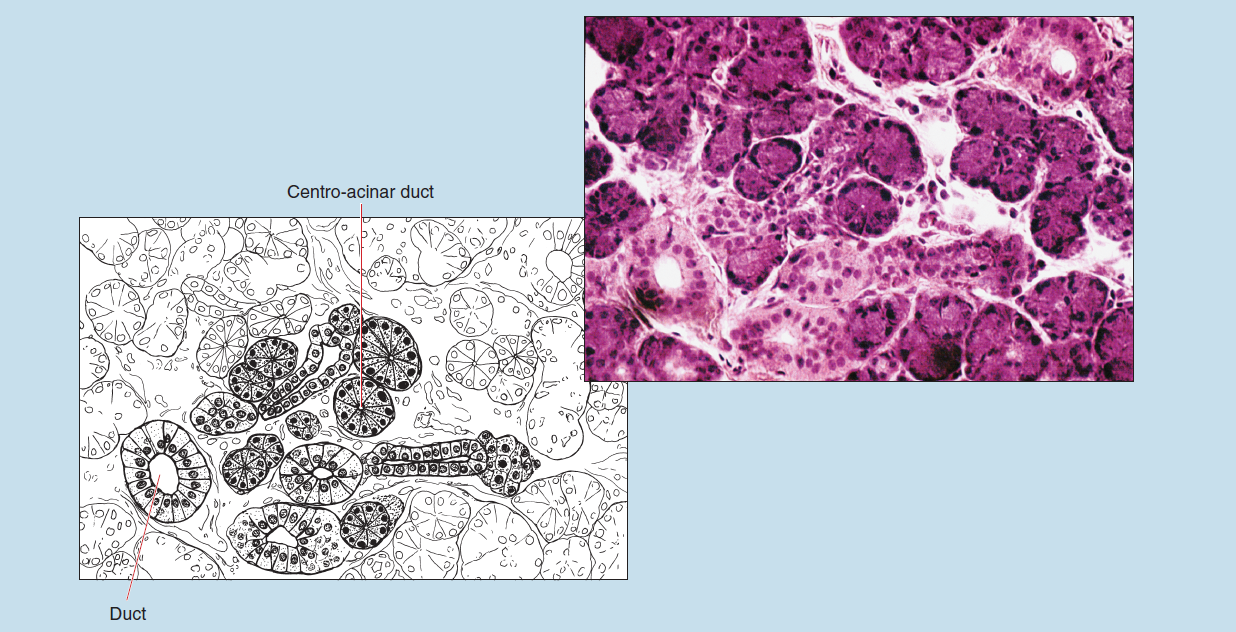
Figure 2-19 (200X): Compound tuboloacinar gland (parotid salivary gland).
Endocrine Glands
A complete histological explanation of endocrine glands is provided in Chapter 14.
Endocrine Pancreas (Pancreatic Islets, or Islets of Langerhans)
Figure 2-20 is a high-dry photomicrograph of pancreatic islets (Islets of Langerhans), which comprise the endocrine portion of the pancreas. Endocrine glands are often composed of epithelioid cells; that is, cells that are predominantly derived from epithelial tissue and therefore have epithelial characteristics. (An exception to this rule is the neurohypophysis, or posterior lobe of the pituitary gland, which is derived from neural tissue.) Their secretions are released into the vascular system without the use of ducts. Endocrine glands may be unicellular, such as the enteroendocrine cells within the digestive system, or multicellular, such as the endocrine portion of the pancreas. If an endocrine gland is multicellular, the cells may be grouped together into an organ, such as the thyroid gland, or may be scattered throughout an organ, as are the islets of the pancreas.
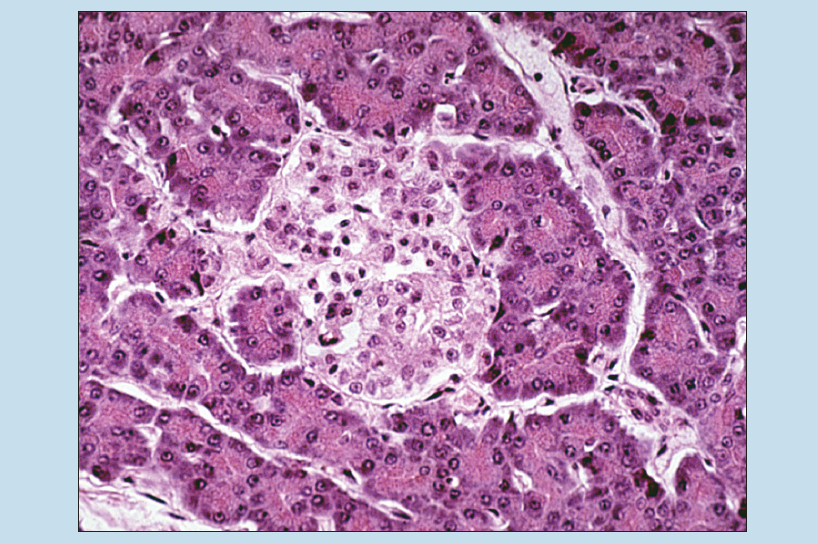 Figure 2-20 (200X): Endocrine pancreas (Islets of Langerhans).
Figure 2-20 (200X): Endocrine pancreas (Islets of Langerhans).
Commonly Misidentified Tissues
Stratified Squamous and Transitional Epithelia
When you are looking at epithelial tissue, it is important to remember that stratified squamous epithelium (nonkeratinized, mucosal type) and transitional epithelium are easily misidentified. Therefore keep in mind the differences between these two types of epithelium.
Stratified Squamous Epithelium (Nonkeratinized, Mucosal Type) (Review Figures 2-6 to 2-8 in “Stratified Epithelia” section)
- Stratified squamous epithelium is composed of many layers.
- The basal cells may appear to be cuboidal or columnar in shape.
- The surface layer is always composed of flattened cells.
- The number and extent of epithelial layers, as well as the shape of the most superficial layer of cells, are relatively consistent from one field of vision to another as you “run the epithelium.”
Transitional Epithelium (Review Figure 2-15 in “Transitional Epithelia” section)
- Transitional epithelium has fewer layers in comparison with stratified squamous epithelium.
- The basal cells are usually of similar shape when compared with the most superficial cells.
- The most superficial cells may be balloon shaped or dome shaped (in a relaxed organ) or flattened (in a distended organ).
- The number and extent of epithelial layers, as well as the shape of the most superficial layer of cells, are relatively inconsistent from one field of vision to another as you “run the epithelium.”