Chapter Objectives
This chapter will enable you to identify:
- The ovary and the stages of follicular development leading to ovulation or follicular atresia
- All the cell types evident in the varying stages of follicular development
- The histological characteristics of the oviducts
- The body and cervix of a mature uterus and all the cell types that comprise the various layers of the uterus
- The histological characteristics of the uterus as it progresses through the stages of the menstrual cycle
- The histological characteristics of the vagina
- The histological characteristics of a lactating mammary gland
Components of the Female Reproductive System and Their Functions
The female reproductive system is composed of the following organs:
- External genitalia
- Vagina
- Uterus
- Uterine (Fallopian) tubes
- Ovaries
- Mammary glands
These organs serve a variety of functions, including the following. They:
- Produce the ova and prepare it for ovulation by the ovaries. In addition, the ovaries produce reproductive steroid hormones.
- Provide a passageway for sperm and ova between the uterus and ovaries by the uterine (Fallopian) tubes
- Provide an environment for blastocyst implantation and fetus development by the uterus. The uterus is also involved in placental development, expulsion of the fetus at birth, and the cyclical changes seen in the endometrium in response to varying blood levels of the hormones estrogen and progesterone.
- Produce and secrete milk
Ovary
The ovary is covered by a simple squamous mesovarium, termed the surface epithelium (Figure 15-1), which changes at the hilus (not visible in this photomicrograph) to a low, cuboidal epithelium (see section on the Classification of Epithelial Tissues in Chapter 2). Deep to the surface epithelium is the tunica albuginea, which is a dense, fibrous, connective tissue layer composed of collagenous and reticular fibers.
In cross section the ovary is composed of two zones: an inner medulla and an outer, broader cortex (Figure 15-1). The medulla is composed of a loose framework of connective tissue rich in elastin, blood vessels, lymphatics, and nerves. The cortex is composed of compact, richly cellular connective tissue in which ovarian follicles are scattered. There is no sharp demarcation line between the cortex and medulla.
The cortex of an ovary from a mature, premenopausal female will contain numerous follicles in varying stages of development and degeneration. The size and complexity of the follicle depends on the stage of development, yet each is composed of an oocyte surrounded by epithelial cells. Larger follicles also contain one or two connective tissue coats. The follicles of the ovary are divided into the following stages of development: primordial, primary, secondary (also termed antral or growing), and mature (Graafian, ovulatory, or tertiary).
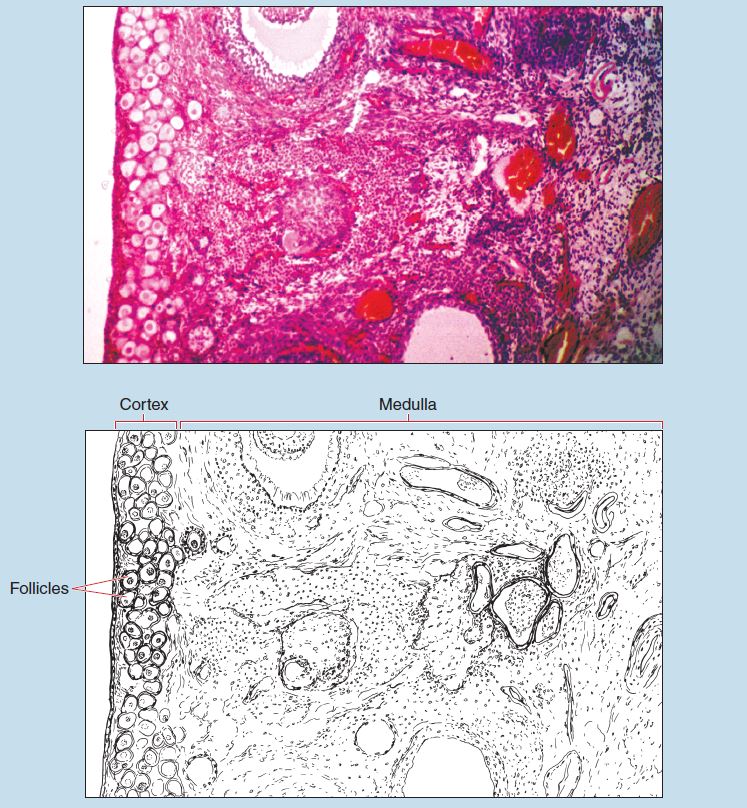
Figure 15-1 (25X): Ovary.
Primordial Follicles
Primordial follicles (Figure 15-2) are the most abundant and smallest of the follicles. Located at the periphery of the ovarian cortex, they consist of a primary oocyte surrounded by a few flattened follicular cells.
Primordial follicles are in a stage of arrested meiotic prophase and are unresponsive to hormones. Primordial follicles have been in this arrested stage of development since the fifth or sixth month of fetal development.
Primary Follicles
Primary follicles have started to grow, and changes are seen in the oocyte, follicular cells, and the adjacent connective tissue stroma. In an early primary follicle (Figure 15-2) the oocyte has started to enlarge, and the simple, squamous follicular cells enlarge to form a complete layer of cuboidal follicular cells around the oocyte. A basal lamina separates them from the rest of the ovary.
As the follicle continues to enlarge, it enters the late primary phase (Figure 15-3). In this phase, the oocyte continues to grow and secretes the zona pellucida, a glycoprotein coat that completely surrounds the oocyte. The follicular cells divide repeatedly, become multilayered, and are now called granulosa cells.
The stromal cells in the connective tissue surrounding the follicle have become organized into a distinct layer, the theca interna. The thecal cells are epithelioid in appearance and rounded in shape. They accumulate cytoplasmic lipid droplets that dissolve during the fixation process and are therefore quite pale staining.
Secondary Follicle
As the follicle continues to mature, it moves deeper into the cortical stroma of the ovary. In the secondary follicle (also termed an antral follicle or maturing follicle) (Figure 15-4), the antrum, a fluid-filled cavity, develops within the granulosa layer. The fluid within the antrum is called the follicular fluid (liquor folliculi). The antrum continues to enlarge in the secondary follicle.
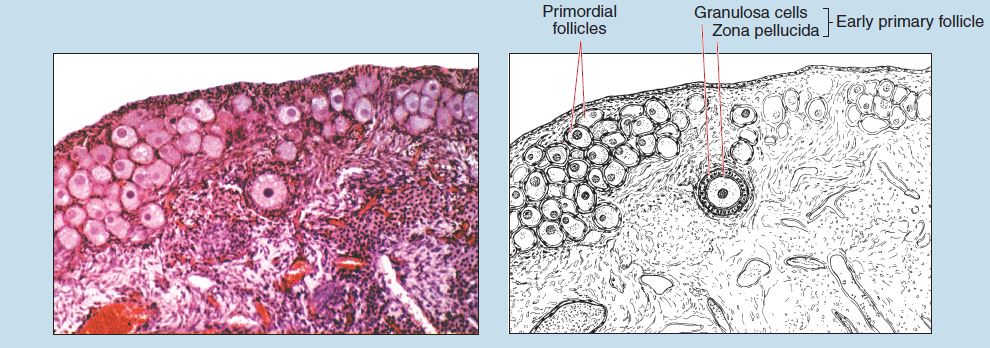
Figure 15-2 (50X): Primordial and early primary follicles within the ovary.
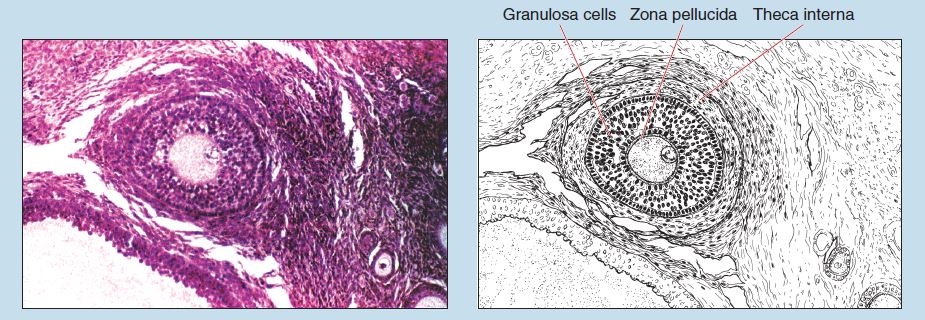
Figure 15-3 (50X): Late primary follicle within the ovary.
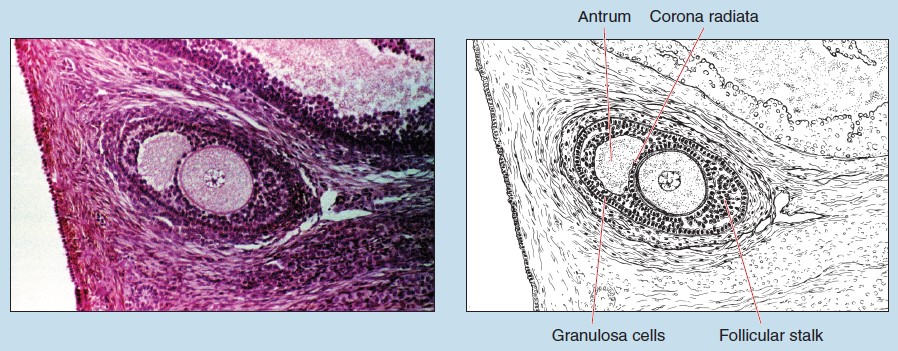
Figure 15-4 (50X): Secondary follicle within the ovary.
Mature Follicle
A mature follicle (also termed preovulatory follicle, Graafian follicle or tertiary follicle) (Figure 15-5) is the largest of the developing follicular stages, spanning the entire thickness of the ovarian cortex and causing a bulge on the surface of the ovary.
The mature follicle contains a large oocyte with a sizable nucleus and a prominent nucleolus (not visible in the current photomicrograph). The zona pellucida is now very thick, and the granulosa cells comprise a stratified epithelium with a basal layer that rests on a prominent basal lamina. The majority of the granulosa cells are small, with irregular cellular outlines, uniform nuclei, and numerous lipid droplets within the cytoplasm, giving the cells a light staining quality.
The antrum has enlarged and comes to occupy the majority of the follicle. As the antrum enlarged, the granulosa cells remained uniform in thickness, except for the region closest to the oocyte. These cells, which form the cumulus oophorus, project into the antrum and form the follicular stalk. The cells of the cumulus oophorus that completely surround the oocyte and that will remain with it at ovulation are termed the corona radiata.
As the mature follicle continues to prepare for ovulation, the corona radiata becomes only one cell thick, and the spaces between the granulosa cells enlarge. In addition, the oocyte and the cumulus oophorus cells gradually loosen from the rest of the granulosa cells. When ovulation occurs, the corona radiata and the loosely attached cells of the cumulus oophorus will remain with the oocyte.
In the mature follicle, the thecal layers have become even more prominent. The theca interna has thickened and now consists of a network of capillaries (see section on Capillaries in Chapter 8) with interspersed epithelioid cells. These cells possess the ultrastructure of steroid-secreting cells, and the cytoplasm contains a large amount of lipid droplets. As a result, the cells stain quite poorly.
The connective tissue surrounding the theca interna has differentiated and is now termed the theca externa. The theca externa is less vascular than the theca interna and possesses a larger number of collagenous fibers (see the discussion of collagenous fibers in the section on Loose, Irregular [Areolar] Connective Tissue in Chapter 3) and smooth muscle cells (see section on Smooth Muscle in Chapter 6).
Follicular Atresia
Numerous follicles in your specimen have undergone or are in the process of undergoing follicular atresia (Figure 15-6). This degenerative process can occur at any stage of follicular development.
Atresia of a primordial follicle is distinguished by the degeneration of the oocyte, indicated by a folding or general disintegration of its nucleus. On completion, atresia of a primordial follicle will leave little, if any, histological trace.
Atresia of a follicle in the primary stage or beyond is marked by hypertrophy of the thecal cells and autolysis of the granulosa cells, in addition to the degenerative changes observed within the oocyte discussed previously. The completion of follicular atresia is marked by a scar that represents the remnants of the zona pellucida.
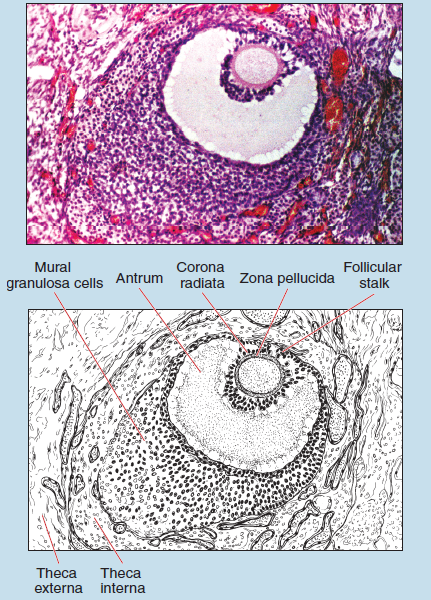
Figure 15-5 (50X): Mature follicule within the ovary.
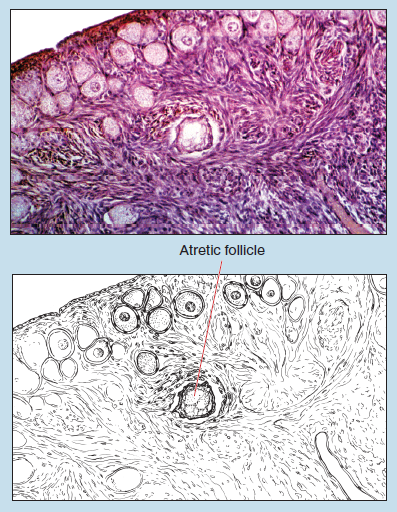
Figure 15-6 (50X): Follicular atresia.
Ovary/Corpus Luteum
Following ovulation and the subsequent release of the follicular fluid, the follicle collapses and becomes deeply infolded, thereby forming the corpus luteum (Figure 15-7). Cells of the theca interna and granulosa change morphologically, increasing in size and lipid content, and develop the ultrastructure of lipidsecreting cells.
Two cell types are identified within the corpus luteum. The greatest bulk of the corpus luteum is composed of granulosa lutein cells, which are differentiated from the granulosa cells. These are large, irregularly shaped cells with a centrally located nucleus and lightly staining cytoplasm.
The cells of the theca interna differentiate into theca lutein cells (also termed paralutein cells) (Figure 15-8). These will be seen along the folds and periphery of the corpus luteum. They are smaller and stain more darkly than the granulosa lutein cells.
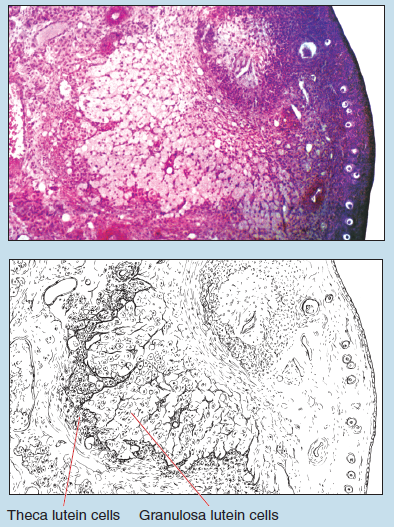
Figure 15-7 (50X): Corpus luteum within the ovary.
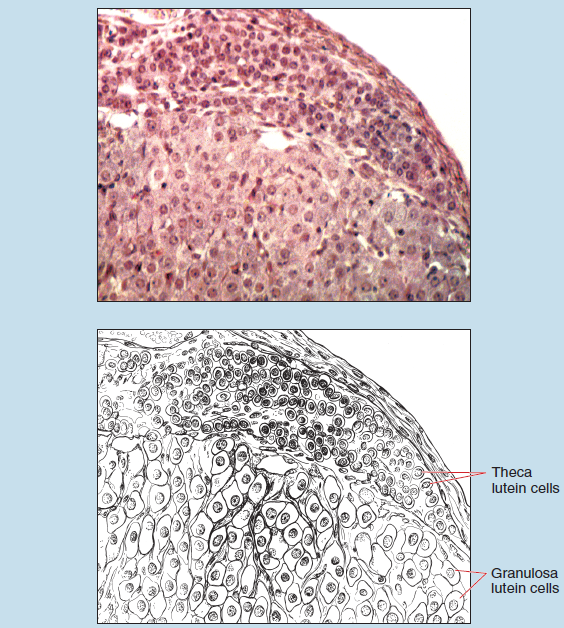
Figure 15-8 (100X): Corpus luteum within the ovary.
Uterine Tubes
The uterine tubes (oviducts or Fallopian tubes) are composed of three regions: infundibulum, ampulla, and isthmus. The walls of the uterine tubes are composed of three layers: an inner mucosa, middle muscularis, and outer serosa.
As you can see in Figures 15-9 and 15-10, the mucosa is folded to a variable extent. These folds will decrease in height as you progress toward the uterus. The epithelium of the mucosa is simple columnar (see section on Simple Columnar Epithelium in Chapter 2), with some of the cells possessing cilia. The lamina propria in the isthmus of the uterine tube is quite cellular because it is composed of loose, irregular (areolar) connective tissue.
The muscularis is composed of an inner circular and an outer longitudinal layer of smooth muscle. The thickness of the muscularis layer will vary, depending on the source of your specimen, with the muscularis in the isthmic region being thicker than that of the ampulla even though the longitudinal layer is less prominent.
The serosa (not visible on this photomicrograph) is a typical peritoneal structure.
Uterus
The wall of the body of the uterus is composed of three layers, the outermost of which is the peritoneum, not visible on this photomicrograph.
The second layer is the myometrium (Figure 15-11), which is composed of three layers of smooth muscle. The inner layer is longitudinally arranged and is termed the submucosal layer (subvascular stratum). The vascular layer comprises the second, circularly arranged layer, which forms the bulk of the myometrium. The outermost layer of the myometrium is called the supravascular layer and is a relatively thin layer of smooth muscle fibers that are circularly and longitudinally arranged. (Note: The inner longitudinal layer of the supravascular layer is absent from the cervix of the uterus.)
Between the smooth muscle layers you will see loosely arranged collagenous and elastic fibers and relatively few connective tissue cells (see section on the cells of Loose, Irregular [Areolar] Connective Tissue in Chapter 3). The connective tissue may be especially evident in the outermost portion of the muscularis.
The innermost layer of the uterus is a mucous membrane termed the endometrium. The luminal surface of the endometrium is lined by a simple columnar epithelium, with some of the cells possessing cilia. The epithelium has numerous branched and coiled tubular glands within it. The length of the glands indicates the depth of the endometrium. The remainder of the endometrium is composed of an extremely cellular connective tissue stroma.
The endometrium undergoes considerable histological changes during the menstrual cycle, and the most superficial portion is lost if implantation does not occur. The part of the endometrium that is lost during menstruation is termed the functional layer (also termed the decidua functionalis); the part that is retained is termed the basal layer (decidua basalis). The basal layer is the deepest portion of the endometrium and may stain more basophilic than the functional layer on your preparation.
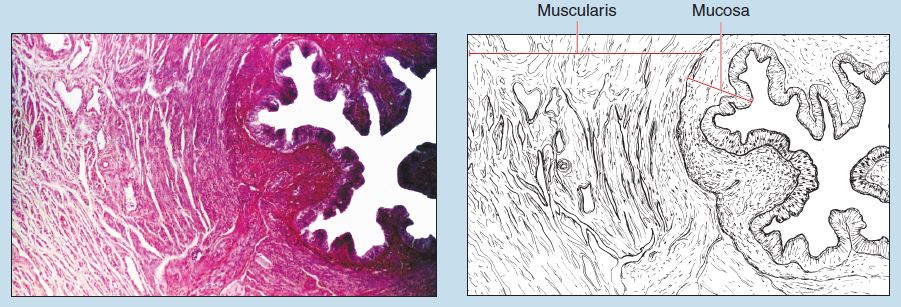
Figure 15-9 (25X): Uterine tube.
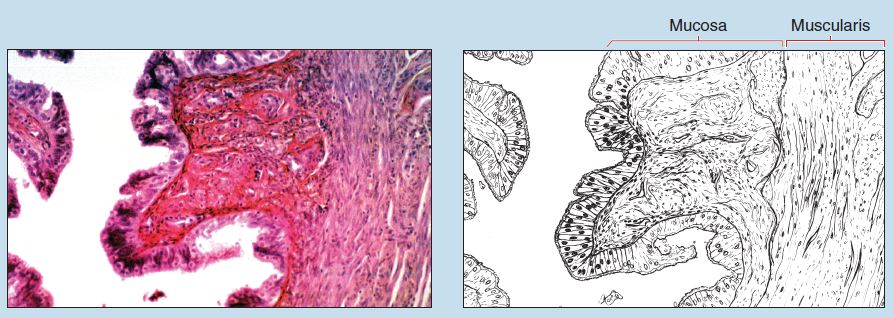
Figure 15-10 (50X): Uterine tube.
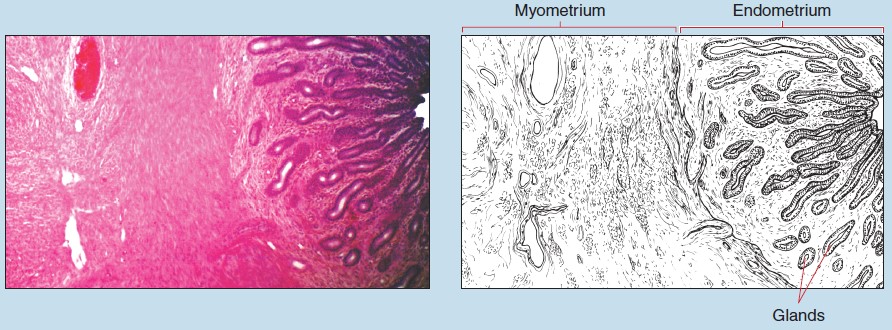
Figure 15-11 (25X): Uterus.
Uterus/Menstrual Cycle
Uterus/Proliferative Phase
The proliferative phase (also termed follicular or early postmenstrual phase) is a period of rapid regeneration of the endometrium (Figure 15-12). The epithelial cells of the glands of the basal layer are rapidly undergoing mitosis, and the resulting daughter cells are spreading over the remaining stromal cells to reestablish the luminal epithelium. As a result, the epithelial layer is a particularly thin, simple columnar epithelium. Mitotic figures may be present within both the luminal epithelium and stroma of the uterus. The uterine glands of the proliferative stage tend to be rather narrow, straight, and short—a major histological feature of this stage.
Uterus/Ovulatory Phase
In the ovulatory phase of the cycle (second week postmenstrual, early luteal, or presecretory) (Figure 15-13) the epithelium becomes pseudostratified columnar (see section on Pseudostratified Epithelia in Chapter 2) and the glands become longer and larger in diameter. Because of their increased length and corkscrew shape, cross and tangential sections of the glands will become more frequent within the endometrium. Both of these are important histological features of this phase of the menstrual cycle.
Late in this phase of the cycle, edema starts to develop within the connective tissue stroma; therefore the connective tissue within the functional layer stains less homogeneously. However, the staining characteristics of the basal layer tend to remain relatively constant throughout this phase. The endometrium increases in size overall, reaching 75% or more of its maximal size during this phase of the cycle.
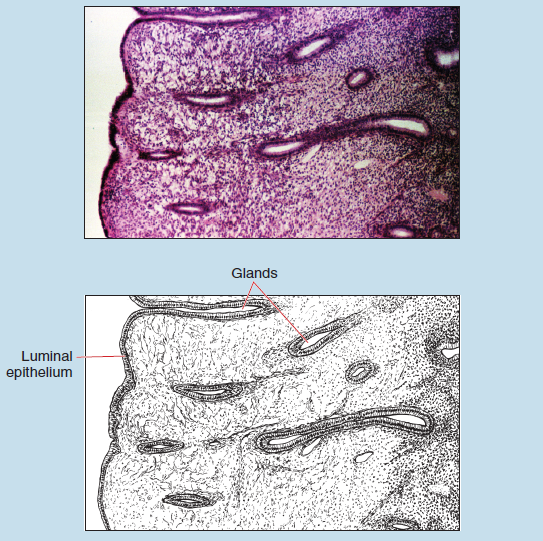
Figure 15-12 (25X): Menstrual cycle of the uterus: Proliferative phase.
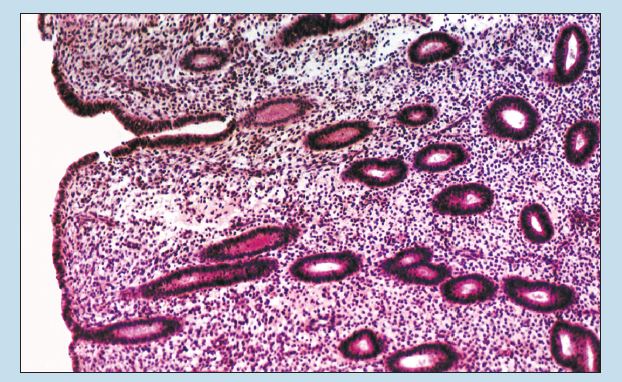
Figure 15-13 (25X): Menstrual cycle of the uterus: Ovulatory phase.
Uterus/Secretory (Late Luteal) Phase
The endometrium continues to increase in thickness during the secretory phase (late luteal phase) (Figure 15-14). The glands have now reached their maximal length and have developed the characteristically saw-toothed appearance. The glycogen content within the cells increases such that late in the secretory phase the nuclei become apically located. Both of these histological features are important in making a correct identification of this phase of the menstrual cycle.
Uterus/Menstrual Phase
In this phase of the cycle, the decidualization (sloughing off) of the stromal cells occurs in the superficial parts of the endometrium (Figure 15-15).
Early in this phase, the basal layer is further subdivided into the superficial stratum compactum and the deeper stratum spongiosum. With the onset of menstruation, red blood cells and leukocytes are present within the stroma and lumen. The endometrium is considerably reduced in thickness because of the loss of the most superficial portions of the stratum functionale.
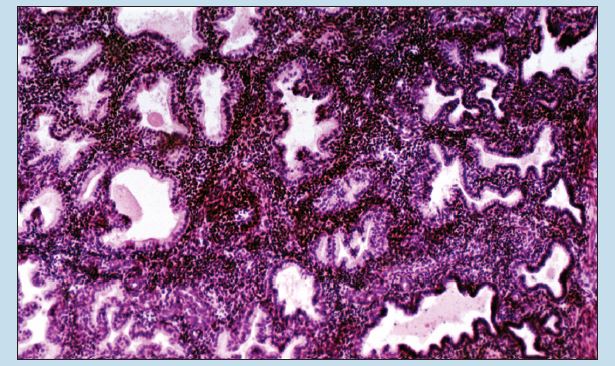
Figure 15-14 (25X): Menstrual cycle of the uterus: Secretory phase.
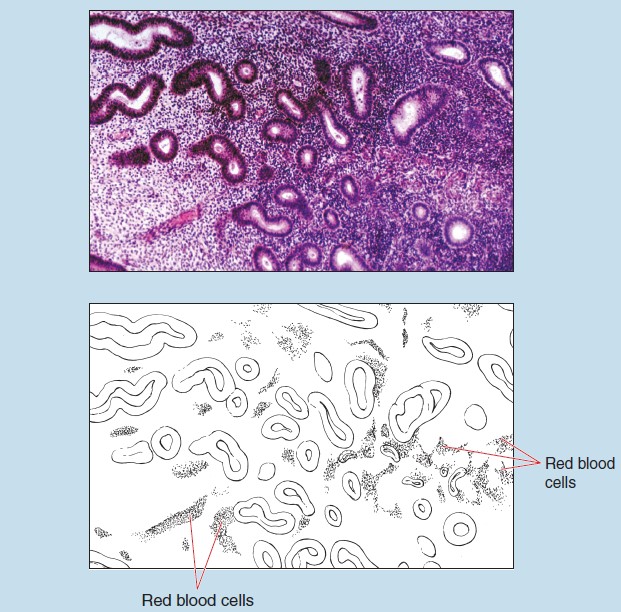
Figure 15-15 (25X): Menstrual cycle of the uterus: Menstrual phase.
Vagina
The wall of the vagina consists of three layers, the innermost of which is the mucosa (Figure 15-16), which demonstrates transversely orientated folds (rugae). The lumen of the vagina is lined by a nonkeratinized, stratified, squamous epithelium (mucosal type) (see section on Stratified Squamous Epithelium [Mucosal Type] in Chapter 2) resting on a prominent basal lamina and an underlying lamina propria. The appearance of lymphocytes and leukocytes is quite common within the lamina propria.
The muscularis of the vagina is made up of bundles of longitudinally and circumferentially arranged smooth muscle. This orientation of the muscularis may serve as a major histological feature of the vagina. Bundles of connective tissue rich in elastic fibers separate the muscle layers.
The outermost layer of the vagina is the adventitia, which is not visible on this photomicrograph. The adventitia is composed of loose, irregular (areolar) connective tissue rich in elastic fibers.
Lactating Mammary Gland
A superficial layer of subcutaneous fat (not visible in this photomicrograph) covers the entire organ, except for the nipple and surrounding the areola.
Each mammary gland is composed of 15 to 20 lobules (Figure 15-17). Each lobule is a compound gland with a separate lobular duct, which is lined by simple cuboidal epithelium. The lobular duct opens at the apex of the nipple.
During lactation, the tubules characteristic of an inactive gland form buds that enlarge into secretory alveoli, all of which are connected to a duct. Many of these alveoli appear as oval or spherical profiles lined by secretory cells arranged into a simple cuboidal epithelium.

Figure 15-16 (25X): Vagina.
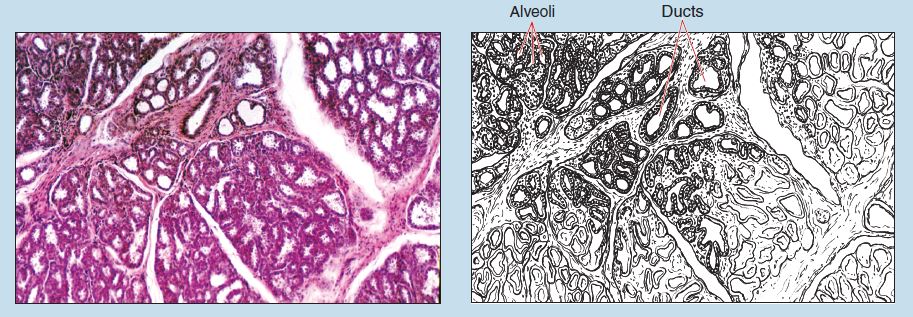
Figure 15-17 (25X): Lactating mammary gland.
Commonly Misidentified Tissues
Lactating Mammary Gland and Thyroid Gland
When identifying various sections of the female reproductive system, several common mistakes are made. It is not uncommon to confuse a lactating mammary gland and the thyroid gland, or to mistake the corpus luteum for the adrenal cortex. Therefore you should keep the following histological features in mind:
Lactating Mammary Gland (Review Figure 15-17 in section on the Lactating Mammary Gland)
-
- There are ducts connected to each alveolus.
- Gland is clearly lobulated.
- Secretion within alveoli appears granulated.
- Alveoli are irregular in shape.
Thyroid Gland (Review Figures 13-5 and 13-6 in section on the Thyroid Gland in Chapter 13)
-
-
- There is an absence of ducts.
- Lobulation is lacking.
- Colloid within follicles stains more homogeneously.
-
Corpus Luteum and Adrenal Gland
Corpus Luteum (Review Figures 15-7 and 15-8 in section on the Ovary and Corpus Luteum)
-
- Developing follicles present within section when viewed under low or medium power
- Arrangement of cells into homogeneous cords within the gland
- Absence of capsule
Adrenal Gland (Review Figures 13-9 to 13-12 in section on the Suprarenal [Adrenal] Gland in Chapter 13)
-
- Cells are arranged into cortex and medulla when viewed under low or medium power.
- Cells of cortex are arranged into three layers.
Ureter and Isthmic Region of the Uterine Tubes
Another common misidentification, even among experienced histologists, involves the ureter and isthmic region of the uterine (Fallopian) tubes. Both of these structures have a convoluted lumen surrounded by a considerable amount of smooth muscle. In trying to differentiate between these two structures, you should keep in mind the following differences:
Ureter (Review Figure 12-8 in section on the Ureter in Chapter 12)
-
- Transitional epithelium
- Muscularis arranged with an inner longitudinal layer and an outer circular layer
- Star-shaped lumen
Isthmic Region of Uterine Tubes (Review Figures 15-9 and 15-10 in section on the Ureter in Chapter 12)
-
- Simple cuboidal epithelium (some possessing cilia)
- Highly folded mucosa
- Muscularis arranged with an inner circular layer and an outer longitudinal layer
