Chapter Objectives
This chapter will enable you to identify and discuss the histological:
- Characteristics of the lips
- Structure of the tongue and the circumvallate papillae and associated taste buds
- Characteristics of the tubuloacinar glands of the salivary glands and the general characteristics of each form of salivary gland
- Characteristics of the esophagus and how these characteristics change with the level of sectioning
- Changes that occur in the hollow organs of the gastrointestinal tract as you progress from the esophagus to the large intestine and appendix
- Forms of mucosal glands of the stomach
- Regional specializations of the small intestine
- Characteristics of the colon
- Characteristics of the appendix and gallbladder
- Characteristics of the pancreas and liver
General Organization of the Hollow Organs of the Digestive System
The gastrointestinal (GI) system is composed of the hollow gastrointestinal tract and associated accessory structures (teeth, salivary glands, tongue, liver, gallbladder, and pancreas). The hollow organs, starting at the esophagus, share a common, general organization. With few exceptions, these organs are arranged into four layers. From superficial to deep, these layers and their general characteristics are as follows:
- Mucosa
- Composed of an epithelium sitting on a connective tissue lamina propria
- May possess a layer of smooth muscle deep to the lamina propria, which is termed the lamina muscularis of the mucosa in the esophagus and muscularis mucosae throughout the remainder of the hollow organs of the digestive tract
- Submucosa
- Composed of irregular connective tissue
- Found deep to the lamina propria and lamina muscularis
- Starts at the level of the esophagus and is found in all hollow organs of the GI system except the gallbladder
- Muscularis Externa
- Typically composed of two layers of smooth muscle (inner circular and outer longitudinal)
- May also include visceral striated muscle, as in the esophagus, or may include a third layer of smooth muscle, as in the stomach
Lips
Figure 16-1 is a hematoxylin and eosin (H & E) preparation of human lips. On scanning power, note the region of transition in the thickness of the epithelium. This is the transitional area (also termed the vermilion part) from the cutaneous (facial or exterior) part of the lip to the mucosal (oral cavity or interior) part. The cutaneous part consists of a keratinized, stratified squamous epithelium (see section on Stratified Squamous Keratinized Epithelium in Chapter 2) resting on a prominent layer of connective tissue. Within the connective tissue you may find sweat glands, sebaceous glands, and the bases of hair follicles.
The transition from the cutaneous part to the mucosal part is marked by the following characteristics:
- A gradual thickening of the epithelium
- A gradual disappearance of keratinized cells and a transition to a stratified squamous epithelium (mucosal type)
- A gradual increase in the height of the connective tissue papillae
- The disappearance of hair follicles, sebaceous and sweat glands
- The appearance of labial (mixed or seromucous) glands in the connective tissue deep to the mucosal surface
Tongue and Vallate Papillae
A thick layer of stratified squamous epithelium covers the tongue (Figure 16-2). The upper surface is studded with projections known as lingual papillae. Deep to the epithelium is the lamina propria (also termed the tunica propria), which is composed of areolar connective tissue (see section on Loose, Irregularly Arranged [Areolar] Connective Tissue in Chapter 3). This connective tissue forms the core of the papillae.
The musculature of the tongue is composed of skeletal muscle (see section on Skeletal Muscle in Chapter 6) arranged into three interlacing layers: vertical, transverse, and longitudinal. Among these bundles, you will note considerable amounts of fibroelastic connective tissue with varying numbers of blood vessels (see section on Blood Vessels in Chapter 8), peripheral nerves (see section on Peripheral nerves in Chapter 7), and adipose cells (see section on White Adipose Tissue in Chapter 3). Seromucous glands (see discussion of compound tubuloacinar glands in the section on the Parotid Salivary Gland in Chapter 2) may also be present on your specimen (not visible in this photomicrograph).
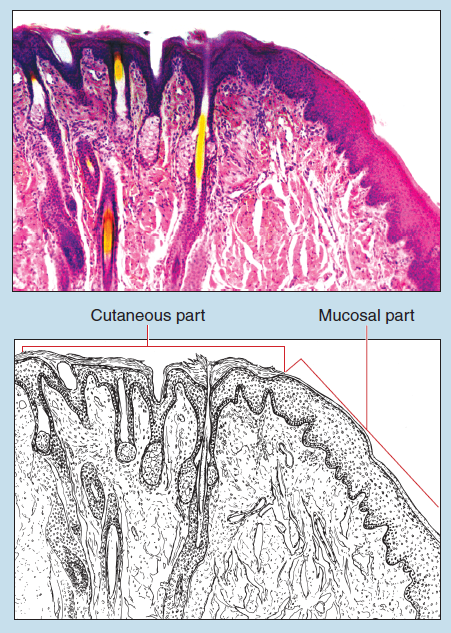
Figure 16-1 (25X): Lip.
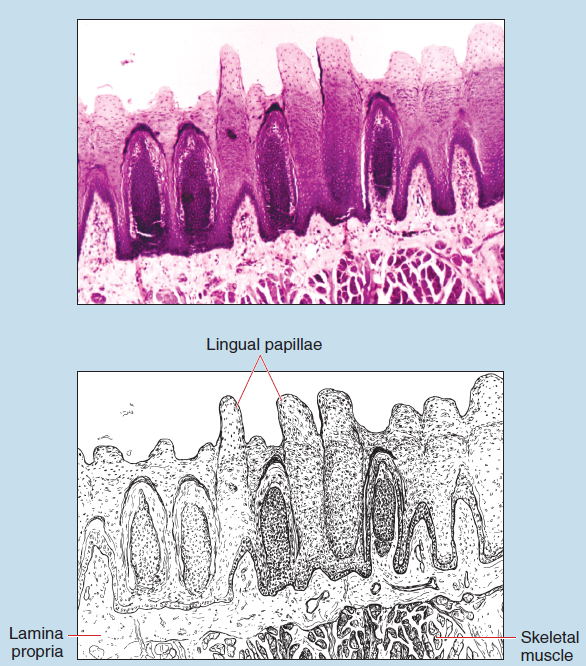
Figure 16-2 (25X) : Tongue.
Four forms of papillae are found on the human tongue: filiform, fungiform, foliate, and vallate (also termed) papillae. Vallate papillae are visible on Figures 16-3 and 16-4. They are rather large, dome-shaped papillae and are surrounded by a moat-like furrow. The papillae and furrow are covered by a noncornified, stratified squamous epithelium.
Taste buds are found on the lateral surface of the papillae and the outer wall of the furrow. Taste buds are little, barrel-shaped groups of cells embedded in the papillae. Each taste bud is connected to the surface by a small opening, the gustatory pore, which may not be visible on your specimen. Two of the following three cell types that make up a taste bud are visible in Figure 16-4:
- Supporting (sustentacular) cells are elongated cells with a slender, darker staining nucleus.
- Gustatory (neuroepithelial, taste or sensory) cells exhibit a lighter, more oval nucleus and cytoplasm that may or may not stain lighter.
- Basal epithelial cells are located at the periphery of the taste bud and possess an elongated, darker-staining nucleus and are not visible in this photomicrograph.
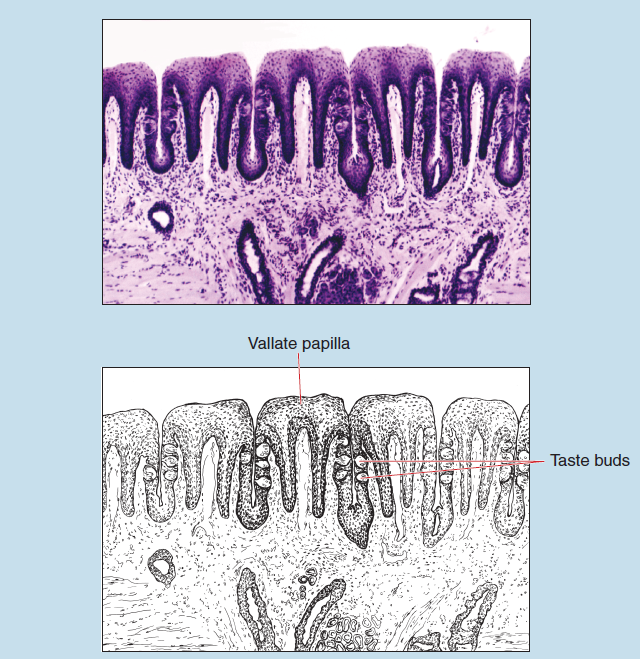
Figure 16-3 (25X): Vallate papillae of the tongue.
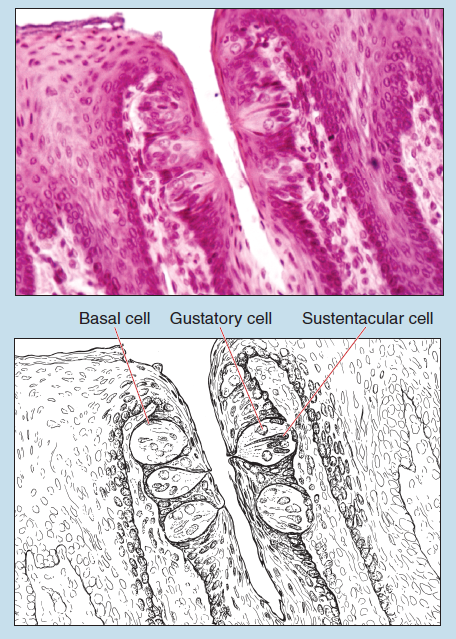
Figure 16-4 (25X): Vallate papillae of the tongue.
Salivary Glands
A number of different types of salivary glands secrete into the oral cavity. For convenience, these are subdivided into two groups: minor salivary glands and major salivary glands. The minor salivary glands secrete continuously and contribute to the saliva of the oral cavity. They open onto the oral mucosa either directly or via short ducts.
The major salivary glands include the parotid, submandibular, and sublingual salivary glands. They release their secretions in response to mechanical, olfactory, or neural stimuli. These glands are located some distance from the oral epithelium and are connected to it by a series of branching ducts. The secretory cells of the major salivary glands are arranged into glandular acini.
Except for the parotid, the major salivary glands are mixed glands. The secretory portions are ovoid or elongated acini at the ends of a duct. In these mixed glands, some acini are made up exclusively of serous cells and others are composed entirely of mucous cells. Other acini consist of mucous cells capped by a crescent layer of serous cells. This arrangement of secretory cells is termed a serous demilune.
In mucous acini, a single layer of plump, pyramidal cells rests on a basal lamina. The cytoplasm of these cells is filled with pale droplets of mucigen. During histological preparation the droplets of mucigen are partially or totally extracted, leaving round, clear areas outlined by a thin network of cytoplasm. The nucleus is displaced far to the base of the cell and may be deformed by the accumulated secretory product that occupies the greater part of the volume of the cell.
In serous acini, the cells have a columnar or truncated pyramidal form and surround a smaller lumen than that seen in mucous acini. The apical portion of the cell is crowded with secretory granules, thereby giving the cells a granular appearance. Cells of serous acini stain richly basophilic and are proteinsecreting cells.
Acini containing both serous and mucous cells were traditionally called seromucous acini. This term is no longer used because it was discovered that some cells secrete both protein and carbohydrate products. To eliminate any possible confusion, acini containing both serous and mucous cells are now called mixed acini. In this type of acinus, both types of cells are segregated. The mucous cells occupy the proximal end of the acinus and the serous cells are displaced to the distal end, where they appear as a crescent cap of dark-staining cells, the serous demilune. The cells of the serous demilune appear to be separated from the lumen of the acinus by the underlying mucous cells. However, the secretions from the serous demilune are conducted to the lumen of the acinus through narrow channels between the mucous cells. These narrow channels are visible with the electron microscope but not with the light microscope.
Salivary ducts have varying diameters. Smaller-diameter intercalated ducts have a small lumen and are lined by a simple cuboidal epithelium. These ducts empty into larger-diameter striated ducts, which are lined by simple columnar epithelial cells with basal infoldings, thereby pushing the nucleus into the upper half of the cell. Interlobular ducts are lined by epithelium that may be simple columnar in the smaller-diameter interlobular ducts or pseudostratified columnar or stratified columnar in the larger-diameter interlobular ducts.
Parotid Salivary Gland
The parotid salivary gland is classified as a serous gland (Figure 16-5). It is surrounded by a connective tissue capsule that sends numerous septa into the interior of the gland, subdividing it into lobules. Numerous blood vessels, adipose cells, and interlobular ducts will be found within the connective tissue septa between the lobules.
Within each lobule (Figure 16-6) are numerous serous acini, isolated adipose cells, and striated ducts.
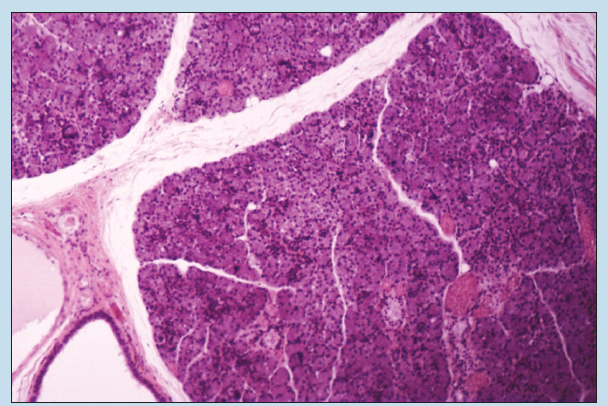
Figure 16-5 (25X): Parotid salivary gland.
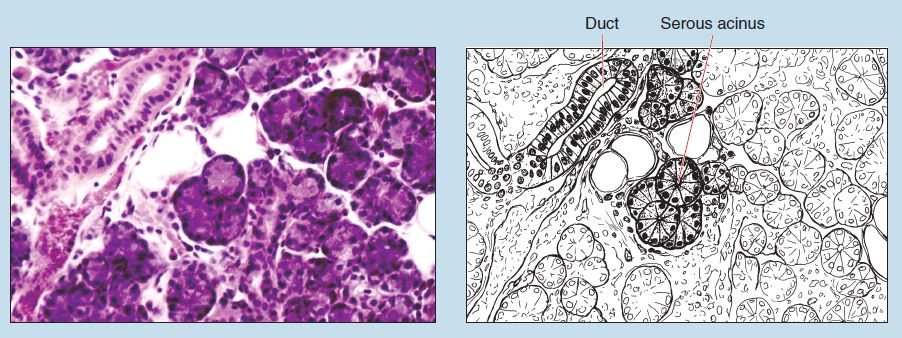
Figure 16-6 (100X): Parotid salivary gland.
Submandibular Salivary Gland
The submandibular gland (Figure 16-7) is a compound, mixed tubuloacinar gland because it is composed of mucous and serous acini. Serous acini dominate within this gland. Serous demilunes are visible within this photomicrograph.
Sublingual Salivary Gland
Like the submandibular salivary gland, the sublingual salivary gland (Figure 16-8) is a compound, mixed tubuloacinar gland composed of mucous and serous acini. However, most of the secretory acini within this salivary gland are mucous in nature.
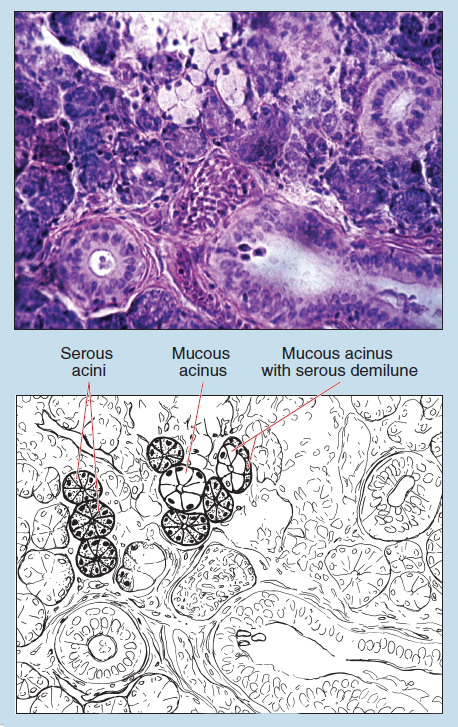
Figure 16-7 (50X): Submandibular salivary gland.
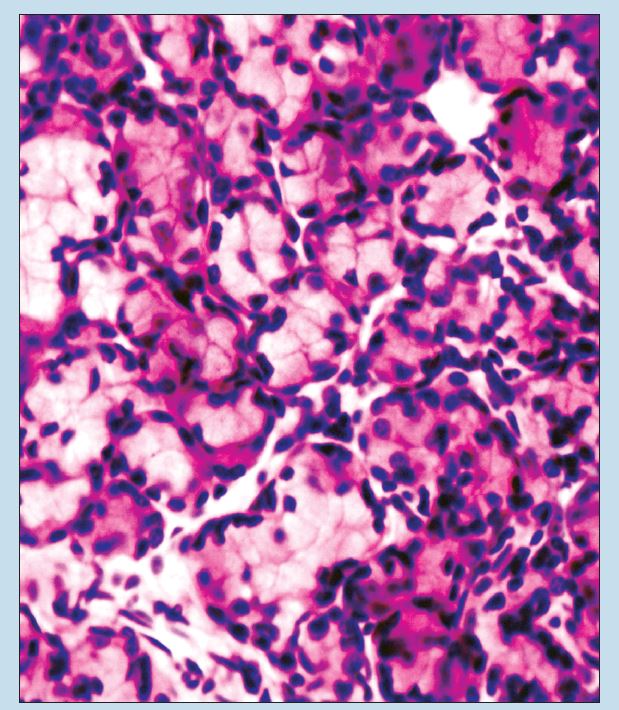
Figure 16-8 (100X): Sublingual salivary gland.
Esophagus
Note: The following descriptions and photomicrographs are of the human esophagus. The mucosa and muscularis externa will vary in specimens obtained from other animals.
The mucosa of the esophagus (Figure 16-9) is composed of a stratified squamous epithelium (mucosal type). The lamina propria is quite prominent and is interspersed with fibroblasts, fibrocytes, and macrophages (see sections on Loose, Irregularly Arranged [Areolar] Connective Tissue [mesenteric spread and lamina propria of duodenum] in Chapter 3).
The lamina muscularis (Figure 16-9) is composed mostly of longitudinally arranged smooth muscle fibers but may possess some circularly arranged fibers (see section on Smooth Muscle in Chapter 6). Esophageal glands are found within the lamina propria of the mucosa. Superior esophageal glands (which may be absent in some specimens) are found in the superior (uppermost) region of the esophagus (Figure 16-9), whereas esophageal cardiac glands are found in the inferior region (see Figure 16-11). Structurally, the esophageal cardiac glands are similar to those found within the cardiac region of the stomach.
The submucosa (Figures 16-9-16-11), which is composed of loose, irregularly arranged (areolar) connective tissue, may contain submucosal glands, blood vessels, lymphatics, and occasionally autonomic nervous system ganglia. Question: These ganglia belong to which branch of the autonomic nervous system and why?
The muscularis externa of the human esophagus has a varying composition, depending on the level of the section. The upper one fourth to one third of the esophagus (Figure 16-9) contains a muscularis externa composed of visceral striated muscle (see classification of two types of Skeletal Muscle in Chapter 6), whereas the middle one-third (Figure 16-10) is a mixture of smooth muscle and visceral striated muscle. The muscularis externa in the lower one third (Figure 16-11) is composed entirely of smooth muscle.
The adventitia (not visible in this photomicrograph) is composed of loose, irregularly arranged (areolar) connective tissue.
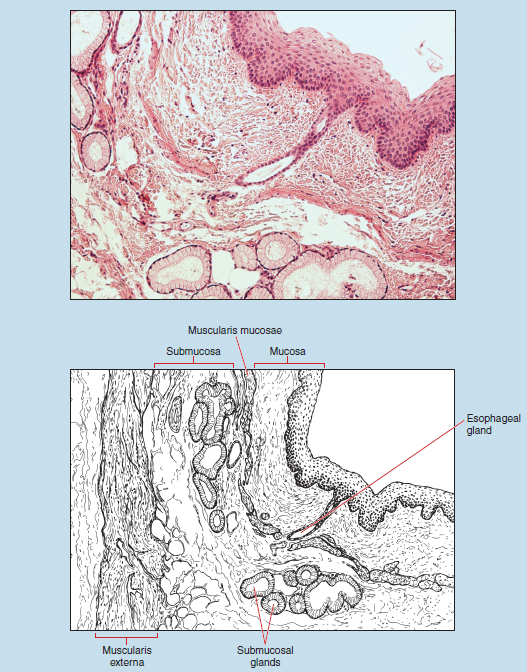
Figure 16-9 (25X): Esophagus (upper one third).
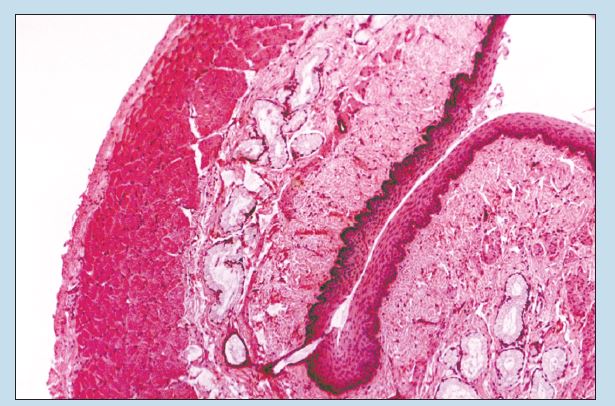
Figure 16-10 (25X): Esophagus (middle one third).
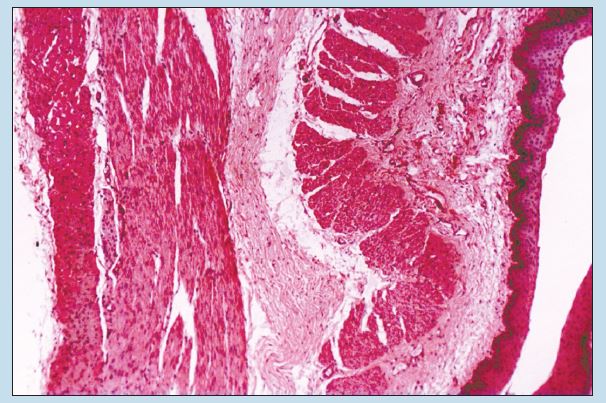
Figure 16-11 (25X): Esophagus (lower one third).
Stomach
Cardio-Esophageal Junction
Figure 16-12 shows the junction of the esophagus and stomach. This photomicrograph clearly demonstrates the abrupt histological changes that occur at the junction of the two organs. In the human esophagus, the mucosal epithelium is stratified squamous and rests on a lamina propria containing numerous papillae, whereas the mucosa of the stomach contains a surface of simple columnar epithelium and numerous tubular glands resting on a highly cellular lamina propria.
At the junction of these two organs, the lowest layer of cells from the esophageal mucosa continues on into the mucosa of the stomach. On examination of this junction during gross dissection of an unpreserved cadaver, you would see the whitish epithelium of the esophagus change into the bright pink of the stomach. This pink color is due to the superficial location of blood vessels within the lamina propria and the thinness of the epithelium.
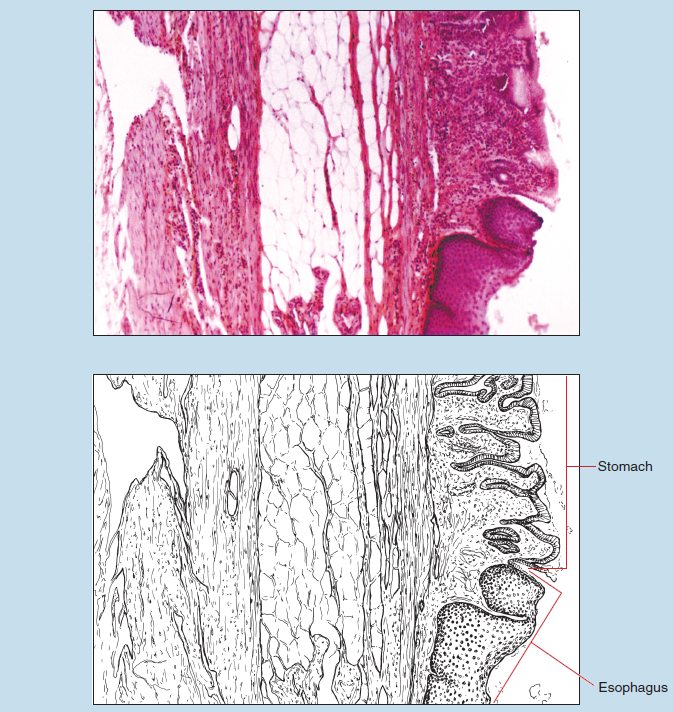
Figure 16-12 (25X): Cardioesophageal junction.
General Histological Description of the Stomach
As you read the general histology of the stomach, you should examine all of the figures in this section because some items listed in italics may be seen better in one region than another or may be seen only in a particular region of the stomach. Subsequent discussions compare the histological differences among the cardiac, fundic, and pyloric regions of the stomach.
As you examine the histology of the stomach, you should direct your attention to two main questions:
- What histological characteristics will differentiate the stomach from other hollow organs of the gastrointestinal tract?
- What histological characteristics will allow you to differentiate among the different regions of the stomach?
Start your examination of the stomach with Figure 16-13. On gross examination of the stomach you would see that the mucosa of the stomach possesses numerous gastric folds (also termed gastric rugae). In addition to the folds, the epithelium is subdivided into smaller grooves termed gastric (or mamillated) areas. These gastric areas are studded with minute depressions termed gastric pits.
The epithelium lining the inner surface of the stomach and gastric pits is composed of simple, columnar, mucous surface cells that differ structurally and functionally from those of the gastric glands. The apical end of the cells has a deep, cup-shaped zone filled with mucigen, which is not preserved in routine histological sections, thereby giving the cells a clear apical end. The single nucleus is oval or spheroidal in shape, depending on the shape of the cell and the amount of mucigen present. Short microvilli may be present on the apical surface of the cell but are not readily visible with the light microscope. As these cells extend deeper into the gastric pits, they become progressively shorter and possess less mucigen.
The lamina propria consists of a delicate interweaving of loose, irregularly arranged (areolar) connective tissue. This region of the mucosa contains the gastric glands, a major histological feature of the stomach. The glands are so numerous that the lamina propria and associated connective tissue fibers are reduced to thin strands. Scattered lymphoid nodules may be present within the lamina propria.
The muscularis mucosae are composed of a thin layer of circularly and longitudinally arranged smooth muscle.
The submucosa consists of dense, irregular connective tissue. Large blood vessels and nerve plexuses may be seen in some sections. (Note: The submucosa in Figure 16-13 is altered significantly by a fixation and sectioning artifact.)
The muscularis externa is a major histological feature of the stomach. It is composed of three separate layers of smooth muscle: inner oblique, middle circular, and outer longitudinal layers. Connective tissue separates these layers, and autonomic nervous system ganglia may be found between the three layers of smooth muscle.
The serosa consists of a layer of loose, irregularly arranged (areolar) connective tissue covered by a simple squamous mesothelium and typically is not visible in histological sections.
Beginning histology students must understand the variation in terminology between the gross anatomy of the stomach and the histological anatomy of the stomach. Gross anatomists divide the stomach into four regions: (1) cardia, or that portion found at the junction between the esophagus and the stomach; (2) fundus, the portion of the stomach that is superior to a horizontal line drawn at the junction of the esophagus and the cardia of the stomach; (3) body, that region found inferior to this horizontal line; and (4) pylorus, the narrow segment found at the junction between the stomach and the duodenum. Histologists, however, divide the stomach into only three regions, based on the type of glands found within a particular region of the stomach: (1) cardiac region, which is that region of the stomach possessing cardiac glands; (2) fundic region, the portion of the stomach containing fundic glands; and (3) pyloric region, that region of the stomach possessing pyloric glands.
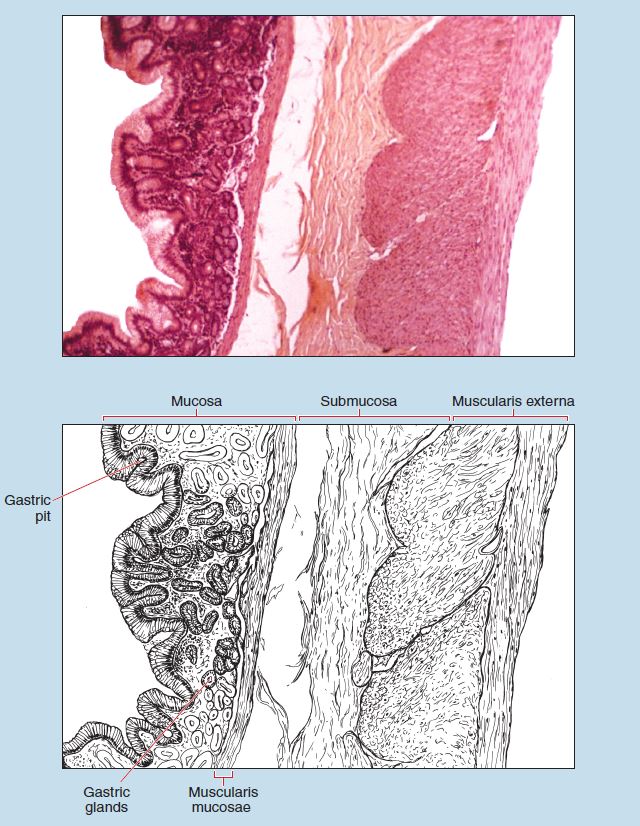
Figure 16-13 (25X): General histology of the stomach.
Cardiac Stomach
Figure 16-14 is of the cardiac region of the stomach. The surface epithelium and the composition of the glands are major histological features of this region of the stomach. The surface epithelium is a simple columnar epithelium (see section on the Simple Columnar Epithelium in Chapter 2) composed of surface mucous cells. The glands of the cardiac stomach are typically shorter than those seen in the fundic or pyloric regions. In addition, the glands of this region are composed mainly of mucous neck cells. The staining intensity of the mucous surface cells and mucous neck cells will vary, ranging from acidophilic to clear, depending on the amount of mucous that was present in the cell at the time of fixation.
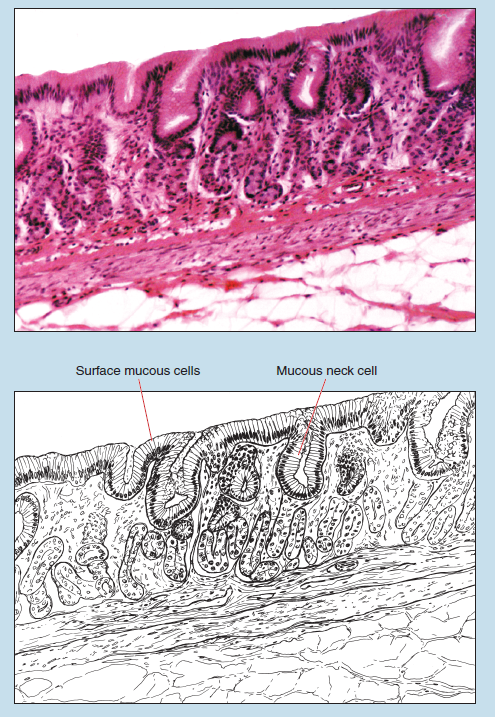
Figure 16-14 (50): Cardiac stomach.
Fundic Stomach
The transition between the cardiac and fundic regions is gradual. Histologically, the fundic stomach differs from the cardiac and pyloric regions in at least two ways (Figures 16-15 and 16-16):
- The arrangement of the muscularis externa: In the fundus the muscle bundles do not run in discrete layers; rather, they course in various directions, making the differentiation of three distinct bundles quite difficult.
- The histological appearance and cellular makeup of the gastric glands, which are termed fundic glands, differs significantly from that of the cardiac and pyloric regions.
Of these two differences, the ability to recognize the histological characteristics of the fundic glands will yield the most consistent results when you are trying to differentiate among the three regions of the stomach.
The fundic glands (Figure 16-15) are straight or slightly branched and extend downward through the entire thickness of the lamina propria to the muscularis mucosae. Three- dimensional reconstruction of these glands shows that three to seven individual gastric glands empty into a single gastric pit. Three cell types typically can be distinguished in the glands (Figure 16-16):
- Chief cells are the most numerous types of cells in the fundic glands. They are large, pyramidal cells with a single, basally located nucleus. The cytoplasm stains lightly basophilic.
- Parietal cells are often larger than chief cells and often found in the upper one third of the gland. They are oval or polygonal in shape. The nucleus is centrally located within the cell; binucleated or multinucleated cells are not uncommon. The cytoplasm is granular in appearance and stains well with acidophilic stains.
- The third cell type is the mucous neck cell. These are found interspersed among the parietal cells. They are cuboidal or low columnar in shape and contain a basally situated nucleus and finely granular cytoplasm. Mucous neck cells stain more lightly than chief cells but not as lightly as the surface epithelium.
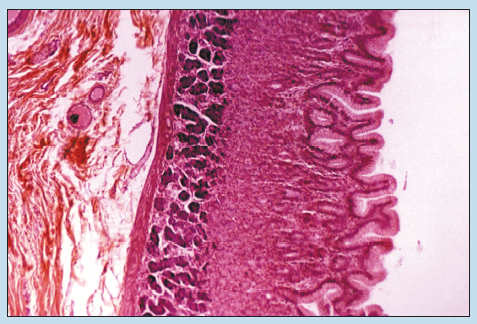
Figure 16-15 (50X): Fundic stomach.
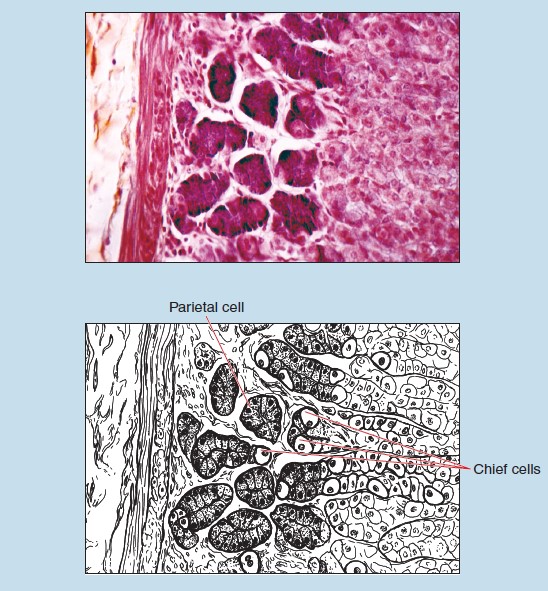
Figure 16-16 (50X): Fundic stomach.
Pyloric Stomach
The pyloric stomach contains simple, branched, tubular pyloric glands, several of which open into each pit (Figure 16-17). The pyloric glands are more tortuous than those of the cardiac or fundic regions; therefore, in any given section, more of the tubules will be in transverse or oblique section. In addition, the majority of the cells within the pyloric glands resemble mucous neck cells. Closer examination, however, will show that these cells are taller than mucous neck cells, and their nuclei generally are orientated parallel to the longitudinal axis of the gland. Again, the transition from fundic to pyloric stomach is gradual. Therefore the pyloric section on your slide may have some characteristics that are intermediate between these two regions.
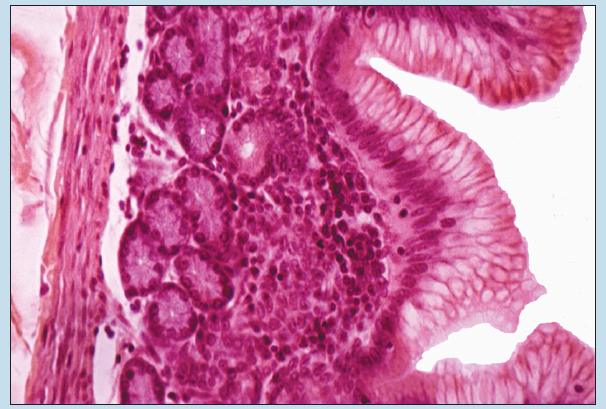
Figure 16-17 (100X): Pyloric stomach.
Small Intestine
General Histological Description of the Small Intestine
The small intestine is subdivided into three regions: duodenum, jejunum, and ileum. Histologically you can differentiate among these regions by comparing several distinct characteristics. The general characteristics of the small intestine are discussed first and should be studied using at least two of the photomicrographs in this section of the text. Only after these general characteristics are mastered should you proceed to the differences among the regions. In comparing the regions of the small intestine it is important for you to examine the photomicrographs in the order in which they are presented because the discussions build on each other.
Begin your examination of the small intestine with Figure 16-18. If you were to open the small intestine by a longitudinal incision you would see a series of definite folds running parallel to each other and passing in circular or oblique directions on the inner surface of the jejunum. These specializations of the mucosa are known as plicae circulares. The mucosa is further carried into a series of finger-like projections termed villi, which cover the entire surface of the plicae and small intestine. (Note: As you examine Figure 16-18, explain why some of the villi are represented in longitudinal section, whereas others are seen as cross section within the lumen of the organ.)
The mucosa also possesses numerous depressions termed intestinal crypts (or crypts of Lieberkuhn), which open between the villi and extend as deep as the muscularis mucosae. The simple, columnar epithelial cells of the mucosa possess a single basal nucleus and an apical brush border. Interspersed between the columnar epithelial cells you will find a varying number of goblet cells.
The muscularis mucosa is thin and composed of inner circular and outer longitudinal smooth muscle layers.
The submucosa is dense, irregular connective tissue (see section on Dense Irregular Connective Tissue in Chapter 3) containing nerves, blood vessels, and lymphoid nodules (see discussion of Diffuse Lymphoid Tissue and Lymphoid Nodules in Chapter 11).
The muscularis externa possesses two layers of smooth muscle: an inner, circularly arranged layer and an outer, longitudinally arranged layer.
As with the stomach, as you examine the histology of the small intestine you must direct your attention to two main questions:
- What histological characteristics will differentiate the small intestine from other hollow organs of the gastrointestinal tract?
- What histological characteristics will allow you to differentiate among the different regions of the small intestine?
Duodenum of the Small Intestine
In the duodenum you will note that the villi are rather low, broad, and leaf-like (Figure 16-18). Plicae circulares (not visible in this section) may or may not be seen in your section because the plicae are absent in the upper regions of the duodenum, as they begin to make their appearance near the junction with the jejunum.
There are several histological features that enable you to differentiate the duodenum from other regions of the small intestine (Figure 16-18):
- Duodenal submucosal glands (also called Brunner’s glands): Duodenal glands will be found within the submucosa of the duodenum. These are highly branched, mucous-secreting, compound tubular glands lined by a simple columnar epithelium. The ducts pass up through the muscularis mucosae and lamina propria to empty into an intestinal crypt. Although most sections of the duodenum contain duodenal glands, you must keep in mind that the most inferior portions of the duodenum may contain a reduced number of these glands; therefore they may be absent from your section.
- The number of goblet cells: Goblet cells increase in number as you progress from the duodenum to the jejunum and ileum. Of the three regions of the small intestine, the duodenum therefore will have the fewest number of goblet cells and the ileum will have the most.
- Shape of the villi: As mentioned earlier, the villi of the duodenum are rather low, broad, and leaf-like. Although the difference in the shape of the villi is difficult to distinguish at first, this is a good histological feature that may be used to confirm your identification of the specimen.
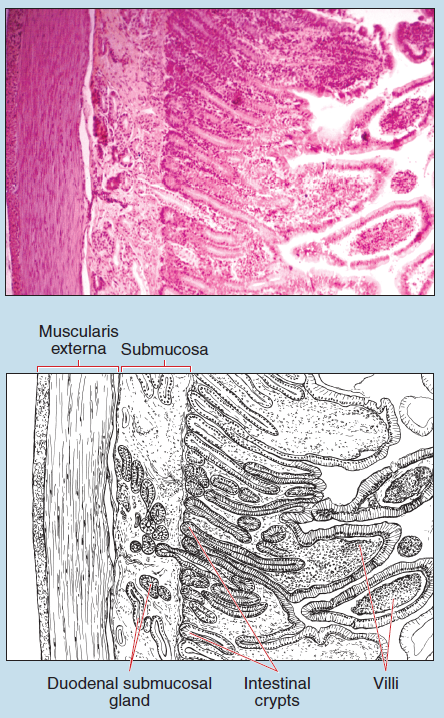
Figure 16-18 (25X): Duodenum of the small intestine.
Jejunum of the Small Intestine
This photomicrograph shows the wall of the jejunum of the small intestine (Figure 16-19). Identification of the jejunum is based on the following characteristics:
- Shape of the villi: The villi are taller and more slender in the jejunum than in any other region of the small intestine.
- Plicae circulares: The jejunum demonstrates a more extensive development of the plicae circulares.
- Number of goblet cells: You note more goblet cells in the mucosa of the jejunum than in the duodenum.
- Absence of duodenal glands: The jejunum lacks duodenal glands and, as you have already learned, the absence of a structure may sometimes be just as valuable in making a correct identification as is the presence of another histological structure.
Ileum of the Small Intestine
Figure 16-20 shows the mucosa and submucosa of the ileum of the small intestine. Following are four major identifying features that help to differentiate the histology of the ileum from that of the duodenum and jejunum:
- Shape of the villi: Within the ileum you will find short, clubshaped villi.
- Plica circulares: The plicae are reduced in size in the ileum.
- Number of goblet cells: You will find a greater accumulation of goblet cells within the mucosal epithelium of the ileum than in any other region of the small intestine.
- Aggregated Lymphoid Nodules: You will note the presence of aggregated lymphoid nodules (also termed Peyer’s Patches) (see section on Aggregated Lymphoid Nodules in Chapter 11) within the lamina propria. These patches are an aggregation of lymphoid nodules on the side of the ileum opposite the attachment of the mesentery.
On gross dissection of the ileum you will note that the mucosa immediately superficial to the aggregated lymphoid nodules is devoid of villi. Histological examination of that portion of the mucosa demonstrates that a single layer of columnar epithelium (without goblet cells) separates the nodules from the gut lumen. (Note: Is this visible in Figure 16-20? If not, what would be an accurate, histological reason for the appearance of this photomicrograph?)
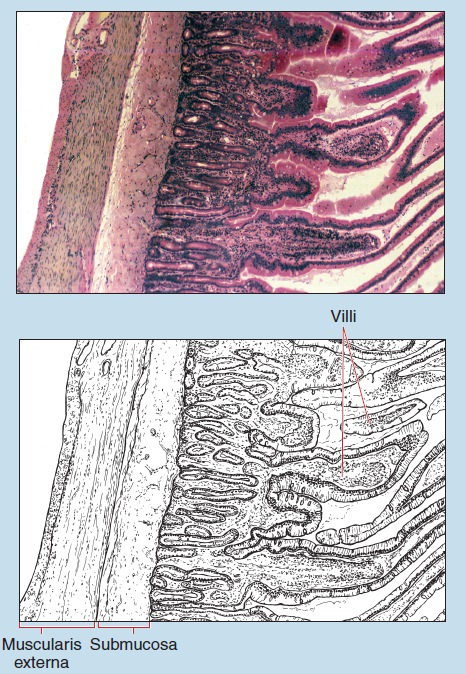
Figure 16-19 (25X): Jejunum of the small intestine.
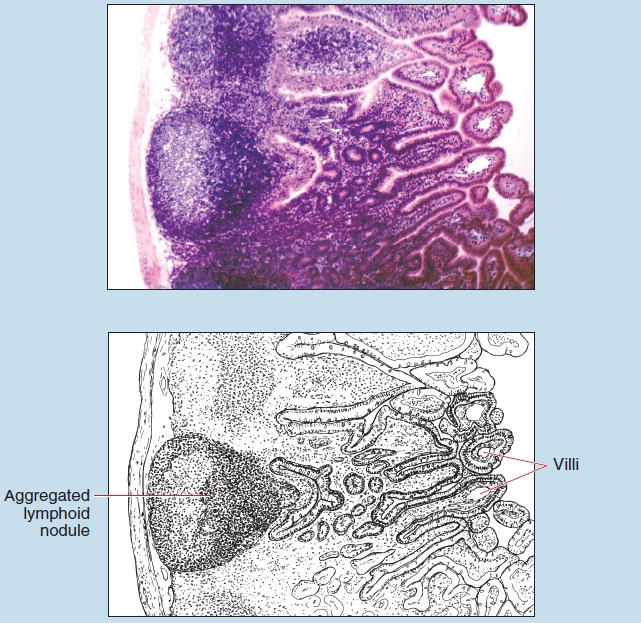
Figure 16-20 (25X): Ileum of the small intestine.
Colon
Figure 16-21 shows the mucosa and submucosa of the colon (large intestine). Note the fixation artifact that has caused a significant increase in the depth of the submucosa.
The mucosa of the large intestine is comparatively smooth when compared with that of the small intestine in that the large intestine lacks plicae or villi. The surface epithelium of the large intestine is composed of a simple columnar epithelium with numerous goblet cells.
Long, straight, tubular glands extend from the surface down through the entire thickness of the mucosa. The lamina propria of the mucosa is reduced to a minimum because of the close proximity of the glands. Solitary lymphoid nodules (see section on Lymphoid Nodules in Chapter 11) and isolated lymphocytes may be seen in the lamina propria of some preparations.
A muscularis mucosae composed of inner, circularly arranged and outer, longitudinally arranged smooth muscle is present. The submucosa is composed of dense, irregular connective tissue.
In humans, the muscularis externa (not visible on this photomicrograph) contains a complete inner, circular layer of smooth muscle and an outer, incomplete layer of longitudinally arranged smooth muscle termed the taeniae coli. Why is the arrangement of the muscularis externa not a reliable diagnostic feature for the colon?
The serosa (not visible in this photomicrograph) is a thin layer of connective tissue covered by a mesothelium.
As you compare the histology of the large intestine to that of the three regions of the small intestine, the following characteristics will serve as major identification features for the colon:
- Number of goblet cells: The mucosa of the large intestine has a significantly greater number of goblet cells than any region of the small intestine.
- Lack of villi and plicae circulares: The mucosa of the large intestine does not possess surface villa or plicae circulares.
- Absence of duodenal glands and aggregated lymphoid nodules: Although these structures are not found in every region of the small intestine, their absence in a specimen, when combined with the other characteristics mentioned above, may aid in confirming your identification of the large intestine.
Anorectal Junction
The histology of the rectum is nearly identical to that of the colon in that the same layers and sublayers are present. However, the rectum demonstrates at least four subtle differences when compared with the colon, as follows:
- The mucosa is deeper than that of the colon.
- The mucosal glands of the rectum are shorter than those of the colon.
- More goblet cells are present in mucosa of the rectum.
- The proximal (upper) portion of the rectum possesses transverse rectal folds.
The anal canal, which is distal to the rectum, may be subdivided into the following three regions or zones:
- Colorectal zone: This area possesses a mucosa composed of a simple columnar epithelium similar to that seen within the distal segments of the colon. The colorectal zone occupies approximately the proximal one third of the anal canal.
- Anal transitional zone: This zone occupies the middle one third of the anal canal and demonstrates a transitional region between the simple columnar epithelium of the colon and the stratified squamous epithelium of the perianal skin. The anal transitional zone possesses a stratified columnar epithelium.
- Squamous zone: Here the mucosal epithelium is a stratified squamous epithelium that becomes continuous with the skin of the perianal region.
Figure 16-22 demonstrates an area of transition between the rectal and anal canals.
The proximal (upper) portion of the anal canal also possesses longitudinal folds, termed anal columns, which are not visible on this photomicrograph. If anal columns are visible on your specimen, the depressions between the anal columns are termed anal sinuses.
If the muscularis externa is present on your specimen, you will note a marked thickening, which represents the internal anal sphincter (not visible on this photomicrograph).
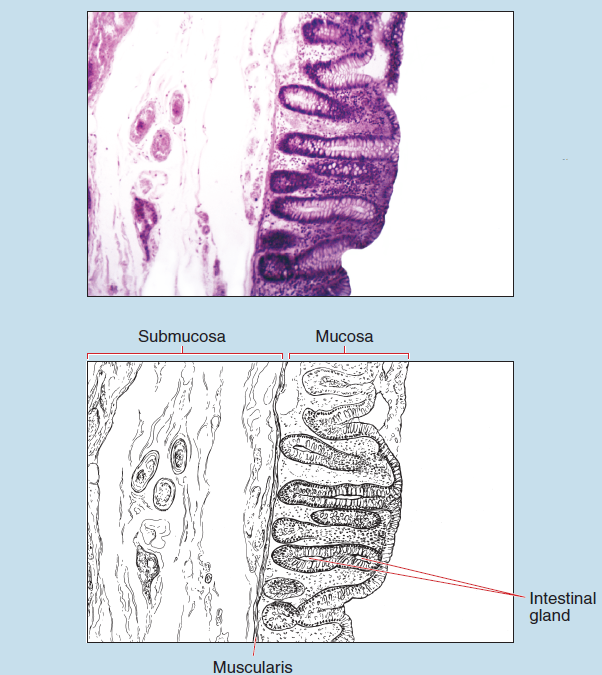
Figure 16-21 (25X): Colon.
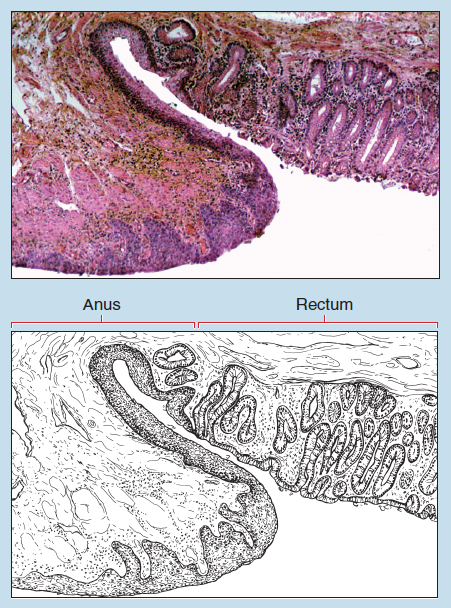
Figure 16-22 (25X): Rectal-anal junction.
Appendix
As you begin your examination of the appendix (Figure 16-23), the first thing you will notice is that the lumen of the appendix varies in size and shape, and is frequently occluded as a result of fibrosis in adults. However, if a patent lumen is present, it is small and cleft-like in cross section. The shape of the lumen may also change with age, being three-horned in youth and slit-like, circular, or another shape in the adult.
Further examination demonstrates that the appendix possesses the same four layers as the other tubular organs of the digestive tract (Figure 16-23). The mucosa of the appendix lacks villi and is composed of a simple columnar epithelium, crypts, a lamina propria, and a muscularis mucosae. The glands of the appendix may be more branched than those of the colon.
The lamina propria contains a large amount of lymphoid tissue in the form of numerous lymphoid nodules that, like the shape of the lumen, is a major histological feature of the appendix. In addition, the muscularis mucosae is poorly developed because of the large amount of lymphoid tissue.
Numerous adipose cells may be found within the submucosa.
The muscularis externa contains two complete layers of smooth muscle: an inner, circularly arranged layer and an outer, longitudinally arranged layer.
A typical serosa is present but may not be visible on your preparation.
Gallbladder
The wall of the gallbladder (Figure 16-24) is composed of only three layers; this is a major histological feature of this organ.
The mucosa has numerous folds that divide the surface into irregular polygonal areas. The surface epithelium is composed of simple columnar cells with oval nuclei. Mucosal crypts (also termed Rokitansky-Aschoff sinuses) are another major histological feature of the gallbladder. These are diverticula of the mucosa that extend into the muscular and perimuscular areas. The epithelium of these sinuses is a continuation of the surface epithelium.
The lamina propria is composed of loose, irregularly arranged (areolar) connective tissue containing extensive vascular plexuses and a few scattered muscle cells. A muscularis mucosae and submucosa are lacking.
The muscularis externa is composed of interlacing bundles of smooth muscle. Longitudinal fibers will be found closer to the lamina propria, whereas the remainder of the muscularis externa is circularly arranged. Connective tissue is found between the individual bundles.
A typical serosa is found external to the muscularis but only on the surface that is not attached to the liver.
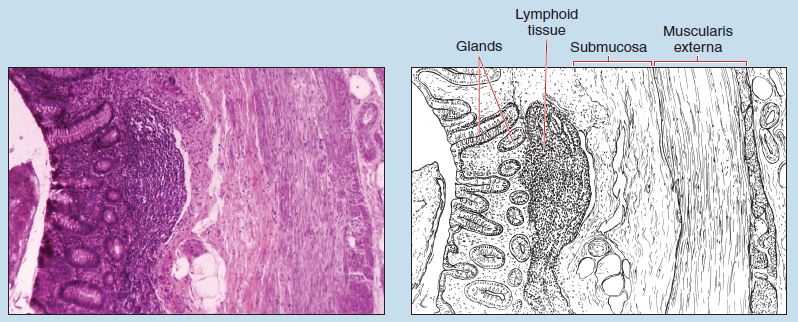
Figure 16-23 (25X): Appendix.
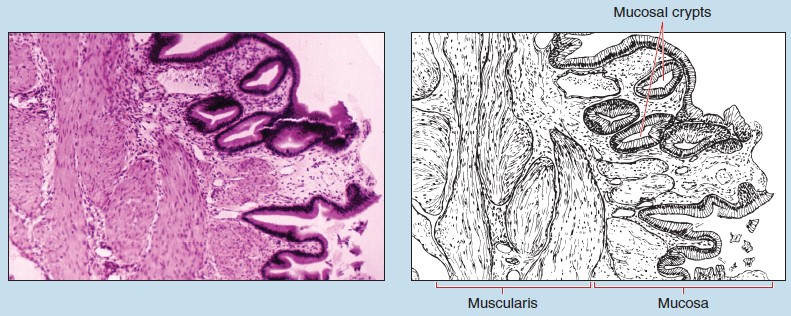
Figure 16-24 (25X): Gallbladder.
Pancreas
The pancreas (Figure 16-25) is a compound tubuloacinar gland with both endocrine and exocrine functions. The organ is covered with a thin layer of loose, irregularly arranged (areolar) connective tissue, not visible in this photomicrograph, and typically is not seen on histological preparations. No true capsule is present. Delicate septa radiate inward, subdividing the organ into lobules.
The duct system of the pancreas is composed of intercalated ducts, intralobular ducts, interlobular ducts, and the main pancreatic duct. The pancreas is unique in that the intercalated ducts, which are not visible on this photomicrograph, actually begin within the acini of the pancreas. Centroacinar cells (not visible on this photomicrograph), which are the initial cells of the intercalated ducts, are located within the serous acini of the pancreas. These ducts are quite short and drain into the intralobular ducts of the pancreas (not visible on this photomicrograph).
Intralobular ducts drain into interlobular ducts, which are lined with a tall, simple cuboidal or simple columnar epithelium resting on a distinct basal lamina (see section on Epithelial Sheets in Chapter 2). Occasionally goblet cells may also be found in the epithelium of these interlobular ducts.
The main excretory duct of the pancreas extends the entire length of the organ, receiving small branches, typically one per lobule. These lobular ducts (not visible in this photomicrograph) are lined by a simple cuboidal epithelium.
Pancreatic acini are all serous in composition. These acini possess a minute central lumen that may or may not be seen on high-dry objective, depending on the plane of section of your specimen.
At this time you should also review the histological discussion of the endocrine pancreas (see the section on the Endocrine Pancreas in Chapter 13), as well as Figure 13-13.
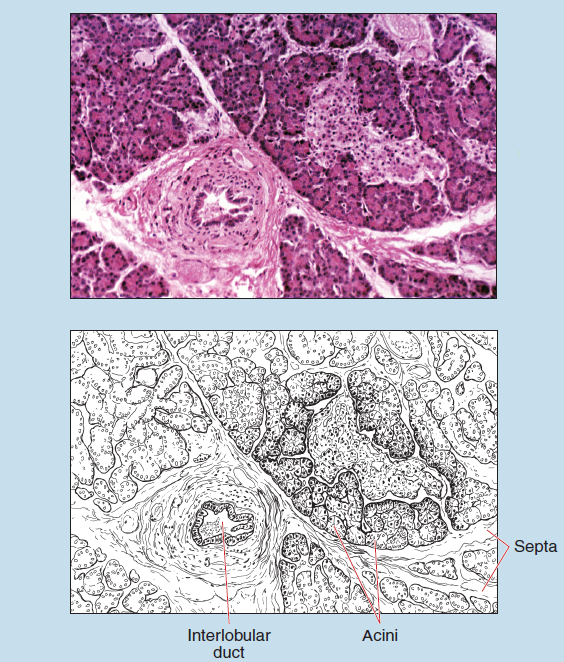
Figure 16-25 (25X): Pancreas.
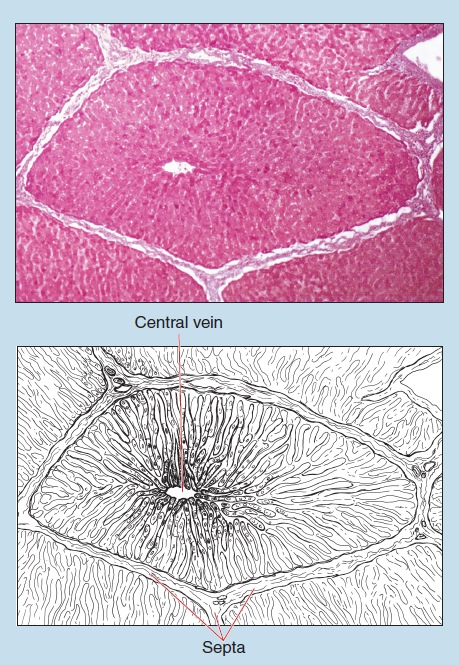
Figure 16-26 (25X): Liver.
Liver
The specimen in these photomicrographs was obtained from a pig and is used to demonstrate more clearly the connective tissue of the hepatic lobule. Distinct connective tissue septa, dividing the liver into clearly defined lobules, is not seen in most animals, including humans.
Histologists may use any one of three ways to discuss the functional unit of the liver—the liver acinus, portal lobule, or classic lobule. The classic lobule is the one described in this text because it is traditionally used to describe the liver and is also the easiest to visualize with the light microscope. The structure of the classic lobule is based on the branches of the portal vein and hepatic artery, as well as the pathway that blood would follow as it perfuses the parenchyma of the liver.
The liver is contained within a delicate connective tissue capsule (not visible in this photomicrograph and typically not seen on histological preparations) from which delicate septa radiate inward, forming the framework for the parenchyma and dividing the liver into lobules (Figure 16-26). At the hilus, the capsule surrounds the entering and exiting blood vessels.
The classic hepatic lobule (see Figure 16-26) has a central vein from which liver parenchymal cells, termed hepatocytes, radiate outward like spokes of a wheel. Hepatocytes are arranged into irregular, branching, and interconnected plates termed hepatic cords (Figure 16-27). These hepatocytes are polyhedral in form, with sharply defined lateral and basal borders. The single central nucleus possesses one or more prominent nucleoli. Although they are not visible in this photomicrograph, when adjacent hepatocytes are viewed under oil immersion bile canaliculi may be visible as a small, pale, circular profile.
At the periphery of the classic liver lobule you will find hepatic triads (Figure 16-27) contained within the connective tissue of the lobule. The hepatic triad contains an interlobular bile duct, interlobular artery (which is a branch of the hepatic artery), and an interlobular vein (a tributary to the hepatic portal vein). A lymphatic vessel may also be present. The interlobular bile duct is easily recognized by its simple cuboidal epithelium. The interlobular artery and vein exhibit the characteristic histological characteristics of arteries and veins (see sections on Arteries and Veins in Chapter 8).
Hepatic sinusoids are abundant between the hepatocytes. These sinusoids make up the intralobular system of capillaries bathing the hepatic cords. By using either the high-dry or oilimmersion objective, you should be able to discern the thin endothelial layer making up the walls of the sinusoids. Between the hepatocytes and sinusoids is a connective tissue space of variable dimensions. This space is termed the perisinusoidal space (also termed the space of Disse), which is known to contain reticular fibers, occasional perisinusoidal cells, Kupffer cells (macrophages), and hepatocytic microvilli.
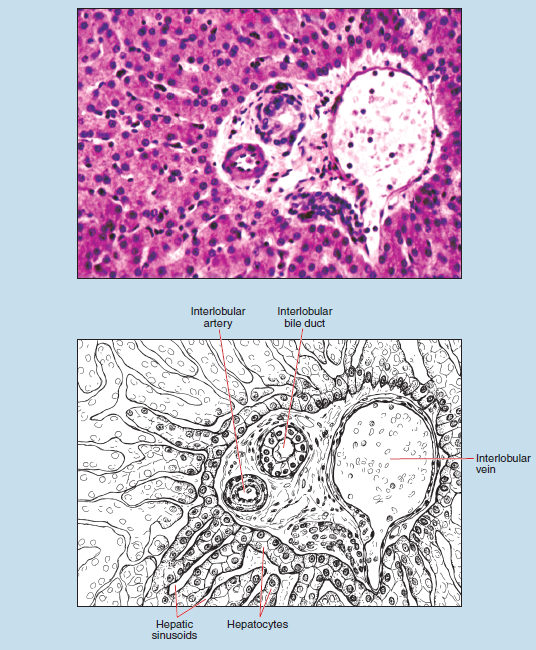
Figure 16-27 (100X): Hepatic triad within the liver.
Commonly Misidentified Tissues
Cardiac, Fundic, and Pyloric Stomach
The gastrointestinal system has a large number of look-alike tissues. The majority of these involve different sections of the same organ (e.g., cardiac vs. fundic stomach).
By comparing cardiac, fundic, and pyloric regions of the stomach you will note that there are distinct but subtle differences among all three regions.
Cardiac Stomach (Review Figure 16-14 in section on the Cardiac Stomach)
-
- Segment of esophagus often found on section
- Gastric glands shorter than other stomach regions
- Parietal and chief cells lacking or found infrequently
Fundic Stomach (Review Figure 16-15 and 16-16 in section on the Fundic Stomach)
-
- Gastric glands usually longer than in any other region of the stomach
- Parietal and chief cells prominent in lower portions of the gland
- Largest portion of the stomach and therefore the most frequently encountered gastric region
Pyloric Stomach (Review Figure 16-17 in section on the Pyloric Stomach)
-
- Segment of duodenum often found on section
- Mucous cells occupy more than half of the epithelium found within the gastric glands
- Parietal and chief cells lacking or found infrequently