Chapter Objectives
This chapter will enable you to discuss and identify:
-
- The various components of the kidney that may be distinguished with the light microscope
- The components of the juxtaglomerular apparatus
- The urinary bladder
- The ureter
- The female urethra and the spongy and prostatic segments of the male urethra
The functions of the urinary system are the formation of urine, fluid balance, the regulation of blood pressure and acid-base balance, and the formation of specific hormones. All of these functions are accomplished by a series of structures found within the kidneys. The remaining structures of the urinary system, termed the extrarenal excretory structures, are the ureters, urinary bladder, and urethra. These structures are responsible for the passage of urine from the kidney to the external environment.
Kidney
When you view the kidney at scanning power you will note the following histological characteristics:
- The kidney is covered by a fibroelastic capsule.
- The kidney is divided into a cortex and medulla.
- The border between renal cortex and renal medulla is marked by the presence of arcuate arteries and veins.
- Renal corpuscles and segments of the uriniferous tubules are found within the renal cortex.
- The medulla, although lacking renal corpuscles, does contain segments of the uriniferous tubules.
Renal Corpuscle
The capsule of the kidney, which is not visible in these photomicrographs, is composed of fibroelastic connective tissue. The kidney is subdivided into cortex and medulla, which contain the uriniferous tubules of the kidney. Each uriniferous tubule is composed of a nephron and a collecting duct. The nephron begins as a double-walled epithelial cup composed of the glomerular capsule (also termed Bowman’s capsule) surrounding a tuft of capillaries termed the glomerulus. Both structures together form the renal (Malpighian) corpuscle.
The glomerular capsule (Figures 12-1 and 12-2) is composed of two continuous, simple squamous epithelial layers (see section on Simple Cuboidal and Simple Squamous Epithelia in Chapter 2). The inner visceral layer covers and closely invests the glomerular capillaries. The cells of this visceral layer are termed podocytes. In these photomicrographs, they are seen facing capsular space (also termed the urinary or Bowman’s space).
Although it is not visible in Figures 12-1 to 12-3, the visceral layer of the renal corpuscle is continuous with the parietal layer at the vascular pole. The parietal layer (Figure 12-3) of the renal corpuscle is composed of a simple squamous epithelium resting on a thin basal lamina. A thin layer of connective tissue surrounds it externally. The cells of the parietal layer are more uniform in thickness than those of the visceral layer.
In Figure 12-3, the urinary pole may be seen where the simple squamous epithelium of the parietal layer of the glomerular capsule is joined by the simple cuboidal epithelium of the proximal convoluted tubule.
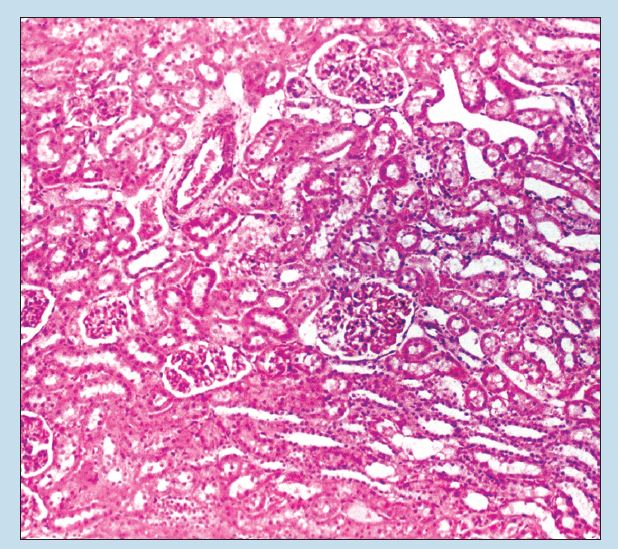
Figure 12-1 (25X): Renal corpuscle.
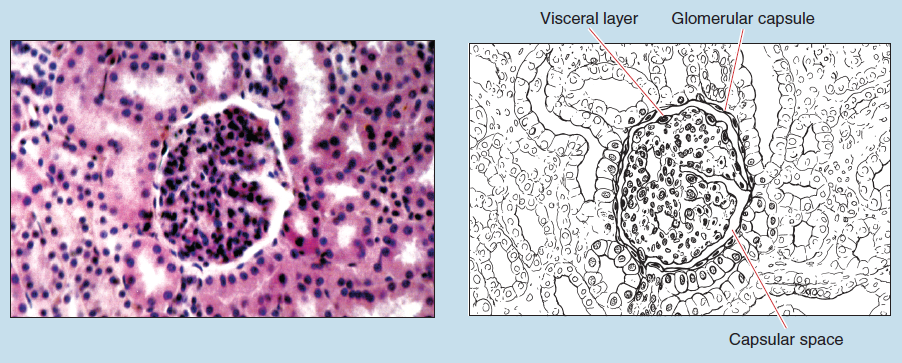
Figure 12-2 (100X): Renal corpuscle.
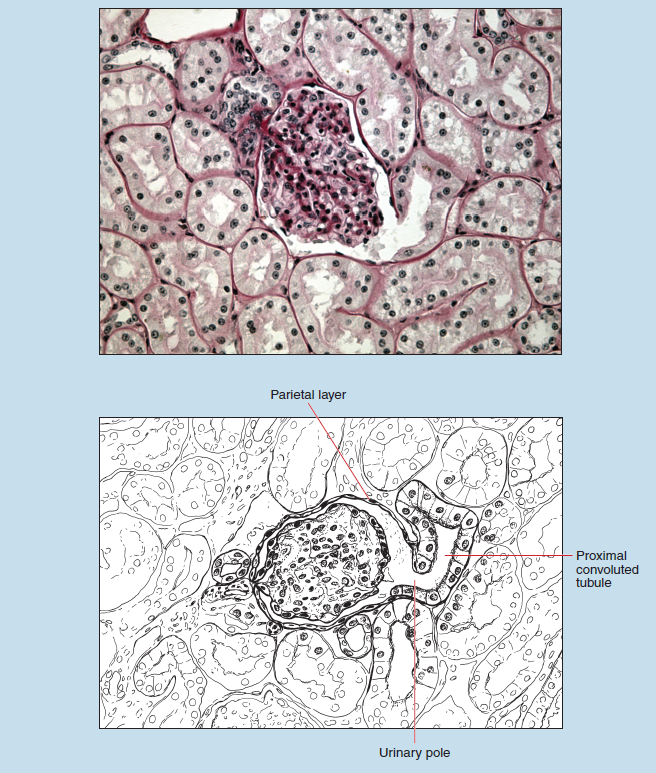
Figure 12-3 (250X): Renal corpuscle.
Proximal and Distal Convoluted Tubules
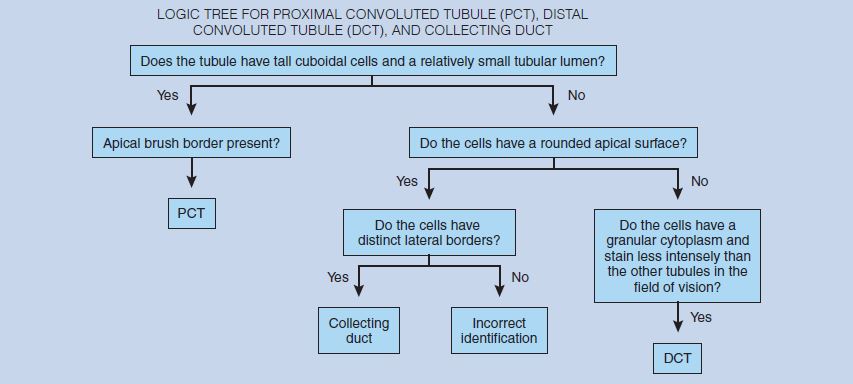
The tubular region of the nephron is composed of the proximal convoluted tubule, thick and thin segments of the nephron loop (loop of Henle), and the distal convoluted tubule. The proximal convoluted tubule (PCT) (Figure 12-4) is the longest and most convoluted segment of the nephron. Therefore the majority of the tubules found in the cortex will be PCT segments.
The PCT (Figure 12-4) is composed of simple cuboidal (or short columnar) epithelial cells. These cells possess a single, round nucleus in the basal portion of the cell, surrounded by granular, acidophilic cytoplasm. The lateral cellular boundaries of these cells are difficult to discern. Another characteristic of the PCT is a rounded, apical brush border that may be seen with high-dry or oil-immersion objectives. Because of these overall characteristics, the PCT possess a small tubular lumen and a sparse distribution of nuclei around the circumference of the tubule; these are two important histological characteristics.
The distal convoluted tubule (DCT) (Figure 12-4) is composed of a simple cuboidal epithelium. These cells also possess a granular cytoplasm but stain less intensely than those of the PCT. No brush border is visible on the apical portion of these cells. The overall size of the DCT cell is smaller, as evidenced by a larger tubular lumen. In addition, more nuclei are usually visible in the DCT.
The proximal convoluted tubule (PCT) and distal convoluted tubule (DCT) may be distinguished from each other by the following histological features:
- The PCT stains more intensely acidophilic.
- The cells of the PCT are cuboidal or short columnar epithelial cells, whereas those of the DCT are a shorter, cuboidal epithelium. Therefore the lumen of the PCT will be smaller than that of the DCT.
- The cells of the PCT have a prominent brush border on their apical surfaces. As a result of the close approximation of the brush borders of adjacent PCT cells, the lumen often appears to be occluded or star shaped.
Juxtaglomerular Apparatus
The juxtaglomerular apparatus (JGA) is found within the renal cortex of the kidney. It is located where the distal convoluted tubule comes into close proximity with the afferent glomerular arteriole at the vascular pole. The juxtaglomerular apparatus is composed of three cell types: macula densa cells, juxtaglomerular epithelioid cells, and extraglomerular mesangial cells.
The macula densa cells (Figure 12-5) are modified cells of the distal convoluted tubule (see Figure 12-4). They are taller and more rounded than other cells of the DCT and possess apical nuclei. Macula densa cells usually stain more acidophilic than the other DCT cells within the same tubule.
The second cell type, found where the afferent glomerular arteriole comes into close proximity to the macula densa, is termed the juxtaglomerular epithelioid cell. These cells are found within the wall of the afferent glomerular arteriole, where they form a collar within the tunica media. They are modified smooth muscle cells (see section on Smooth Muscle in Chapter 6) in that they are larger and more epithelioid in appearance than the other smooth muscle cells within the tunica media of the same arteriole.
The final cell type of the JGA is the extraglomerular mesangial cell (not visible on this photomicrograph). It is found between the afferent and efferent glomerular arterioles and therefore will be visible only in sections containing both arterioles. These cells are modified smooth muscle cells.
Collecting Duct (Collecting Tubule)
The collecting ducts (collecting tubules) may be found within the renal cortex; however, they are most numerous within the renal medulla (Figure 12-6). Cells of the collecting duct range in height from simple cuboidal to simple columnar (see section on Simple Columnar Epithelium in Chapter 2). The intercellular borders are quite distinct; the cells possess a rounded apical surface and stain less intensely than the other renal tubules.
The cells of the collecting duct may be distinguished from cells of the PCT (see section on the Proximal and Distal Convoluted Tubules in this chapter) and DCT by the following major histological features:
- Most segments of the collecting duct will be found within the medulla of the kidney, whereas proximal (PCT) and distal convoluted tubules (DCT) are most commonly seen within the renal cortex.
- Cells of the collecting duct tend to be smaller than those of the PCT or DCT.
- Cells of the collecting duct possess a rounded, apical surface, as do those of the PCT. However, cells of the collecting duct are considerably smaller than those of the PCT.
- Cells of the collecting duct stain less intensely than those of the PCT or DCT and lack the distinct brush border seen in cells of the PCT.
- Cells of the collecting duct have distinct intercellular boundaries that are not seen in the PCT or DCT.
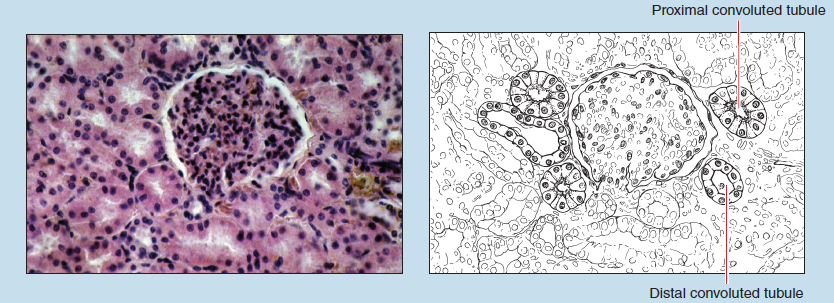 Figure 12-4 (100X): Proximal and distal convoluted tubules.
Figure 12-4 (100X): Proximal and distal convoluted tubules.
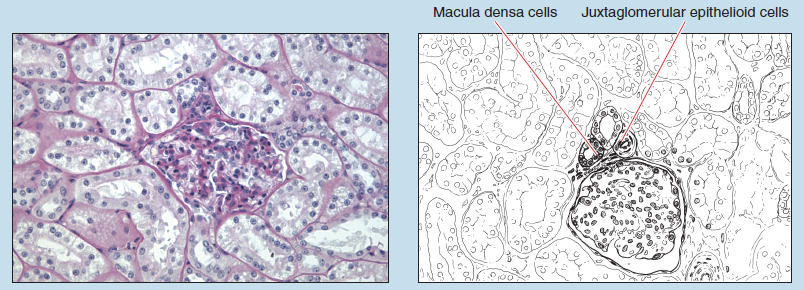
Figure 12-5 (100X): Juxtaglomerular apparatus.
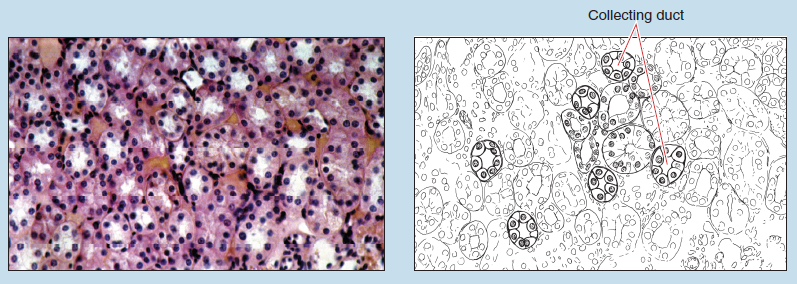
Figure 12-6 (100X): Collecting duct.
Nephron Loop
Figure 12-7 is of the medulla of the kidney. The thin limb of nephron loop (loop of Henle) is lined by a simple squamous epithelium. The nuclei of these cells bulge into the lumen of the tubule and appear somewhat less flattened than the nuclei of the adjacent endothelial cells of the vasa recta.
Ureter
The ureter and renal pelvis, and its subdivisions, constitute the main excretory ducts of the kidney. The walls of the ureter are composed of three layers: an inner mucosa, a middle muscularis, and an outer adventitia. Because of the high content of elastic fibers within the wall of the ureter, the lumen is quite often star shaped.
The mucosa of the ureter (Figure 12-8) is lined by a transitional epithelium (see section on Transitional Epithelia in Chapter 2) sitting on a thin basal lamina that is not discernible with the light microscope. Diffuse lymphoid tissue (see section on Diffuse Lymphatic Tissue in Chapter 11) may be present within the lamina propria.
The muscularis in the upper two thirds of the ureter is composed of two layers of smooth muscle—an inner longitudinal and outer circular layer. In the inferior one third of the ureter, an additional layer might be present, represented by a discontinuous outer longitudinal layer of smooth muscle.
The adventitia is composed of areolar connective tissue with numerous blood vessels. It may not be present in all sections.
Urinary Bladder
Urinary Bladder (Relaxed)
The wall of the urinary bladder is quite similar to that of the ureter, except for the increased thickness of the muscularis.
The mucosa of the urinary bladder (Figures 12-9 and 2-15) is composed of a transitional epithelium (see Figure 2-15) resting on a thin basal lamina and a lamina propria. The mucosa may be thrown into folds or may be comparatively smooth, depending on the state of stretch of the organ at the time of fixation.
The muscularis is rather thick, possessing three layers of smooth muscle: inner and outer longitudinal layers and a middle circular layer. This is a major histological feature of the urinary bladder. The fiber bundles are arranged in anastomosing bundles with connective tissue between the layers.
The adventitia of the lower bladder (if visible in your section) is identical to that of the ureter, whereas that of the upper two thirds possesses an outer serosa composed of a mesothelium and loose connective tissue.
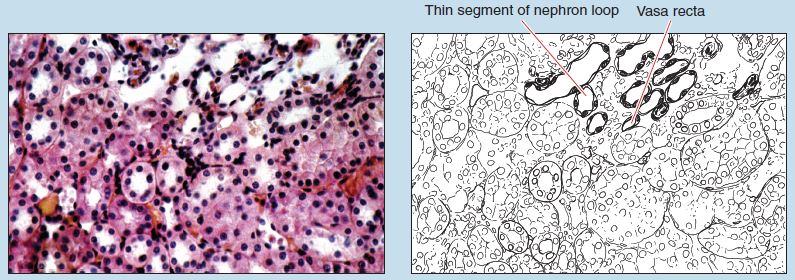 Figure 12-7 (100X): Thin segment of the nephron loop (of Henle).
Figure 12-7 (100X): Thin segment of the nephron loop (of Henle).
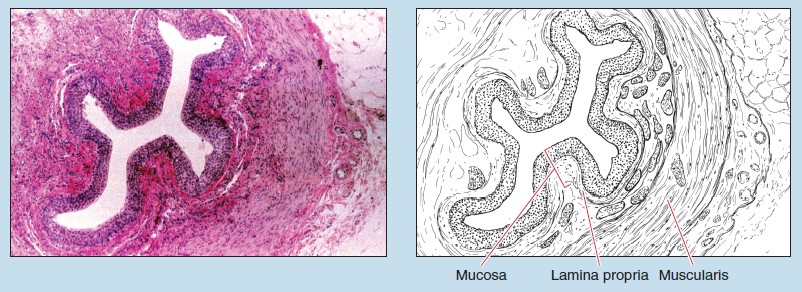
Figure 12-8 (25X): Ureter (cross section).
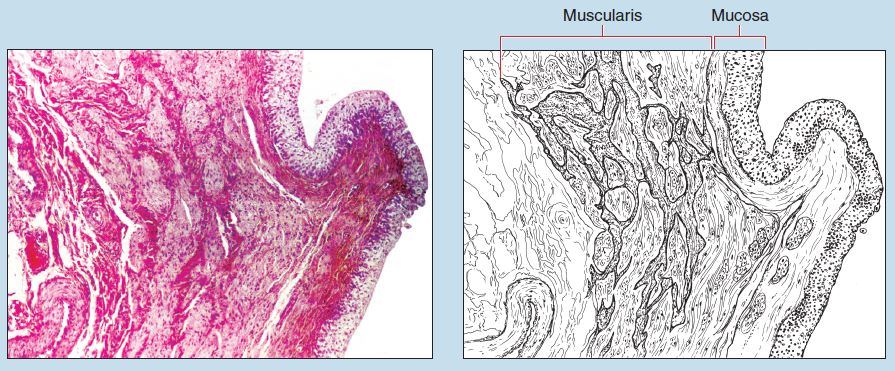 Figure 12-9 (25X): Urinary bladder (relaxed).
Figure 12-9 (25X): Urinary bladder (relaxed).
Urinary Bladder (Distended)
In the distended urinary bladder, the transitional epithelium may be reduced to as few as three layers of epithelial cells. Note that the superficial layer of cells in Figure 12-10 are squamosal in shape, whereas the deeper epithelial cells are quite variable in shape. Compare Figures 12-10 and 2-15 to note the differences between the transitional epithelium of a relaxed bladder and that of a distended bladder. Because the most superficial layers of epithelial cells in a distended urinary bladder do not possess the “typical” transitional epithelium shape (described as dome shaped, balloon shaped, broadly cuboidal, or somewhat flattened) the identification of a distended urinary bladder must be based on the three layers of smooth muscle found within the muscularis of the bladder.
Urethra
Male
Prostatic Urethra
The male urethra is subdivided into three regions: prostatic urethra, intermediate part of the urethra (membranous urethra), and spongy urethra. Figure 12-11 is a photomicrograph of the prostatic urethra.
The mucosa of the prostatic urethra possesses a transitional epithelium resting on a lamina propria that consists of fibroelastic connective tissue with prominent venous sinuses. The lumen of the prostatic urethra is irregular in shape because of the folding of the mucosa.
Throughout the entire length of the male urethra, numerous outfoldings of the mucosa may be seen. These are the urethral glands (glands of Littré). In the prostatic urethra, these branched, tubular glands extend for variable distances into the stroma of the prostate gland.
The muscularis (which is not clearly visible on this photomicrograph) consists of two indistinguishable layers: an inner longitudinal and an outer circular layer of smooth muscle. The adventitia (also not visible) is composed of fibroelastic areolar connective tissue.
Although the histology of the prostate is not discussed until Chapter 14, note its general histological organization, because the presence or absence of the prostate will aid you in your identification of male and female urethra specimens.
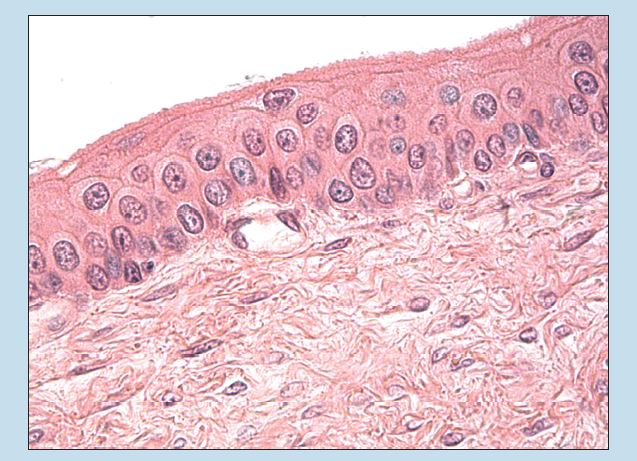
Figure 12-10 (40X): Urinary bladder (distended).
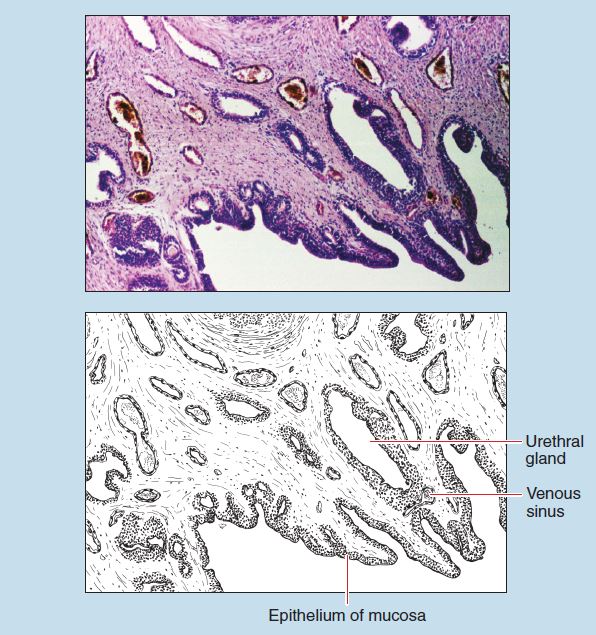
Figure 12-11 (25X): Male prostatic urethra.
Penis/Spongy Urethra
Figure 12-12 is a line drawing of a human penis. The spongy urethra is found within the inferior, medial erectile body of the penis. The presence of erectile bodies is a major histological feature of the spongy urethra.
This section is from a human penis. Other slides used for specimens of the spongy urethra may have been obtained from animals possessing an os penis, identified by the presence of bone within the section.
The epithelium of the mucosa (Figure 12-13) within the spongy urethra varies from location to location, from stratified columnar to pseudostratified columnar (see sections on Stratified Columnar Epithelium and Pseudostratified Columnar Epithelium in Chapter 2). Smooth muscle fibers may be found within the mucosa. A lamina propria of fibroelastic connective tissue is found immediately deep to the epithelium. The mucosa of the spongy urethra possesses urethral glands (glands of Littré; not visible on this section), which may extend deep into the stroma and penetrate into the corpus spongiosum.
Although the histology of the penis is not discussed until Chapter 14, note its general histological organization. The presence or absence of the penis will aid you in your identification of male and female urethra specimens.
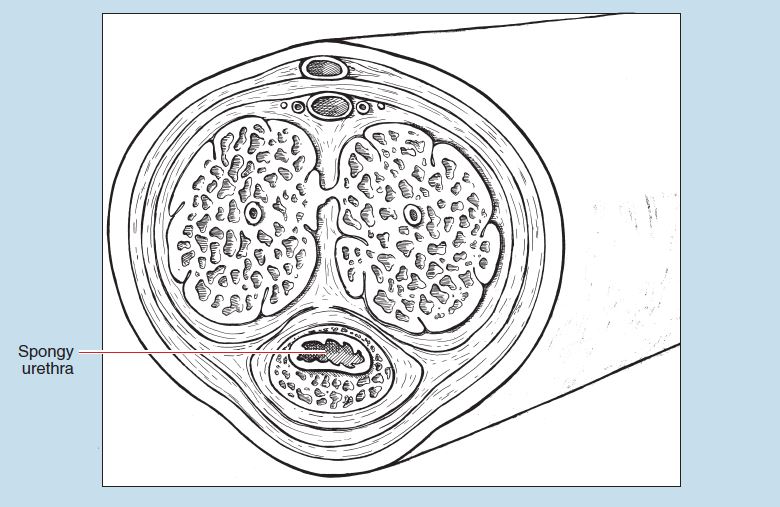
Figure 12-12: Line drawing of a cross section of a human penis.
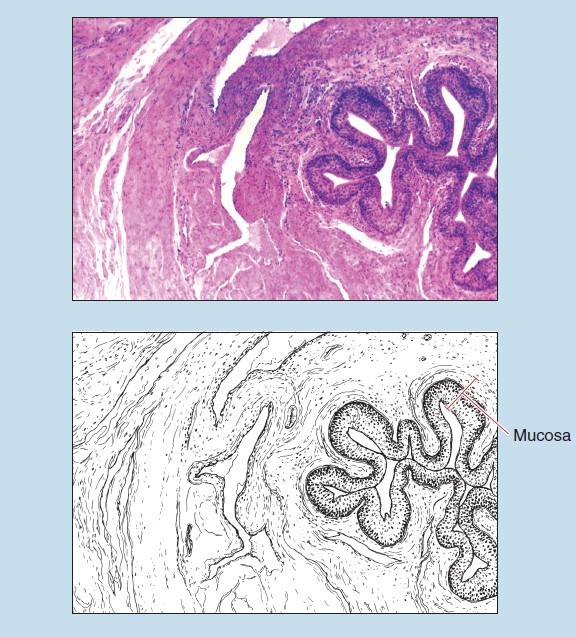
Figure 12-13 (25X): Human penis (cross section).
Female Urethra
The epithelium of the mucosa (Figures 12-14 and 12-15) will vary considerably from individual to individual. Near the bladder it is usually transitional; the remainder of the female urethra may be lined with stratified squamous, stratified columnar epithelium or pseudostratified columnar epithelium. The mucosa is thrown into longitudinal folds, and urethral glands are also visible in Figure 12-15. There are fewer urethral glands in the female urethra than in the male urethra; this is a major histological feature of this specimen. The stroma of the mucosa is rich in elastic fibers, owing to the longitudinal folding of the female urethra.
The muscularis (see Figure 12-14) is rather indefinite yet contains both longitudinal and circular layers of smooth muscle. An outer layer of skeletal muscle (not visible on this photomicrograph) may be present if your section was taken at the site of the voluntary sphincter. A definite adventitia is absent.
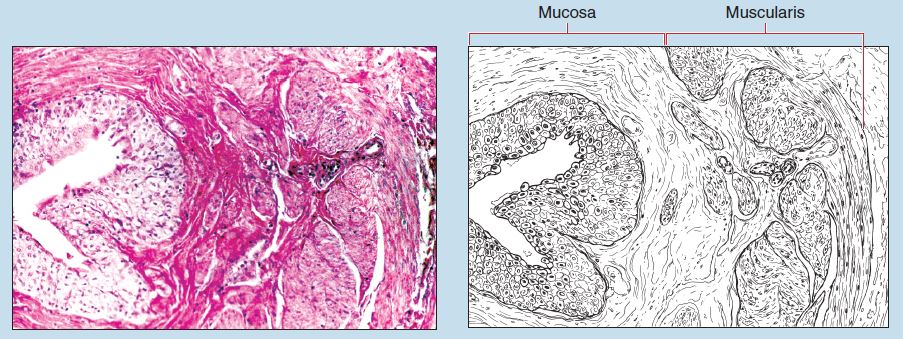
Figure 12-14 (25X): Female urethra.
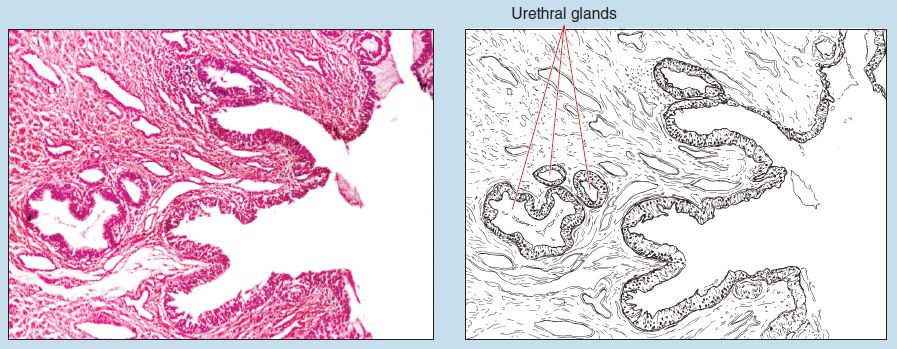
Figure 12-15 (50X): Female urethra.
Commonly Misidentified Tissues
Ureter and Relaxed Urinary Bladder
Ureter (Review Figure 12-8 in section on the Ureter)
-
- Mucosa is folded, usually resulting in a star-shaped lumen.
- Epithelium of the mucosa is uniform in thickness around the entire lumen.
- Muscularis is composed of either two layers of smooth muscle.
Urinary Bladder (Review Figure 12-9 in section on the Urinary Bladder [Relaxed])
-
- Mucosal folding is variable, depending on the state of organ distension at fixation.
- Epithelium of the mucosa is not uniform in thickness, owing to the variable distention of the organ.
- Although it may be difficult to distinguish, the muscularis is always composed of three layers.
Male and Female Urethra
Male Urethra (Prostatic or Spongy) (Review Figure 12-12 in section on the Penis/Spongy Urethra)
-
- Presence of prostate gland (with its numerous outpocketings surrounding prostatic urethra) or penile tissue surrounding urethra
- Urethral glands very prominent. Muscularis absent in two of three regions (being present only in the intermediate part of the urethra)
Female Urethra (Review Figures 12-14 and 12-15 in section on the Female Urethra)
-
- Prostate gland or penile erectile tissue absent
- Voluntary sphincter and corresponding outer layer of skeletal muscle usually present
- Urethral glands present but in a reduced number