Chapter Objectives
This chapter will enable you to identify:
-
- The components of the male testis
- The conducting tubule components
- The histological characteristics of the penis
- The histological characteristics of the accessory glands
Components of the Male Reproductive System and Their Functions
The male reproductive system is responsible for the production of male sex hormones and the formation and delivery of spermatozoa, in the form of semen, to the female reproductive system. The organs responsible for these functions are:
- Testis (spermatogenesis and production of male sex hormones)
- Duct system (spermatogenesis and the delivery of semen to the urethra)
- Accessory glands (production of fluid components of semen)
Testis
Seminiferous Tubules
The testis is covered externally on its anterior and lateral aspects by a mesothelial layer of simple squamous epithelium termed the tunica vaginalis. (Not visible in these photomicrographs.) Deep to the tunica vaginalis you will find the tough connective tissue capsule of the testis, the tunica albuginea (Figure 14-1).
The tunica albuginea is composed of coarse, interweaving, collagenous fibers. The inner portion of the capsule is termed the vascular layer of the testis (also termed the tunica vasculosa), which is composed of a looser, highly vascularized layer of connective tissue. Extensions of the vascular layer extend inward as connective tissue septa, which divide the testis into numerous lobules.
Deep to the vascular layer of the testis you will find the seminiferous tubules (Figure 14-1). These tubules are composed of a complex, stratified epithelium (see section on Stratified Epithelia in Chapter 2) resting on a thick, basal lamina and alternating layers of collagen fibers and flattened cells termed myoid cells. Peripheral to the myoid cells may also be a layer of fibroblasts and fibrocytes.
The epithelium of the seminiferous tubules is composed of nurse cells (also termed Sertoli cells) and spermatogenic cells (Figure 14-2). Nurse cells are the only cells that extend from the basal lamina to the tubular lumen; they form the major structural component of the seminiferous tubules. However, because of their staining characteristics it is difficult, if not impossible, to discern the apical portion of a nurse cell with the light microscope. Therefore nurse cells do not appear to extend from the basal lamina to the tubular lumen in a typical hematoxylin and eosin (H & E) preparation.
Nurse cells are slender and elongated, with irregular lateral outlines that are not visible with the light microscope. The cytoplasm of these cells often exhibits faint longitudinal striations. The distinctive nucleus is ovoid or somewhat triangular in shape, clearly outlined, and pale staining, with fine, sparse chromatin. One or more prominent nucleoli are often seen within the nucleus of a nurse cell, and the position of the nucleus may vary from cell to cell.
Spermatogenesis is the process by which sperm are produced by the testis. During this process, spermatogonial cells undergo a series of developmental changes and cellular mitotic and meiotic divisions. Only two stages of spermatogenesis will be addressed in this photomicrograph.
Within the seminiferous tubules of Figure 14-2 you should be able to identify late spermatids, which are usually located closest to the tubular lumen. Late spermatids have prominent tails that extend into the lumen and nuclei that are small and bullet shaped. In many H & E preparations only the nucleus is visible.
Near the basal lamina of the seminiferous tubules of Figure 14-2 you should be able to identify primary spermatocytes. These spherical cells demonstrate a significant clumping of the chromatin.
Not every seminiferous tubule will contain spermatogenic cells in the same state of differentiation. If you wish to identify the various stages of spermatogenesis, you may have to use numerous fields of vision to see them. Other stages that may be found in H & E preparations (but are not labeled on this photomicrograph) would include early spermatids, secondary spermatocytes, and Type A and Type B spermatogonia.
Located within the stroma and between the seminiferous tubules in Figure 14-3 are the interstitial endocrine cells (interstitial cells of Leydig). These cells, which usually occur in groups, are large and ovoid and possess a large, eccentrically located nucleus. The cytoplasm is granular and fairly dense near the nucleus, whereas the peripheral cytoplasm is vesicular and vacuolated. These cells will stain lightly acidophilic in H & E preparations because of the large number of cytoplasmic lipid droplets.
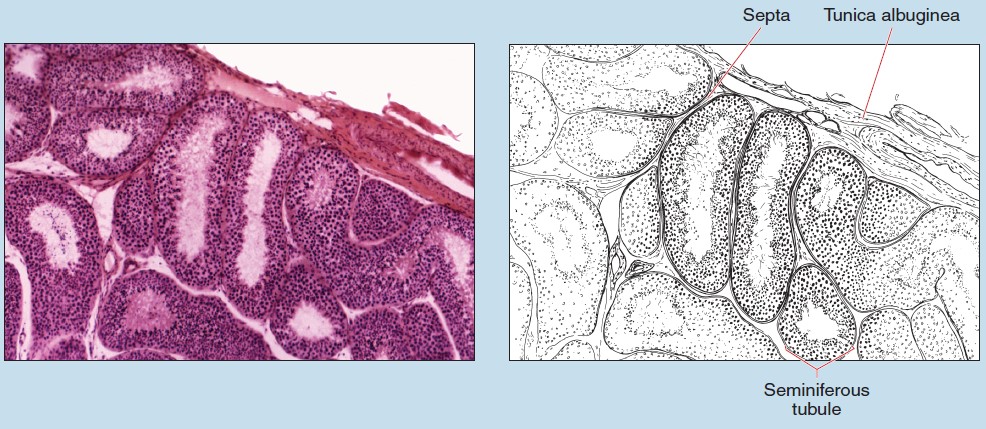 Figure 14-1 (25X): Testis.
Figure 14-1 (25X): Testis.
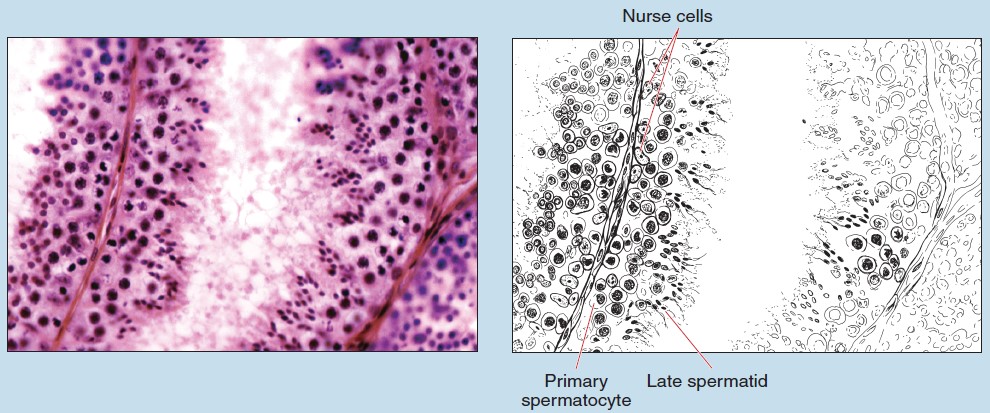
Figure 14-2 (100X): Testis.
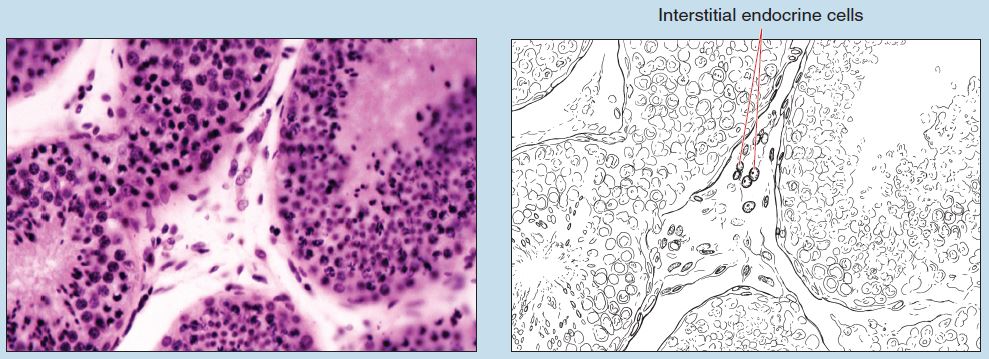
Figure 14-3 (100X): Interstitial cells (of Leydig).
Rete Testis
When looking for the rete testis on a slide it is important to orientate yourself first at low power. Follow the tunica albuginea around the periphery of the section until you locate the posterior surface of the testis, where the tunica albuginea thickens and invaginates. This invagination is termed the mediastinum of the testis; it is the location of the rete testis (Figure 14-4).
The rete testis is composed of wide, anastomosing channels lined with simple cuboidal epithelium (see section on Simple Cuboidal Epithelia in Chapter 2). The nuclei of the rete stain deeply, and the lateral borders of the cells are well defined under higher magnifications. No definite lamina propria is seen deep to the epithelium because of the connective tissue of the surrounding mediastinum.
Efferent Ductules and Epididymis
Sperm are transported from the rete testis to the epididymis via the efferent ductules. The efferent ductules (Figure 14-5) possess an epithelium composed of high columnar cells alternating with low columnar cells, thereby giving the lumen a scalloped appearance. This epithelium is pseudostratified columnar (see section on Pseudostratified Epithelia in Chapter 2), but it does not resemble that of the respiratory system (see section on the Trachea in Chapter 10). Some of the tall cells will possess cilia, and the epithelium rests on a distinct basal lamina. Deep to the lamina propria will be smooth muscle (see section on Smooth Muscle in Chapter 6) and a rich capillary network (see section on Capillaries in Chapter 8).
The epididymis is the site of sperm maturation and is subdivided into three regions: head, body, and tail. In contrast to the efferent ductules, the epididymis (Figure 14-6) presents smooth internal and external contours. The epithelium is pseudostratified columnar and is composed of tall, columnar principal cells and intermittent basal cells. The tall columnar cells are uniformin height and have numerous long, branching microvilli termed stereocilia.
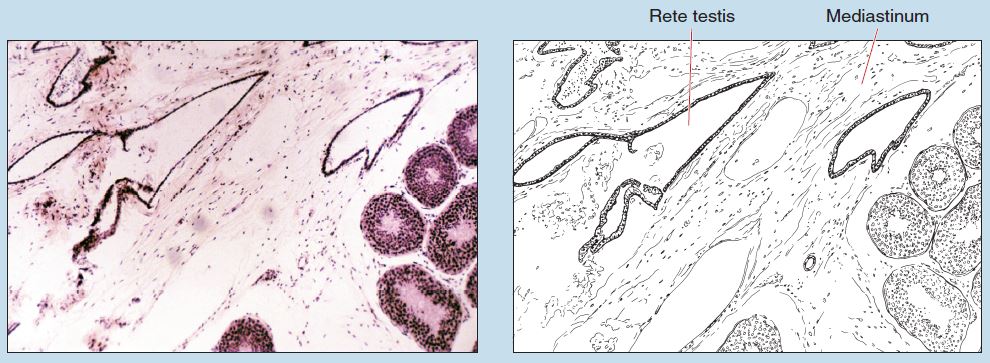
Figure 14-4 (25X): Rete testis.
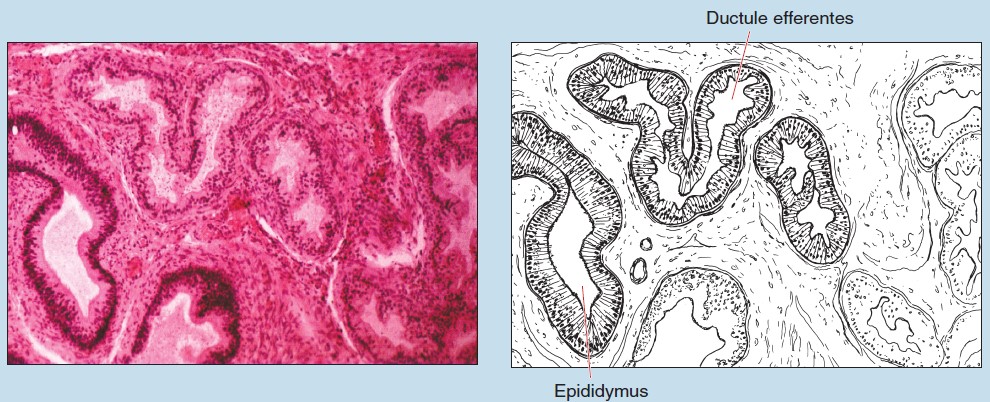 Figure 14-5 (25X): Efferent ductules.
Figure 14-5 (25X): Efferent ductules.
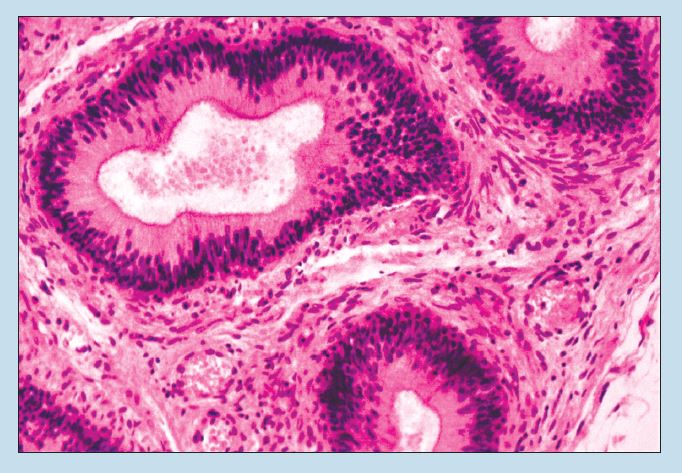
Figure 14-6 (50X): Epididymis.
Penis
Before studying the histology of the penis, review its gross anatomy by reexamining the structures seen in Figure 14-7. Note that the penis is composed of three cylindrical bodies:
- Two corpora cavernosa located dorsally
- One corpus spongiosum located inferiorly and seen to contain the spongy urethra
Some histological preparations of the penis are hemi-cross sections; therefore only part of the corpus spongiosum and spongy urethra and one of the two corpora cavernosa will be present. This photomicrograph (Figure 14-8) shows a hemisection of a human penis. Other slides used for penis specimens may have been obtained from animals possessing an os penis, as evidenced by the presence of bone (see section on Compact Bone—Cross Section—Ground Bone in Chapter 5) within the section. Keep these possibilities in mind as you examine your histological preparation.
Figure 14-8 is a photomicrograph of a segment of the wall from the corpora cavernosa within the human penis. The corpora cavernosa are surrounded by a dense capsule, termed the tunica albuginea. The tunica albuginea is composed of an inner circular and outer longitudinal layer of collagenous and elastic fibers. The interior of the body consists of a network of large spaces, or lacunae, lined by endothelium (termed cavernous veins) and separated by fibrous trabeculae rich in smooth muscle.
The corpus spongiosum is similar in structure to the corpora cavernosa. The corpus spongiosum, however, contains a higher density of elastic fibers and houses the spongy urethra (see section on Penis/Spongy Urethra in Chapter 12).
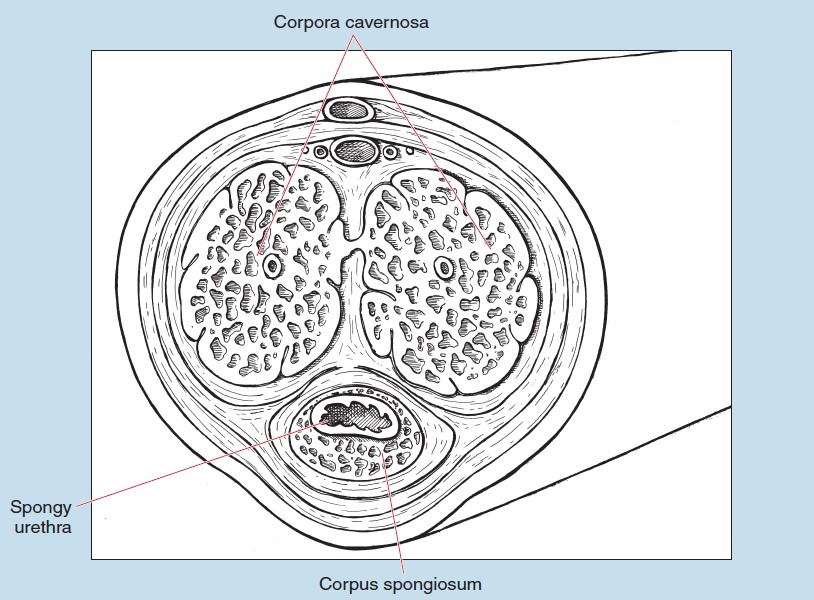
Figure 14-7: Cross section of the male penis.
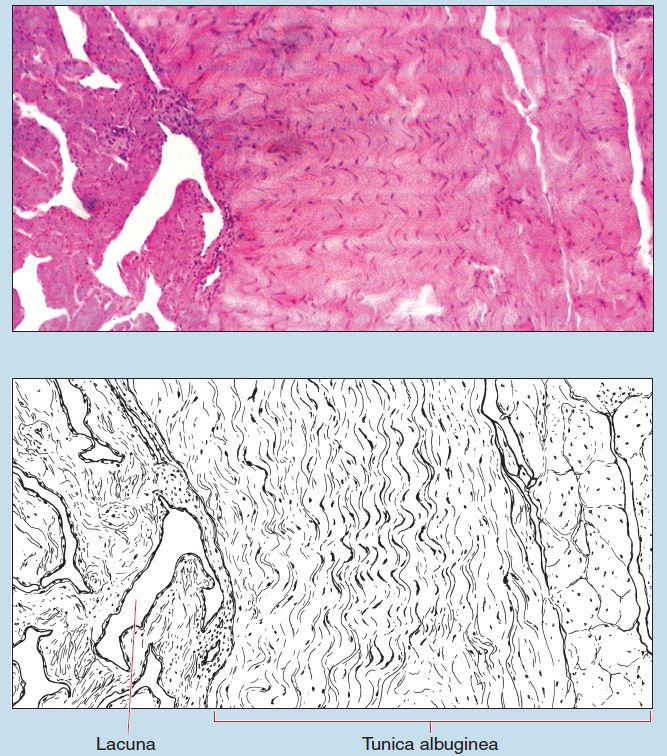
Figure 14-8 (25X): Cross section of the human penis.
Prostate
The prostate may be separated into two regions: a central portion (including the urethra) that contains short glands and a more peripheral region containing slightly longer glands. The structures mentioned below may or may not be present in your preparation, depending on the plane of section.
A vascular, fibroelastic capsule with numerous smooth muscle fibers surrounds the prostate (Figures 14-9 and 14-10). (The capsule may not be present on your preparation.) From this capsule, broad septa radiate inward and become continuous with the abundant connective tissue of the interior of the prostate. The stroma is fibromuscular, being a mix of smooth muscle and collagen fibers—a histological feature of the prostate.
The glands of the prostate (Figures 14-9 and 14-10) are lined with an epithelium that varies from low, simple columnar to pseudostratified columnar. The cells of the central region tend to be more irregular in height and more crowded when compared with the peripheral regions.
The ducts of the glands (which are not visible in these photomicrographs) possess a simple, columnar epithelium that will become transitional (see section on Transitional Epithelia in Chapter 2) near the junction of the urethra.
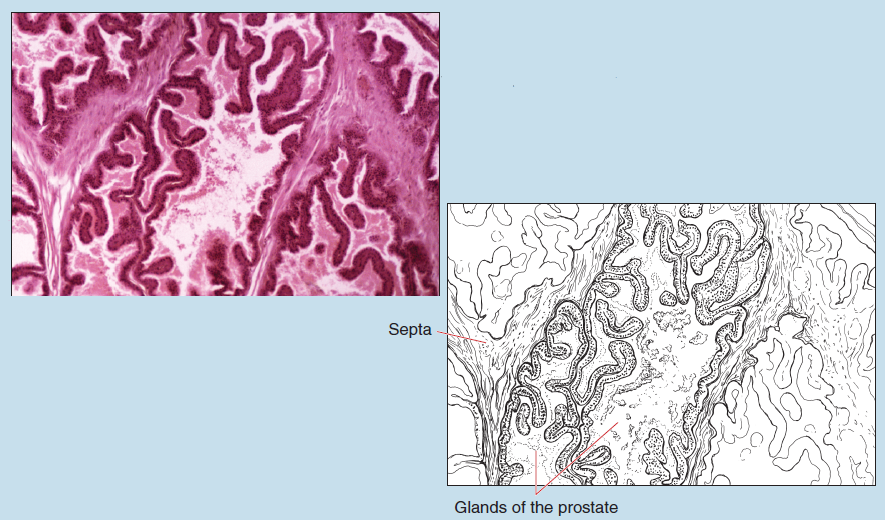
Figure 14-9 (25X): Prostate.
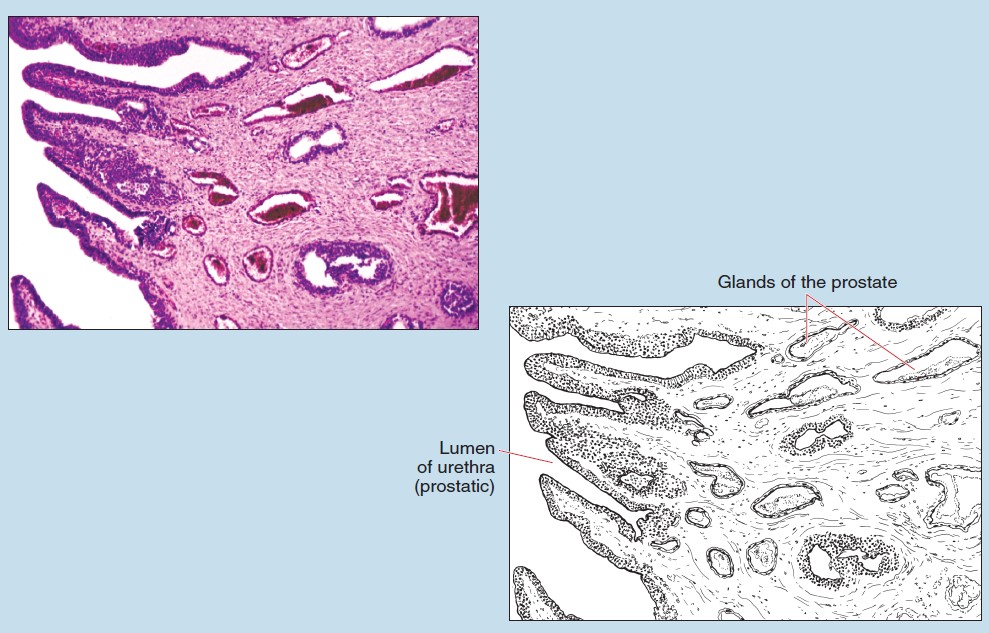
Figure 14-10 (25X): Prostate.
Ductus Deferens
The ductus deferens (vas deferens) possesses a thin mucosa, thick muscularis, and an outer adventitia (Figure 14-11).
The epithelium of the mucosa is a pseudostratified, columnar epithelium closely resembling that of the epididymis (see section on Efferent Ductules and the Epididymis in this chapter). However, unlike the epididymis, the mucosa of the ductus deferens is often thrown into longitudinal folds because of the contraction of underlying smooth muscle during fixation.
The muscularis of the ductus deferens consists of three layers of smooth muscle that are difficult to discern. These smooth muscle layers are arranged longitudinally (inner and outer layers) and circularly (middle layer).
Seminal Glands
The mucosa of the seminal glands (seminal vesicles) possesses numerous folds, which serve to increase the secretory surface area (Figure 14-12). The epithelium is a pseudostratified, columnar epithelium that may vary somewhat from location to location within the gland. The taller, nonciliated, columnar cells are secretory in nature, whereas the basal cells appear to be identical to those seen within other excretory ducts of the male reproductive system.
The lamina propria of the seminal gland forms the core of the primary and secondary mucosal folds, which extend into the lumen of the seminal glands.
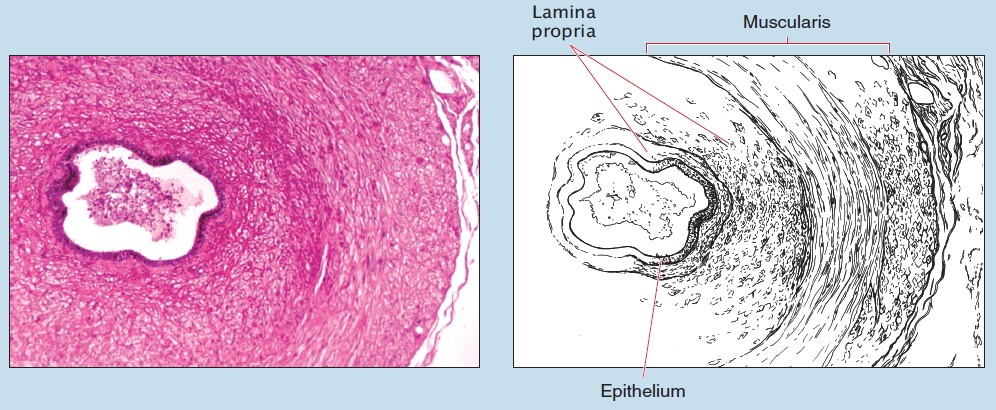
Figure 14-11 (25X): Ductus deferens.
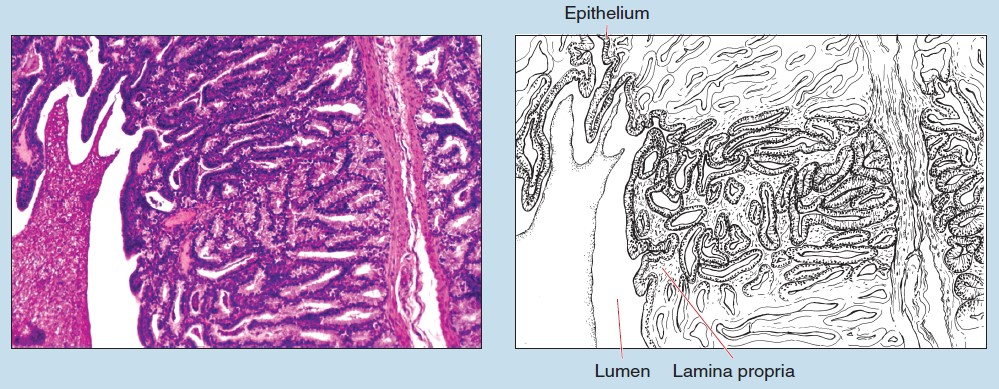
Figure 14-12 (25X): Seminal gland.
