Chapter Objectives
This chapter will enable you to:
-
- Understand the differences between membranous and endochondral ossification.
- Identify the various cell types and understand the various subprocesses that occur during membranous and endochondral ossification.
- Be able to identify the components of osteons (Haversian systems) found in mature bone.
- Be able to identify the components of the periosteum.
- Be able to distinguish between ground bone and decalcified bone preparations and understand the different information presented by each.
- Be able to differentiate between trabecular and compact bone.
Histological Similarities Between Bone and Cartilage
Bone and cartilage are different forms of connective tissue. As a result, as you progress through this chapter you will note a considerable number of histological similarities and differences between cartilage (particularly hyaline cartilage; see section on hyaline cartilage in Chapter 4) and bone. Some similarities are:
- Bone and cartilage both consist of cells embedded within a matrix of organic and inorganic materials.
- Cartilage and bone both have cells trapped within lacunae.
- Bone and cartilage, particularly hyaline and elastic cartilage, both possess a bilayered connective tissue covering.
Histological Differences Between Bone and Cartilage
You will see several histological differences between bone and cartilage:
- Bone has a greater ratio of cells to amorphous ground substance.
- The bilayered connective tissue covering bone is termed the periosteum.
- The matrix in bone is composed primarily of hydroxyapatite crystals, hence the need for blood vessels and cell-to-cell contact for nourishment and the elimination of wastes. Therefore mature bone is highly vascular.
Cells of Bone
Four different cell types will be found within mature bone: osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts.
Osteoprogenitor cells are located on the external and internal surfaces of bones. Surrounding the external surface of all bones is a layer of connective tissue termed the periosteum. In addition, lining the marrow cavity of long bones is another, considerably thinner layer of connective tissue, the endosteum. The periosteum is divided into two layers: an outer fibrous layer and an inner osteogenic layer. Osteoprogenitor cells are found in the innermost layer of the periosteum, where they are called periosteal cells. They are also found in the endosteum, where they are termed endosteal cells. Endosteal cells are also found in the connective tissue lining the central (Haversian) and penetrating (Volkmann’s) canals of mature bone. Osteoprogenitor cells typically differentiate into osteoblasts, although they may also differentiate into adipocytes or fibroblasts.
Histologically, osteoprogenitor cells have the following characteristics:
- Thin, attenuated, flattened shape
- Lightly staining, elongated or ovoid-shaped nuclei
- Variably staining cytoplasm, ranging from lightly acidophilic to lightly basophilic
The second cell type found in mature bone is the osteoblast. The primary function of osteoblasts is the synthesis and secretion of the collagenous fibers and ground substance of bone. In addition, osteoblasts participate in the ossification process by the secretion of matrix vesicles containing alkaline phosphatase.
Osteoblasts are found immediately deep to the periosteum and endosteum of mature bone. These cells have the following histological characteristics:
- Large cells that are rounded or polygonal in shape
- A single, eccentrically placed nucleus, typically found in the portion of the cell farthest from the developing bone
- Deeply basophilic-staining cytoplasm, nucleus, and nucleolus resulting from active protein synthesis
The third cell type found in mature bone is the osteocyte. An osteocyte is a mature cell trapped within a lacuna; it is responsible for maintaining the bony matrix. Osteocytes have the following histological characteristics:
- They are found within a lacuna within the bony matrix.
- The nucleus stains lightly basophilic, whereas the cytoplasm does not stain or will stain lightly acidophilic because of the reduced synthetic activity of the cell.
- They are slightly smaller in size than an osteoblast.
- They have thin, cytoplasmic processes that extend into the canaliculi of the bony matrix.
Osteoclasts are the fourth cell type of mature bone. These are large cells that are responsible for synthesis of the enzymes essential for the reabsorption of bone matrix during the remodeling of bone. Osteoclasts are found in two locations in mature bone: (1) associated with the inner portion of the endosteum, and (2) located within a depression termed a resorption bay (osteoclast crypt or Howship’s lacuna).
Osteoclasts exhibit the following histological characteristics:
- They are large, multinucleate cells.
- The cytoplasm will usually stain acidophilic but may vary in staining intensity, depending on the synthetic activity of the cell.
Adult bone may be divided into two subcategories: compact bone (also termed lamellar, dense, or cortical bone) and trabecular (spongy or cancellous) bone. Compact bone is typically limited to the cortex or outer layer of adult bones; it is quite strong and heavy.
Trabecular bone, in contrast, generally lies within the interior of the bone, including the expanded epiphyseal ends of long bones. Trabecular bone provides strength with minimal weight.
The histology of bone depends on the age and level of development of the specimen. Developing, immature, and mature bones exhibit considerable histological differences. To understand the histology of mature, adult bone, it is essential to develop an understanding of the development, or osteogenesis, of bone.
Bone Development
Membranous Bone Development
Bone develops by two mechanisms: membranous (also termed intramembranous development) and endochondral (intracartilaginous development). Membranous ossification occurs in the formation of bones such as the clavicle, mandible, and the flat bones of the face and skull.
Membranous bone development occurs within vascularized embryonic mesenchyme. Briefly, mesenchymal cells in close proximity to the newly arrived blood vessels differentiate into osteoblasts and establish centers of ossification. Osteoblasts will secrete the organic matrix first, followed by the inorganic matrix, thereby forming bony spicules or trabeculae. Osteoblasts become increasingly farther apart as additional matrix is synthesized. As they become separated, osteoblasts develop thin, cytoplasmic processes, which enable intercellular communication via gap junctions. As the osteoblasts become trapped within lacuna, they differentiate and are termed osteocytes.
Initially, the newly formed bone is trabecular in nature. Further development may result in the formation of compact bone with its corresponding osteons (Haversian systems).
Membranous Bone Development (Fetal Pig)
As discussed earlier, during membranous (intramembranous) bone development embryonic mesenchyme develops a rich vascular network, and the embryonic mesenchymal cells develop long, tapering processes that enable the cells to maintain contact with one another. The spaces between the cells soon become occupied with bundles of collagenous fibers. Mesenchymal cells then differentiate into osteoprogenitor cells, which ultimately differentiate into osteoblasts, cells that are responsible for membranous bone development.
Figure 5-1 demonstrates slender eosinophilic (acidophilic) bone spicules developing within embryonic mesenchyme. Closer examination of a series of these spicules in Figures 5-2 and 5-3 will illustrate the processes that occur during membrane bone development.
Figures 5-2 and 5-3 demonstrate small spicules of bone within the embryonic mesenchymal tissue. The periphery of the bony spicules is surrounded by basophilic osteoblasts. In the center of the spicules, note the osteocytes trapped within lacunae.
As you examine Figure 5-3, you will note a narrow region directly deep to the osteoblasts that stains differently when compared with the rest of the bony matrix. The developing bone in this narrow region is termed osteoid. Osteoid is the organic matrix of the developing bone that has been laid down by the osteoblasts but has not yet undergone ossification.
Osteoclasts are giant, multinucleate cells located within a resorption bay (also termed an osteoclast crypt or Howship’s lacuna), a depression on the periphery of the bony matrix. Osteoclasts are often incorrectly identified because several osteocytes may be stacked on top of one another, thereby resembling an osteoclast. Although not foolproof, following is a trick to locating an osteoclast on your laboratory slides and preventing a misidentification of this cell type:
- Scan the specimen on low or medium power and look for a cell that is significantly larger than any other in the field. (Note the cell indicated on Figure 5-2.)
- On locating such a cell, switch to high-dry objective and determine how many nuclei are in the cell in question. (Now note the corresponding cell on Figure 5-3.)
- If the cell appears to be multinucleate, you must determine whether or not it actually is an osteoclast. The easiest way to do this is to slowly alter the fi ne focus and see whether all (or most) of the nuclei come into and out of focus simultaneously. If they do, you have located an osteoclast; if not, you have probably located several osteoblasts stacked on top of each other, as indicated by the nuclei being within different planes of focus.
- Because some osteoclasts have nuclei in multiple planes of focus, this method of identifying multinucleate cells is not foolproof.
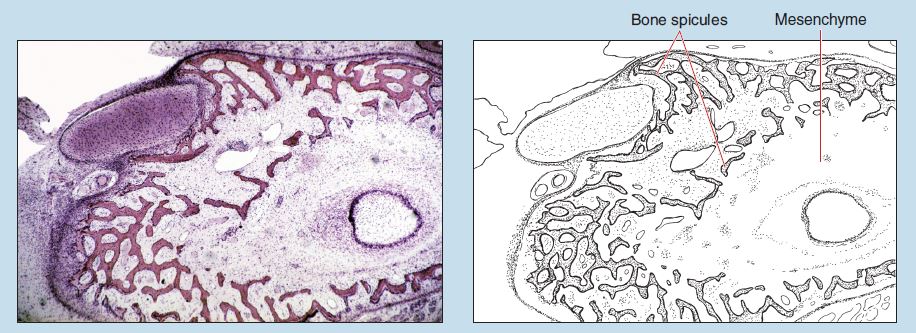
Figure 5-1 (25X): Membranous bone development (fetal pig).
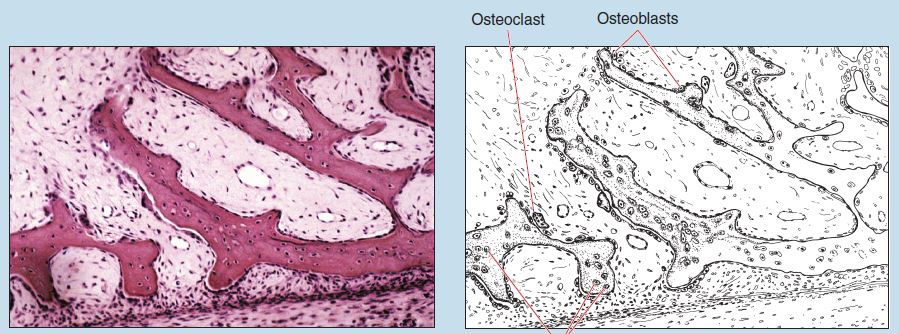
Figure 5-2 (50X): Membranous bone development (fetal pig).
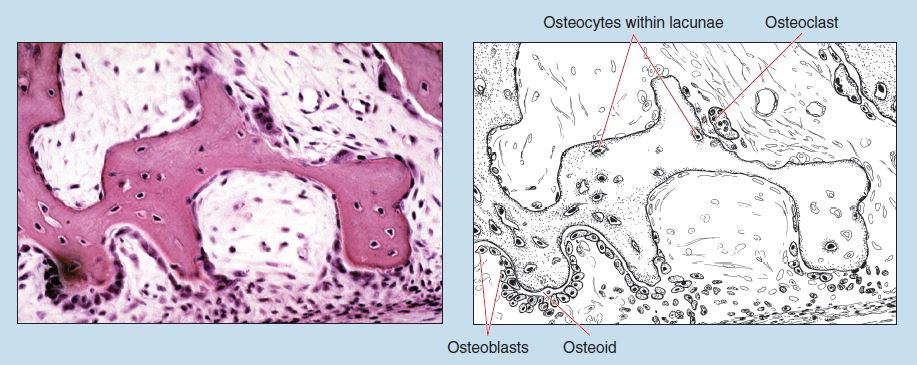
Figure 5-3 (100X): Membranous bone development (fetal pig).
Endochondral Bone Development
The bones of the limbs and other bones that bear weight, such as the vertebral column, develop by endochondral (intracartilaginous) ossification. This type of ossification starts with the formation of a cartilage model, which is then replaced with bone by the process outlined below.
The first step is the formation of a hyaline cartilage model of the long bone. All subsequent ossification will occur within this model. Endochondral ossification occurs initially within the diaphysis of the bone in an area termed the primary ossification center. The following steps will occur at the primary ossification center:
- The perichondrium surrounding the cartilage model differentiates into a periosteum as osteoprogenitor cells form within the periosteum. These cells will differentiate into osteoblasts, and osteoblasts will secrete a bony collar around the diaphysis of the hyaline cartilage model.
- Subsequent to the formation of the bony collar, histological changes will be observed within the interior of the cartilage model. The chondrocytes will hypertrophy, and the matrix surrounding them will calcify. Subsequently, the chondrocytes within the calcified matrix die.
- The newly developed periosteum increases in vascularity, and these newly formed capillaries invade the cartilage model of the bone.
- Osteoprogenitor cells from the periosteum will migrate into the interior of the calcified cartilage model, following the capillaries from the periosteum. These cells will then differentiate into osteoblasts.
- Osteoblasts will secrete bone within the center of the cartilage model. Initially, this newly formed bone is secreted on and around the calcified cartilage matrix within the center of the cartilage model. Therefore the first bone formed by this process will surround a core of cartilage. Because of the different staining properties of cartilage and bone, these trabeculae will have a spotty or mottled appearance. This spotty appearance is seen only within the center of the cartilage model of the newly forming bone; the bone laid down immediately deep to the periosteum is compact bone.
- Subsequently, the calcified cartilage within the center of the cartilage model will be removed, and newly synthesized bone will take its place.
As ossification progresses within the diaphysis of the bone, the process will begin to repeat at the expanded epiphyseal ends of the bone. These newly formed ossification centers at the epiphyseal ends are termed secondary ossification centers. As ossification progresses within the secondary ossifi cation centers, the hyaline cartilage that remains between the diaphysis and the epiphysis is termed the epiphyseal plate. This epiphyseal plate will ultimately separate the epiphyseal and diaphyseal portions of the developing bones and is responsible for increasing the length of the developing bone.
Endochondral Ossification at the Epiphyseal Region (Fetal Metatarsal Bone)
Figure 5-4 shows a fetal metatarsal bone at the junction between the epiphyseal and diaphyseal regions. Note that the epiphyseal region on the right is composed of hyaline cartilage. A secondary ossification center has not yet developed in the epiphyseal end, but note the invasion of the hyaline cartilage by several vascular elements. The primary ossification center is located within the diaphysis of the developing bone.
Figure 5-5 is a higher magnification of the same distal (epiphyseal) end of a fetal metatarsal bone. Bone formation is occurring at the junction between the epiphyseal and diaphyseal regions of the bony model, which is seen at the left in this photomicrograph.
The hyaline cartilage within the epiphyseal end of a developing long bone will demonstrate a characteristic zonation as the epiphyseal plate begins to form. Beginning at the distal end of the bone and progressing toward the junction with the diaphysis you will see the following zones:
- Resting Zone (zone of resting or reserve cartilage). This zone is composed of typical hyaline cartilage.
- Proliferation Zone. Cells within this zone are undergoing cellular division and are aligning themselves into distinct rows parallel to the longitudinal axis of the developing bone.
- Hypertrophic Zone (zone of maturation). This zone contains chondrocytes that have enlarged considerably. In addition, chondrocytes within this zone accumulate glycogen, which will be dissolved during the fixation process.
- Calcification Zone. The cells within this narrow zone have begun to degenerate, and the matrix surrounding them is beginning to calcify.
Figure 5-6 shows bony spicules within the diaphysis of the developing bone. Note the osteoblasts located on the periphery of the developing bone. Osteocytes are seen trapped within lacunae of the spicule.
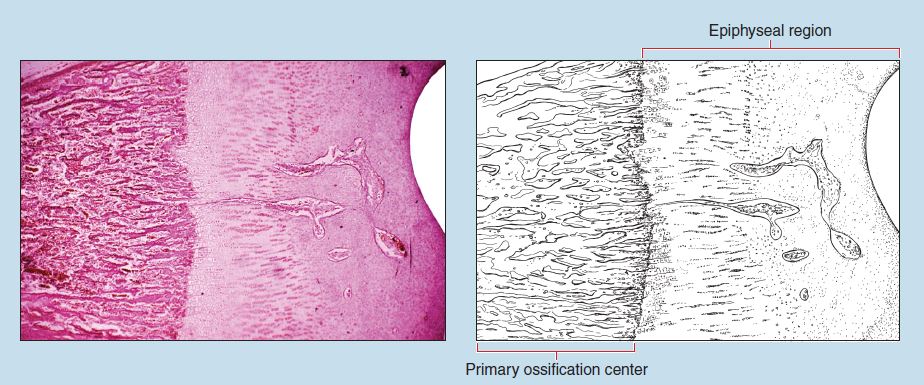
Figure 5-4 (40X): Endochondral ossification at the epiphyseal plate (fetal metatarsal bone).
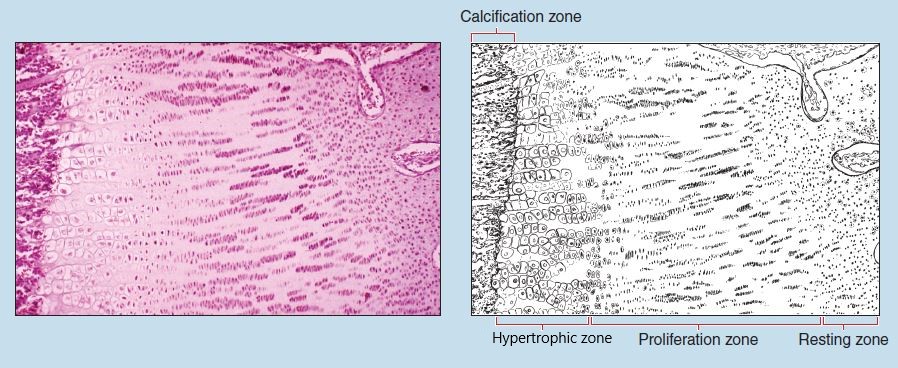
Figure 5-5 (25X): Endochondral ossification at the epiphyseal plate (fetal metatarsal bone).
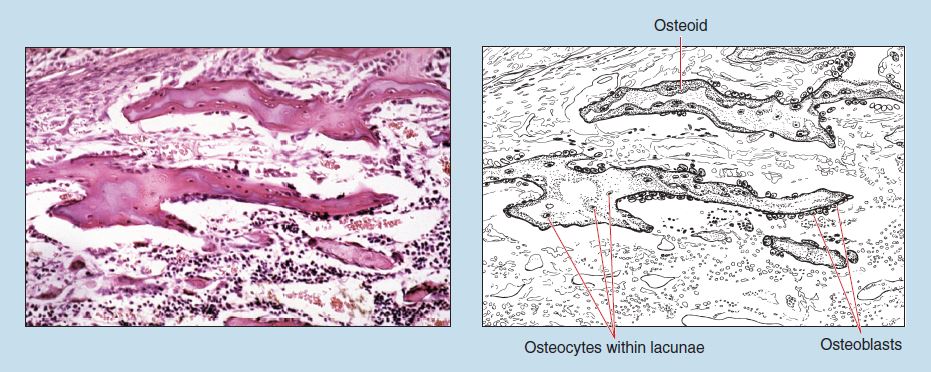
Figure 5-6 (50X): Bony spicules within the diaphysis of the developing bone (intracartilaginous development) (fetal metatarsal bone).
Mature Bone
Mature bone may be in the form of compact or trabecular (cancellous) bone. Trabecular bone is composed of slender, interlacing bony trabeculae. Marrow is located within the spaces between the trabeculae. Both types of mature bone are organized into layers, called lamellae. Trabecular bone presents parallel lamellae, whereas compact bone presents circular lamellae.
Compact Bone – Cross Section – Ground Bone
Figure 5-7 is a cross section of ground, compact bone obtained from the diaphysis of a long bone. Because of this style of tissue preparation, the inorganic matrix is maintained, and the organic components (blood vessels, cells, and unmineralized matrix) are absent.
Compact bone is organized into a lamellar arrangement termed osteons (Haversian systems). Osteons consist of concentric, circumferentially arranged lamellae of osteocytes within lacunae and a central (Haversian) canal. Also visible in this figure is a perforating (Volkmann’s) canal connecting two central canals.
The remodeling of bone continues throughout the life of an individual. Changes in an individual’s level of physical activity will produce variations in stress at tendon and ligament attachment sites that contribute to bone remodeling. As bone is remodeled, new bone is deposited, and other areas of older bone are reabsorbed. Interstitial lamellae are the result of this remodeling process. These are fragments of osteons of older bone that persist following the reabsorption of older bone and the deposition of newer bone during the remodeling process.
Figure 5-8 is an oil-immersion photomicrograph of a cross section of ground, compact bone. This figure demonstrates lacunae and their interconnecting canaliculi.
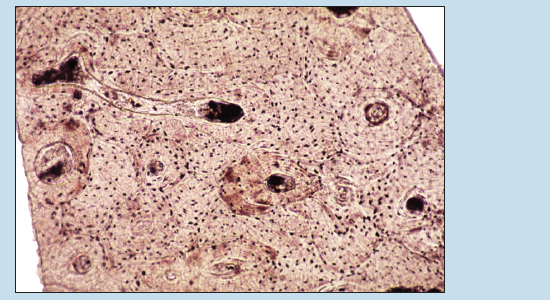
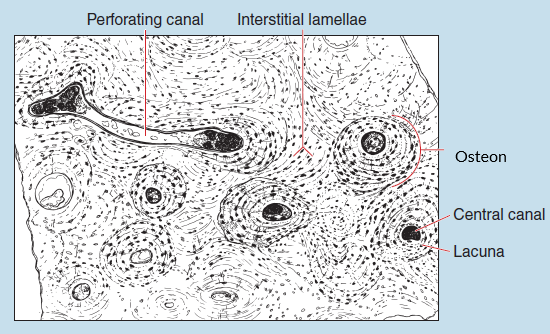
Figure 5-7 (25X): Compact bone (cross section) – ground bone.
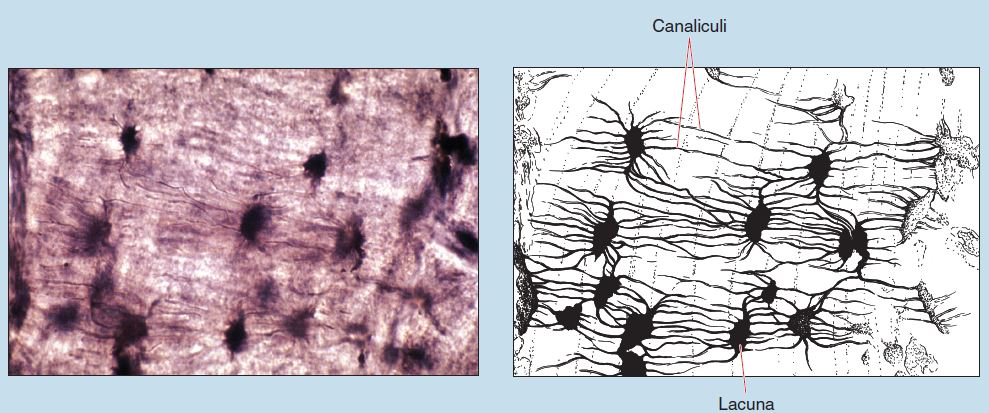
Figure 5-8 (250X): Compact bone (cross section) – ground bone.
Periosteum
Figure 5-9 is a cross section of a decalcified, compact bone. At the periphery of this section you will note the periosteum. Because of the thickness of the specimen, note how the photomicrograph makes the transition from being in focus to out of focus as you scan the specimen from left to right. This is yet another example of specimen artifact, attributable either to the plane of section or the mounting of the specimen on the slide.
The periosteum is composed of two layers: an outer fibrous layer and an inner osteogenic layer. The fibrous layer is composed of dense connective tissue. The nuclei of fibrocytes found within this layer are visible.
The inner layer of the periosteum is termed the osteogenic layer. Within this layer are osteoprogenitor cells and osteoblasts. Osteoprogenitor cells (not visible in this photomicrograph) are flattened, resting cells with the ability to differentiate into osteoblasts that are visible in the inner portion of the periosteum.
What accounts for the histological differences seen among Figures 5-9 (decalcified bone), 5-7, and 5-8 (ground bone)?
Trabecular Bone
Figure 5-10 is taken from the epiphysis of a long bone. The trabeculae (bony spicules) throughout this figure are immature and still undergoing osteogenesis, as evidenced by the variations in the staining characteristics. Compare the histological appearances of trabecular (cancellous) and compact bone (see Figures 5-7 and 5-8). What would be a major difference between these two forms of mature bone?
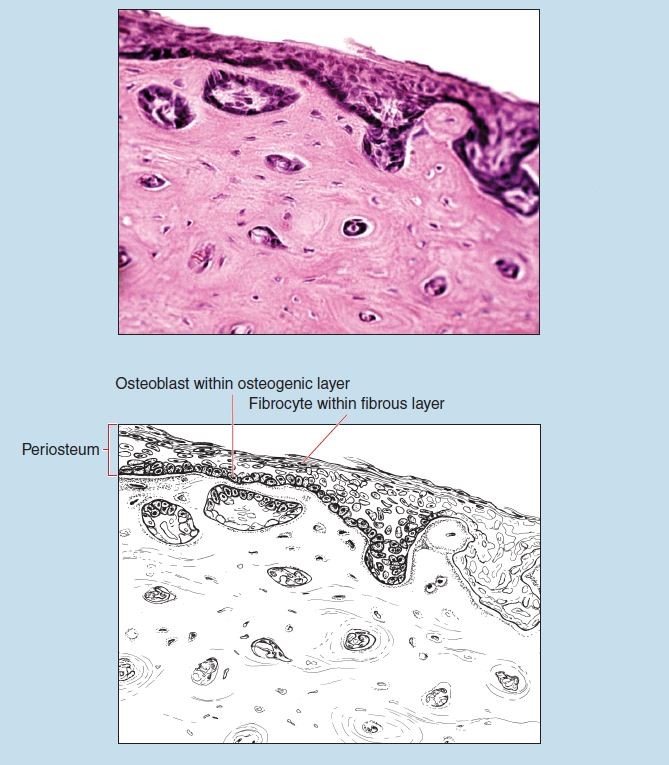
Figure 5-9 (100X): Cross section of decalcified, compact bone demonstrating periosteum.
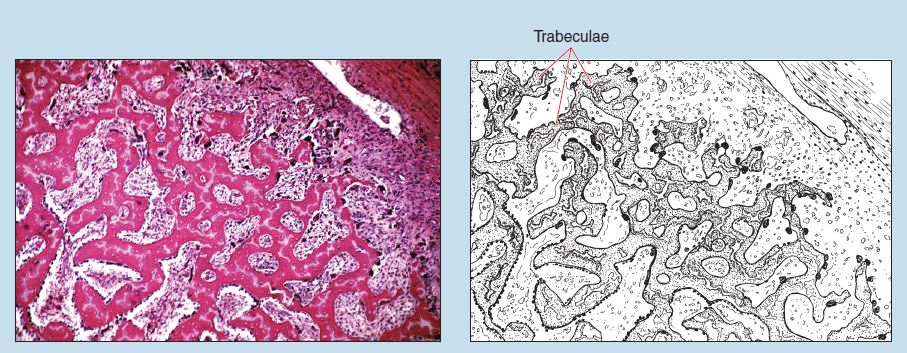
Figure 5-10 (50X): Trabecular bone.
