USING MVA AND EVA EQUIPMENT
Images adapted from MVA, a presentation by PRH and ARHP, 2000; 2012.
 |
Manual Vacuum Aspirator Plus
- Cap
- Cap release
- Valve buttons
- Clasp
- Plunger O-ring
- Collar stop Retaining Clip
- Collar stop
- Cylinder base
- Plunger arms
- Plunger handle
|
|

|
Prepare the aspirator
- Begin with valve buttons open and plunger pushed fully into the barrel.
- Close valve by pushing the buttons down and forward until locked in place.
|
|

|
Create the vacuum
- Pull the plunger back until its arms snap outward over the rim at the end of the barrel.
- Make sure plunger arms are positioned over wide edges of the barrel rim.
|
|
|
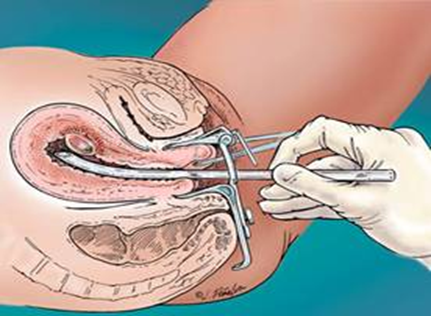
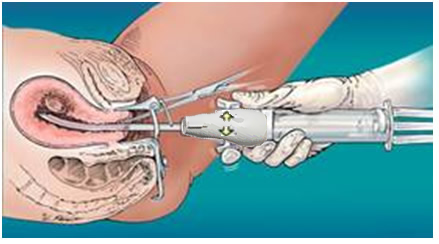
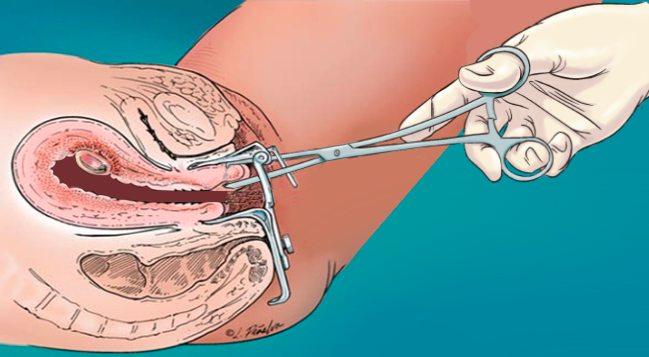
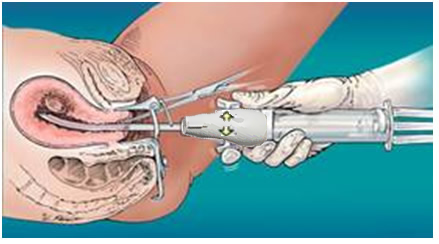
Attach the tenaculum
- Gently attach the tenaculum to the cervix (either anterior lip, as shown here) or posterior lip (for a retroverted uterus), closing slowly 1-2 clicks.
- Exert gradual traction to straighten cervical canal.
|
|
|
Gently dilate the cervix after paracervical block
- Use dilators of increasing size to accommodate cannula size chosen based on gestational weeks.
- Dilator:
- Denniston – dilate to cannula size (e.g. size 7 for 7 mm cannula)
- Pratt – dilate to cannula size x 3 (e.g. 21 French for 7mm cannula)
|
|

|
Choose a cannula
- Flexible: longer with two openings at tip
- Rigid: larger single opening at tip
- No significant difference safety or efficacy (Kulier 2001)
- Larger cannula: faster aspiration, more intact tissue
- Smaller cannula: less dilation and less resistance
Last NAF Provider’s survey (O’Connell 2009):
-
- 54% used size (in mm) = weeks gestation
- 37% used 1-2 mm < weeks gestation
- 9% used 1-3 mm > weeks gestation
|
 |
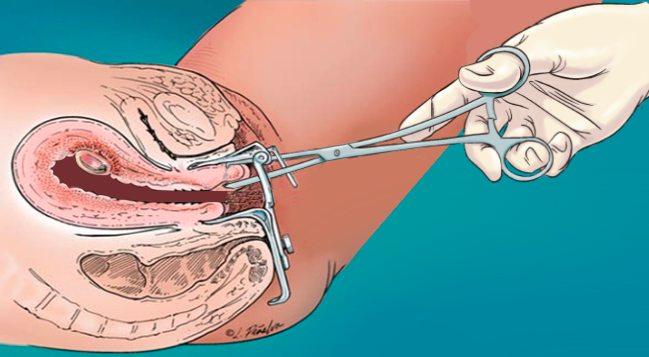
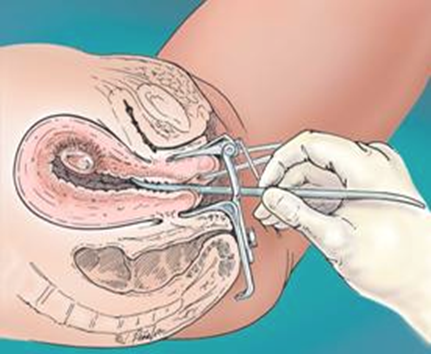
Insert the cannula
- Apply traction to tenaculum to straighten uterus. While holding cannula with fingertips, gently insert through cervix with rotating motion.
- Attach aspirator to cannula.
- Do not grasp aspirator by plunger arms.
|
|
|
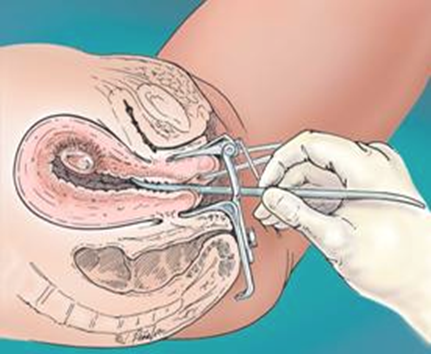
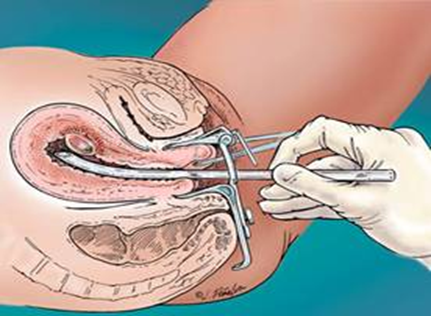
Release the valve buttons
- When the pinch valve is released, the vacuum is transferred through the cannula into the uterus.
- Blood, tissue, and bubbles will flow through the cannula into the aspirator.
|
|
|
Evacuate the uterus
- Rotate the cannula and move it gently from fundus to the internal os, applying a back and forth motion as clinically indicated until:
- Grittiness is felt through cannula
- Uterus contracts and grips cannula
- There is increased cramping, and / or
- No more blood passes through cannula.
|
|

|
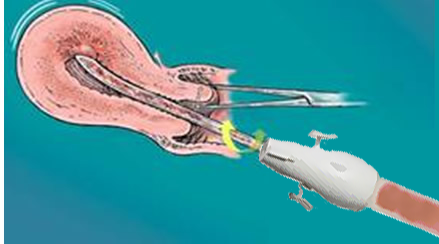
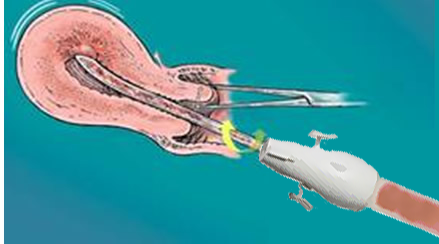
Choice of Vacuum for Aspiration
- Availability / preference determine use
- Some use > 1 MVA to facilitate emptying, or switch to EVA > 9 weeks
- Minimal differences in pain, anxiety, bleeding, or acceptability (Dean 2003)
- EVA sound may be audible to patients; silent, in-wall suction is available.
EVA use:
- Turn on and check suction gauge, turn dial to adjust
- Attach cannula
- Open thumb valve, keep open while placing cannula in uterus
- Once at fundus, close thumb valve to initiate suction
- Release suction by opening thumb valve when passing out of the cervical canal.
|
|

|
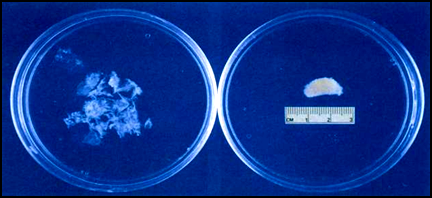
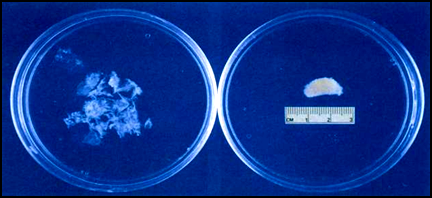
Inspect the tissue
- Rinse and strain the tissue
- Place tissue in a clear container
- Backlight is recommended to inspect tissue if gross visual inspection is non-diagnostic.
|
|
|
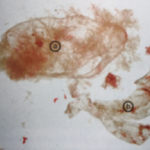
Gestational sac at 6 weeks
- Shredded (on left) vs. intact
- To minimize shredding, consider using MVA and/or a slightly larger cannula.
|
|
|
|
|
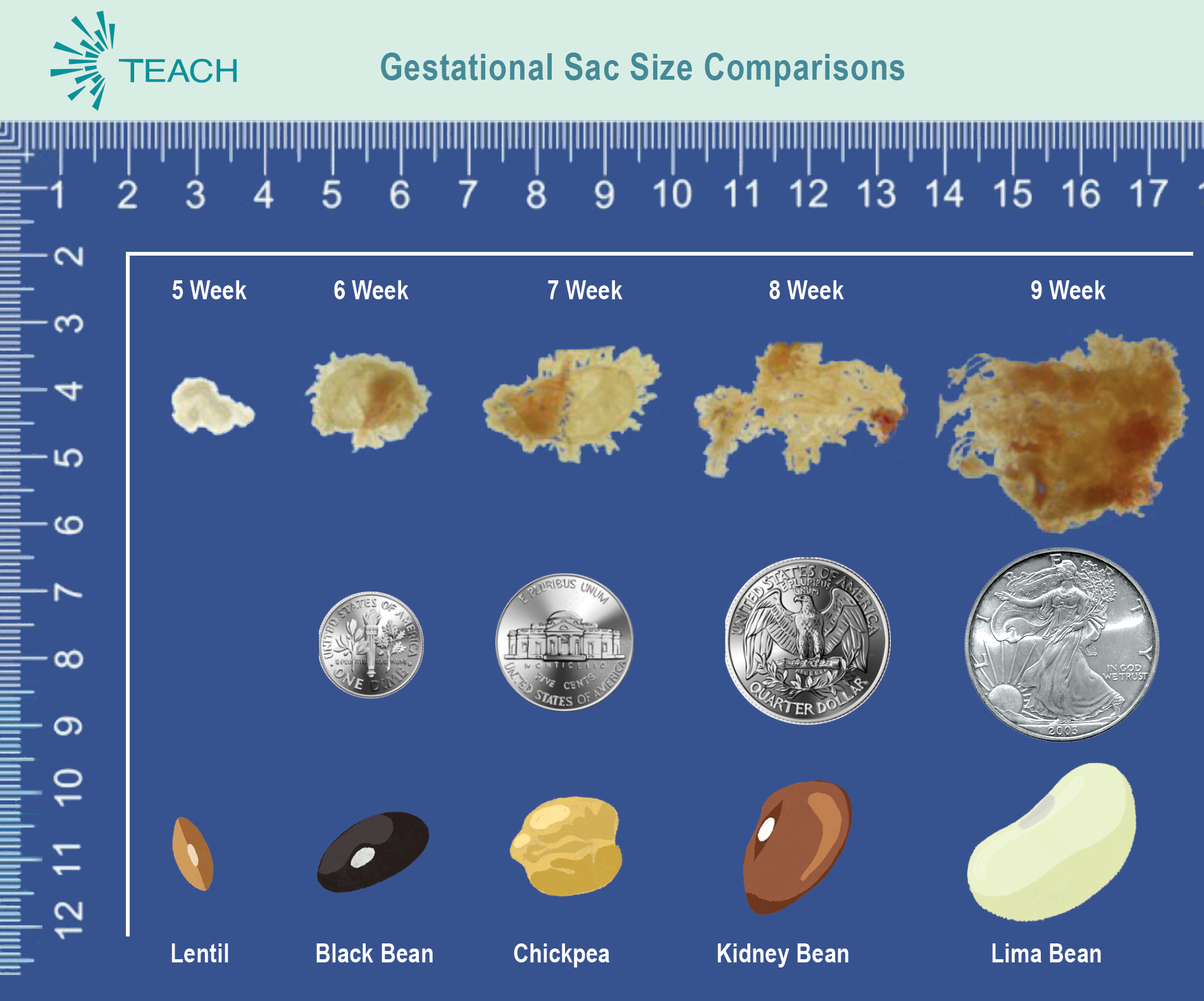
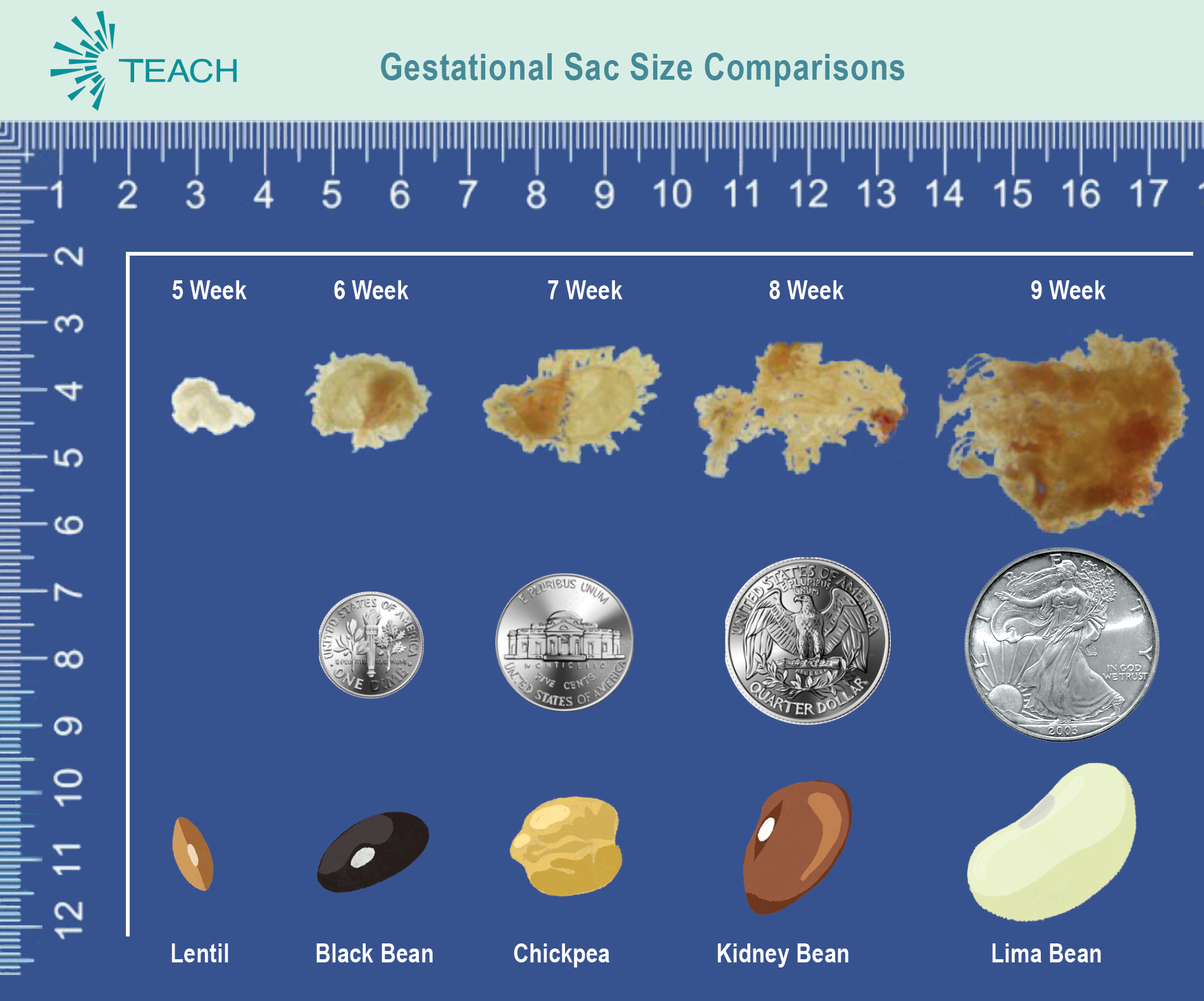
Membranes and Villi (POC)
- Frond-like villi
- Clumps held by membrane
- Transparent like plastic wrap
- Luminescent; light refractory
- Turns white if vinegar added
- More stretchy
- Floats more in liquid media
|
Decidua (not POC)
- No fronds
- No villi or thin membrane
- Opaque like wax paper
- Less light refractory
- Minimal color change
- More breakable
- Sinks more in liquid media
- Quantity variable
|
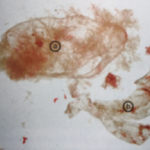 |
Decidua capsularis
Caution not to confuse
a) gestational sac (8 wk) with
b) decidua capsularis, a portion of the decidua which grows proportionally to gestational sac but is thicker and tougher (Paul 2009). |
Fetal part development
Parts may be seen earlier.
≥ 10W look for 4 extremities, spine, calvarium and gestational sac.
≥12W must find all fetal parts + placenta.
|