20
Case
Age: 62-year-old man
Reason for referral to ophthalmology: Double vision
Past medical history: Hypertension
Past ocular history: None
Medications: Valsartan, nifedipine
Habits: Non-smoker and non-drinker
HPI: Two days ago, his wife noticed the his “eyes weren’t moving right” and he had double vision with objects separated horizontally. The double vision was worse when looking to the right and resolved if he covered either eye. He presented to the emergency room and a CT scan of the head without contrast was normal. An ophthalmology consultation was requested.
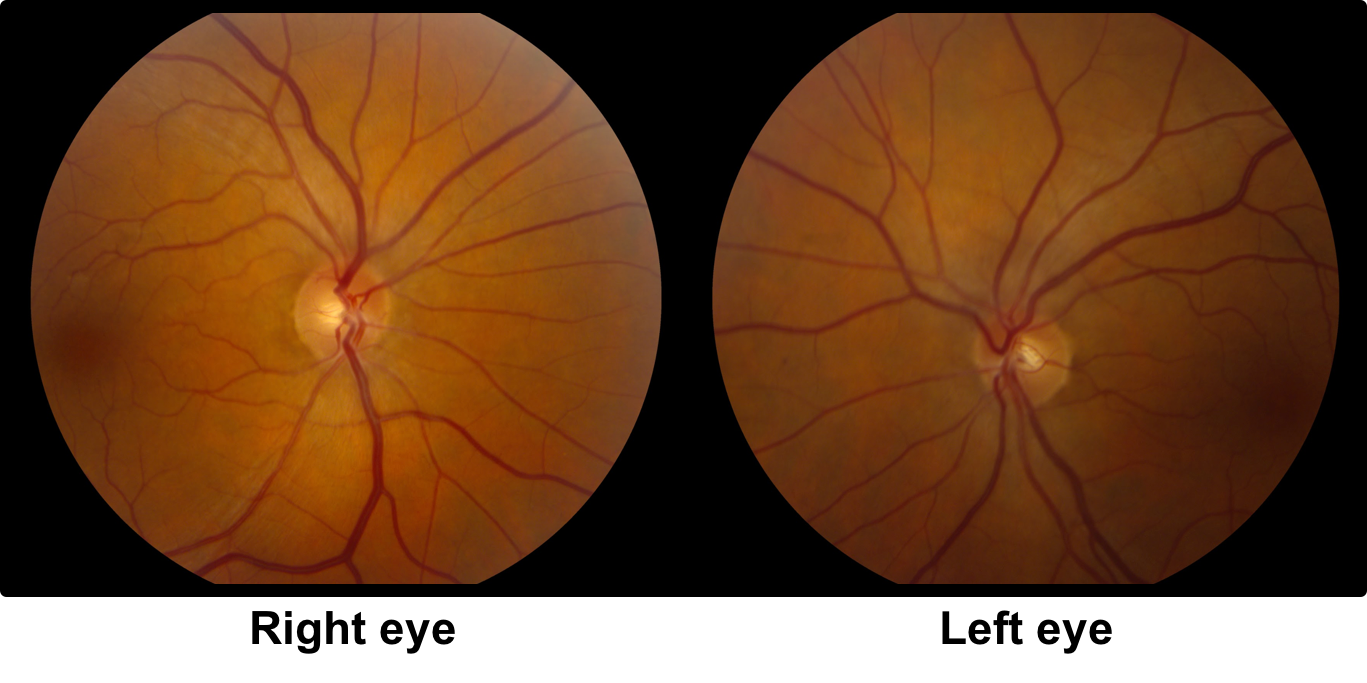
Ophthalmological examination:
Blood pressure: 146/89, heart rate 75
Visual acuity is 20/20 OD, 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision is 14/14 OD and 14/14 OS correct Ishihara plates
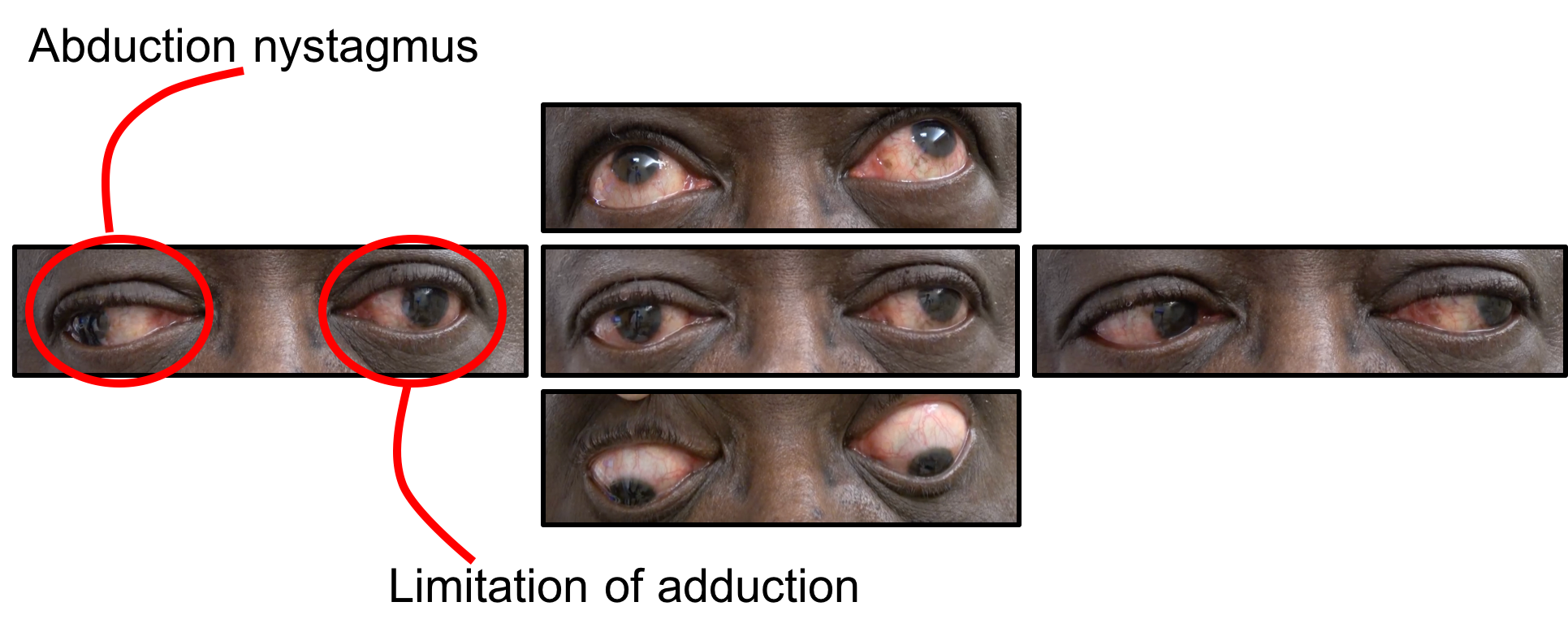
Ocular motility and alignment are shown below
Slit lamp examination is normal
Neurological examination is otherwise normal

1. What is included in the differential diagnosis for this patient?
- Ocular myasthenia gravis
- Orbital mass
- Internuclear ophthalmoplegia (INO)
- All of the above
1. What is included in the differential diagnosis for this patient? 4. All of the above
The patient has a limitation of adduction in the left eye, which may be caused by a left orbital process restricting adduction, ocular myasthenia gravis, or an internuclear ophthalmoplegia (INO). Examining for associated signs of each of these conditions is therefore important.
2. Which of the following is true regarding an isolated left adduction deficit?
- It may be due to a lesion of the left 3rd nerve nucleus
- It may be due to a lesion of the right 3rd nerve nucleus
- It may be due to a lesion in the right medial longitudinal fasciculus (MLF)
- It may be due to a lesion in the left MLF
2. Which of the following is true regarding an isolated left adduction deficit? 4. It may be due to a lesion in the left MLF
The MLF exists as a pair of long white matter tracts in the brainstem that coordinate horizontal gaze by connecting a number of brainstem nuclei including the 6th nerve nucleus with the contralateral 3rd nerve nucleus. The conjugate horizontal gaze centre is the paramedian pontine reticular formation (PPRF) in the pons. Burst cells in the PPRF innervate the 6th nerve nucleus, which contains motor neurons that innervate the lateral rectus and interneurons that cross the midline and ascend in the MLF to innervate the medial rectus subnuclei of the 3rd nerve nucleus. Therefore, if there is a left MLF lesion there will be a limitation of adduction on the left side. The adduction deficit may vary from complete loss of adduction beyond the midline to a mild decrease in velocity or acceleration of adduction without any limitation of the range of motion.
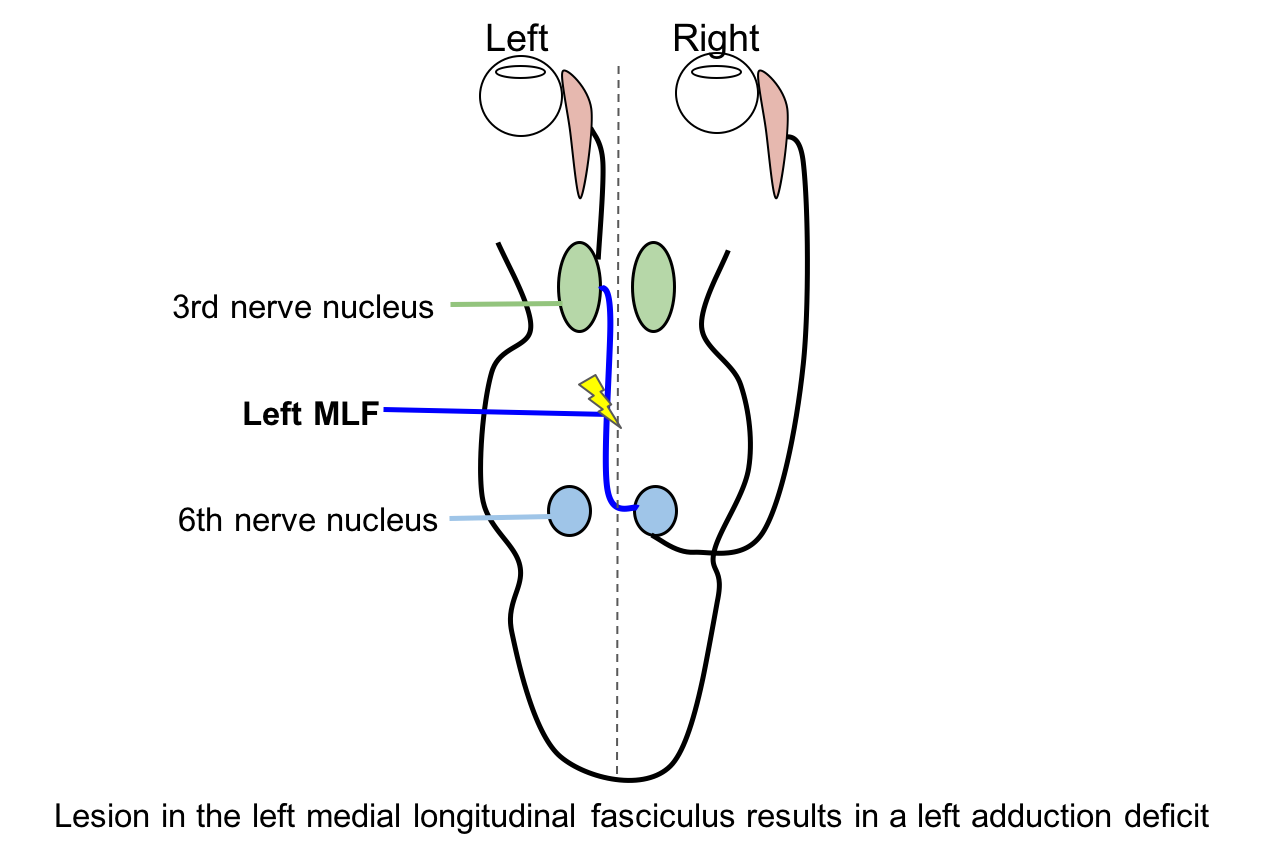
The medial rectus subnuclei lie in three different locations within the 3rd nerve nucleus. Therefore, an isolated medial rectus palsy without other muscle involvement is not consistent with a nuclear 3rd nerve palsy due to the multiple locations of the medial rectus subnuclei.
Clinical Pearl
The side of the INO is the side with the adduction deficit.
3. Assuming there are no orbital signs on examination, what is the next most appropriate investigation for this patient?
- CT angiogram of the head
- MRI of the brain
- CT scan of the head with contrast
- Observation
3. Assuming there are no orbital signs on examination, what is the next most appropriate investigation for this patient? 2. MRI of the brain
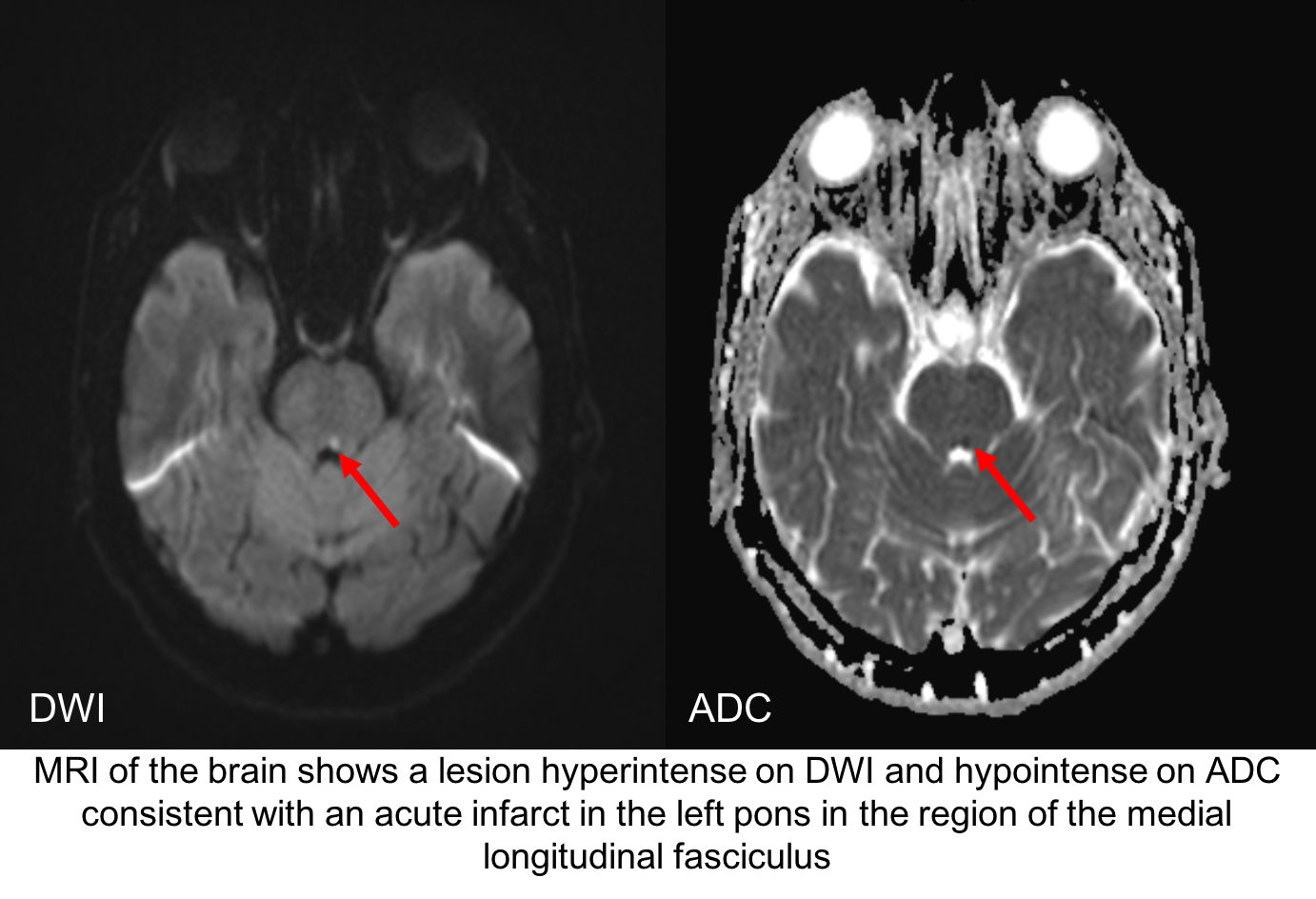
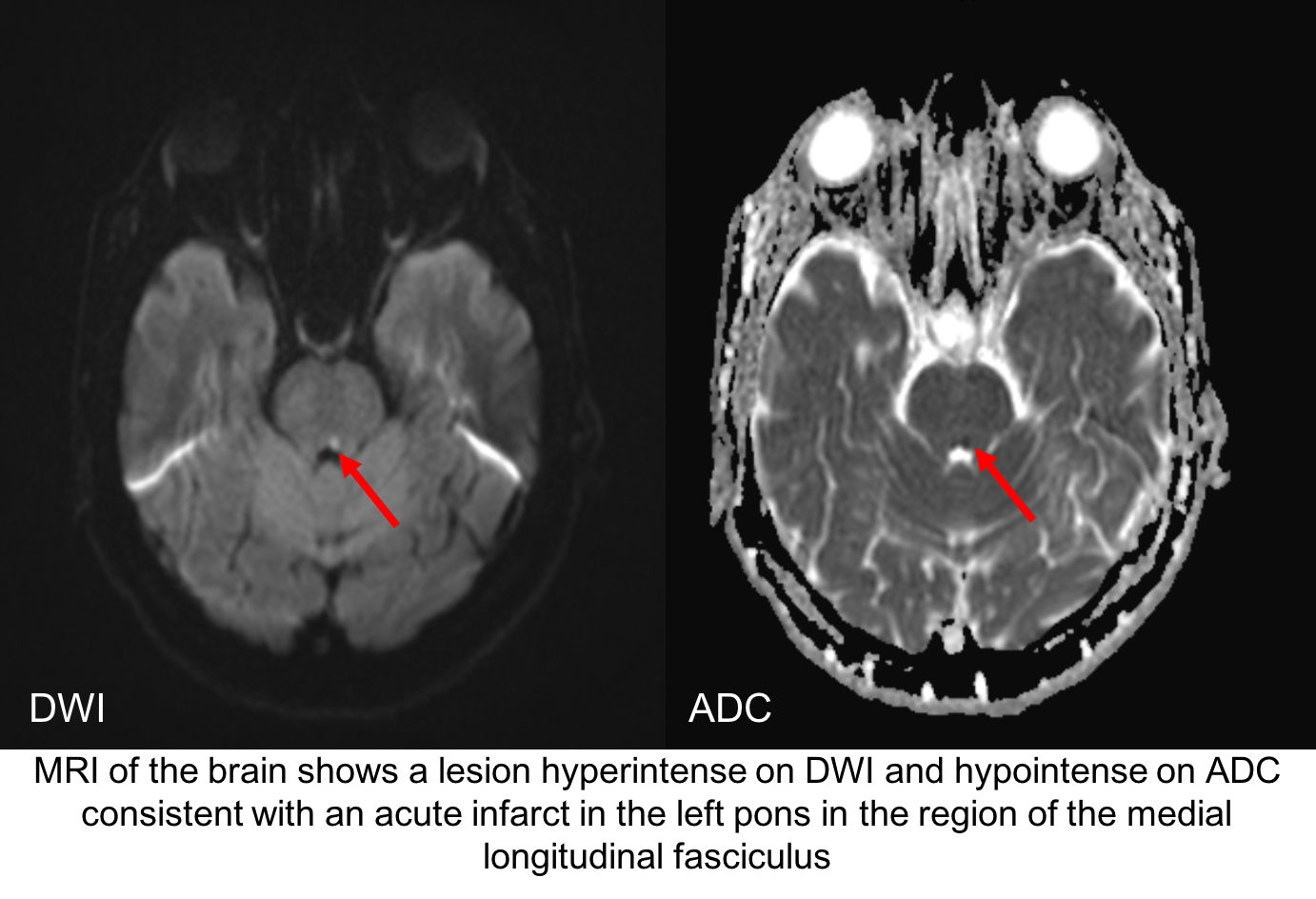
An MRI of the brain is the next most appropriate test for this patient to evaluate the brainstem, particularly the region of the left MLF. Since this is a unilateral INO in an older patient with vascular risk factors, ischemia is the most likely cause. Usually the lesion is small and may be subtle on MRI.
4. What would you expected to see in his right eye when he looks to the right?
- Slowing of abducting saccades
- Abduction nystagmus
- Pupillary constriction
- Globe retraction
4. What would you expected to see in his right eye when he looks to the right? 2. Abduction nystagmus
A left INO was suspected in this patient and was confirmed with MRI that showed a lesion in the region of the left MLF. An additional clinical sign of an INO is abduction nystagmus in the eye contralateral to the lesion, although this may not always be seen. The exact mechanism of the nystagmus is not known but theories include an adaptive response to overcome the weakness of the contralateral medial rectus muscle or involvement of adjacent structures such as the vestibular nuclei.
5. What is the prognosis for the left ischemic INO in this patient?
- Will be stable without improvement
- Should worsen within 3 months
- Should resolve within 3 months
- Should resolve between 8 and 12 months
5. What is the prognosis for the isolated left ischemic INO in this patient? 3. Should resolve within 3 months
Similar to ischemic ocular motor nerve palsies, INO secondary to ischemia has a good prognosis with most patients having their deficit resolve within 2-3 months. The presence of associated neurological deficits has a worse prognosis likely due to the larger size of the causative lesion.
6. Fibers subserving which type of conjugate eye movements are found in the medial longitudinal fasciculus (MLF)?
- Saccades
- Quick phases of nystagmus
- Smooth pursuit and optokinetic following
- Vestibular slow phases
- All of the above
6. Fibers subserving which type of conjugate eye movements are found in the medial longitudinal fasciculus (MLF)? 5. All of the above
The MLF is a long tract and contains fibres subserving all types of eye movements including vestibular slow phases, smooth pursuit and optokinetic following, and saccades and quick phases of nystagmus.
7. A new patient has a lesion in the region of the left MLF seen on MRI, but has full range of motion when smooth pursuit was tested. How should you assess the patient’s eye movements to better elicit any possible deficit from an INO?
- Test range of motion with the dolls head maneuver
- Test saccades
- Ask the patient to rest for 30 minutes and re-test smooth pursuit
- Test optokinetic nysatgmus with an OKN drum
7. A new patient has a lesion in the region of the left MLF seen on MRI, but has full range of motion when smooth pursuit was tested. How should you assess the patient’s eye movements to better elicit any possible deficit from an INO? 2. Test saccades
Although fibers subserving all types of eye movements are carried in the MLF, the adduction weakness may be more obvious for saccades since damaged axons show a greater defect for high-frequency rather than low-frequency impulses. Saccades are best tested by asking the patient to make a large amplitude, quick movement from one object to another. A decrease in velocity or acceleration of adduction may be the only sign of an INO and may be missed if only pursuit eye movements are tested.
Clinical Pearl
Testing saccades is important since a patient with a mild INO may have full range of motion, but slowed adduction saccades.
8. A patient with limitation of adduction from a unilateral INO has normal convergence. What does this suggest?
- The lesion is located higher up in the brainstem (rostral) with involvement of the medial rectus subnucleus
- The lesion is located lower down in the brainstem (caudal) with preservation of the medical rectus subnucleus
- The lesion is located more lateral in the brainstem with involvement of the utricle-ocular motor pathways
- There are multiple lesions in the brainstem
8. A patient with limitation of adduction from a unilateral INO has normal convergence. What does this suggest? 2. The lesion is located lower down in the brainstem (caudal) with preservation of the medical rectus subnucleus
Preservation on convergence despite absence of voluntary adduction implies that the lesion is located caudally (lower down) in the brainstem without affecting the medial rectus subnucleus in the oculomotor nuclear complex. This has been referred to as a “posterior INO” by Cogan. The absence of convergence does not necessarily imply a rostral lesion since some patient are not able to produce a strong convergence effort.
9. Which of the following is true regarding the causes of INO?
- Infarction is a common cause in older patients and is more likely to be bilateral
- Demyelination is a common cause in younger patients and may produce a bilateral INO
- Compression by a basilar artery aneurysm is a common cause in younger patients and is more likely to be bilateral
- Infection has not been reported as a cause
9. Which of the following is true regarding the causes of INO? 2. Demyelination is a common cause in younger patients and may produce a bilateral INO
The most common causes of INO are ischemia and demyelination. The former is more common in older individuals, especially those with vascular risk factors. Ischemia typically causes a unilateral INO, although there may be subtle involvement of the fellow eye. Demyelination is more common in younger individuals and often causes bilateral involvement, although this may be asymmetric. In a case series of 410 neurology inpatients with INO, the most common causes were infarction (38%), multiple sclerosis (34%), and others (28%). Other causes included trauma, tentorial herniation, infection, tumor, and iatrogenic injury.
10. A patient with a left INO was also found to have a left hypertropia. This is likely due to the presence of a:
- Fourth nerve palsy
- Third nerve palsy
- Sixth nerve palsy
- Skew deviation
10. A patient with a left INO was also found to have a left hypertropia. This is likely due to the presence of a: 4. Skew deviation
Skew deviation may be seen in patients with unilateral INO since vestibular pathways also ascend within the MLF. If there is a skew deviation with an INO, the higher eye is usually on the side of the lesion. Skew deviation is rarely seen in patients with bilateral INOs. Medial longitudinal fasciculus lesions in the caudal midbrain may cause an INO with a 4th nerve palsy. In these cases, the hypertropia will be in the eye contralateral to the eye with the INO since the 4th cranial nerves cross before exiting the midbrain dorsally. The hypertropic eye should be excyclotorted in a 4th nerve palsy and incyclotorted in a skew deviation.
11. What type of nystagmus may be seen in a patient with INO?
- Upbeat in up gaze
- Downbeat in down gaze
- Torsional nystagmus
- All of the above
11. What type of nystagmus may be seen in a patient with INO? 5. All of the above
In addition to abduction nystagmus in the contralateral eye, other patterns of nystagmus are often seen in patients with INO. Vertical nystagmus is common (upbeat in upgaze or downbeat in downgaze) and may be due to involvement of descending fibers from the interstitial nucleus of Cajal (INC) or nearby paramedian cell groups that transmit information to the flocculus. Torsional nystagmus in the setting of MLF injury is almost always ipsilesional (the superior poles move towards the side of the lesion) and is due to involvement of the semicircular canal pathways. Jerk or hemi-seesaw nystagmus with dissociated vertical components may also be observed.
12. What should be seen in a patient with a right one-and-a-half syndrome?
- Bilateral abduction deficits
- Left abduction nystagmus
- Left adduction and abduction nystagmus
- Right abduction nystagmus
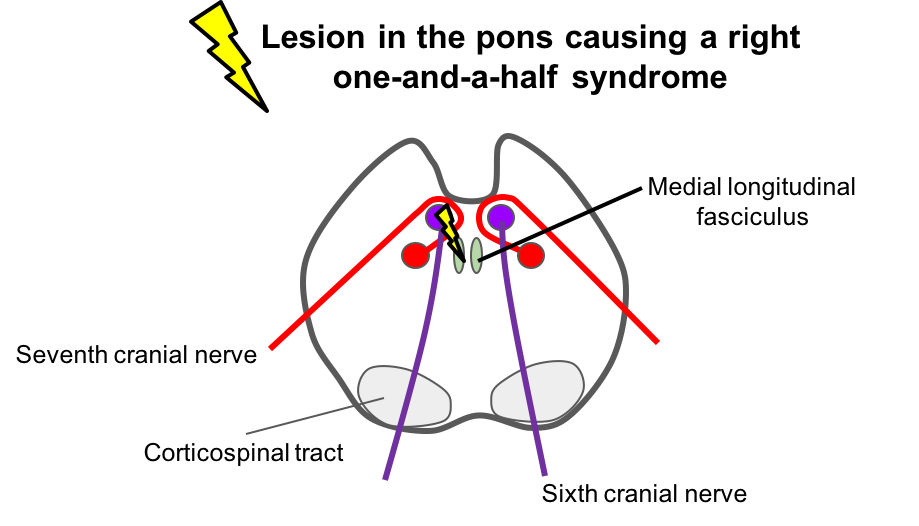
12. What should be seen in a patient with a right one-and-a-half syndrome? 2. Left abduction nystagmus
A one-and-a-half syndrome consists of a horizontal gaze palsy and internuclear ophthalmoplegia (INO), due to a lesion affecting the 6th nerve nucleus and adjacent medial longitudinal fasciculus (MLF). In a patient with a right one-and-a-half syndrome, there is a right horizontal gaze palsy (the patient cannot look to the right) and a right INO (limitation of adduction in the right eye and intact abduction of the left eye with abducting nystagmus). Like INO, the most common cause of one-and-a-half syndrome is demyelination in younger individuals and stroke in older individuals.
13. In a patient with a right one-and-a-half syndrome, what other cranial nerve is likely to be dysfunctional?
- Cranial nerve 4
- Cranial nerve 5
- Cranial nerve 7
- Cranial nerve 8
13. In a patient with a right one-and-a-half syndrome, what other cranial nerve is likely to be dysfunctional? 3. Cranial nerve 7
A one-and-a-half syndrome should almost always be associated with an ipsilateral seventh nerve palsy since the lesion is in the dorsal tegmentum of the caudal pons where the 6th nerve nucleus, MLF, and facial nucleus/fascicle are in close proximity. Facial nerve function should be examined carefully in every patient with a one-and-a-half syndrome.
14. What is the usual position of the eyes in primary position in a patient with a unilateral INO?
-
- Orthophoric or slight exophoria
- Large exotropia
- Large esotropia
- Alternating between esotropia and exotropia
14. What is the usual position of the eyes in primary position in a patient with a unilateral INO? 1. Orthophoric or slight exophoria
In a patient with a unilateral INO, the eyes are usually well-aligned in primary position, but may be slightly exophoric on alternate cover testing. A primary position exotropia may be seen in a patient with a one-and-a-half syndrome due to tonic abduction of the contralateral eye (known as paralytic pontine exotropia). Patients with bilateral INO may have disruption of the vergence and oculomotor pathways resulting in a wall-eyed, bilateral INO (WEBINO).
15. A patient presents with confusion and ataxia and is found to have bilateral INOs. His history is significant for alcohol abuse. What treatment should be initiated as soon as possible?
- Niacin
- Ethanol
- Thiamine
- Glucose
15. A patient presents with confusion and ataxia and is found to have bilateral INOs. His history is significant for alcohol abuse. What treatment should be initiated as soon as possible? 3. Thiamine
Wernicke’s encephalopathy is characterized by the triad of ophthalmoplegia, encephalopathy (confusion), and ataxia. It may present with a variety of ocular motor findings including INO, weakness of abduction, nystagmus and total ophthalmoplegia. It is caused by thiamine deficiency and is most commonly encountered in alcoholics. Thiamine should be initiated immediately in suspected cases to prevent Korsakoff’s syndrome with severe and enduring memory loss.
16. A patient has significant limitation of adduction in the right eye and abduction nystagmus in the left eye. MRI of the brain is normal. What test should be considered for this patient?
- Computed tomography angiography (CTA)
- Magnetic resonance venography (MRV)
- Acetylcholine receptor antibodies
- Multifocal electroretinogram (mfERG)
16. A patient has significant limitation of adduction in the right eye and abduction nystagmus in the left eye. MRI of the brain is normal. What test should be considered for this patient? 3. Acetylcholine receptor antibodies
Pseudo-INO is a well-recognized manifestation of ocular myasthenia gravis. This is because myasthenia has a predilection for involving the muscles innervation by the oculomotor nerve, particularly the medial rectus muscle. Ocular myasthenia gravis is discussed in more detail in the next chapter.
Case Summary
He had the new onset of horizontal binocular diplopia primarily when looking to the right. Examination showed limitation of adduction in the left eye and abduction nystagmus in the right eye, highly suggestive of an left INO. This was confirmed with MRI of the brain, which showed an acute infarct in the left pons. He was seen in consultation by a stroke neurologist for optimization of his vascular risk factors. His double vision resolved in 2 months.
Further reading:
-
Virgo JD, Plant GT. Internuclear ophthalmoplegia. Pract Neurol 2017;17(2):149153. https://www.ncbi.nlm.nih.gov/pubmed/27927777
-
Keane JR. Internuclear ophthalmoplegia: unusual causes in 114 of 410 patients. Arch Neural 2005;62(5):714-7. https://jamanetwork.com/journals/jamaneurology/fullarticle/788389
-
Frohman TC, Galetta S, Fox R, et al. Pearls and Oy-sters: the medial longitudinal fascicles in ocular motor physiology. Neurology 2008;70(17):e57-67. https://www.ncbi.nlm.nih.gov/pubmed/18427066