13
Case
Age: 69-year-old white man
Reason for referral to ophthalmology: Bilateral visual field defect
Past medical history: Hypertension
Past ocular history: Cataract surgery with posterior chamber intraocular lens in both eyes 1 month ago
Medications: Amlodipine, hydrochlorothiazide
Habits: Smokes ½ pack per day for 30 years, 1-2 glasses of wine per day
HPI: He noticed blurry vision in both eyes for several months. He saw an ophthalmologist who diagnosed cataracts and performed cataract surgery in both eyes 1 month ago. After the cataract surgery, he noticed blurry vision on the right side of his visual field in both eyes. A neuro-ophthalmology consultation was requested.
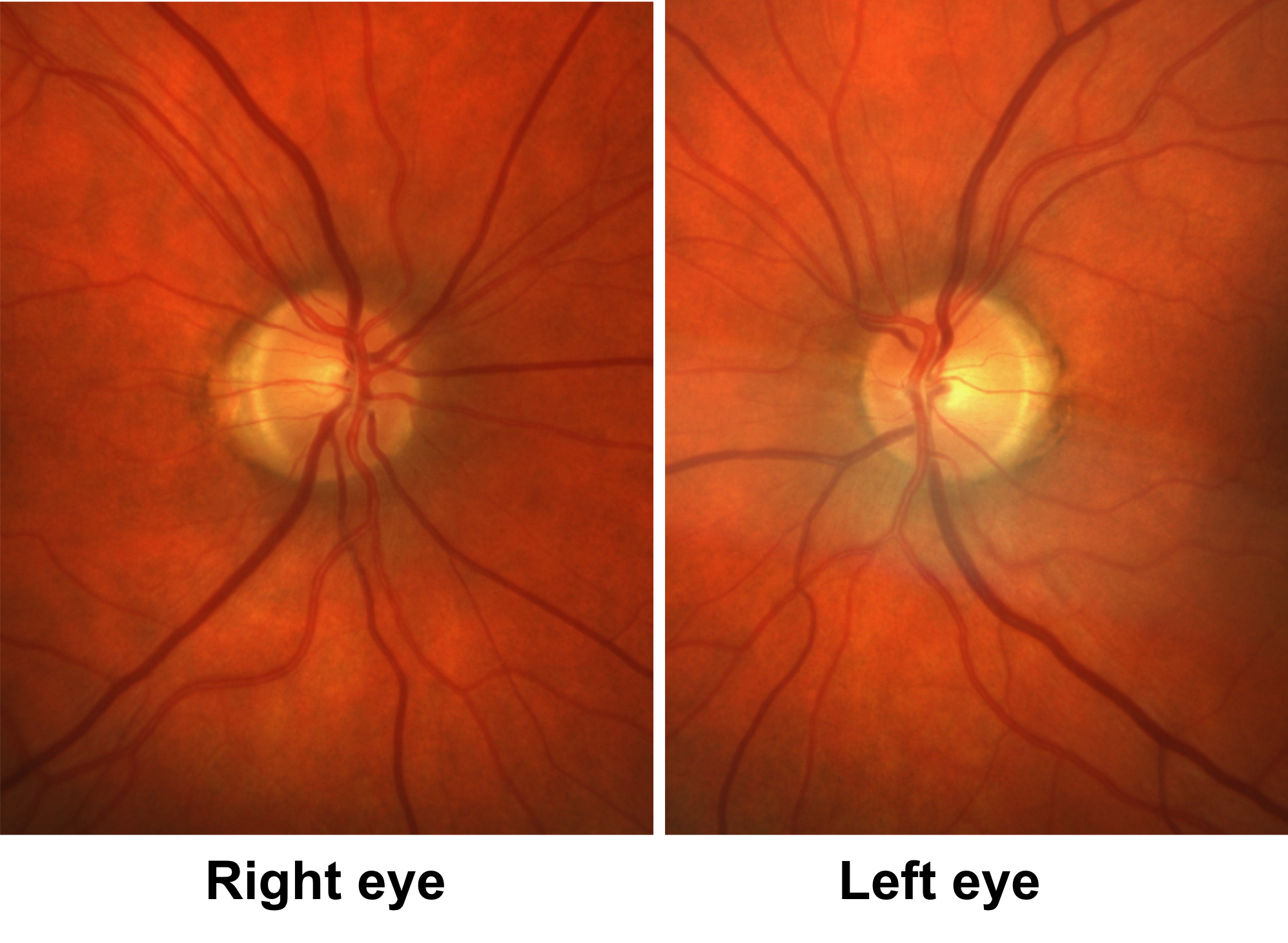
Ophthalmological examination:
Blood pressure: 143/86, heart rate 86
Visual acuity is discussed in the first multiple choice question.
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision: 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal
Slit lamp examination is normal. There are posterior-chamber intraocular lenses.
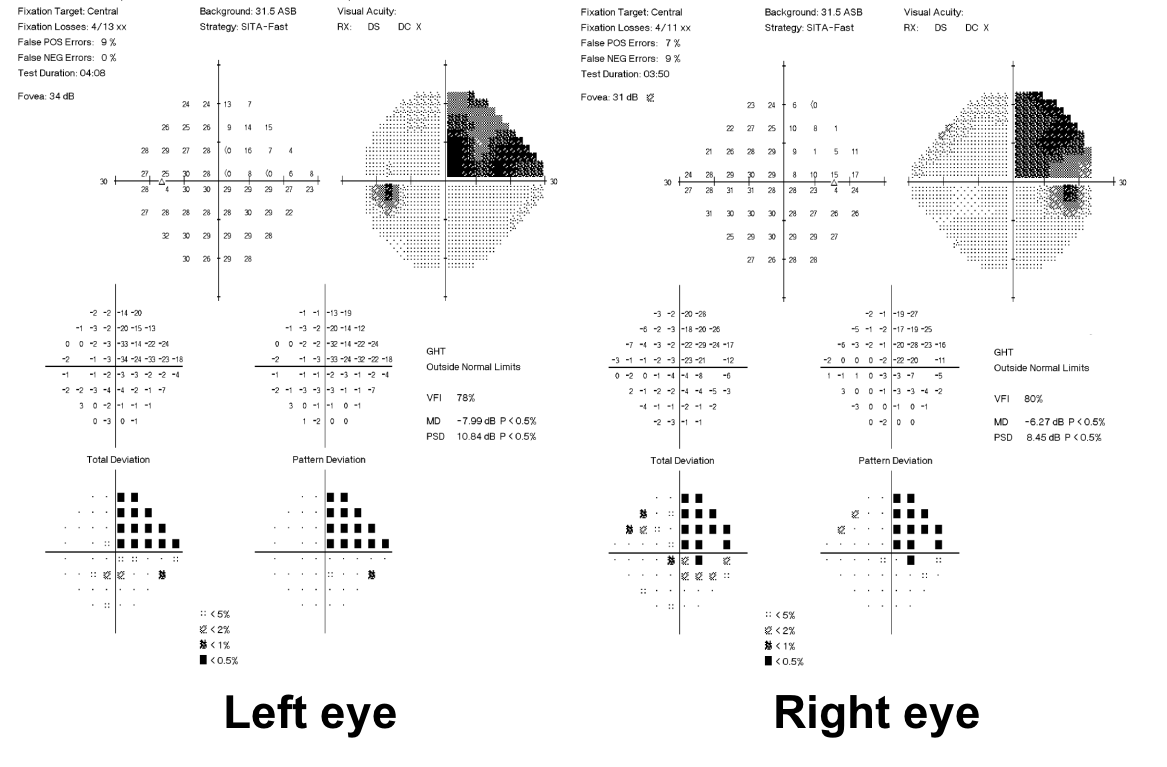
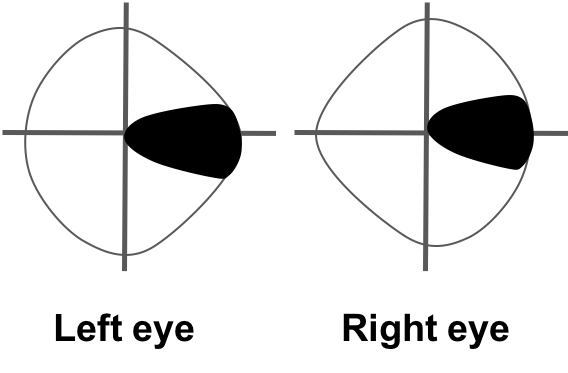
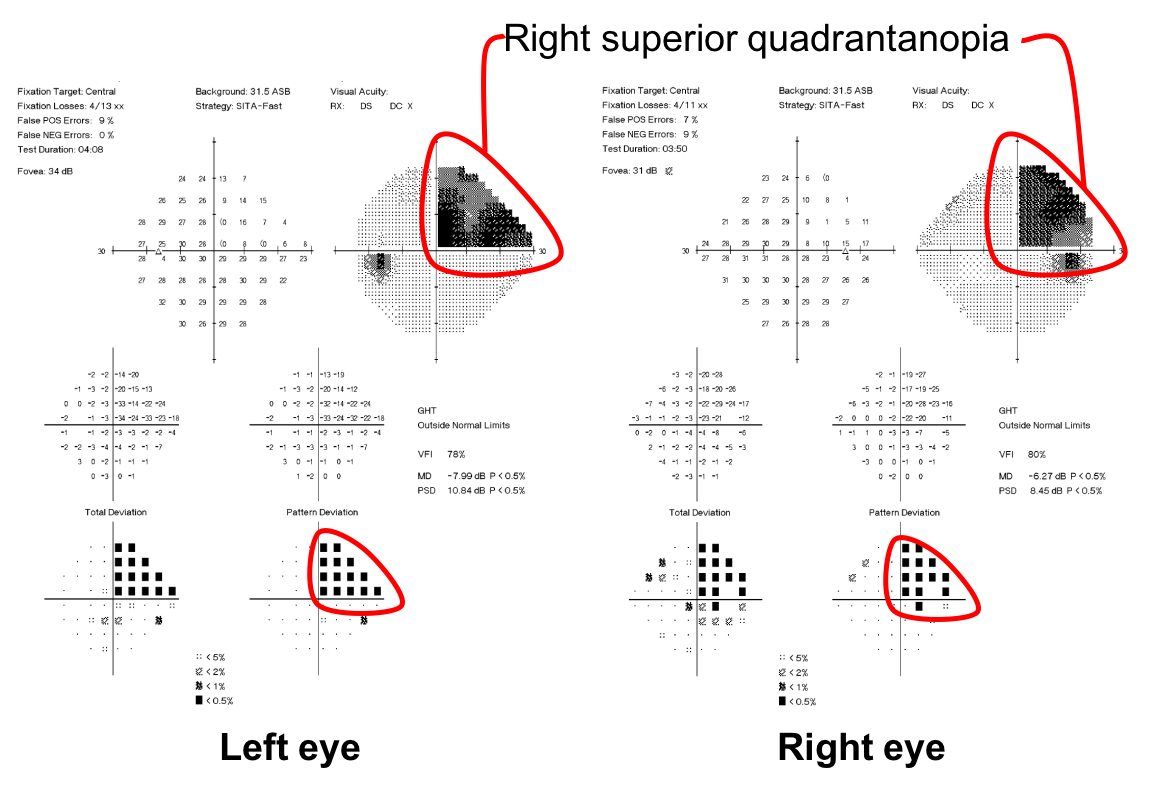
Neurological examination is normal apart from the visual field defect shown below.
1. This patient’s visual field defect localizes to which part of the visual system?
- Anterior segment
- Bilateral optic nerves
- Optic chiasm
- Retrochiasmal visual pathways
1. This patient’s visual field defect localizes to which part of the visual system? 4. Retrochiasmal visual pathways
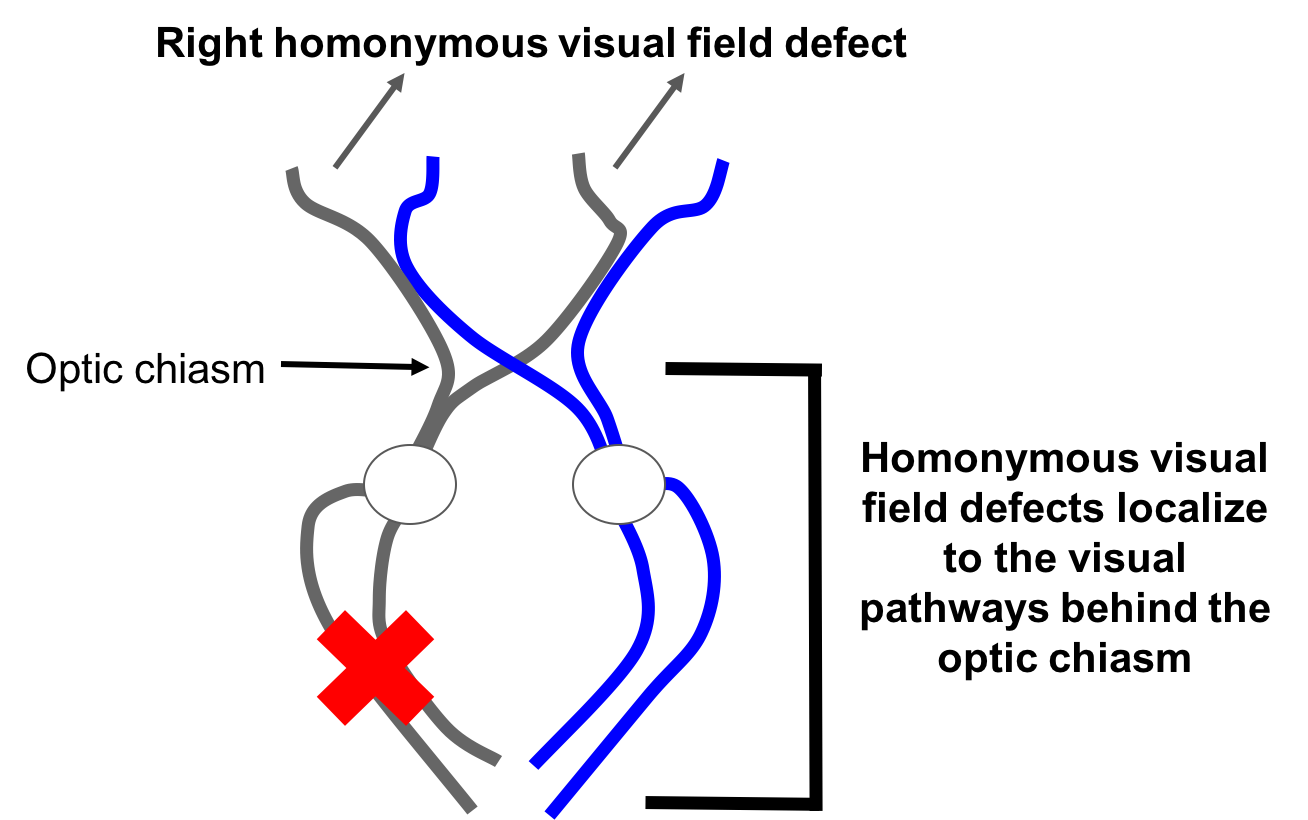
This patient has homonymous visual field defects, meaning that are on the same side of the visual field in both eyes. This localizes to the retrochiasmal visual pathways in the brain and not the eye or optic nerves. Since it is a right-sided visual field defect, the lesion is on the left side of the brain.
2. What do you expect this patient’s visual acuity to be?
- He should have preserved visual acuity in both eyes
- His visual acuity will be moderately affected in both eyes
- He will have poor visual acuity in both eyes
- The right eye will have worse visual acuity than the left eye since the temporal visual field is involved
2. What do you expect this patient’s visual acuity to be? 1. He should have preserved visual acuity in both eyes
Regardless of the size or shape of a retrochiasmal visual field defect, visual acuity should be preserved. There are 2 exceptions to this rule: 1) if there is a superimposed lesion in the anterior visual pathway or 2) there are bilateral retrochiasmal defects. This patient’s visual acuity was 20/20 in each eye.
Clinical Pearl
Visual acuity is preserved in patients with unilateral retrochiasmal visual field defects
3. What is the rule of congruity?
- The more anterior the lesion in the retrogeniculate visual pathway, the more congruous the visual field defect
- The more posterior the lesion in the retrogeniculate visual pathway, the more congruous the visual field defect
- The more posterior the lesion in the retrogeniculate visual pathway, the more likely it is to be a complete homonymous defect
- The more congruous the visual field defect, the less likely there will be a relative afferent pupillary defect
3. What is the rule of congruity? 2. The more posterior the lesion in the retrogeniculate visual pathway, the more congruous the visual field defect
A congruous visual field defect is one that is very similar in both eyes, such as that seen in this patient. The classic “rule of congruity” states that the more posterior the lesion in retrochiasmal visual pathway, the more congruous the visual field defect is. This is because just posterior to the lateral geniculate nucleus crossed and uncrossed fibers corresponding to the same visual field area remain spatially distant, whereas they run together in the occipital lobe. The rule of congruity only applies to incomplete homonymous visual field defects, because complete homonymous visual defects in themselves are nonlocalizing (other than to say they are located in the retrochiasmal visual pathway). This is because a lesion anywhere in the retrochiasmal visual pathway has the potential to affect all afferent fibers and produce a complete homonymous defect. This rule is not absolute since up to 16% of occipital lobe lesions are incongruous and should not be applied to optic tract lesions since up to 50% of optic tract lesions are congruous.
Clinical Pearl
Complete homonymous hemianopias are non-localizing (other than to say they are located in the retrochiasmal visual pathways).
4. Where is the lesion producing this visual field defect most likely to be located?
- Optic tract
- Temporal lobe
- Parietal lobe
- Occipital lobe
4. Where is the lesion producing this visual field defect most likely to be located? 4. Occipital lobe
This patient has an isolated right superior quadrantanopia. This is a congruous lesion (it is very similar in both eyes) which suggests the lesion is located posteriorly in the retrogeniculate visual pathway. A superior quadrantanopia was found in a large case series to localize in a large majority of cases to the occipital lobe (83%), followed by the temporal lobe (13%) and parietal lobe (3%).
5. Which of the following can cause a homonymous visual field defect?
- Stroke
- Trauma
- Neurosurgical procedures
- Neoplasms
- All of the above
5. Which of the following can cause a homonymous visual field defect? 5. All of the above
In a study of 850 patients with 902 homonymous hemianopias, 70% had vascular lesions such as infarction or hemorrhage and the remaining 30% had lesions from trauma, tumor, neurosurgical procedures, or demyelinating disease. Rarer causes of homonymous visual field defects include occipital lobe seizures, posterior cortical atrophy, the Heidenhain variant of Creutzfeld-Jacob disease, and hyperosmolar nonketotic hyperglycemia.
6. What is the next best step in the workup of this patient?
- MRI of the brain
- CBC, ESR, CRP
- MRI of the orbits
- Optimization of vascular risk factors
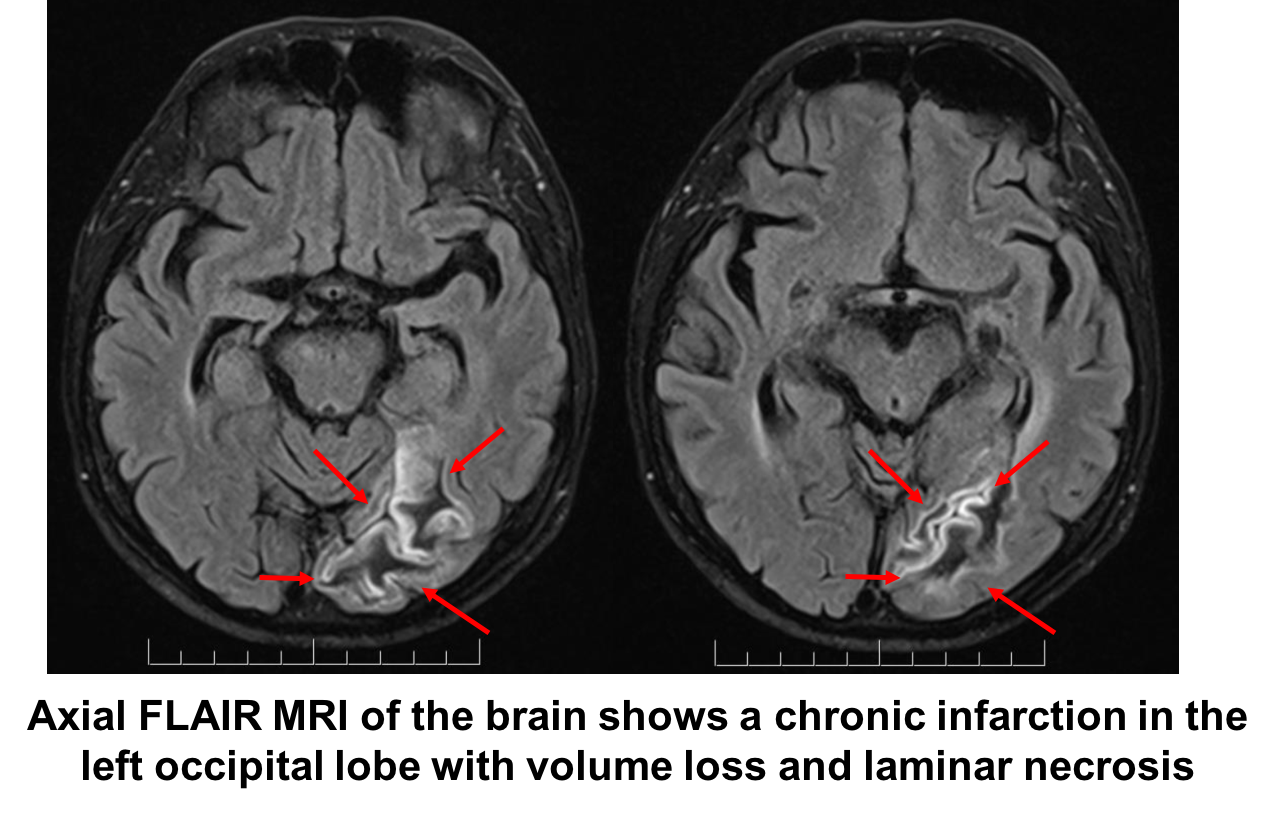
6. What is the next best step in the workup of this patient? 1. MRI of the brain
This patient has a homonymous visual field defect and requires neuroimaging to determine the nature of the lesion. The most likely lesion is a previous stroke, but the patient may also have a tumor, vascular malformation or other lesion in the retrochiasmal visual pathways.
7. A patient is having an anterior temporal lobectomy for the treatment of seizures. What is the anterior extent of Meyer’s loop in the temporal lobe?
- 1 cm
- 2.5 cm
- 5 cm
- 8 cm
7. A patient is having an anterior temporal lobectomy for the treatment of seizures. What is the anterior extent of Meyer’s loop in the temporal lobe? 2. 2.5 cm
A quantitative analysis of visual field defects related to anterior temporal lobectomy estimated an anterior extent of Meyer’s loop of 2.5 cm and a posterior extent of 7.5 cm with macular involvement at a resection length of 5.8 cm. Therefore, an anterior temporal lobectomy may produce some degree of a homonymous visual field defect when the resection is greater than 2.5 cm and a complete homonymous visual field defect when the resection is greater than 8 cm. Visual field defects due to temporal lobe lesions may also be associated with memory disturbances, complex auditory and visual disturbances, personality changes and a receptive aphasia.
Clinical Pearl
Visual field defects produced by temporal lobe lesions are often incomplete and superior due to the anatomy of Meyer’s loop
8. Which of the following may be seen with a homonymous hemianopia associated with a parietal lobe lesion?
- Relative afferent pupillary defect
- Macular sparing
- Impairment of smooth pursuit towards the side of the lesion
- Ipsilateral sensory changes
8. Which of the following may be seen with a homonymous hemianopia associated with a parietal lobe lesion? 3. Impairment of smooth pursuit towards the side of the lesion
Patients with homonymous visual field defects associated with lesions in the parietal lobe may also have impairment of smooth pursuit towards the side of the lesion. This is because of involvement of descending smooth pursuit fibers from the parieto-occipitotemporal junction as they pass near the optic radiation. An optokinetic nystagmus drum or tape can be used to detect this abnormality. Parietal lobe lesions may also cause sensory changes on the contralateral side due to involvement of the postcentral gyrus or more complex changes in sensory integration seen with testing of tactile discrimination and position sense. Lesions in the dominant parietal lobe can cause aphasia (more often a receptive aphasia) and involvement of the angular gyrus can cause Gerstmann’s syndrome (finger agnosia, right-left disorientation, agraphia and acalculia). Lesions in the nondominant parietal lobe may cause inattention or neglect and contribute to poor recovery.
Clinical Pearl
Parietal lobe lesions often affect the inferior part of the visual field more than the superior visual field
9. Which of the following localizes a homonymous visual field defect to the occipital lobe?
- Nystagmus
- Respects the horizontal meridian
- Preserved visual acuity
- Macular sparing
9. Which of the following localizes a homonymous visual field defect to the occipital lobe? 4. Macular sparing
A complete homonymous hemianopia with sparing of 2 to 10 degrees of central vision is characteristic of occipital lobe lesions. This is because the posterior pole of the occipital lobe has a dual blood supply from both the posterior and middle cerebral arteries. A stroke involving the posterior cerebral artery may produce a complete homonymous hemianopia with macular sparing since the occipital lobe pole still has an intact blood supply from the middle cerebral artery. This collateral blood supply is not found in other areas of the retrochiasmal visual pathways. Alternative theories for macular sparing have also been proposed and include a perimetric artifact and bilateral representation of the macula in the occipital lobes.

10. A right-handed patient is unable to read his own handwritten words. He also has a right homonymous visual field defect due to a stroke in the territory of the left posterior cerebral artery affecting the left occipital lobe. Which other structure is affected by the stroke?
- Right angular gyrus
- Splenium of the corpus callosum
- Optic chiasm
- Midbrain
10. A right-handed patient is unable to read his own handwritten words. He also has a right homonymous visual field defect due to a stroke in the territory of the left posterior cerebral artery affecting the left occipital lobe. Which other structure is affected by the stroke? 2. Splenium of the corpus callosum
This patient has alexia without agraphia, which is a disconnection syndrome between the dominant angular gyrus (region of language processing in anterolateral parietal lobe) and the occipital lobe. Visual information is received by the right occipital lobe and is normally transferred to the left angular gyrus by the corpus callosum. This cannot occur if the splenium of the corpus callosum is damaged as in this case. The patient can write because the structures anterior to the splenium of the corpus callosum are intact, but cannot read these words.
11. A patient presents with a complaint of seeing afterimages. She finds that she continues to see an object even after it has been removed from her visual field. What is this called?
- Pulfrich phenomenon
- Palinopsia
- Extinction
- Hemeralopia
11. A patient presents with a complaint of seeing afterimages. She finds that she continues to see an object even after it has been removed from her visual field. What is this called? 2. Palinopsia
Palinopsia is the preservation of afterimages and may be associated with a homonymous hemianopia (palinoptic images appear in the blind hemifield). Palinopsia may be seen in the context of migraines, hallucinogenic drugs (LSD), other medications (eg. trazodone, topiramate), and lesions of the parieto-occipital lobe, usually in the nondominant hemisphere.
The Pulfrich phenomenon is when a small object oscillating in the frontal plane appears to be moving in an elliptical path in a patient with unilateral or asymmetric bilateral optic neuropathies. Extinction is the inability to see a stimulus in one hemifield when a target is simultaneously presented to both hemifields. Hemeralopia refers to a deterioration of vision in bright light and is seen in patients with cone dystrophy.
12. A 64-year-old woman complains of difficulty driving at night and reading. Her examination reveals a right homonymous hemianopia, but MRI does not show any evidence of a stroke or tumor. What other abnormality might also be detected on examination?
- Memory impairment
- Simultagnosia
- Nonfluent speech
- Parkinsonian tremor
12. A 64-year-old woman complains of difficulty driving at night and reading. Her examination reveals a right homonymous hemianopia, but MRI does not show any evidence of a stroke or tumor. What other abnormality might also be detected on examination? 2. Simultagnosia
In this patient with difficulty processing visual information and a homonymous visual field defect without evidence of a structural abnormality, posterior cortical atrophy should be suspected. This is a neurodegenerative condition characterized by a progressive decline in visual processing skills, but relative preservation of memory, executive functions, and linguistic skills due to involvement of the parietal-occipital areas. It has been considered a visual variant of Alzheimer’s disease. Testing of higher order visual processing usually reveals simultagnosia, which is an inability to see the visual scene as a whole despite the ability to identify individual elements. This may be part of Balint syndrome (simultagnosia, oculomotor apraxia, optic ataxia) and associated with elements of Gerstmann’s syndrome (finger agnosia, right-left disorientation, agraphia and acalculia). Findings that support this diagnosis are focal or asymmetric atrophy in parietal or occipital regions on MRI or focal or asymmetric hypometabolism/hypoperfusion in parietal or occipital regions on functional imaging.
13. In a patient with severe bilateral vision loss, what finding on examination would support bilateral occipital lobe involvement rather than a bilateral optic neuropathy?
- Relative afferent pupillary defect
- Miotic pupils
- Normally reactive pupils
- Tadpole pupils
13. In a patient with severe bilateral vision loss, what finding on examination would support bilateral occipital lobe involvement rather than a bilateral optic neuropathy? 3. Normally reactive pupils
A patient with cortical blindness would have a normal fundus examination and a normal pupillary examination. This is because the afferent fibers in the pupillary pathway leave the optic tract and go to the midbrain and are not affected by lesions in the occipital lobe. A patient with severe bilateral optic neuropathies would be expected to have sluggish, minimally reactive or nonreactive pupils due to the impairment of information entering the pupillary pathway. The reactivity of the pupils is one way to help differentiate these two causes of severe bilateral vision loss.
Clinical Pearl
Pupil reactivity is not affected by retrogeniculate visual pathway lesions.
14. A patient has severe bilateral visual field defects but sparing of the temporal crescent (located between 60 and 90 degrees). Where is the lesion producing his visual loss?
- Optic tract
- Temporal lobe
- Parietal lobe
- Occipital lobe
14. A patient has severe bilateral visual field defects but sparing of the temporal crescent (between 60 and 90 degrees). Where is the lesion producing his visual loss? 4. Occipital lobe
The monocular temporal crescent is an area of the visual field that has no correlate in the nasal visual field of the fellow eye. Lesions in the occipital visual cortex tend to spare this temporal crescent, whereas those in the anterior visual pathways tend to destroy it. It is therefore of high localizing value. The monocular temporal crescent is located between 60 and 90o from fixation and is detected with Goldmann visual field testing and missed by Humphrey visual fields.
15. A patient with blindness due to diffuse damage to the occipital lobes is unaware of his deficit and denies he is blind. This is called:
- Riddoch syndrome
- Pulfrich syndrome
- Anton syndrome
- Gerstmann syndrome
15. A patient with blindness due to diffuse damage to the occipital lobes is unaware of his deficit and denies he is blind. This is called: 3. Anton syndrome
Anton syndrome is a denial of blindness seen in patients with cortical blindness. The pathophysiology remains unclear, but may be related to a lesion elsewhere in the brain.
16. What is the natural history of homonymous hemianopias?
- Do not improve
- Improve usually within the first 3 months and not after 6 months
- Continuous improvement throughout life
- Improvement up to 2 years after onset
16. What is the natural history of homonymous hemianopias? 2. Improve usually within the first 3 months and not after 6 months
A large natural history study of 263 homonymous hemianopias of various etiologies found that almost 40% improved. Improvement decreased with increasing time after injury. In most cases, improvement was within the first 3 months after injury and improvement after 6 months was mainly due to improvement in the patient’s ability to perform visual field testing reliably.
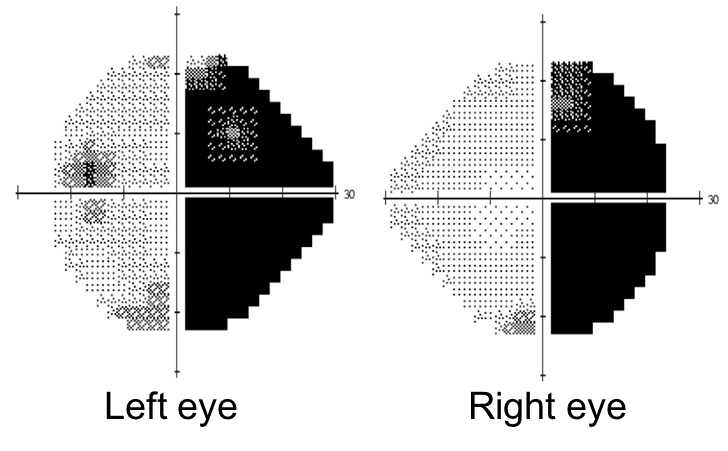
17. A patient presents with left hemianesthesia and hemiparesis and the following visual field defect. Where is the most likely location of the lesion?
- Bilateral optic nerves
- Optic chasm
- Lateral geniculate nucleus
- Occipital lobe
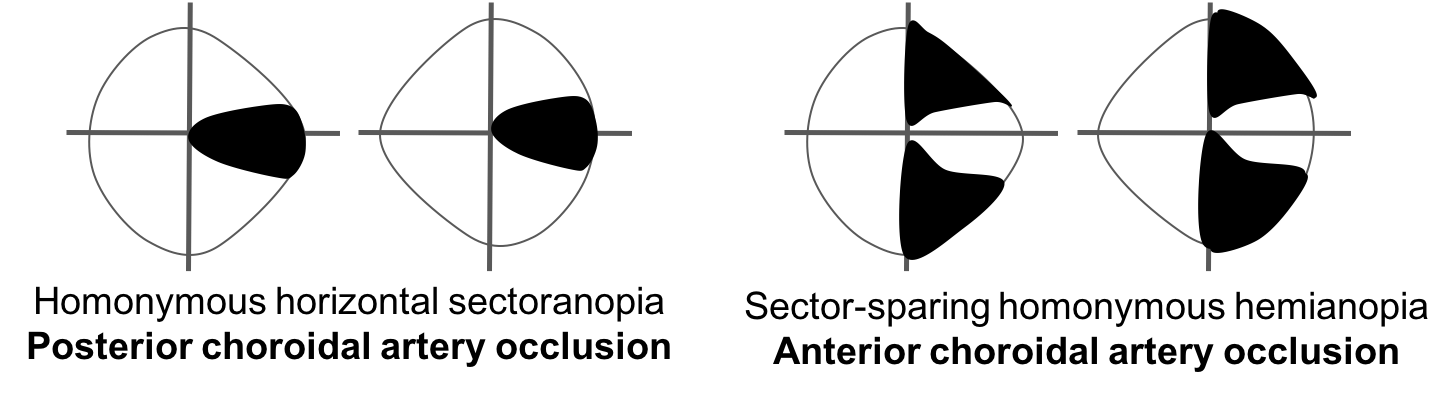
17. A patient presents with left hemianesthesia and hemiparesis and the following visual field defect. Where is the most likely location of the lesion? 3. Lateral geniculate nucleus
Compressive and infiltrative lesions of the lateral geniculate nucleus (LGN) may cause an incongruous homonymous hemianopia. Vascular lesions may cause a “sectoranopia” due to the distinctive blood supply and retinotopic organization of the LGN (shown below). When sectoranopias occur, they are usually very congruous due to the well-defined vascular territories of the LGN. Involvement of neighbouring structures in the thalamus and pyramidal tracts may result in contralateral hemianesthesia or hemiparesis.
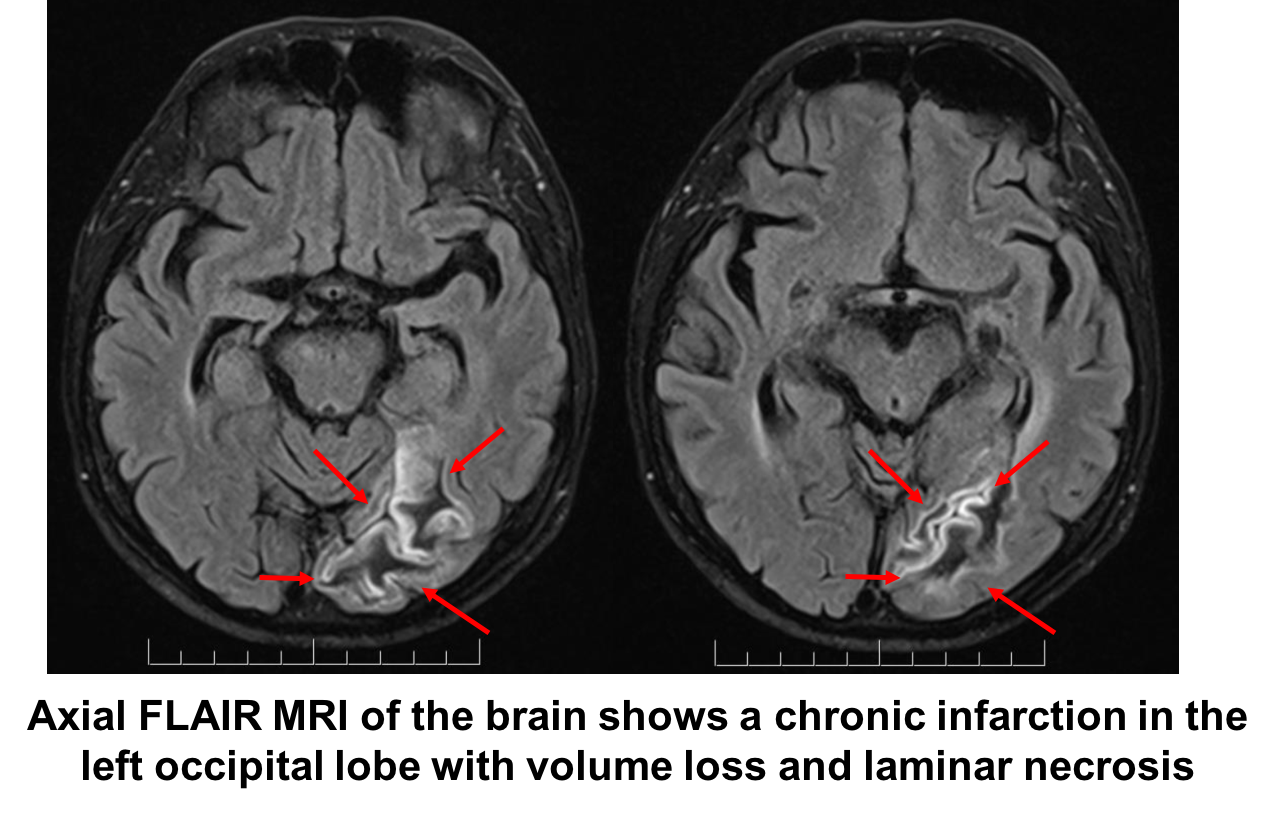
Case Summary
He had blurry vision in both eyes, but noticed that the right side of his visual field was particularly blurry after cataract surgery. Examination revealed a right superior homonymous quadrantanopia, which localized to the left retrochiasmal visual pathways. A congruous quadrantanopia such as this was highly suggestive of an occipital lobe lesion. MRI revealed a chronic left occipital infarction. He was referred to a stroke neurologist for further investigations. The regional driving requirements were reviewed and he did not meet the legal requirements. A follow-up visual field 6 months later remained stable.
Further reading:
-
Fraser JA, Newman NJ, Biousse V. Disorders of the optic tract, radiation, and occipital lobe. Handb Clin Neurol 2011;102:205-11. https://www.ncbi.nlm.nih.gov/pubmed/21601068
-
Jacobson DM. The localizing value of a quadrantanopia. Arch Neurol 1997;54:401-404. https://jamanetwork.com/journals/jamaneurology/article-abstract/594510?redirect=true
-
Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Homonymous hemianopia in stroke. J Neuroophthalmol 2006;26(3):180-3. https://www.ncbi.nlm.nih.gov/pubmed/16966935
-
Barton JJS, Hefter R, Chang B et al. The field defects of anterior temporal lobectomy: a quantitative reassessment of Meyer’s loop. Brain 2005;128:2123–2133. https://www.ncbi.nlm.nih.gov/pubmed/15917289
-
Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Natural history of homonymous hemianopia. Neurology 2006;66(6):901-5. https://www.ncbi.nlm.nih.gov/pubmed/16567709
-
Crutch SJ, Lehmann M, Schott JM, Rabinovici GD, Rossor MN, Fox NC. Posterior cortical atrophy. Lancet Neurol 2012;11(2):170-178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3740271/