22
Case
Age: 52-year-old woman
Reason for referral to ophthalmology: Double vision and difficulty looking upwards
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and does not drink alcohol
HPI: For the past 2 weeks, she has had difficulty looking upwards and has noticed double vision when looking to the right. When she looks to the right, objects are separated vertically and this resolves when she covers either eye. Her husband has noticed that she prefers to keep her chin positioned upwards and tilts her head towards the right shoulder. She saw her primary care physician who requested a neuro-ophthalmology consultation.
Ophthalmological examination:
Blood pressure: 126/85, heart rate 72
Visual acuity: 20/20 OD, 20/20 OS
Color vision: 14/14 correct Ishihara plates in both eyes
Slit lamp examination is normal
Neurological examination is otherwise normal apart from what is seen below. A video of her eye movements can be found at https://youtu.be/DL1hzVO5W2Y

1. Which of the following examination findings are present in this patient?
- Vertical gaze palsy
- Convergence-retraction nystagmus
- Light-near dissociation
- Papilledema
- All of the above
1. Which of the following examination findings are present in this patient? 5. All of the above
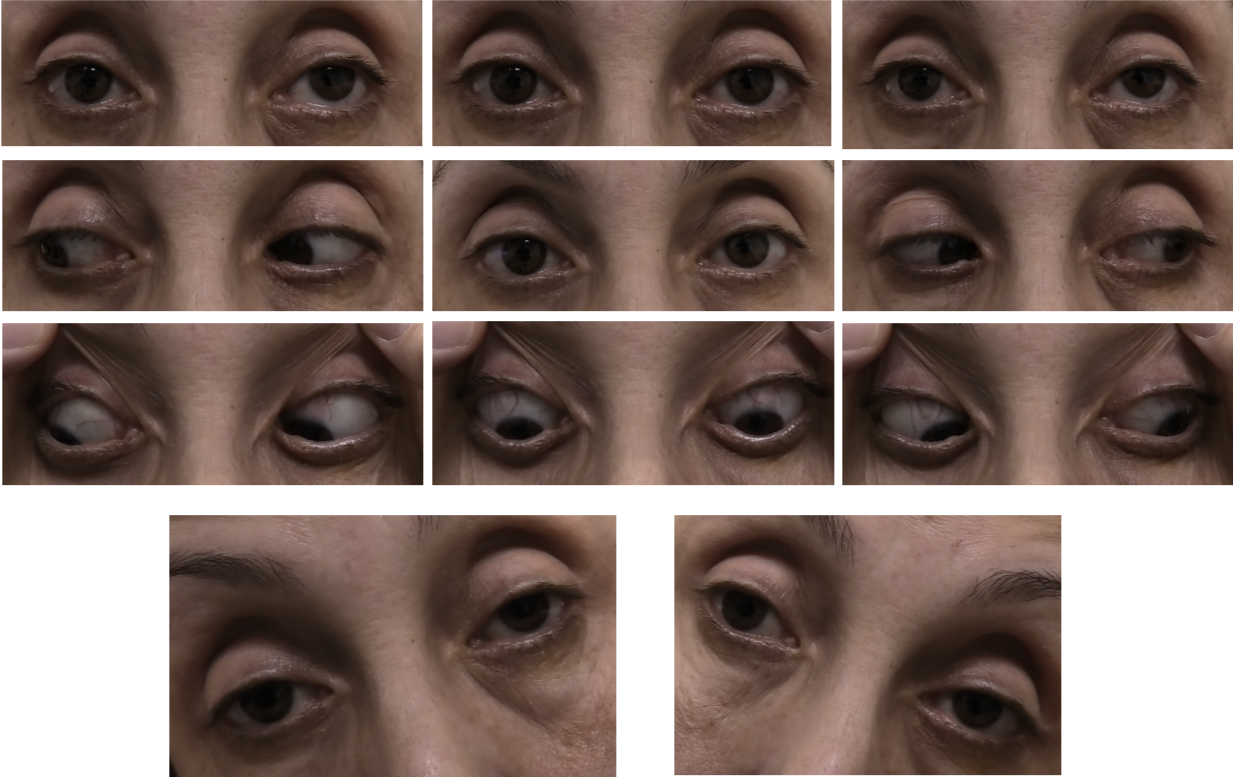
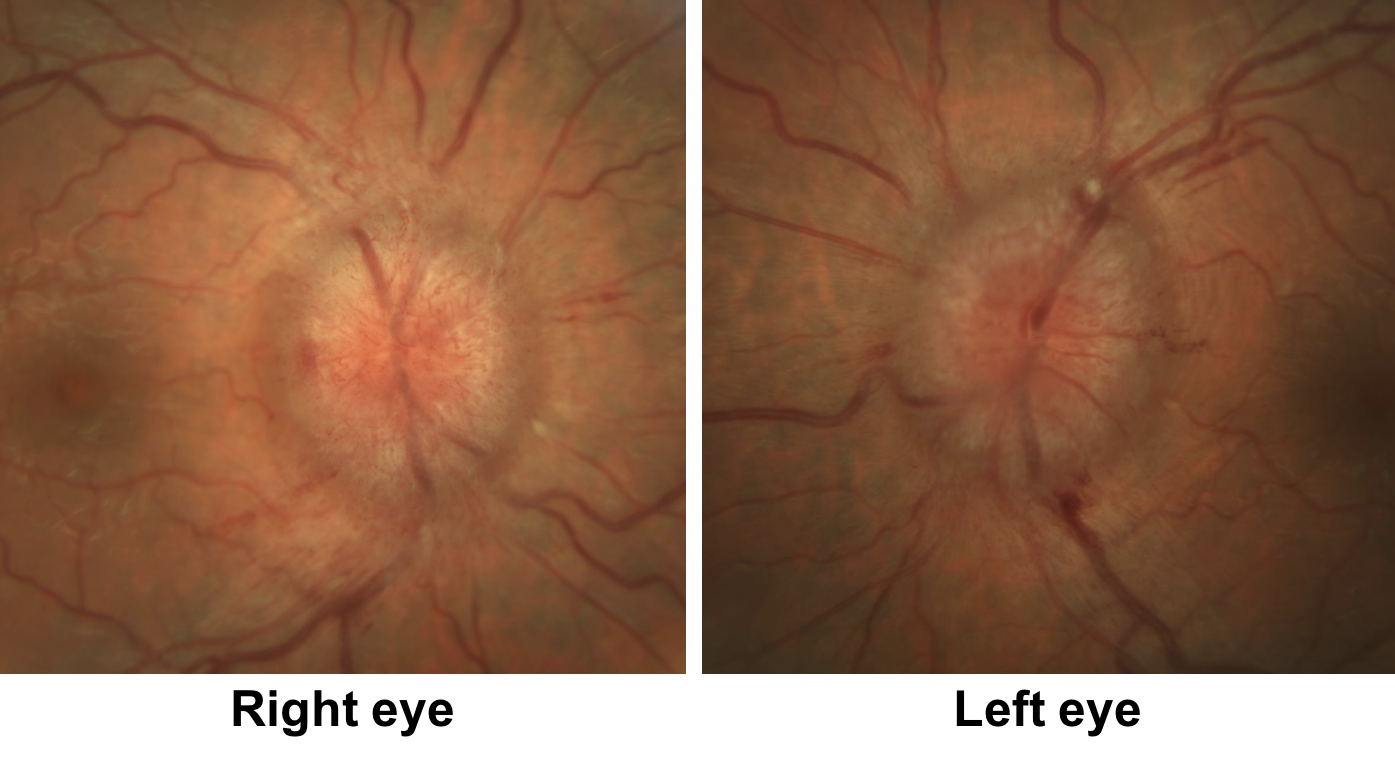
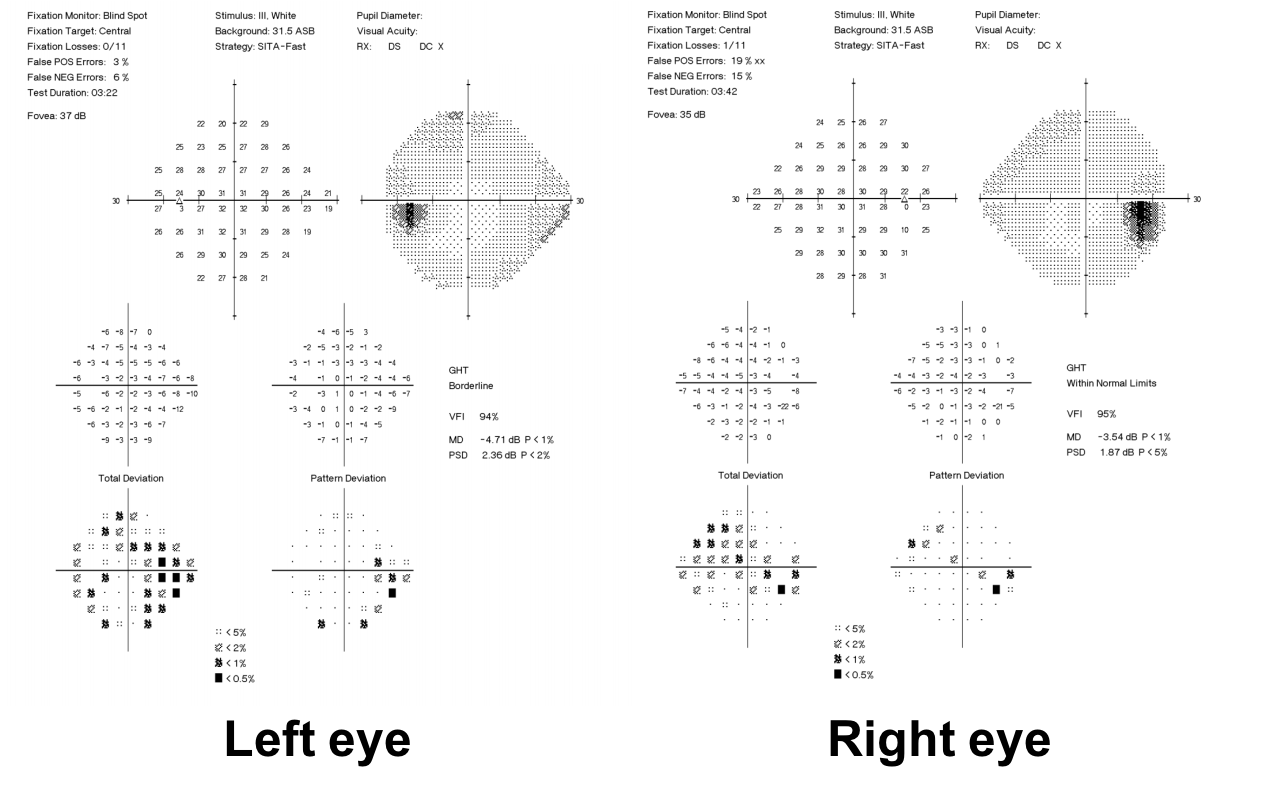
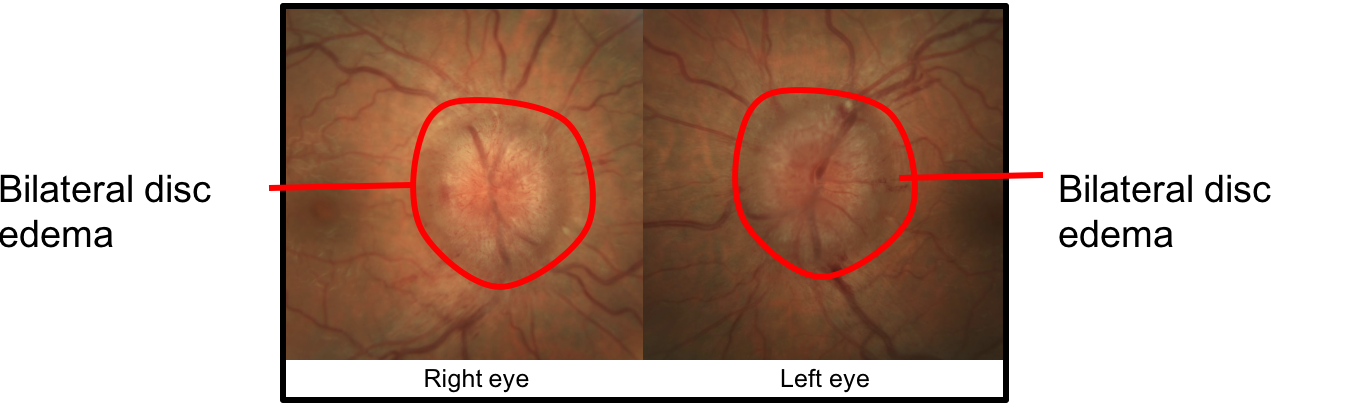
This patient has complete limitation of upward eye movements, light-near dissociation, convergence-retraction nystagmus (seen on the video) and bilateral optic disc edema with preserved vision function, highly suggestive of papilledema.
2. Where do these examination findings localize?
- Bilateral 3rd cranial peripheral nerve
- Cavernous sinus
- Dorsal midbrain
- Cervicomedullary junction
2. Where do these examination findings localize? 3. Dorsal midbrain
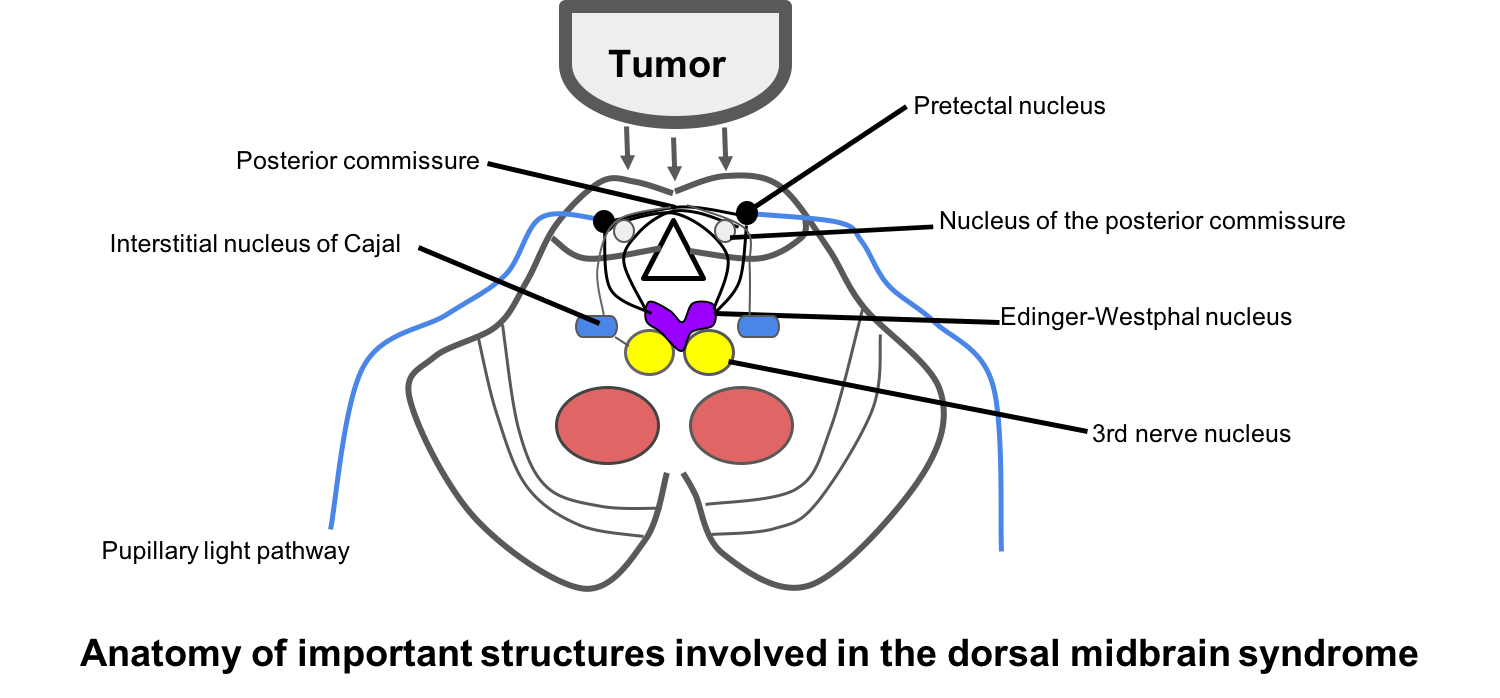
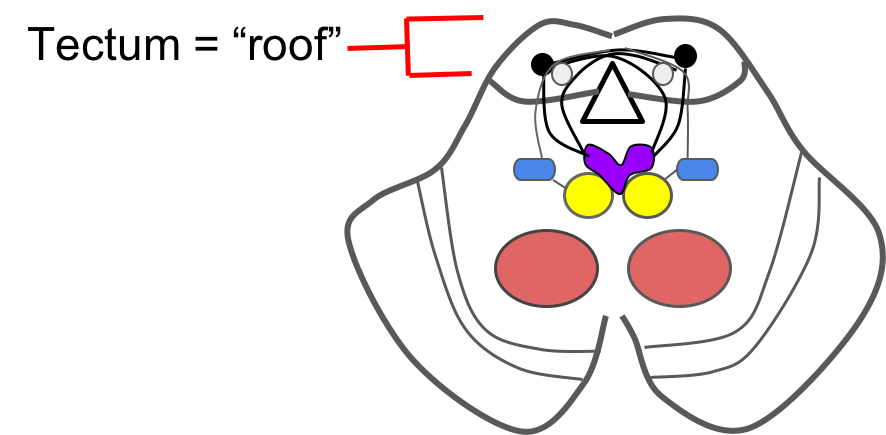
The clinical findings in this patient are a result of involvement of structures in the rostral midbrain and pretectal area near the level of the superior colliculus. These structures include the posterior commissure, nucleus of the posterior commissure, rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF), and the interstitial nucleus of Cajal (INC). They are highlighted on the diagram below.
3. What would be the best way to test for full vertical ocular range of motion in this patient?
- Ask her to make a quick saccade upwards
- Ask her to slowly follow your finger upwards
- Ask her to look down for 30-seconds and then make a quick saccade upwards
- Ask her to focus on his own stationary finger while moving his chin downwards
3. How might you test for full vertical ocular range of motion in this patient? 4. Ask her to focus on his own stationary finger while moving his chin downwards
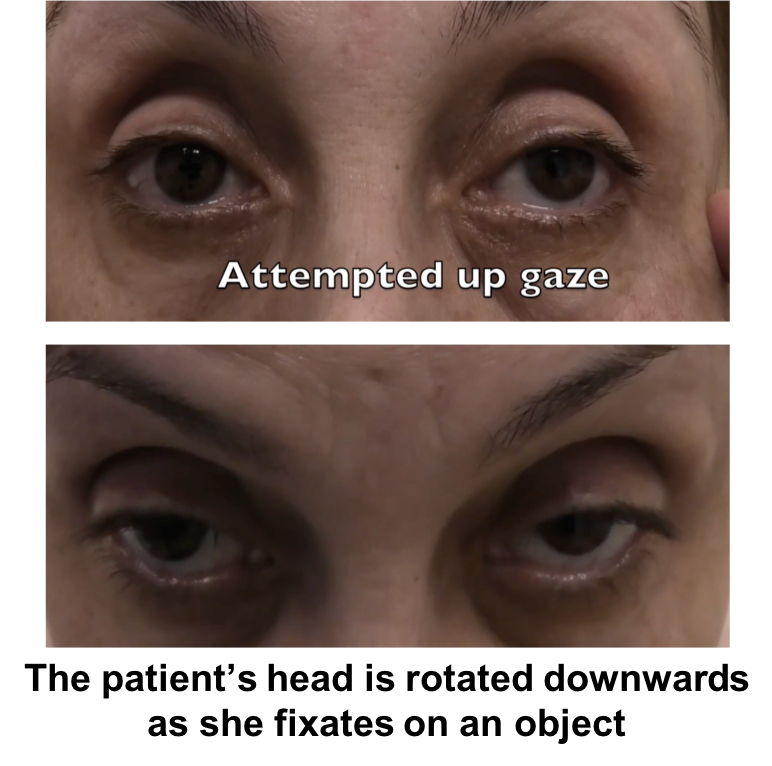
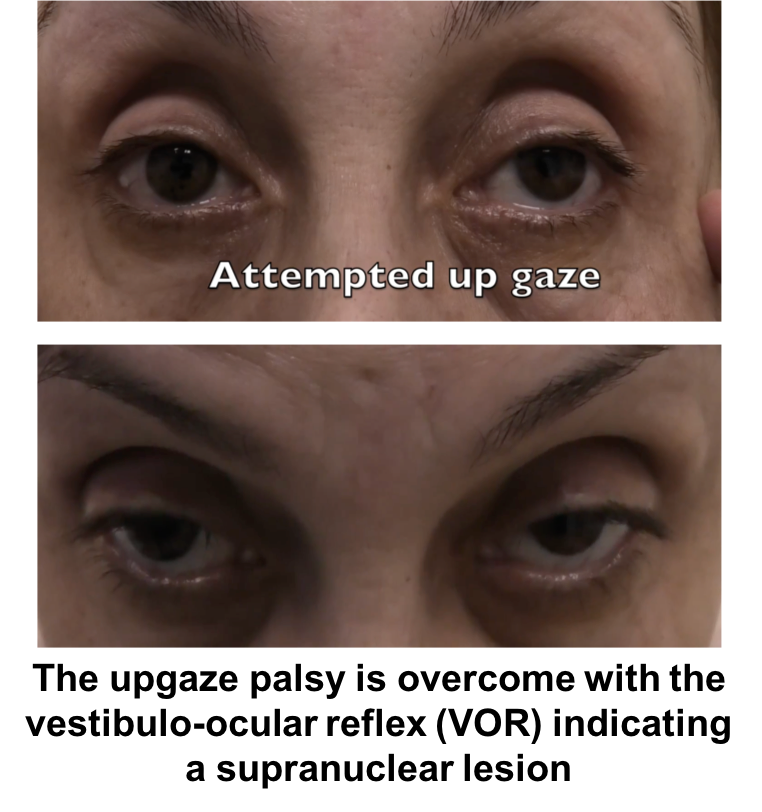
The dorsal midbrain syndrome is characterized by loss of all types of upward eye movements, but relative sparing of the vestibulo-ocular reflex (VOR). The VOR is responsible for maintaining fixation of the eyes during head rotation and is produced by the direct vestibular input to the oculomotor nuclei in the brainstem. It therefore bypasses the supranuclear pathways, which is why it is spared in supranuclear ocular motility disorders such as dorsal midbrain syndrome. This patient has full vertical excursions when she fixates on a target and her head is rotated downwards as shown below.
4. Why is she having vertical binocular diplopia when she looks to the right?
- Childhood strabimus
- Ocular myasthenia gravis
- Left 4th nerve palsy
- Bilateral 3rd nerve palsy
4. Why is she having vertical binocular diplopia when she looks to the right? 3. Left 4th nerve palsy
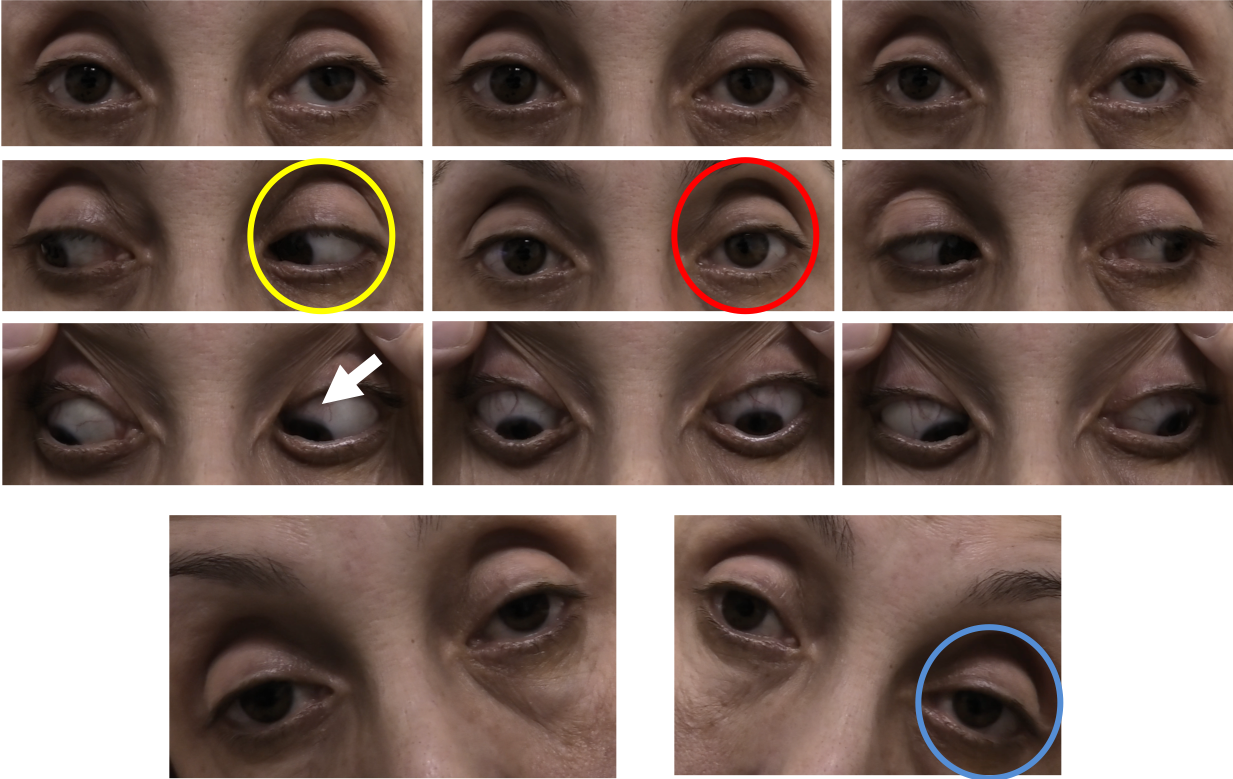
The patient has vertical binocular diplopia when looking to the right and adopts a right head tilt at rest. When examining her eye movements, we observe a left hypertropia (red circle) that is worse in right gaze (yellow arrow) and worse with left head tilt (blue arrow). This left hypertropia follows the Parks-Bielschowsky 3-step test, indicating left superior oblique weakness. She also has a limitation of depression in adduction (white arrow). There were no orbital signs and therefore the most likely diagnosis is a left 4th nerve palsy. The 4th cranial nerve exists from the dorsal midbrain and is likely being affected by the pathology in the dorsal midbrain.
5. What is the next most appropriate investigation for this patient?
- CT scan of the orbits
- MRI of the brain
- CBC, ESR, CRP
- Acetylcholine receptor antibodies
5. What is the next most appropriate investigation for this patient? 2. MRI of the brain
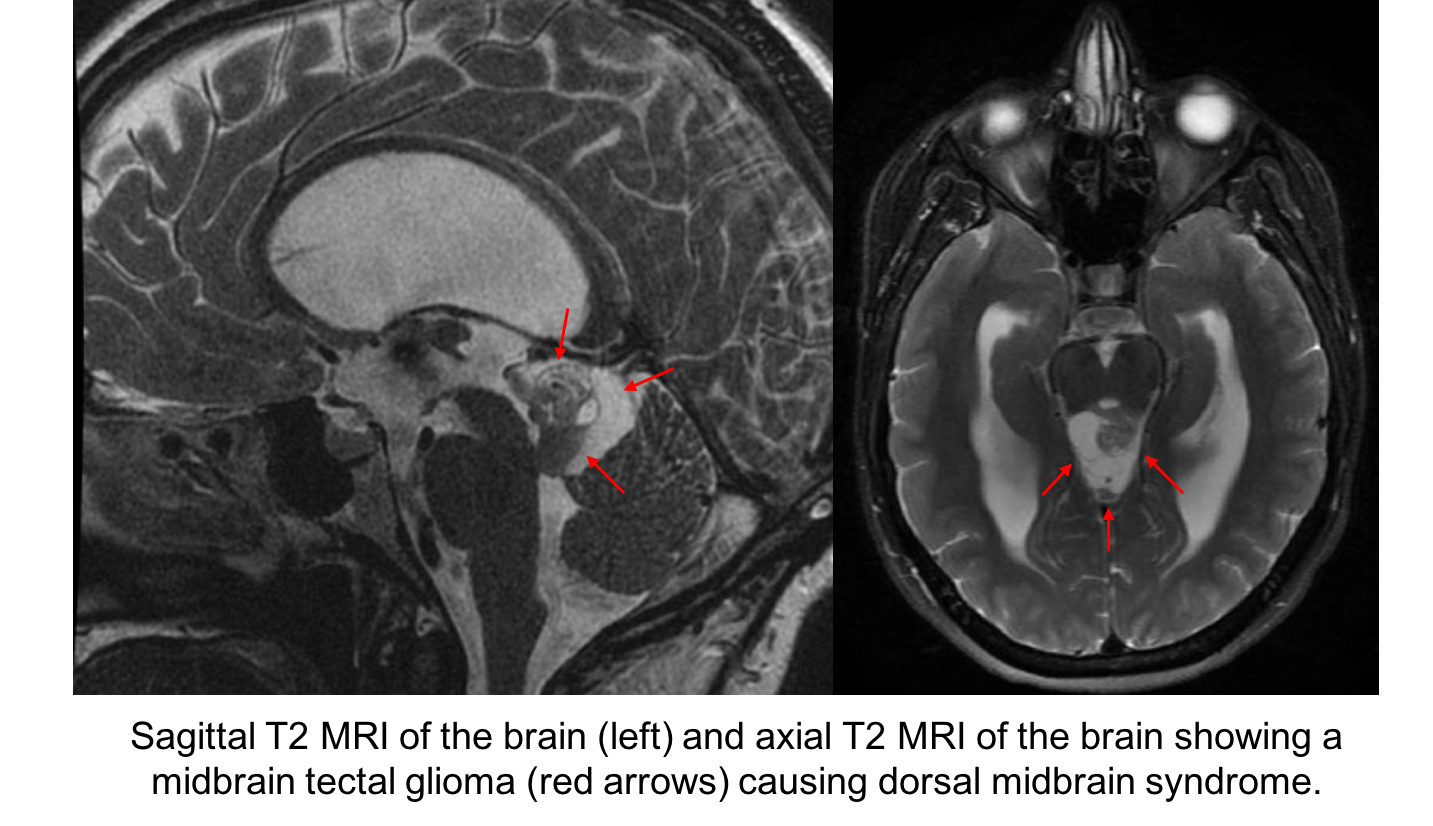
Since this patient is suspected of having dorsal midbrain syndrome, the next most important test is an MRI of the brain to look for a lesion compressing the dorsal midbrain such as pineal tumor or hydrocelphalus. Hydrocephalus may cause aqueductal stenosis leading to dilation of the third ventricle resulting in pressure on the posterior commissure. This patient’s MRI (seen below) showed a partially cystic and solid tectal mass most consistent with a glioma. There was acute hydrocephalus of the lateral and third ventricles leading to elevated intracranial pressure and he underwent ventriculoperitoneal shunt placement.
6. Why do the pupils not react to light in this patient?
- There is severe papilledema in both eyes
- There is damage to the pretectal light fibers entering the Edinger-Westphal nucleus
- The 4th nerve nuclei are affected by the tectal mass
- The pupillary light pathway is affected by the tectal mass in the optic tract
6. Why do the pupils not react to light in this patient? 2. There is damage to the pretectal light fibers entering the Edinger-Westphal nucleus
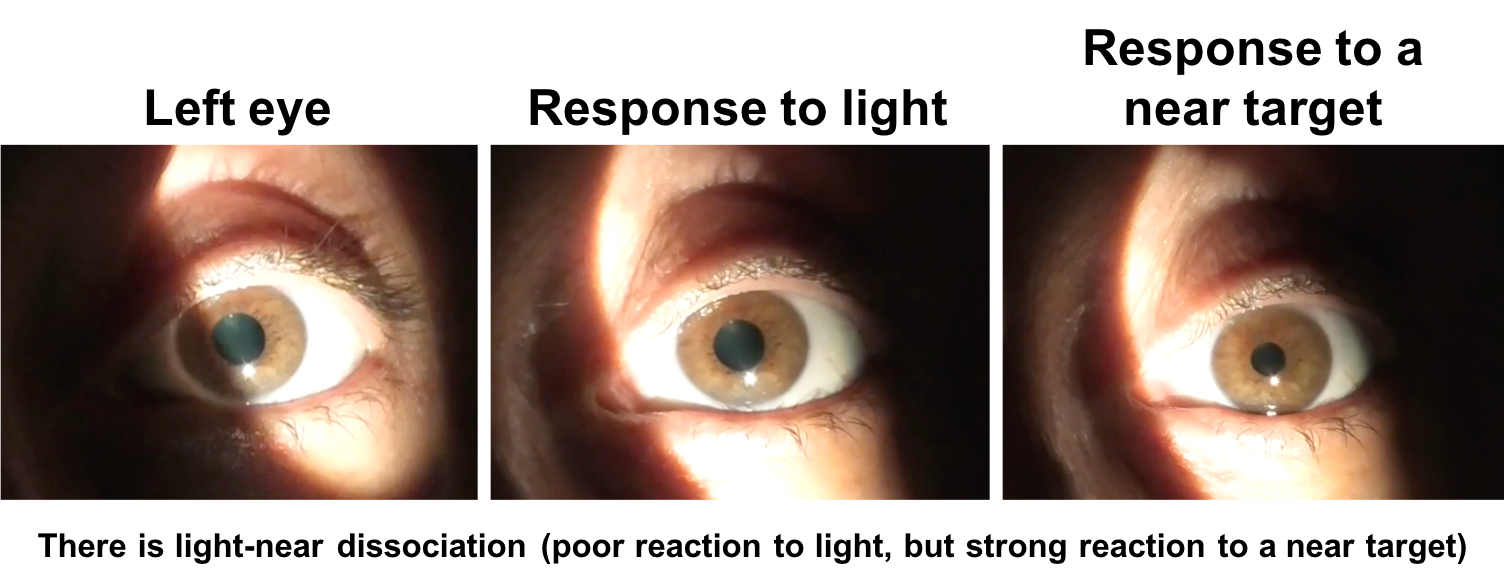
The pupillary light pathway enters the midbrain and ultimately synapse in the Edinger-Westphal nucleus where the pre-ganglionic parasympathetic pupillary fibers originate. The tectal mass in this case is affecting the afferent input of information into the Edinger-Westphal nucleus. Because the fibers for accommodation enter the Edinger-Westphal nucleus more ventrally, they are spared and there is light-near dissociation. Light-near dissociation means that the pupils do not react to light, but constrict in response to a near target.
Clinical Pearl
Tectum is latin for roof. The midbrain tectum is the most dorsal part of the midbrain.
7. Why might a patient with dorsal midbrain syndrome have an esotropia and slowed abducting saccades?
- Involvement of the sixth nerve nucleus
- Involvement of the medial longitudinal fasciculus (MLF)
- Increased convergence tone
- Involvement of the vestibular nuclei
7. Why might a patient with dorsal midbrain syndrome have an esotropia and slowed abducting saccades with normal intracranial pressure? 3. Increased convergence tone
A “pseudo-abducens palsy” may be seen in patients with dorsal midbrain syndrome resulting in an esotropia and abduction deficits. This finding is due to the loss of inhibitory convergence pathways and an increase in convergence tone. Testing ductions in each eye while occluding the other and the oculocephalic reflex may overcome this limitation. This is similar to what is seen in thalamic esoptropia. The 6th nerve nucleus is located in the pons and would not be expected to be involved in a patient with dorsal midbrain syndrome.
8. What is the best way to test for convergence-retraction nystagmus?
- Ask the patient to look down
- Rotate an optokinetic nystagmus (OKN) drum downwards
- Ask the patient to look rapidly in both horizontal directions
- Ask the patient to look rapidly at a near target
8. What is the best way to test for convergence-retraction nystagmus? 2. Rotate an optokinetic nystagmus (OKN) drum downwards
Convergence-retraction nystagmus is a characteristic feature of dorsal midbrain syndrome. It is not a true nystagmus, but rather a saccadic disorder consisting of asynchronous, opposed saccades. If the patient is observed from the side, the eyes will retract with attempted upgaze and this can also be tested with a downward rotating OKN drum. As the drum is rotated downwards, the slow phase of the OKN response involves following the target downwards and then a quick upward corrective saccade. This upward saccade is useful in bringing out the convergence-retraction nystagmus. Convergence-retraction nystagmus results from damage to the posterior commissure and can be produced by experimentally ablating this area.
9. What is Collier’s sign?
- Downward positioning of the eyes
- Bilateral ptosis
- Eyelid retraction
- Light-near dissociation
9. What is Collier’s sign? 3. Eyelid retraction
Abnormalities of the eyelids are common in patients with dorsal midbrain syndrome and include eyelid retraction (Collier’s sign), lid lag and occasionally ptosis. Lid retraction may be due to involvement of the nucleus of the posterior commissure, which provides a tonic inhibitory signal to the cranial caudal nucleus that controls the levator palpebrae superioris muscle.
Clinical Pearl
The signs of dorsal midbrain syndrome include:
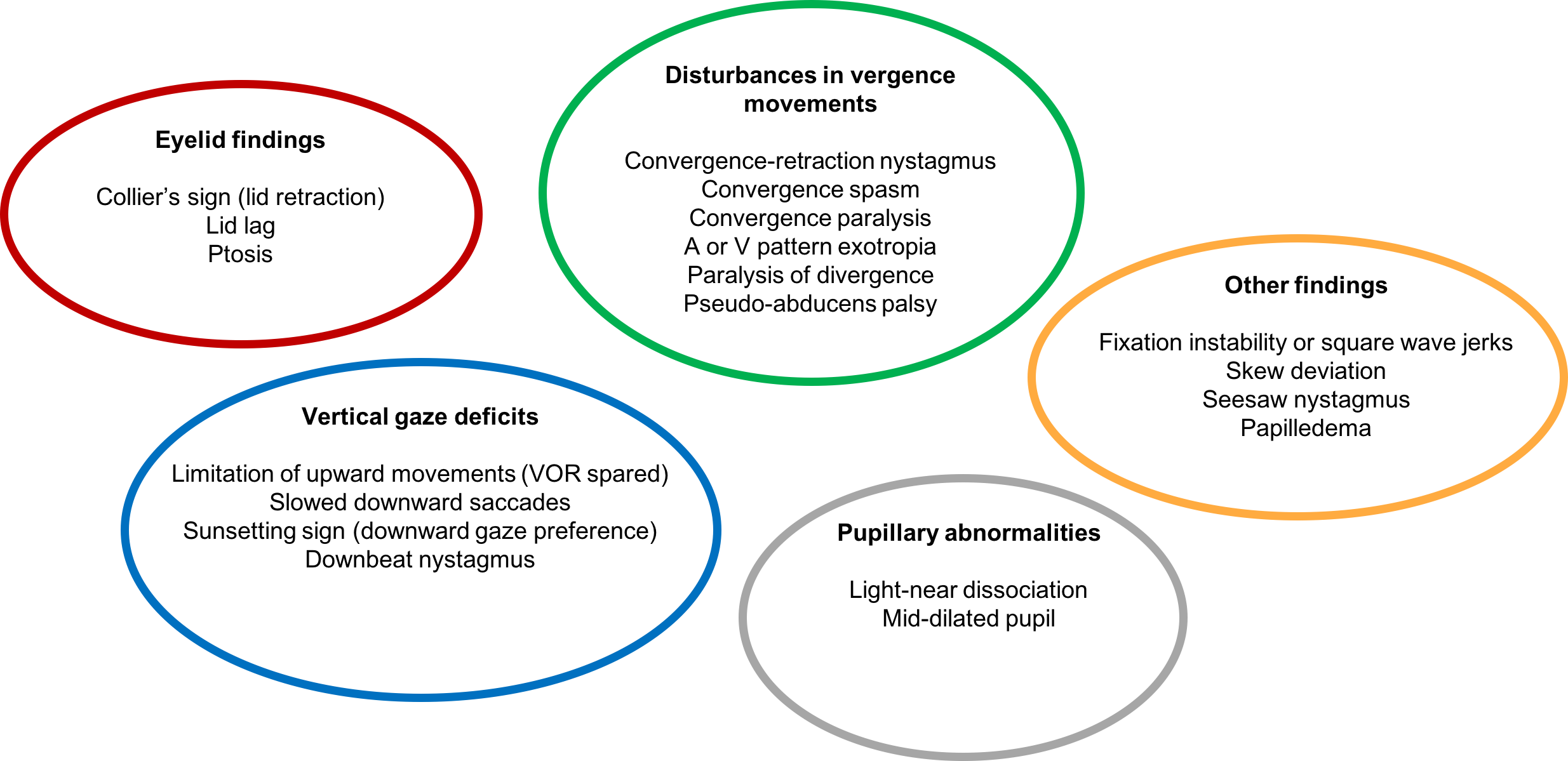
10. A 70-year old woman has frequent falls backwards, difficulty swallowing and memory problems. She complains of difficulty reading. Her husband comments that she seems depressed for the past year.What might be seen on her ophthalmic examination?
- Impairment of vertical saccades
- Square-wave jerks
- Convergence insufficiency
- All of the above
10. A 70-year old woman has frequent falls backwards, difficulty swallowing and memory problems. She complains of difficulty reading.Her husband comments that she seems depressed for the past year. What might be seen on her ophthalmic examination? 4. All of the above
This patient has symptoms concerning for progressive supranuclear palsy (PSP), which is a neuro-degenerative disorder with parkinsonian features characterized by vertical supranuclear gaze palsy, postural instability, unexplained falls, cognitive dysfunction, depression, mood swings and akinesia. Ocular manifestations of PSP including eyelid findings such as blepharospasm, apraxia of eyelid closing or opening, lid lag and lid retraction. There is impairment of vertical saccades (downward more than upward) that can be overcome with the vestibulo-ocular reflex. Smooth pursuit is usually relatively preserved. Impairment of downward saccades causes difficulty with reading and patients are helped by using a separate set of reading glasses and not bifocals and multifocal lenses, which require them to look through a small area for near viewing. Patients also have square-wave jerks, which are saccadic intrusions characterized by an involuntary saccade away from fixation followed by a brief interval and saccadic return to fixation position. They are best observed at the slit lamp.
11. What finding would be expected with bilateral lesions to the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF)?
- Loss of vertical saccades
- Complete horizontal gaze palsy
- 3rd nerve palsy
- Bilateral ptosis
11. What finding would be expected with bilateral lesions to the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF)? 1. Loss of vertical saccades
The riMLF contains excitatory burst neurons that send signals to the oculomotor and trochlear nerve nuclei, which generate a saccadic pulse to move the eyes rapidly to a new position. The interstitial nucleus of Cajal (INC) then generates a saccadic step to hold the eyes in their new position. Bilateral lesions of the riMLF can be seen with small infarctions involving the arteries of Percheron at the top of the basilar artery since one medial artery often vascularizes both riMLFs. Patients that have bilateral riMLF lesions will have a loss of vertical saccades with downward saccades being affected more than upward saccades. A unilateral riMLF lesion will affect downward saccades more than upward saccades since there is duplication of the input to the nuclei responsible for up gaze.
12. A patient has a large acute intracerebral hemorrhage affecting the right frontal eye field. Which way do you expect the eyes to be deviated?
- Deviated to the right
- Deviated to the left
- Deviated upwards
- Deviated downwards
12. A patient has a large acute intracerebral hemorrhage affecting the right frontal eye field. Which way do you expect the eyes to be deviated? 1. Deviated to the right
The frontal eye fields are involved in the generation of volitional saccades. Activation of the frontal eye fields produces conjugate, contralateral saccades by sending signals to many structures including the contralateral paramedian pontine reticular formation (PPRF). Therefore, in the acute stage after a hemorrhage affecting the frontal eye fields, patients will look towards the side of the lesion. This is usually temporary and improves within 72 hours. This is in contrast to pontine lesions and cortical seizures, which cause the eyes to deviate away from the side of the lesion.
Case Summary
She had the new onset of difficulty with upward eye movements and binocular vertical diplopia when looking to the right. Examination revealed a baseline head up and right head tilt position, loss of upward saccades, preservation of downward saccades, and full ocular excursions with the vestibulo-ocular reflex. There was also a left hypertropia, worse with right gaze and left head tilt and bilateral disc edema with preserved visual function from papilledema. Due to concern for compression of the dorsal midbrain, an MRI of the brain was arranged and showed a tectal mass with cystic and solid components most consistent with a tectal glioma. She underwent a procedure to insert a VP shunt due to acute hydrocephalus that developed and she recovered well, suggesting that her symptoms of dorsal midbrain syndrome were related to hydrocephalus secondary to the tectal mass. She recovered most of her upward eye movements and her papilledema resolved. A radiation oncology consultation was obtained, but he was monitored with regular MRIs and no treatment was recommended. The mass remained stable on the MRI.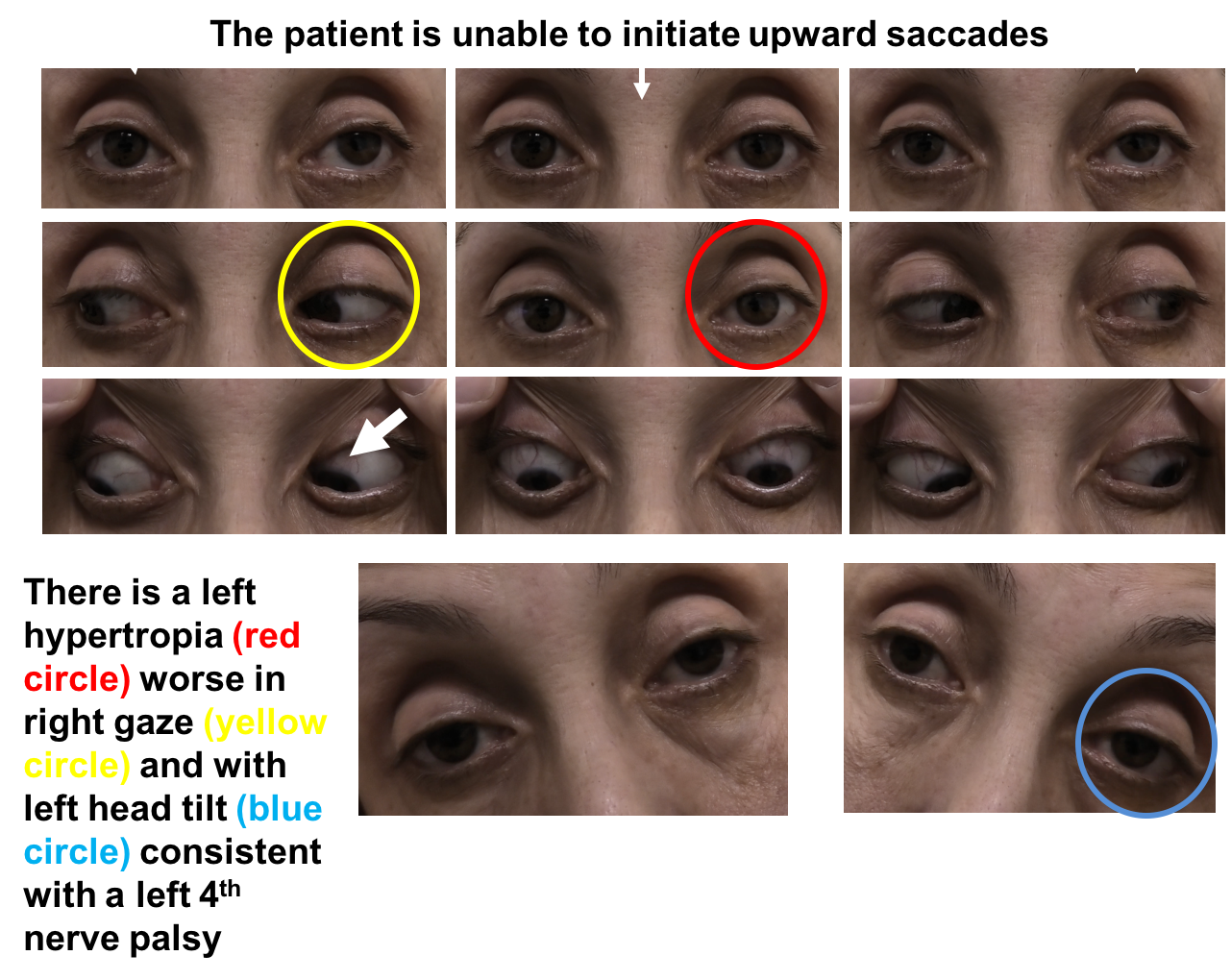
Further reading:
-
Shields M, Sinkar S, Chan W, Crompton J. Parinaud syndrome: a 25-year (1991-2016) review of 40 consecutive adult cases. Acta Ophthalmol 2017;95(8):e792-793. https://www.ncbi.nlm.nih.gov/pubmed/27778456
-
Eggenberger E. Supranuclear eye movement abnormalities. Continuum (Minneap Minn) 2014;20(4 Neuro-ophthalmology):981-92. https://www.ncbi.nlm.nih.gov/pubmed/25099104