2
1. Which of the following is true regarding the principles of optical coherence tomography (OCT)?
- The time delay and magnitude change of backscattered light from the retina are used to create cross-sectional images of the retina
- It uses low-dose ionizing radiation (radio waves) to penetrate through the lens of the eye and map the contour of the retina
- It is similar to ultrasound in that sound waves are used except a higher frequency setting allows deeper penetration into the orbit
- It uses visible light to penetrate the retina and a sensor positioned behind the patient’s head detects the prismatic effect of the light
1. Which of the following is true regarding the principles of optical coherence tomography (OCT)? 1. The time delay and magnitude change of backscattered light from the retina are used to create cross-sectional images of the retina
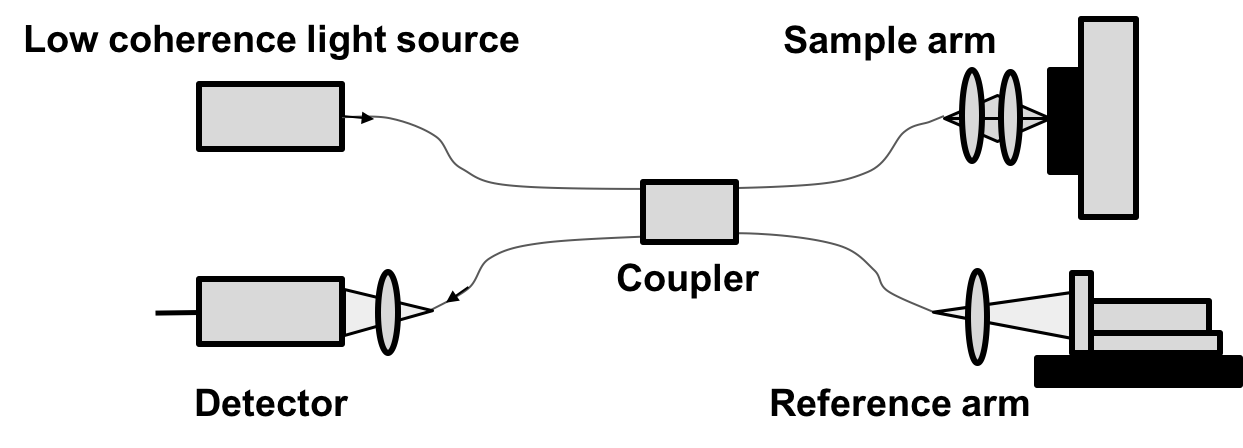
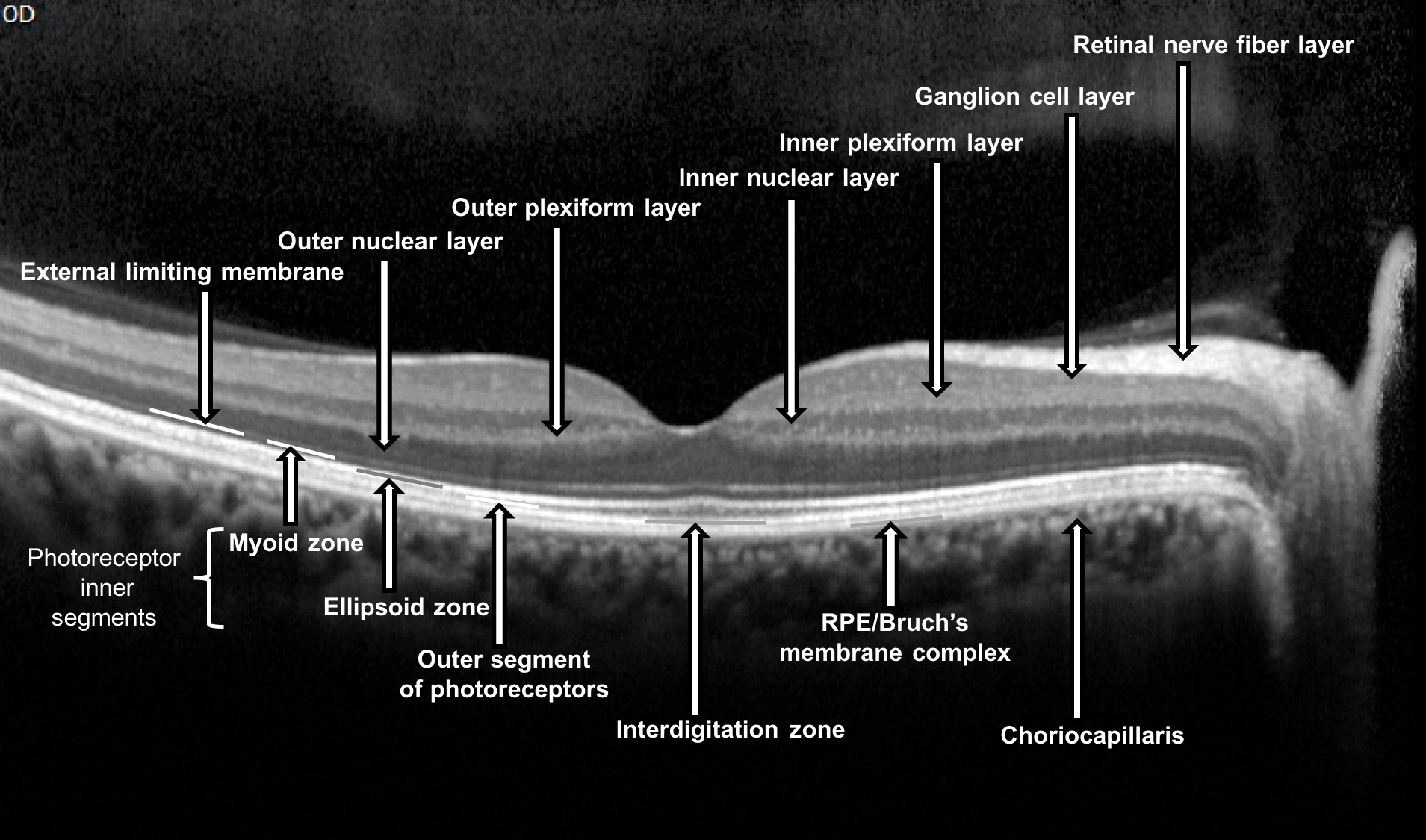
Optical coherence tomography is a non-invasive, noncontact imaging tool that allows for histology-like cross-sectional images of the human retina to be obtained. It makes use of visible light and measures the amount of optical reflectivity from a tissue. Light from a low-coherence light source is split by a coupler into two paths, a sample and reference arm. In the reference arm, the light is reflected back by a reference mirror and returns into the interference system in the opposite direction that it came from. In the sample arm, the same process occurs except the beam is backscattered by the sample when materials of different indices of refraction are encountered. The returning light from both arms are combined by the coupler and generate an interference pattern, which arrives at the detector and is recorded.
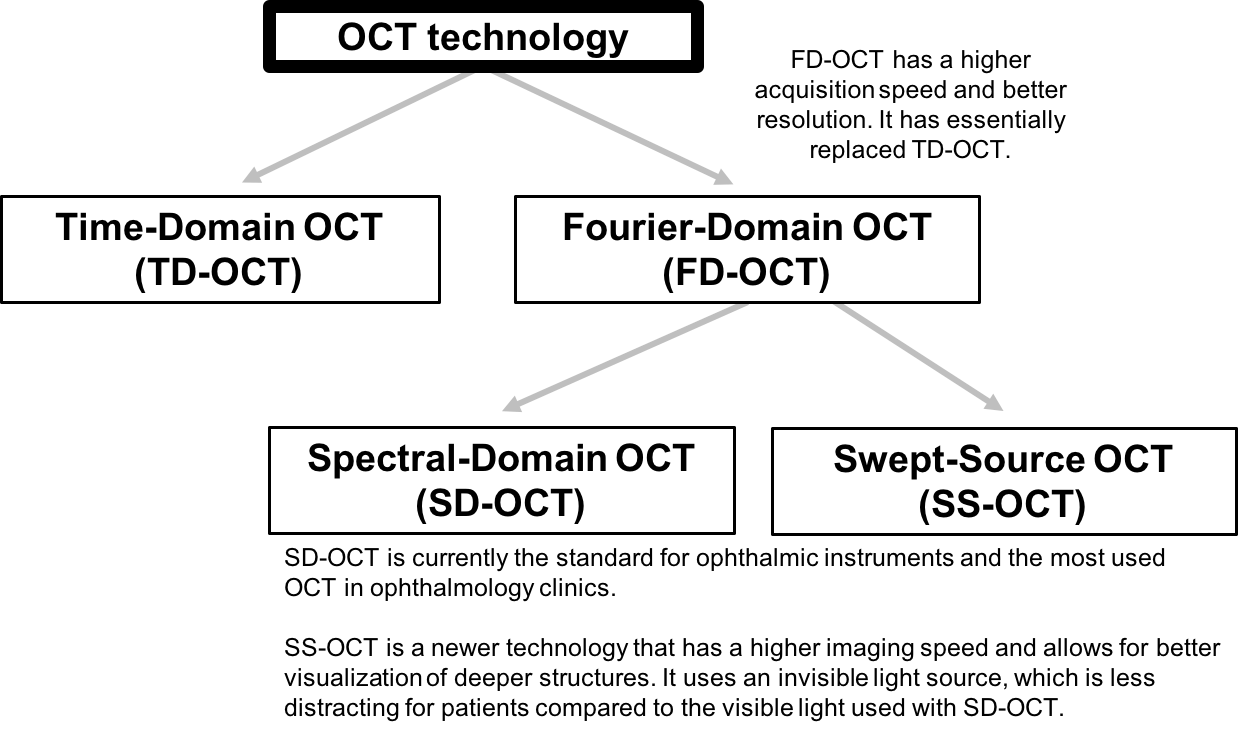
OCT technology
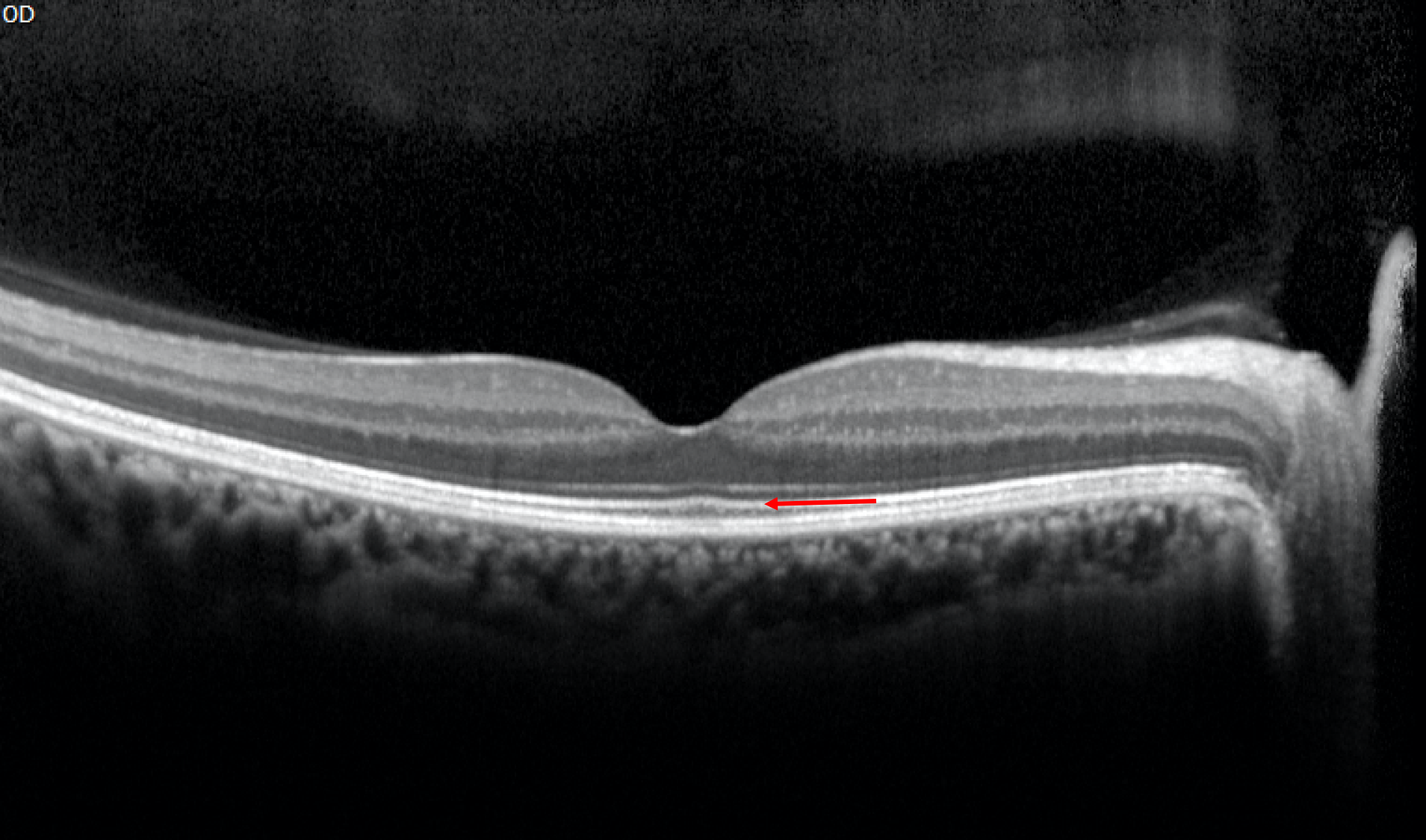
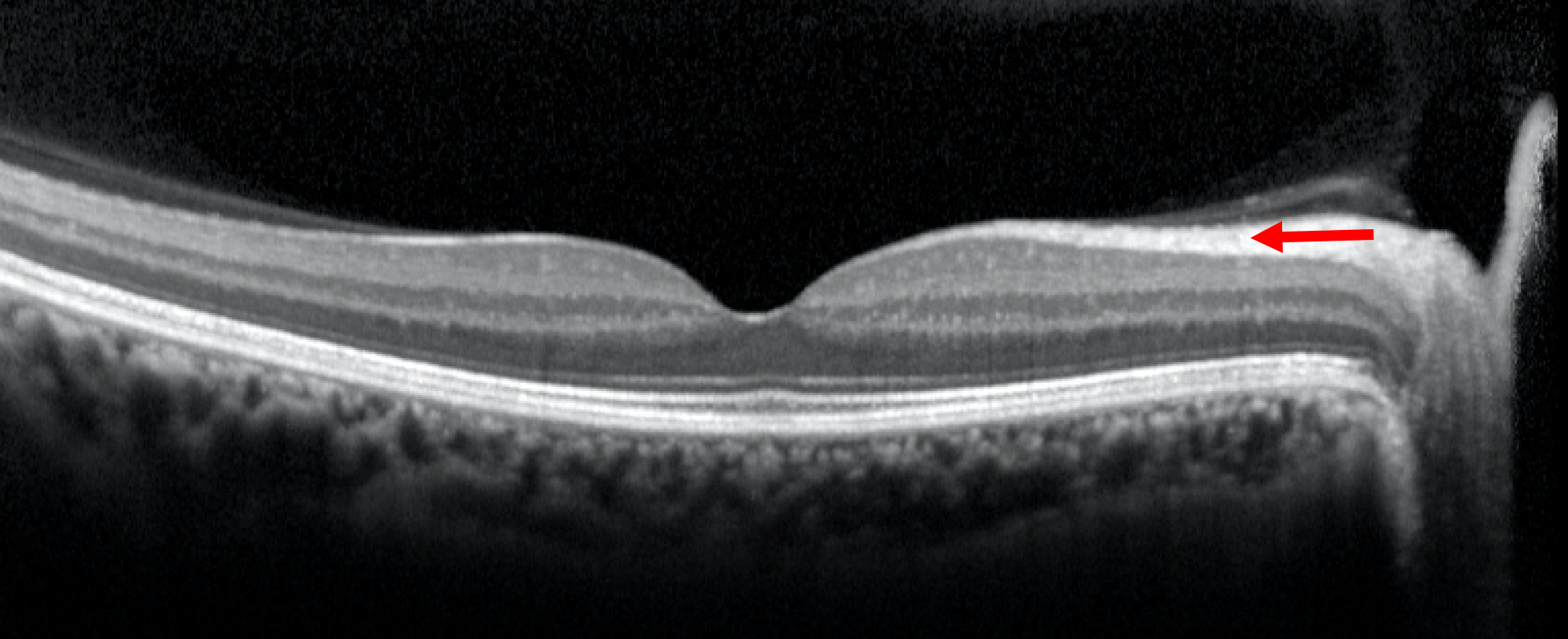
2. An OCT of the macula is shown below. What layer of the retina is indicated by the red arrow?
- Inner plexiform layer
- Inner nuclear layer
- Outer plexiform layer
- Outer nuclear layer
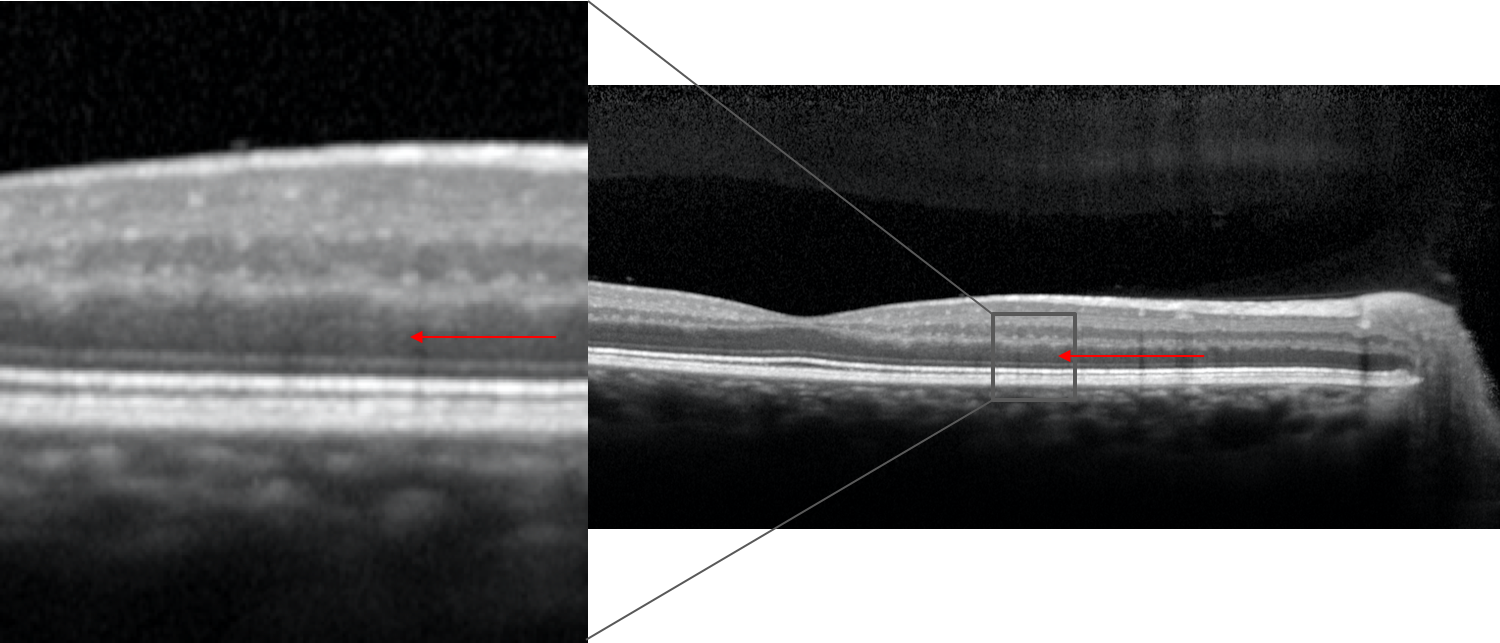
2. An OCT of the macula is shown below. What layer of the retina is indicated by the red arrow? 4. Outer nuclear layer
The different layers of the retina visualized with OCT are summarized below. The nuclear layers appear as darker bands compared to the plexiform, ganglion cell and retinal nerve fiber layers. The outer nuclear layer contains the cell bodies of the rod and cone photoreceptors whereas the inner nuclear layer consists of the cell bodies of horizontal cells, bipolar cells, amacrine cells, interplexiform neurons, and Müller cells.
Layers of the retina visualized with OCT
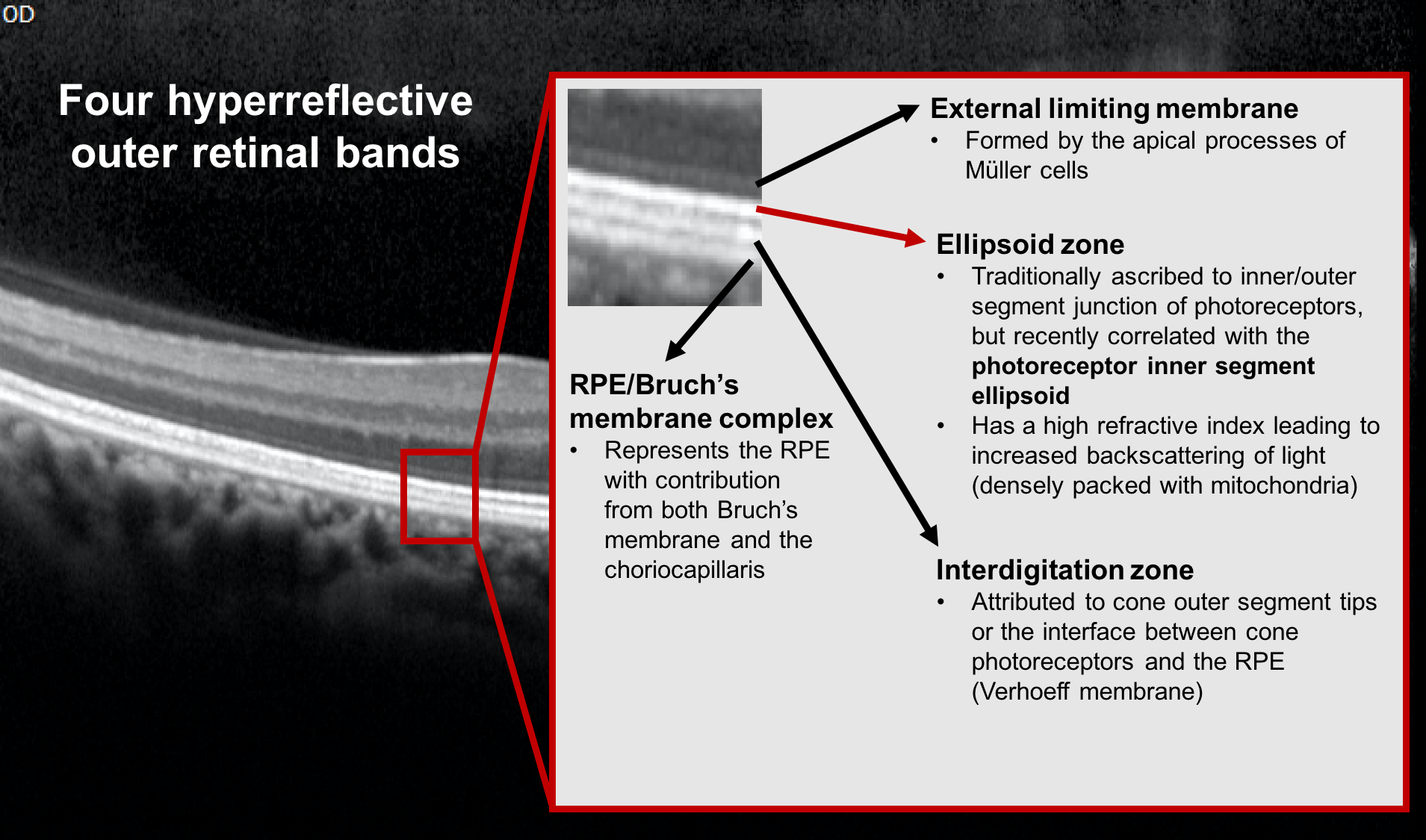
3. An OCT of the macula of a right eye is shown. The second hyperreflective band is indicated by a red arrow. What is this layer called?
- Retinal pigment epithelium/Bruch’s membrane complex
- Photoreceptor outer segments
- Ellipsoid zone
- External limiting membrane
3. An OCT of the macula of a right eye is shown. The second hyperreflective band is indicated by a red arrow. What is this layer called? 3. Ellipsoid zone
The ability to perform higher-resolution SD-OCT has allowed for better delineation of the outer retinal layers. Four hyper-reflective bands can be identified in the human retina and are summarized below. The second hyperreflective outer band corresponds to the ellipsoid zone and its integrity correlates with visual outcomes in a number of retinal conditions.
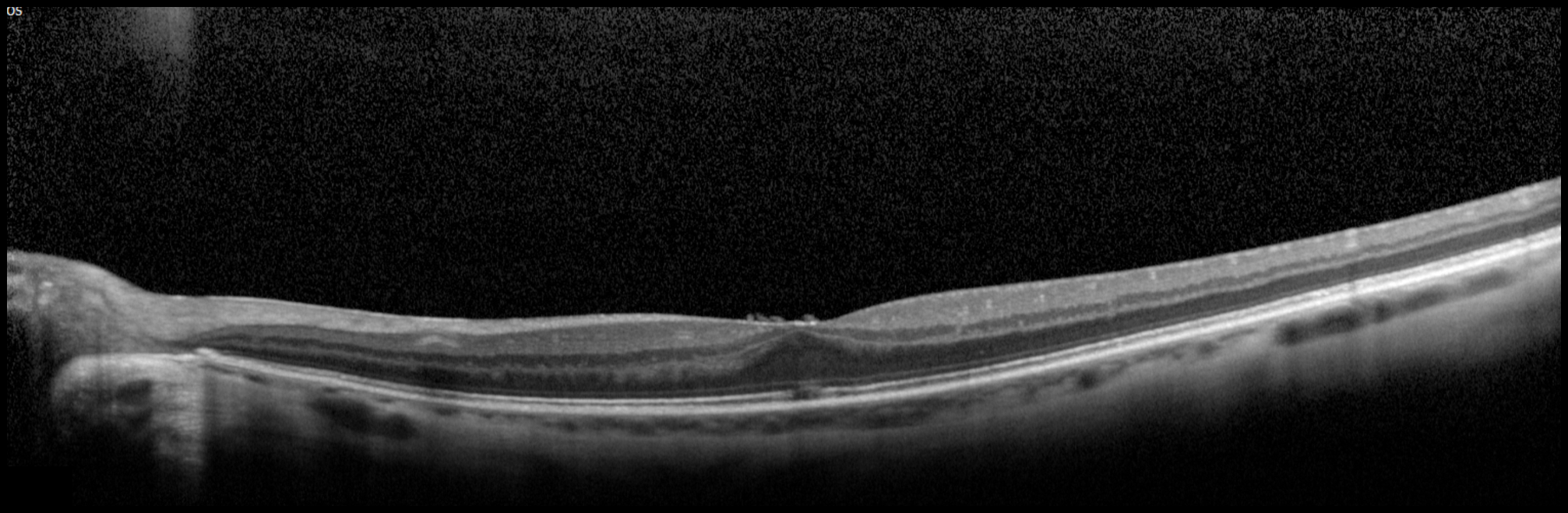
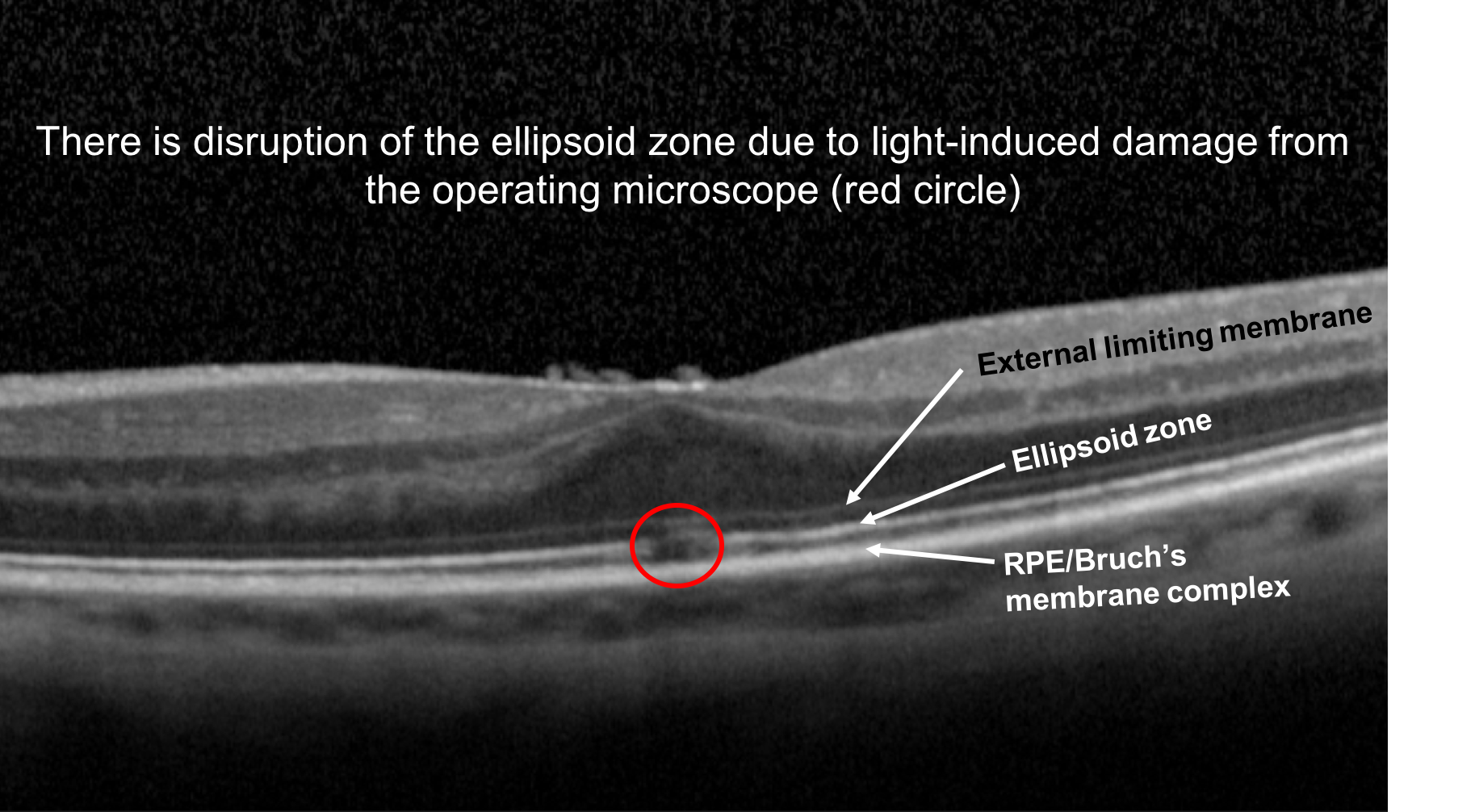
4. A patient notices a central scotoma in her left eye after she had intraocular surgery. What change in her OCT of the macula shown below explains her symptom?
- Loss of the retinal pigment epithelium (RPE)/Bruch’s membrane complex
- Focal disruption of the ellipsoid zone
- Disruption of the external limiting membrane
- Increased space between the RPE and choriocapillaris
4. A patient notices a central scotoma in her left eye after she had intraocular surgery. What change in her OCT of the macula shown below explains her symptom? 2. Focal disruption of the ellipsoid zone
This patient developed a central scotoma from photic maculopathy, which was a result of light exposure from the operating microscope during her surgery. This can be detected as a focal foveal disruption of the ellipsoid zone, representing damage to the photoreceptors in this area.
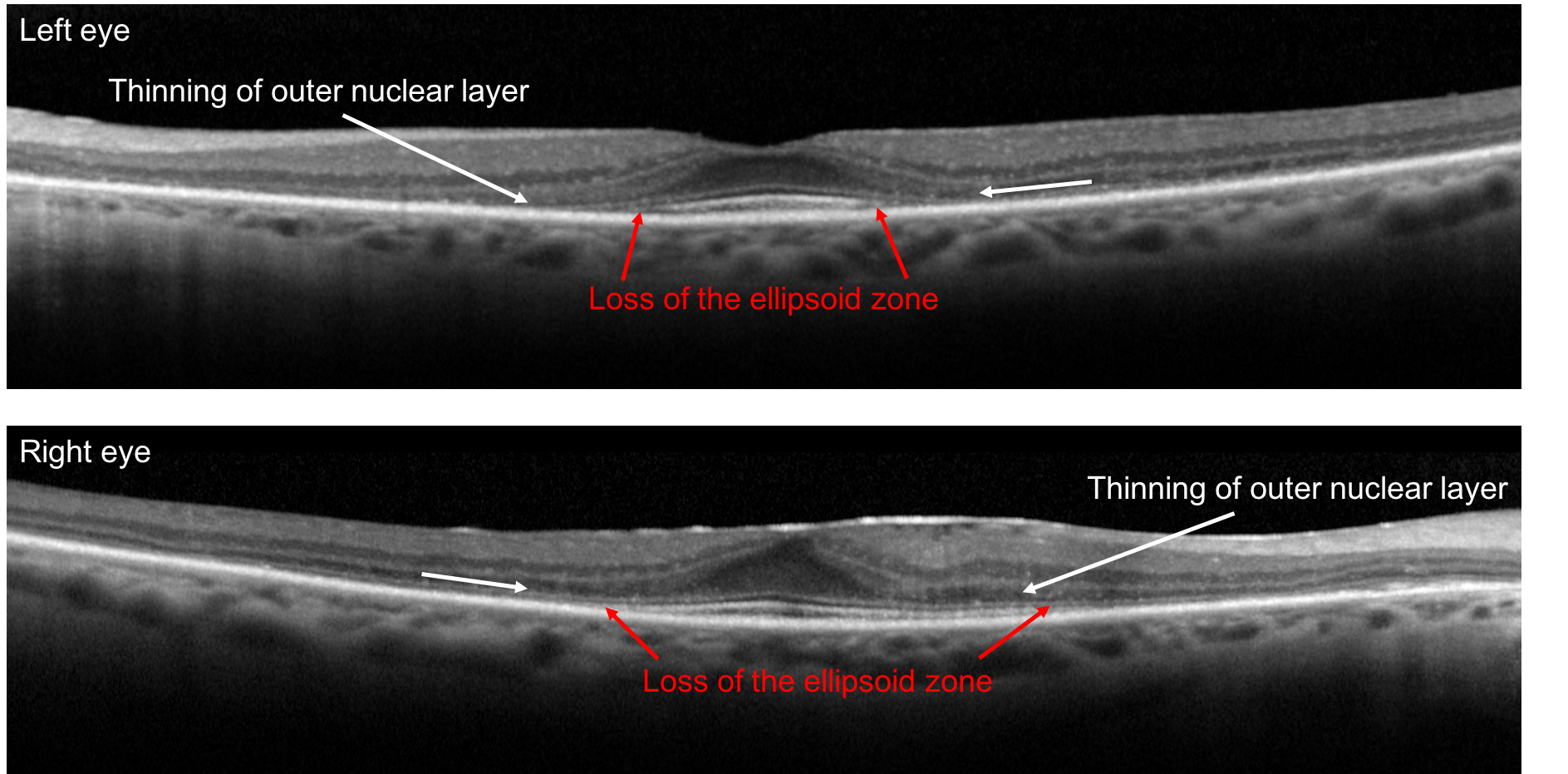
5. A 75-year-old woman presents with slowly developing bilateral central visual field defects. OCT of the macula from both her eyes are shown below. Which of the following medications is she most likely taking?
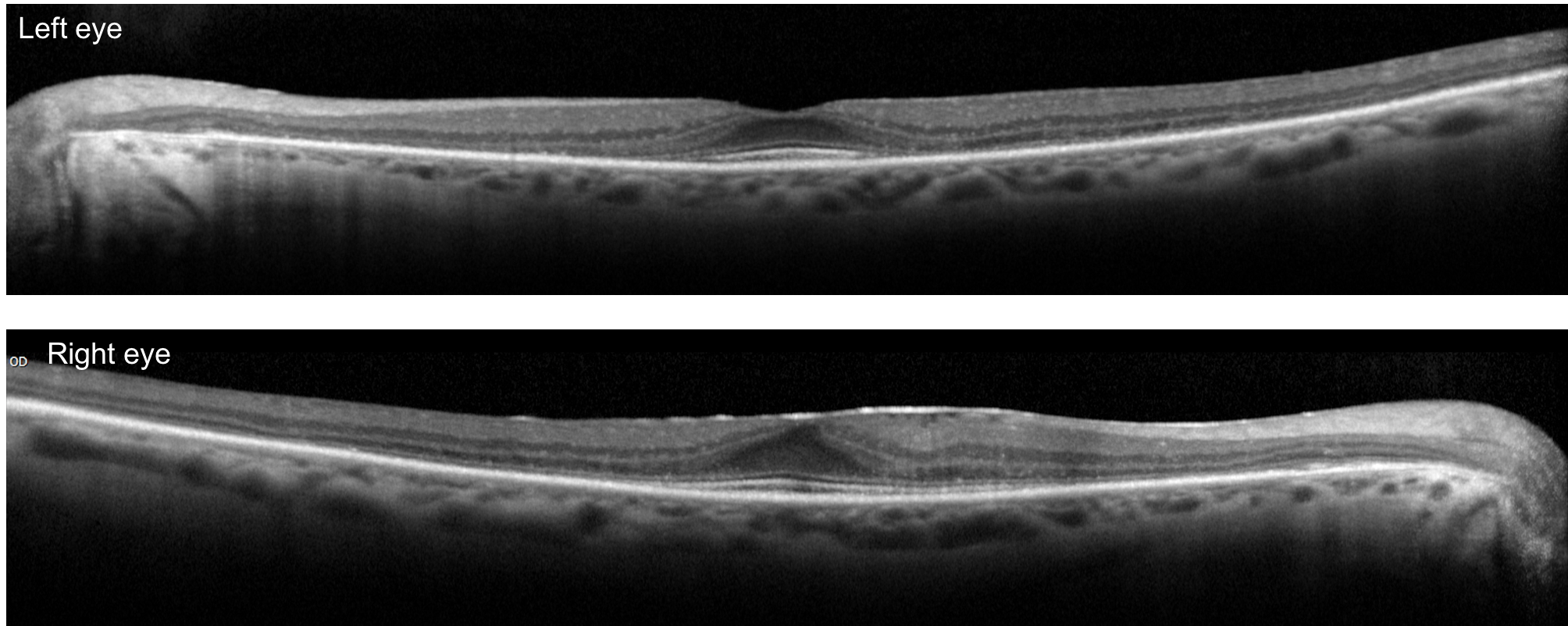
- Amiodarone
- Hydroxychloroquine
- Cialis
- Aspirin
5. A 75-year-old woman presents with slowly developing bilateral central visual field defects. OCT of the macula from both her eyes are shown below. Which of the following medications is she most likely taking? 2. Hydroxychloroquine
This patient’s visual field defects are a result of hydroxychlorquine toxicity, a medication she had been taking for over 15 years for rheumatoid arthritis. Patients on this medication should be regularly screened on an annual basis for ocular toxicity after 5 years of taking the drug since retinal toxicity is irreversible. Acceptable screening methods include spectral-domain OCT, fundus autofluorescence, and multifocal ERG. The mechanism of toxicity is not well understood, but the primary damage appears to occur to the photoreceptors and as the outer nuclear layer degenerates, there is secondary disruption of the retinal pigment epithelium.
6. A patient developed sudden, painless vision loss in his left eye two days ago. What is the cause of his vision loss?
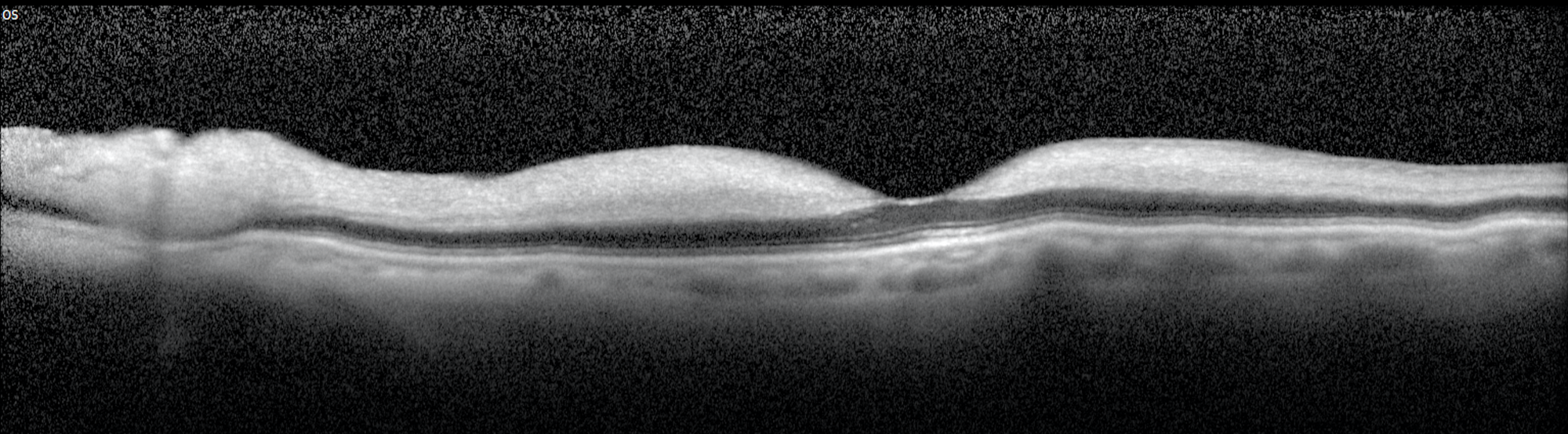
- Ischemic optic neuropathy
- Branch retinal artery occlusion
- Central retinal artery occlusion
- Vitreous hemorrhage
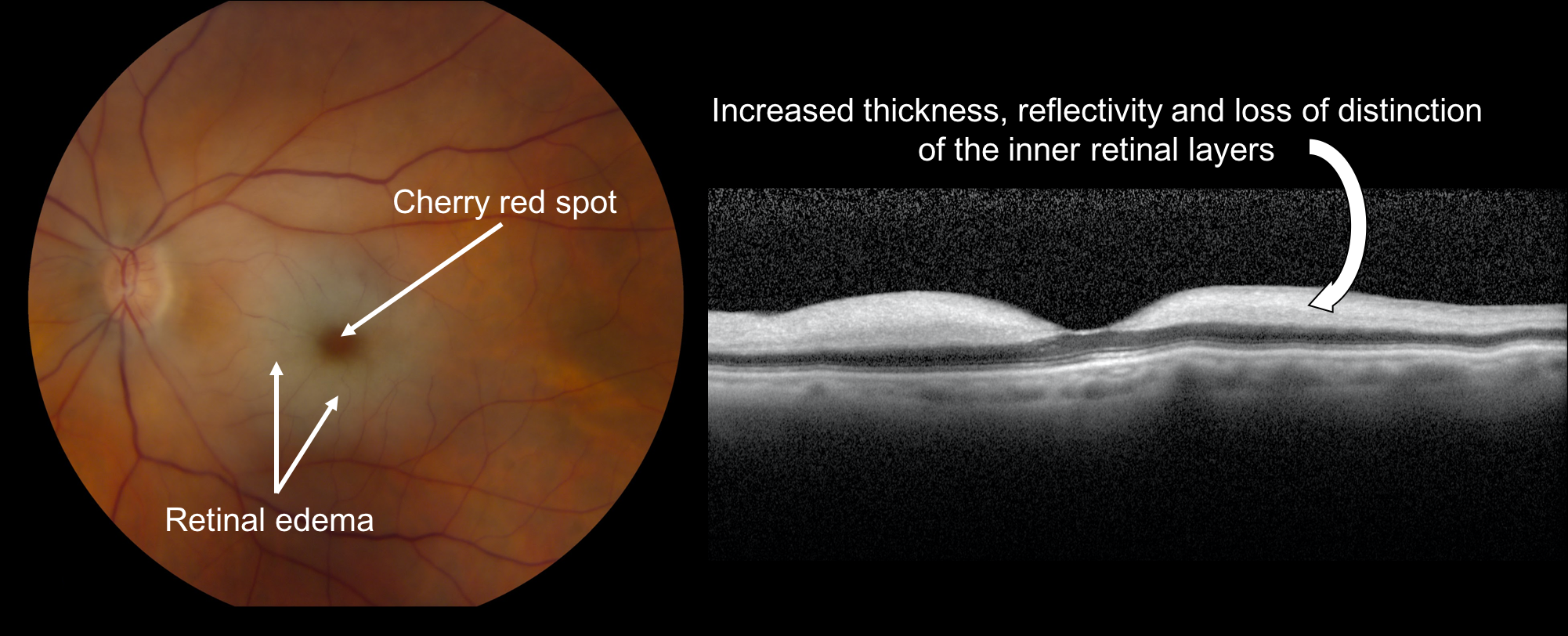
6. A patient has sudden painless, vision loss in his left eye. What is the cause of the vision loss? 3. Central retinal artery occlusion
In the acute phase of a central retinal artery occlusion, there is increased reflectivity and thickness of the inner retinal layers due to the edema that results from the inner retinal ischemia. There is a corresponding decrease in the reflectivity of the outer retina and choriocapillaris since less light is reflected back from these layers. After the edema resolves, there is a decrease in the inner retinal thickness and disorganization and atrophy of the inner retinal layers.
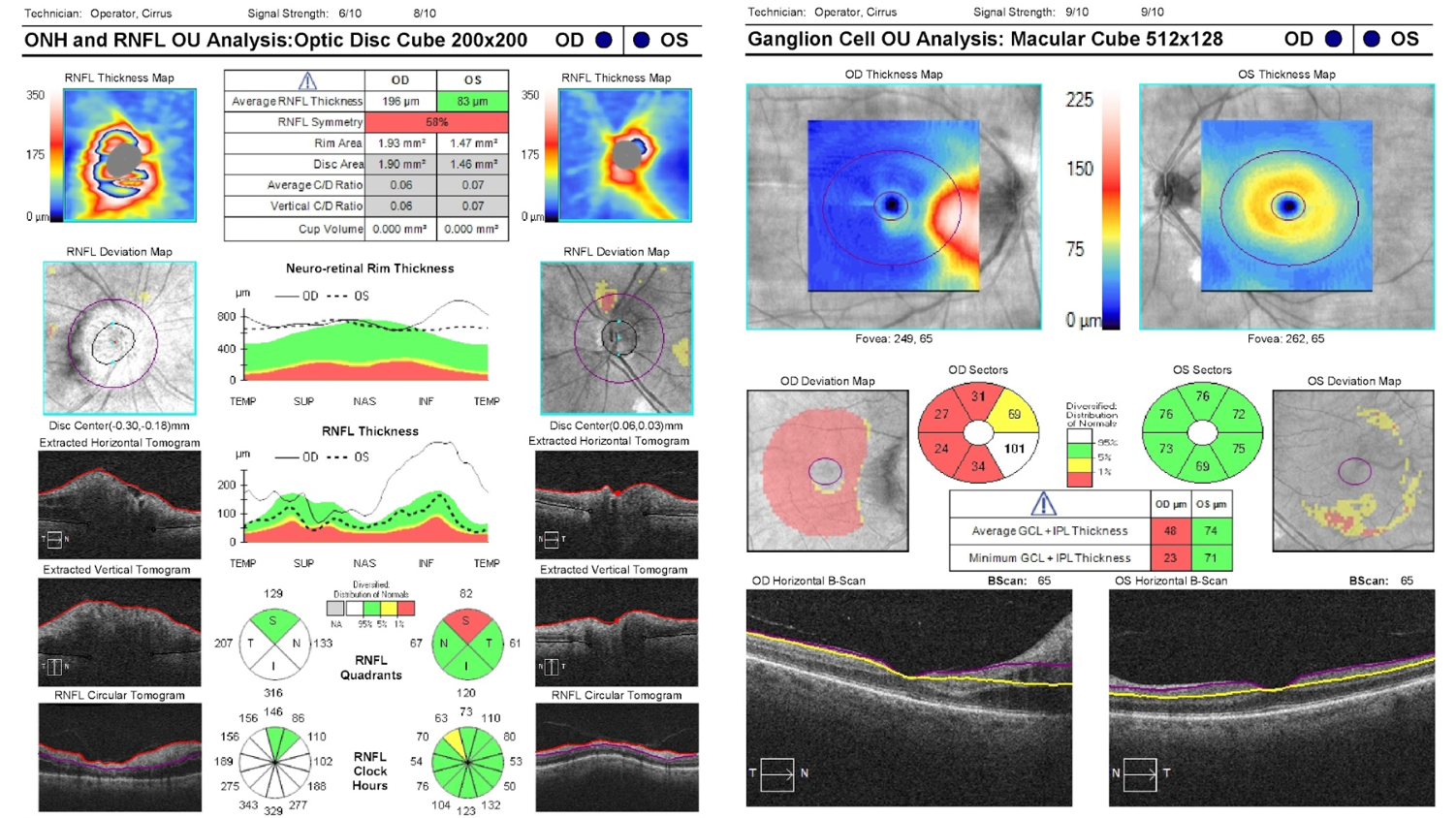
7. A patient experienced vision loss in the superior part of the visual field of his right eye several years ago. Which of the following macular OCTs obtained at this time is most consistent with a branch retinal artery occlusion (BRAO) as the cause of his vision loss?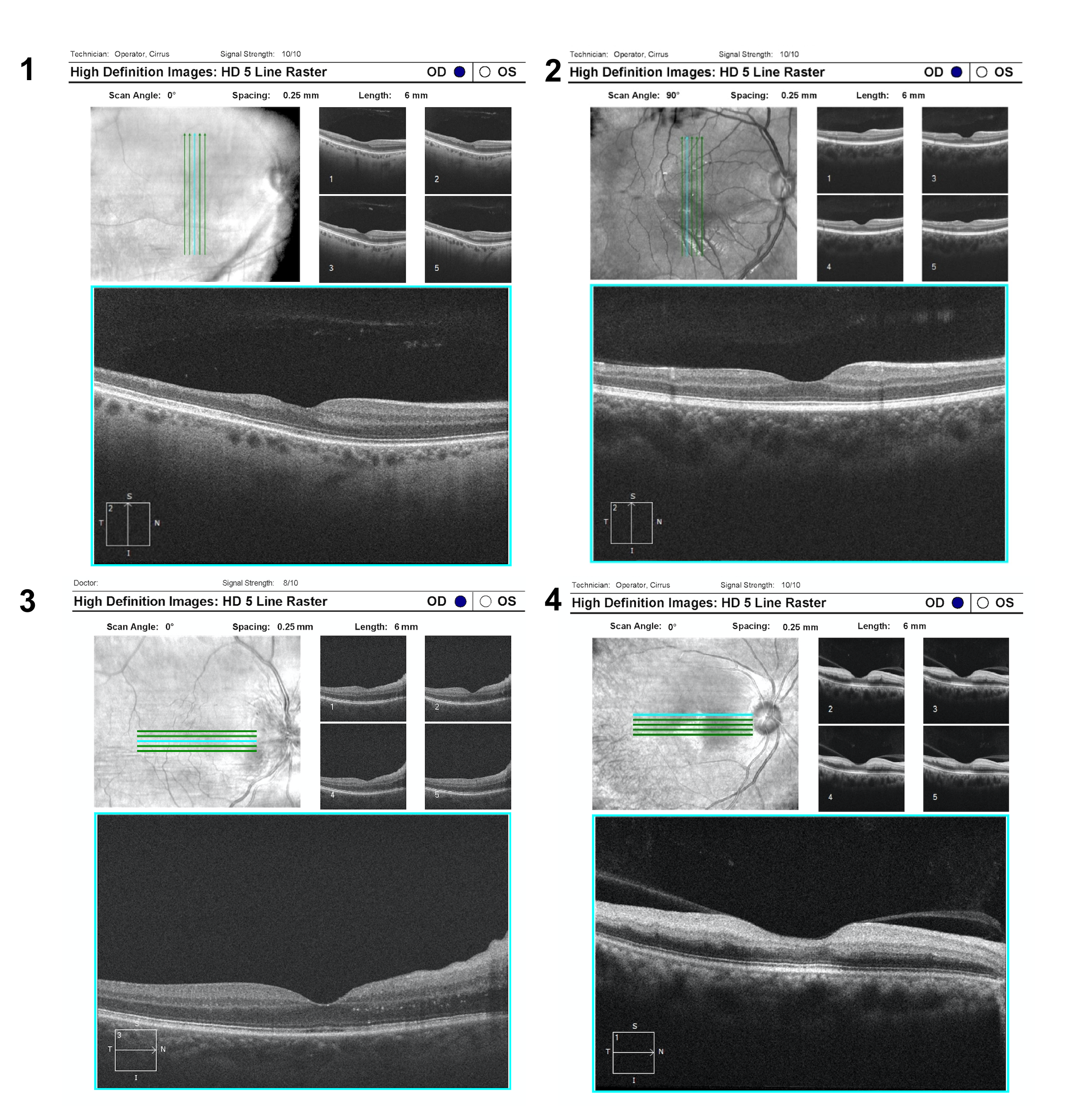
7. A patient experienced vision loss in the superior part of the visual field of his right eye several years ago. Which of the following macular OCTs is most consistent with a branch retinal artery occlusion (BRAO) as the cause of his vision loss? 1
In a patient with an altitudinal visual field defect, OCT can help differentiate a retinal artery occlusion from other optic neuropathies even years after vision loss. Branch retinal artery occlusions demonstrate significant inner retinal atrophy with loss of the normal stratification of the inner retinal layers whereas optic neuropathies such as glaucoma or non-arteritic anterior ischemic optic neuropathy demonstrate thinning of only the ganglion cell and retinal nerve fiber layers. Vertically orienting the OCT scans can help in comparing healthy and atrophic retina in patients with altitudinal visual field defects since the retinal nerve fiber layer respects the horizontal meridian.
8. In what layer of the retina are the cell bodies of the retinal ganglion cells located?
- Retinal nerve fiber layer
- Ganglion cell layer
- Inner plexiform layer
- Inner nuclear layer
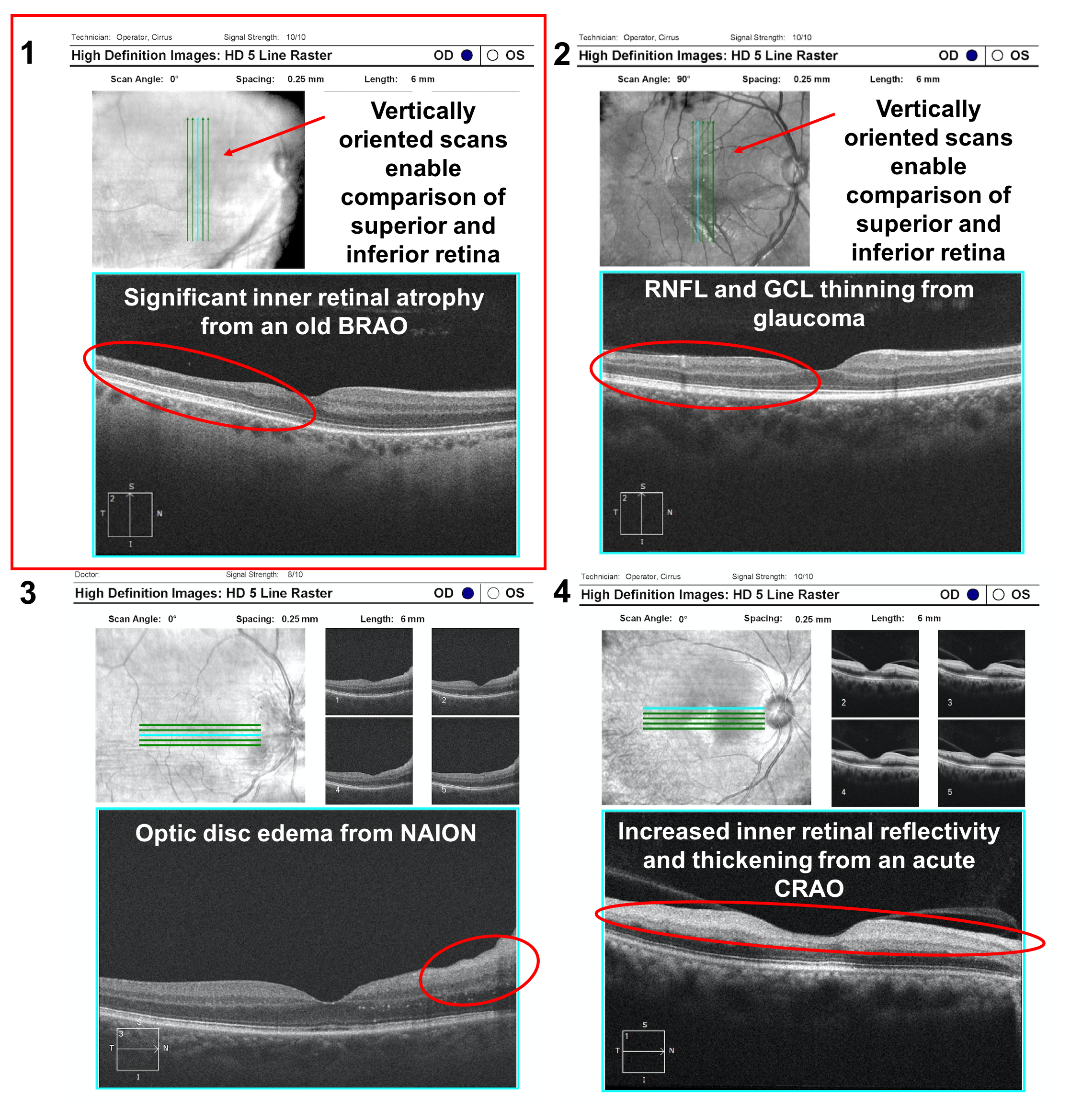
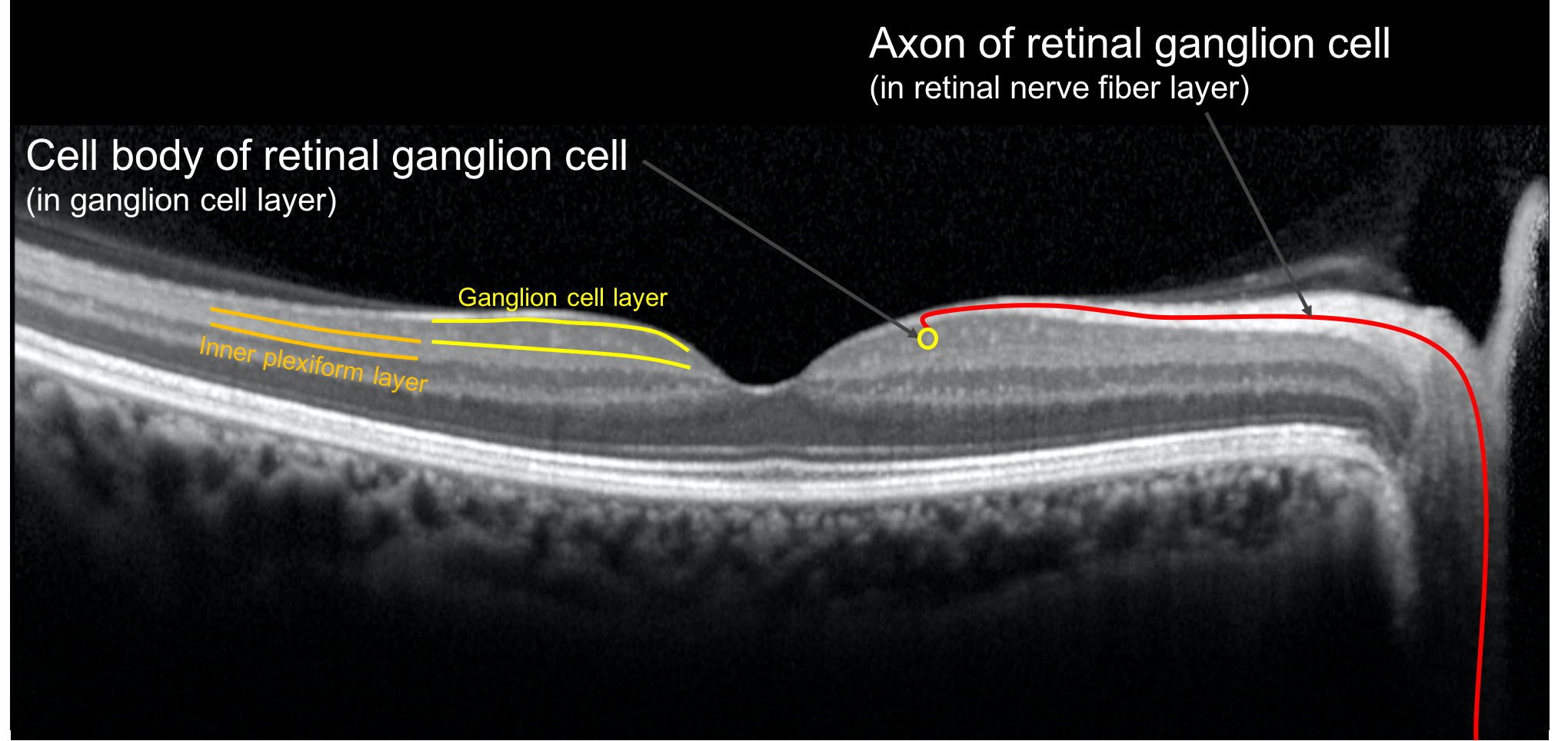
8. In what layer of the retina are the cell bodies of the retinal ganglion cells located? 2. Ganglion cell layer
The cell bodies of the retinal ganglion cells are located in the ganglion cell layer and their axons travel in the retinal nerve fiber layer.
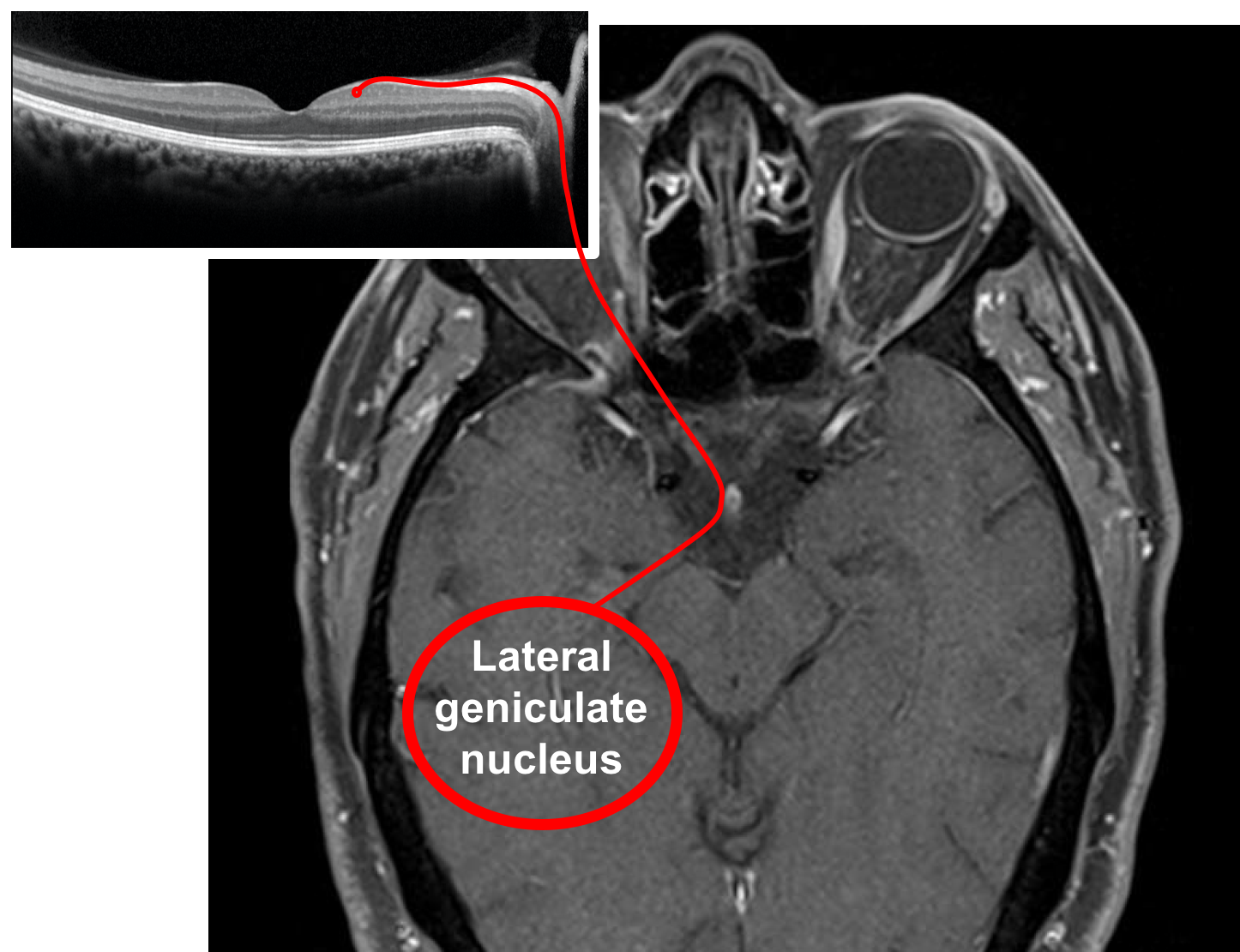
9. Where do most of the axons in the indicated layer synapse?
- Optic chiasm
- Optic tract
- Lateral geniculate nucleus
- Occipital lobe
9. Where do most of the axons in the indicated layer synapse? 3. Lateral geniculate nucleus
The red arrow is pointing to the retinal nerve fiber layer, which is composed of axons of the retinal ganglion cells that travel in the optic nerve, chiasm, and tract and synapse in the lateral geniculate body before they convey their information to the visual cortex. Disruption and death of the retinal ganglion cell axons in the optic nerve, chiasm or tract by compressive lesions will manifest as thinning of the RNFL and GCL in the retina.
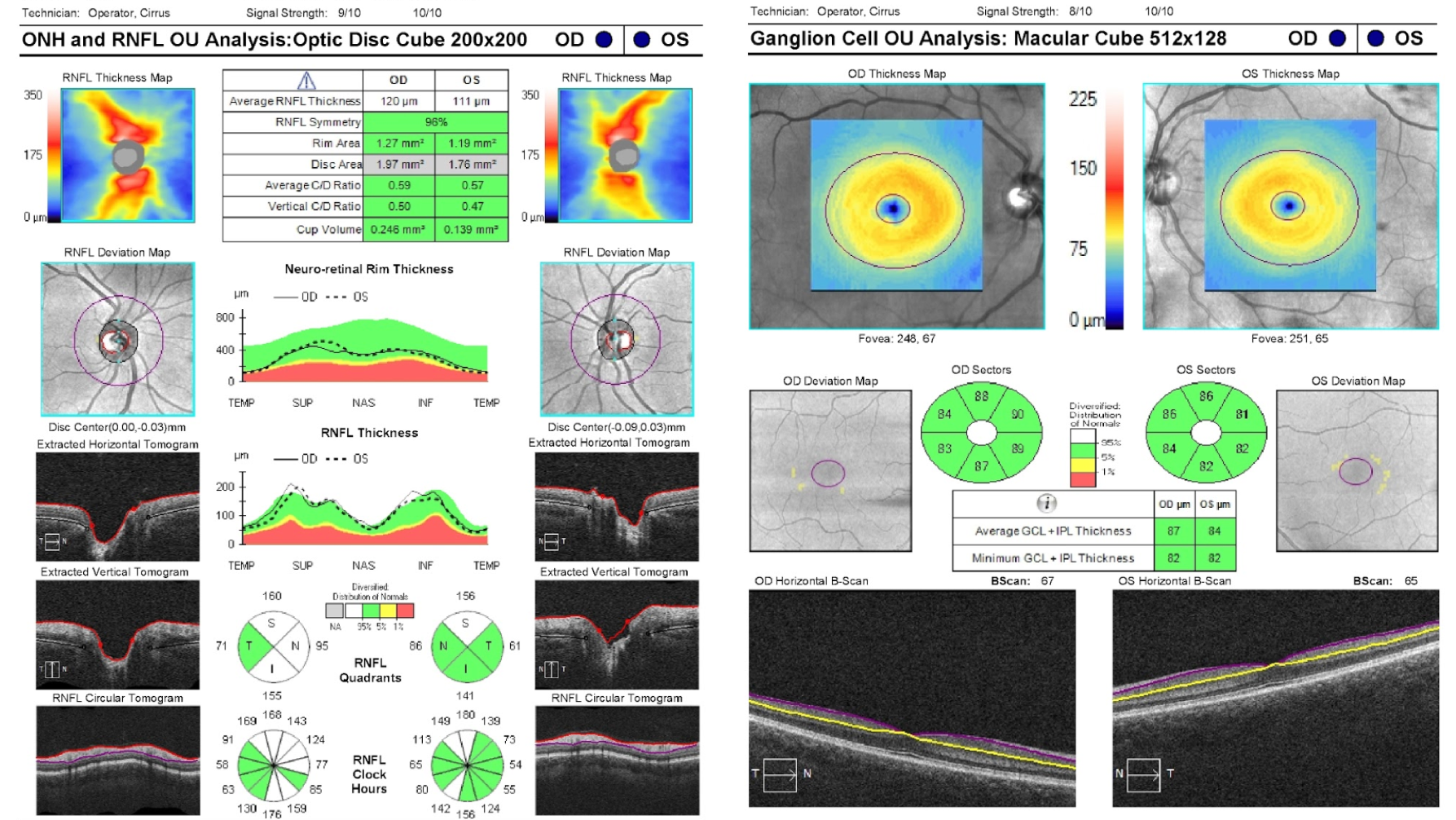
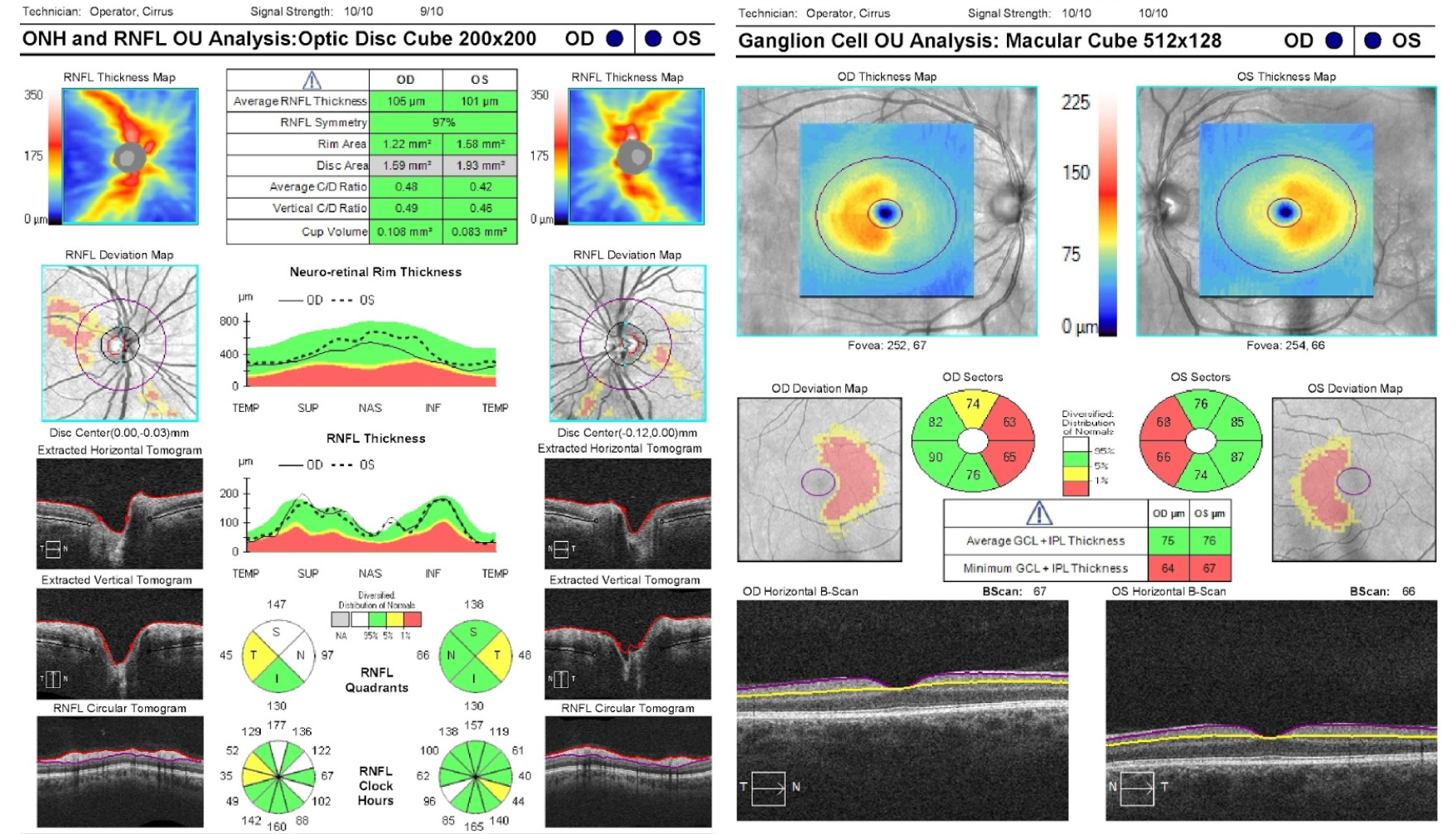
10. A normal Cirrus OCT of the retinal nerve fiber layer (RNFL) and macular ganglion cell complex (GCC) are shown below. What retinal layers are included in the GCC?
- Retinal nerve fiber layer, ganglion cell layer, inner plexiform layer
- Ganglion cell layer, inner plexiform layer, inner nuclear layer
- Ganglion cell layer and inner plexiform layer
- Ganglion cell layer only
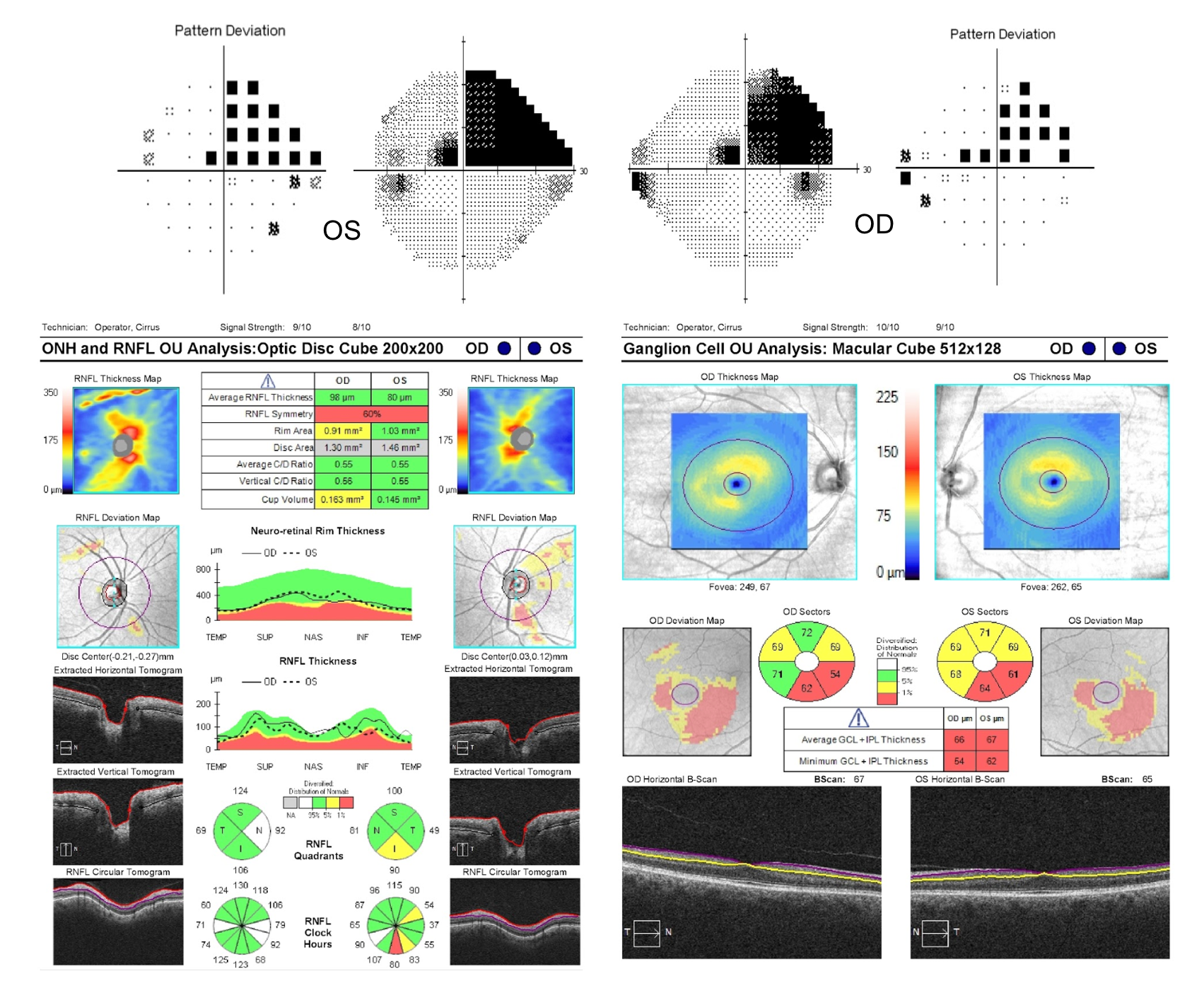
10. A normal Cirrus OCT of the retinal nerve fiber layer (RNFL) and macular ganglion cell complex (GCC) are shown below. What retinal layers are included in the ganglion cell complex? 3. Ganglion cell layer and inner plexiform layer
The Cirrus OCT machine measures the macular ganglion cell complex, which is the combination of the ganglion cell layer and inner plexiform layer, rather than just the ganglion cell layer alone. This scan is derived from the macular cube and is segmented to only measure the thickness of the GCC (located between the yellow and purple lines on the horizontal B-scan). Optic neuropathies lead to thinning of the macular ganglion cell complex and peripapillary RNFL and are useful in diagnosing and following patients with optic neuropathies.
Clinical Pearl
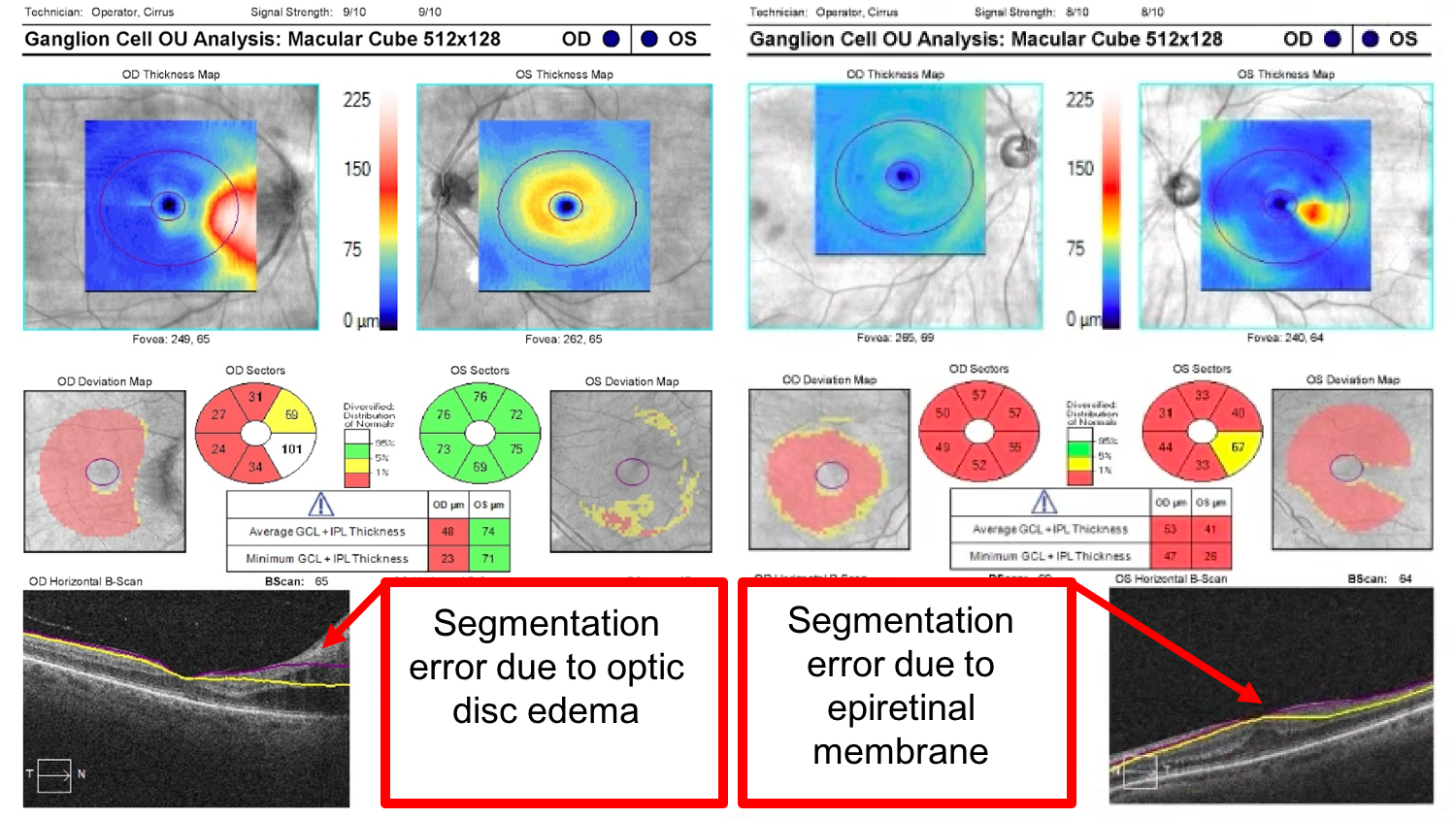
It is important to review the segmentation lines on the OCT of the macular ganglion cell complex.
11. A patient presents with mildly decreased vision in both eyes. The patient’s fundus appears normal and OCT of the RNFL and macular GCC are performed. What is the next best step for this patient?
- Intravenous fluorescein angiogram
- Multifocal ERG
- Automated perimetry and MRI of the brain and orbits
- Computer tomography angiography
11. A patient presents with mildly decreased vision in both eyes. The patient’s fundus appears normal and OCT of the RNFL and macular GCC are performed. What is the next best step for this patient? 3. Automated perimetry and MRI of the brain and orbits
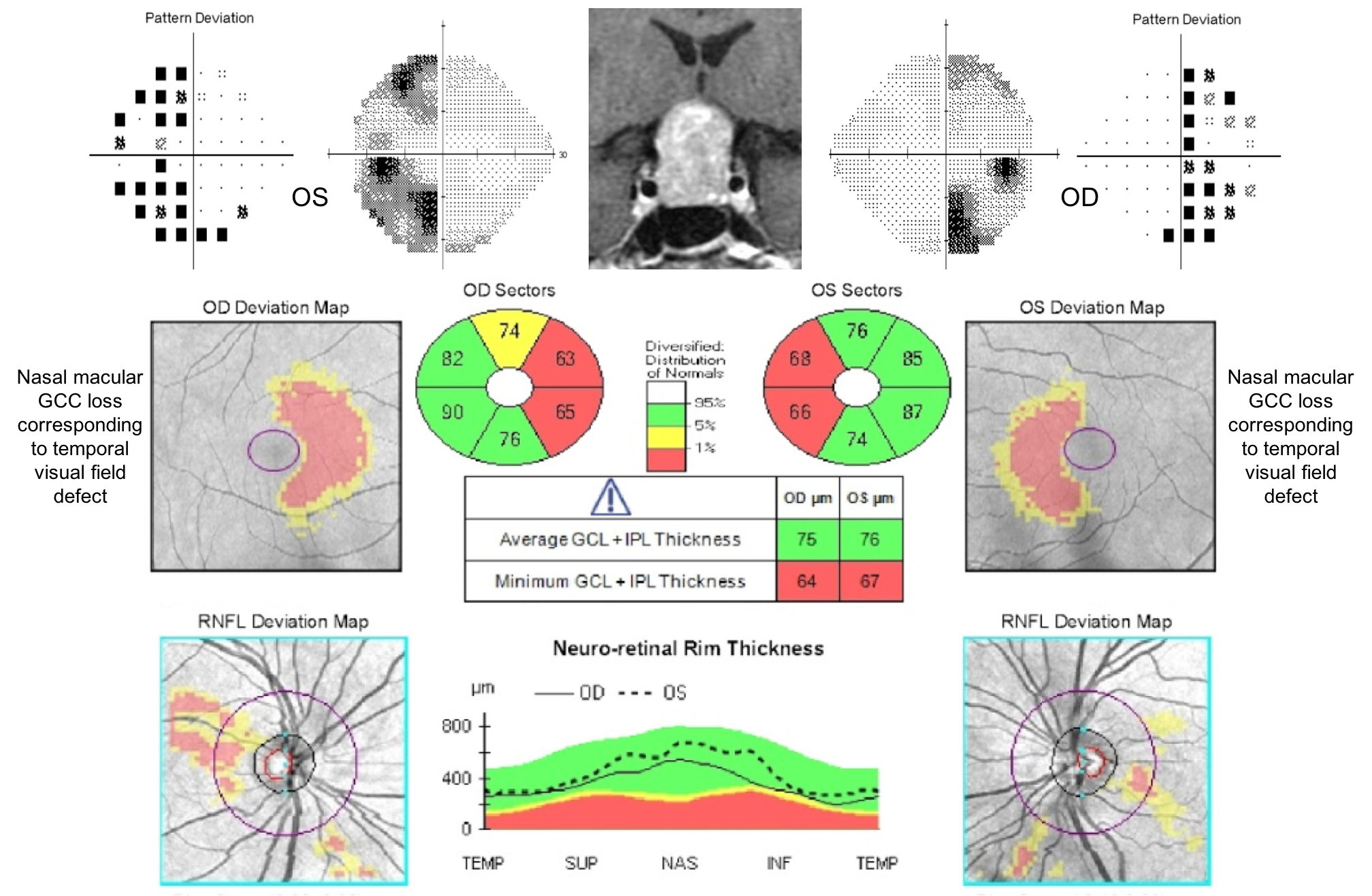
This patient has binasal thinning of the macular GCC indicating involvement of crossing nasal retinal fibers in the optic chiasm. The patient should be further evaluated in the clinic with formal visual field testing, which may show a bitemporal visual field defect since the nasal retina is responsible for the temporal visual field. Even in the absence of a visual field defect, the patient should be evaluated with an MRI of the brain and orbits with contrast due to concern for chiasmal compression. Damage to the anterior visual pathways may occur before visual field changes and OCT of the RNFL and macular GCC allows for earlier diagnosis of compressive optic neuropathies. This patient had a bitemporal hemianopia from a pituitary adenoma.
12. A patient developed vision loss in both eyes. An OCT of the RNFL and macular GCC are shown below. What visual field defect does he likely have?
- Right homonymous hemianopia
- Left homonymous hemianopia
- Bitemporal hemianopia
- Generalized constriction
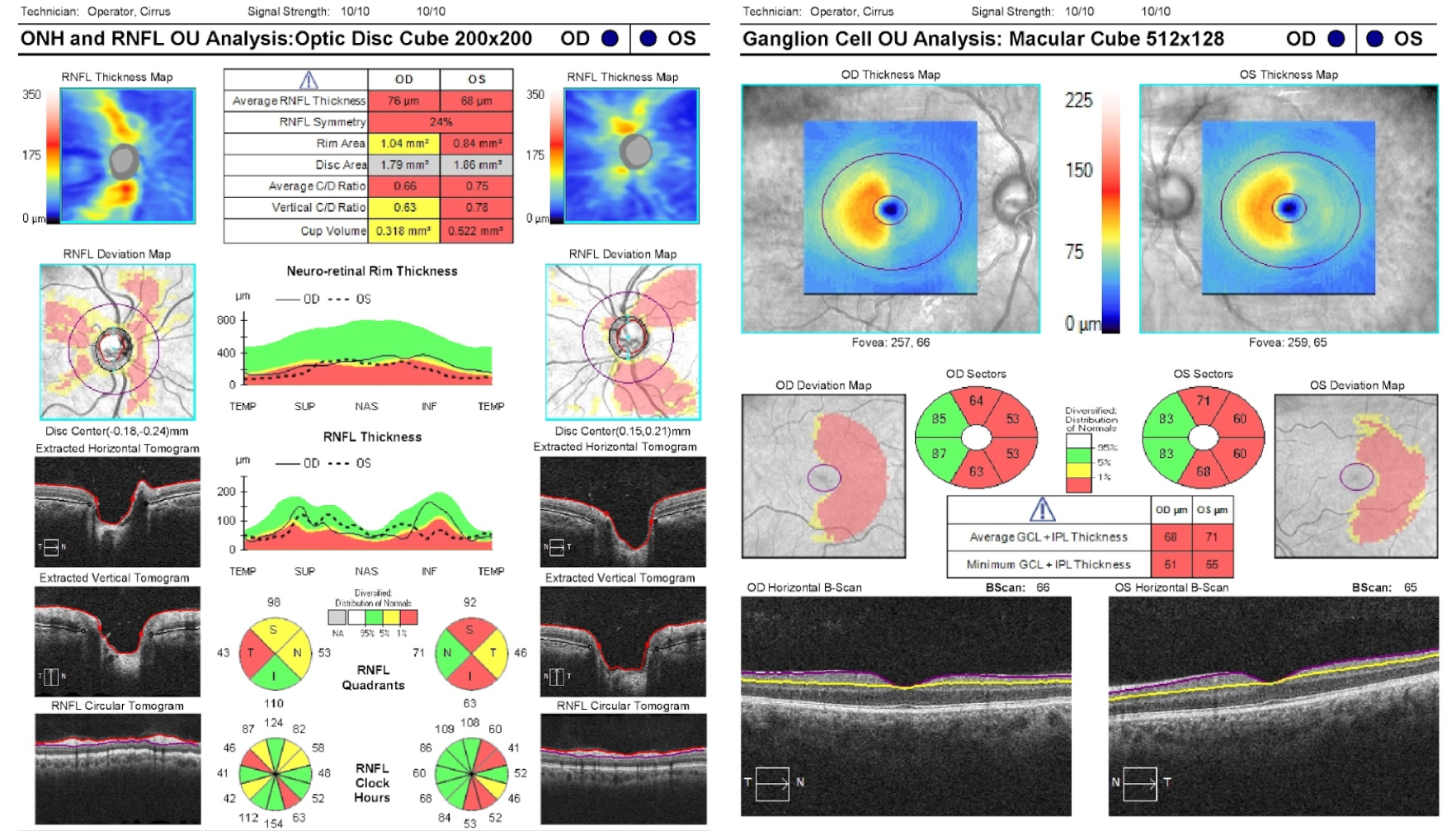
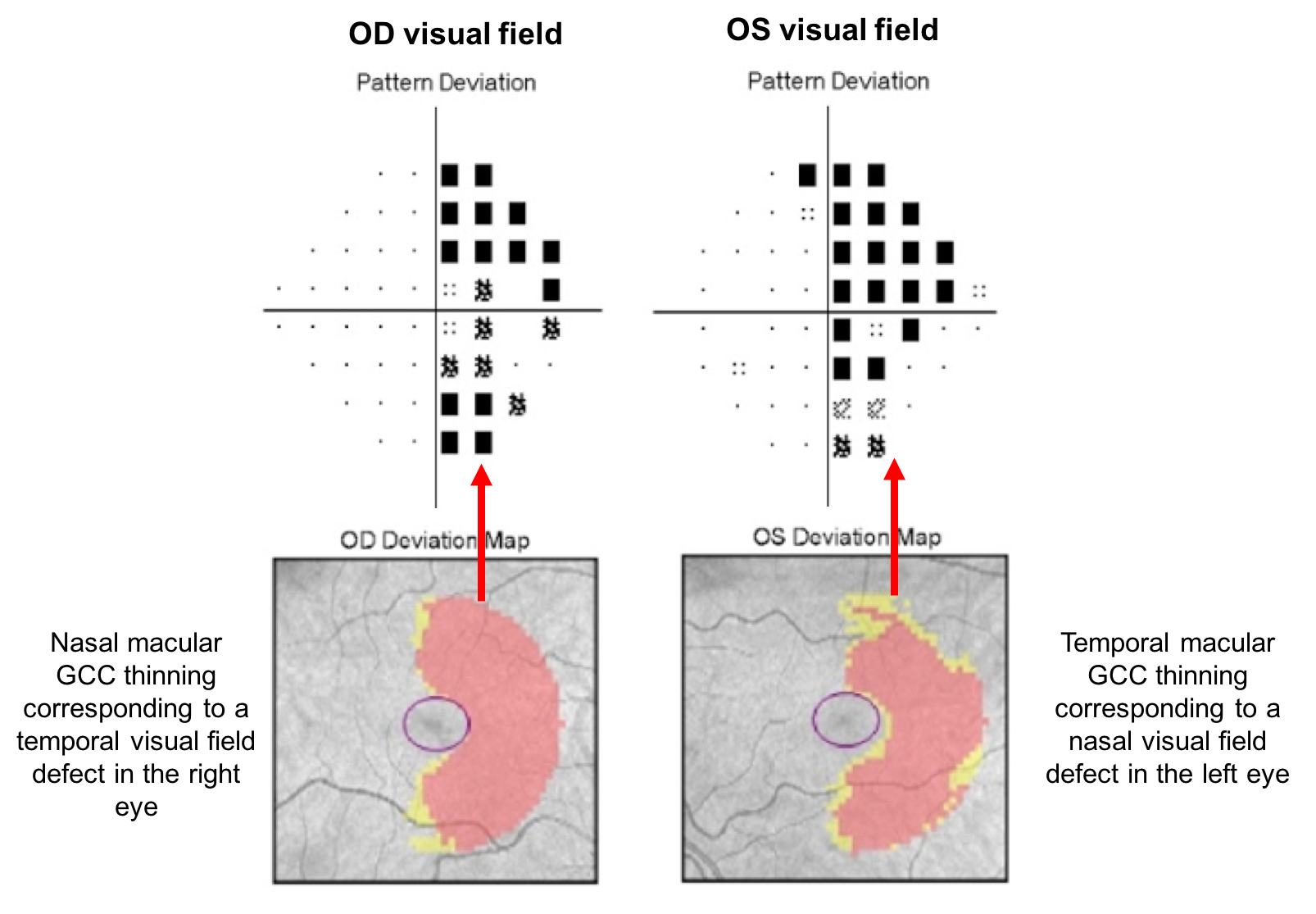
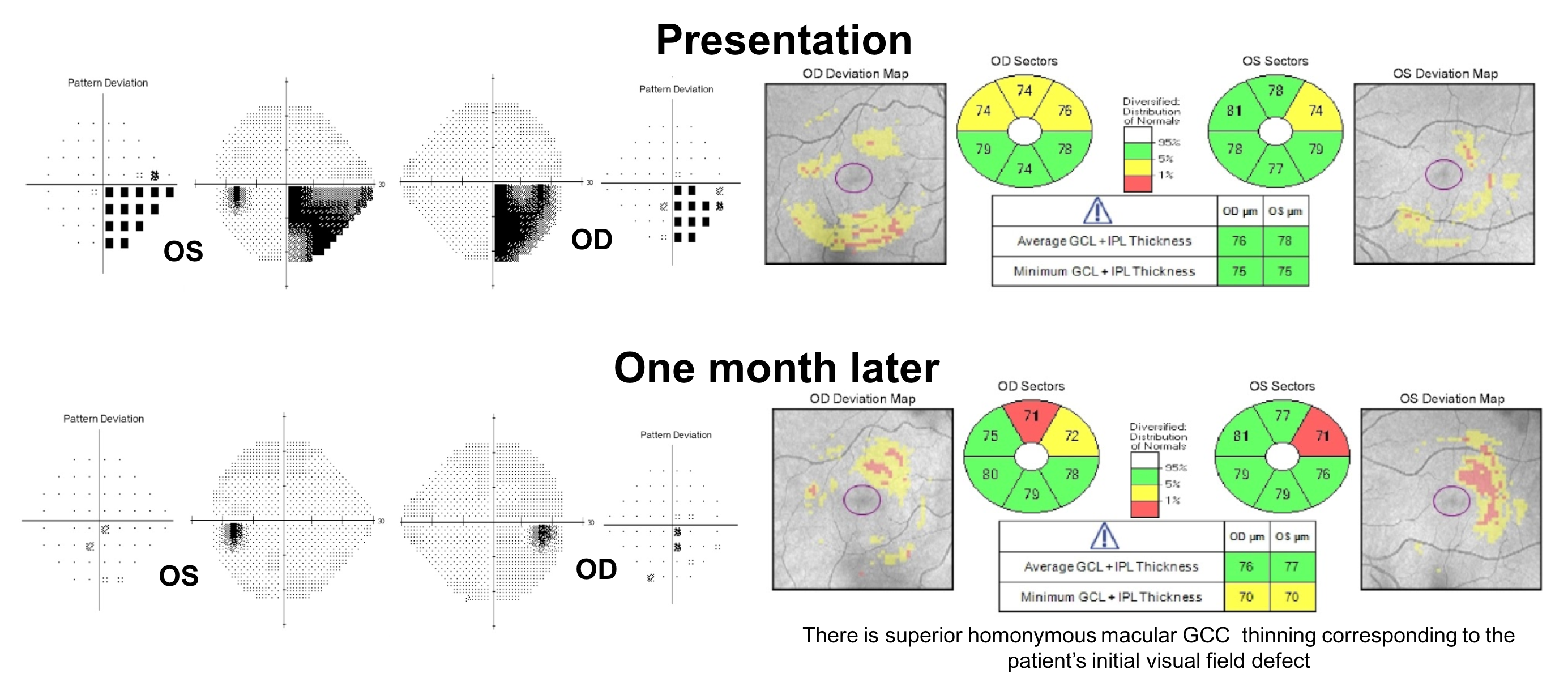
12. A patient developed vision loss in both eyes. An OCT of the RNFL and macular GCC are shown below. What visual field defect does he likely have? 1. Right homonymous hemianopia
This patient has homonymous macular GCC thinning, which corresponds to a homonymous visual field defect. The thinning of the macular GCC is nasal in the right eye and temporal in the left eye corresponding to temporal visual field loss in the right eye and nasal visual field loss in the left eye since the nasal retina is responsible for vision in the temporal visual field and vice versa. A temporal visual field defect in the right eye and a nasal visual field defect in the left eye corresponds to a right homonymous hemianopia as shown below.
13. The OCTs from the patient in the previous question were obtained within 3 months of vision loss. What is the most likely location of the patient’s lesion?
- Optic tract
- Temporal lobe
- Parietal lobe
- Occipital lobe
13. The OCTs from the patient in the previous question were obtained within 3 months of vision loss. What is the most likely location of the patient’s lesion? 1. Optic tract
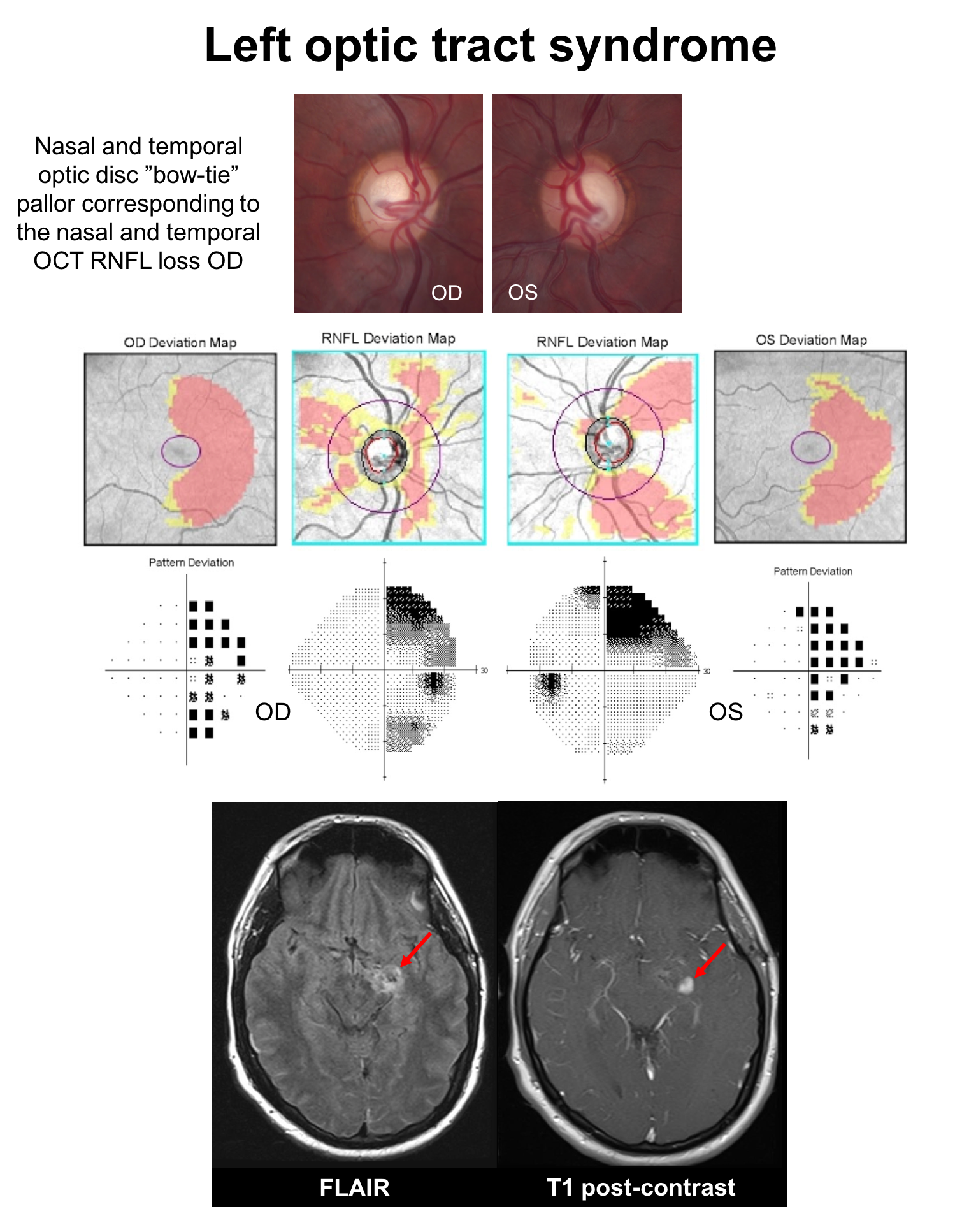
The patient has a right homonymous hemianopia localizing the process of the left retrochiasmal visual pathways. Since thinning of the inner retina occurred within 3 months of vision loss, the patient’s lesion is most likely in the left optic tract. If the lesion was retrogeniculate, then retrograde transsynaptic degeneration would need to occur and this takes much longer than 3 months to occur to this extent. Although the exact timing of retrograde transsynaptic degeneration has not been well characterized, it likely takes years to produce the amount of atrophy seen in this patient.
This patient has a pilocytic astrocytoma causing a left optic tract syndrome, which is characterized by a right RAPD (due to unequal crossing of fibers at the optic chiasm), right homonymous hemianopia and right “bow-tie” optic disc pallor (nasal and temporal pallor). Optic tract lesions are discussed in more detail in Chapter 12.
14. A 30-year-old man develops vision loss on the right side of his visual field and is found to have a demyelinating lesion in his left optic tract and other periventricular and infratentorial lesions disseminated in time and space. He is diagnosed with multiple sclerosis and treated with 3 days of intravenous methylprednisone 1 g daily and his visual field defect resolves after a week. What do you expect his OCT of the macular GCC to show in 1 month.
- It will remain normal
- Only the right eye will show thinning in the nasal retina
- Only the left eye will show thinning in the temporal retina
- There will be homonymous thinning corresponding to the original visual field defect
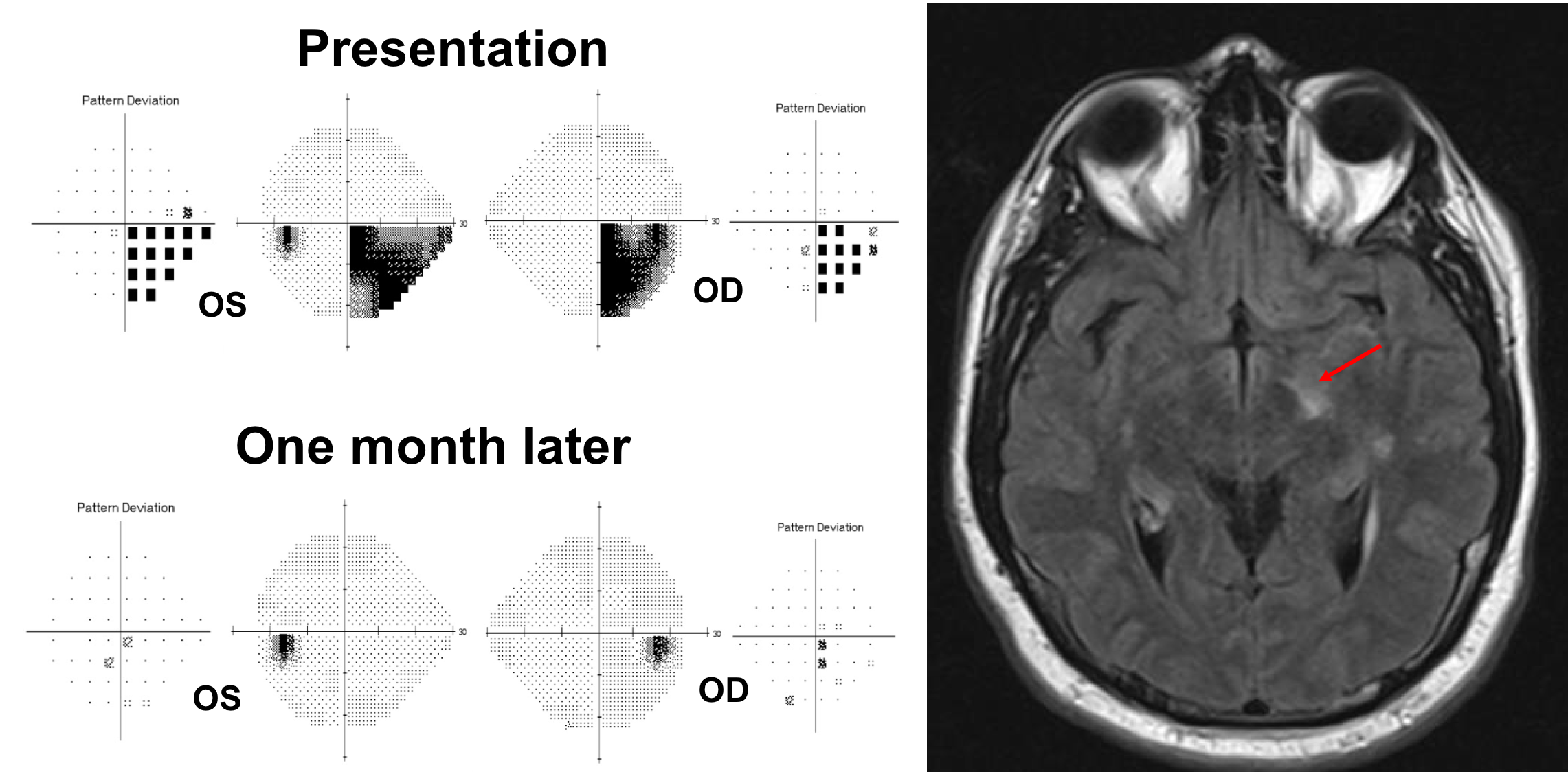
14. A 30-year-old man develops vision loss on the right side of his visual field and is found to have a demyelinating lesion in his left optic tract and other periventricular and infratentorial lesions disseminated in time and space. He is diagnosed with multiple sclerosis and treated with 3 days of intravenous methylprednisone 1 g daily and his visual field defect resolves. What do you expect his OCT of the macular GCC to show in 1 month. 4. There will be homonymous thinning corresponding to the original visual field defect
Homonymous visual field defects are uncommon in multiple sclerosis and are primarily a result of involvement of the optic tract. Although recovery of vision is the norm, the visual pathways sustain some permanent damage and retinal ganglion cells are lost. This patient had homonymous thinning of the macular GCC corresponding to the initial visual field defect. Due to the redundancy in the visual system, visual function is often well preserved even with a mild reduction in fibers in the anterior visual pathways.
15. A patient suffered bilateral occipital lobe strokes from atrial fibrillation 5 years ago. He presents for a routine follow-up and an OCT of the macular GCC is obtained. Why does he have macular GCC thinning?
- Bilateral optic neuropathies due to emboli from atrial fibrillation
- Papilledema related to atrial fibrillation
- Retinal artery occlusions related to atrial fibrilattion
- Retrograde transsynaptic degeneration
15. A patient suffered bilateral occipital lobe strokes from atrial fibrillation 5 years ago. He presents for a routine follow-up and an OCT of the macular GCC is obtained. Why does he have macular GCC thinning? 4. Retrograde transsynaptic degeneration
The patient has bilateral homonymous macular GCC loss from bilateral occipital lobe strokes suffered 5 years ago due to retrograde transsynaptic degeneration, which is a degeneration of neurons and axons following injury to cells with with which they synapse. The retinal ganglion cells synapse in the lateral geniculate nucleus before conveying their information to the visual cortex in the occipital lobe. Injury in the retrogeniculate visual pathways may lead to changes in the anterior visual pathways due to retrograde transsynaptic degeneration, which takes at least many months to years to develop. Retrochiasmal visual field defects are discussed in more detail in Chapter 13.
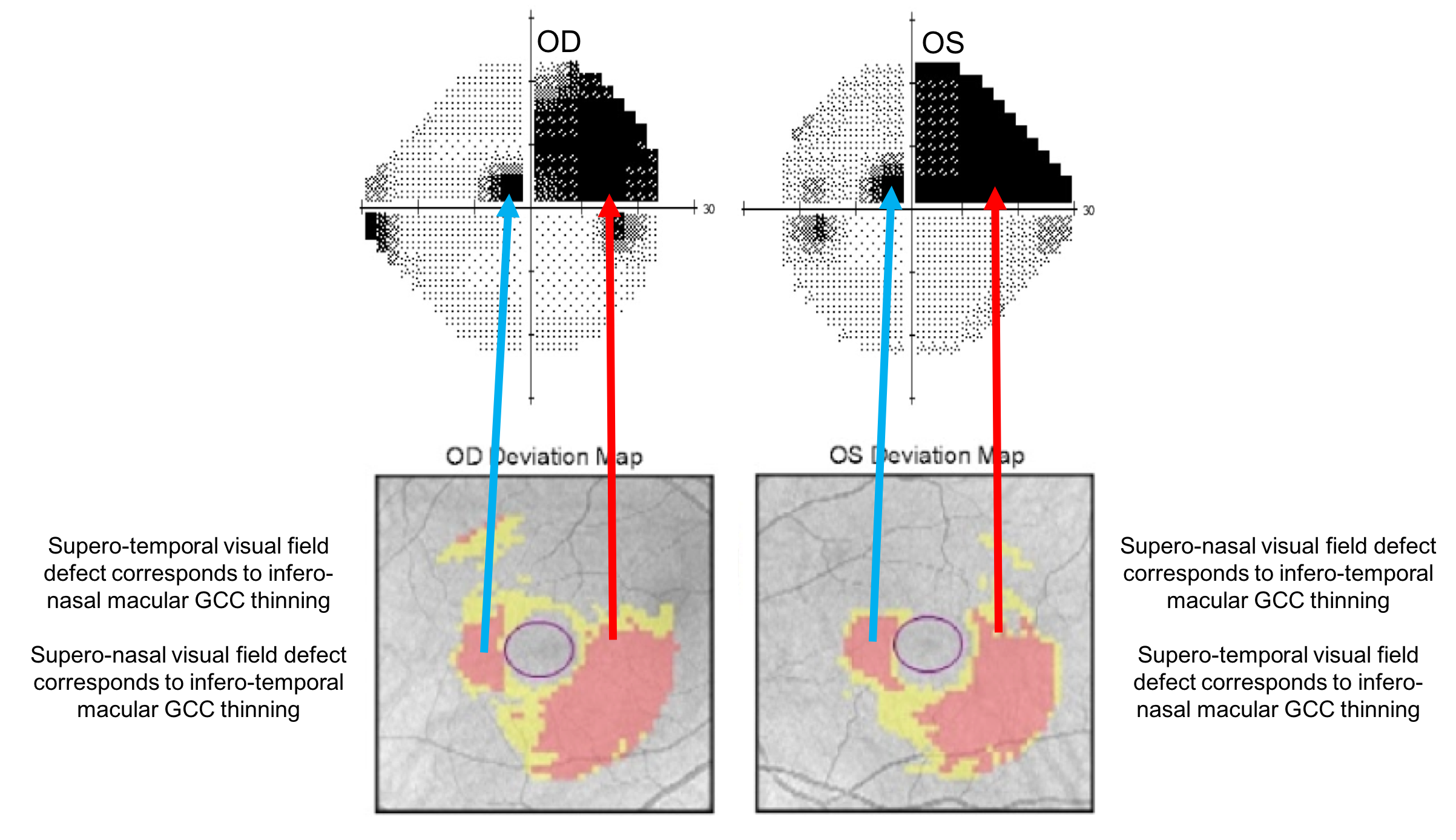
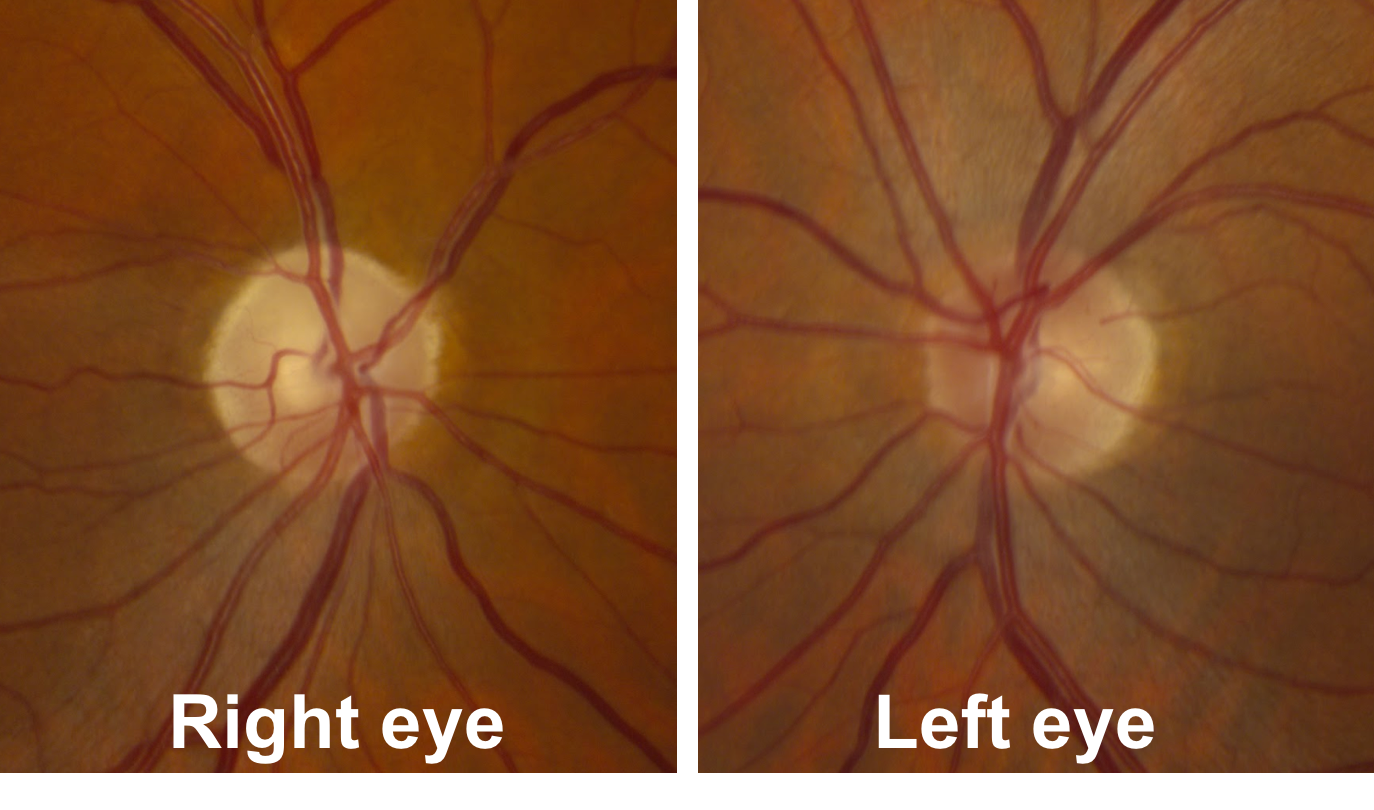
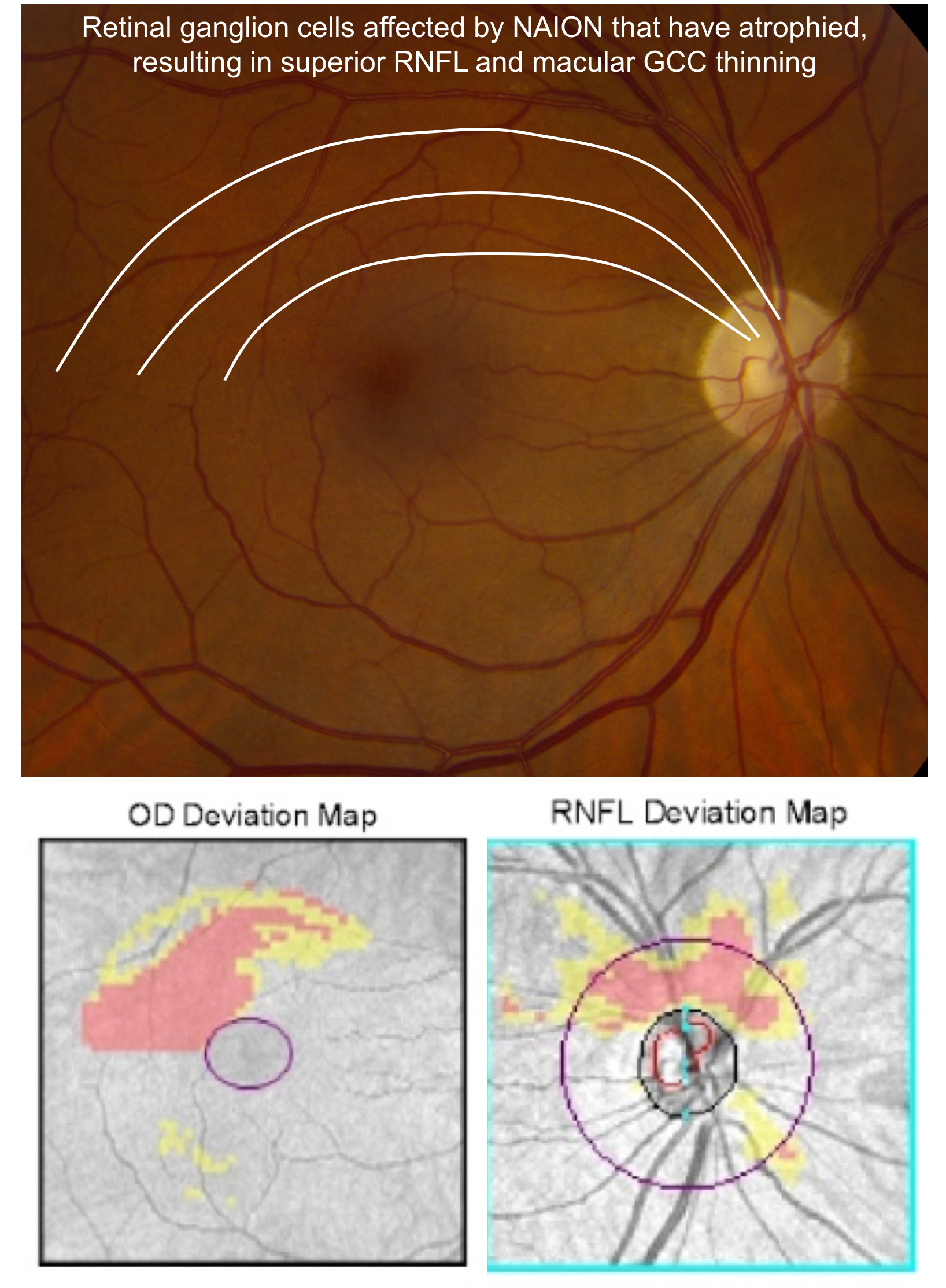
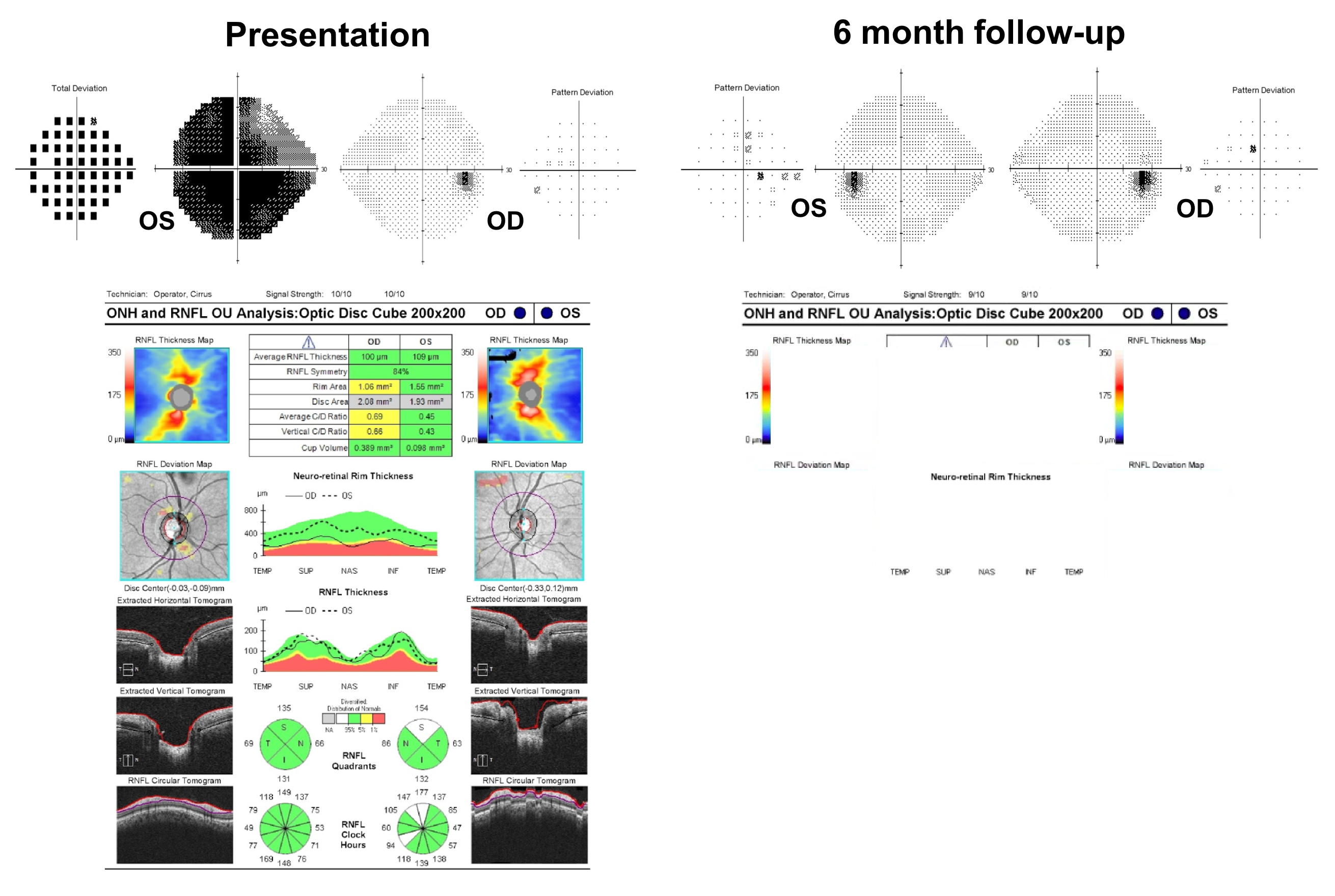
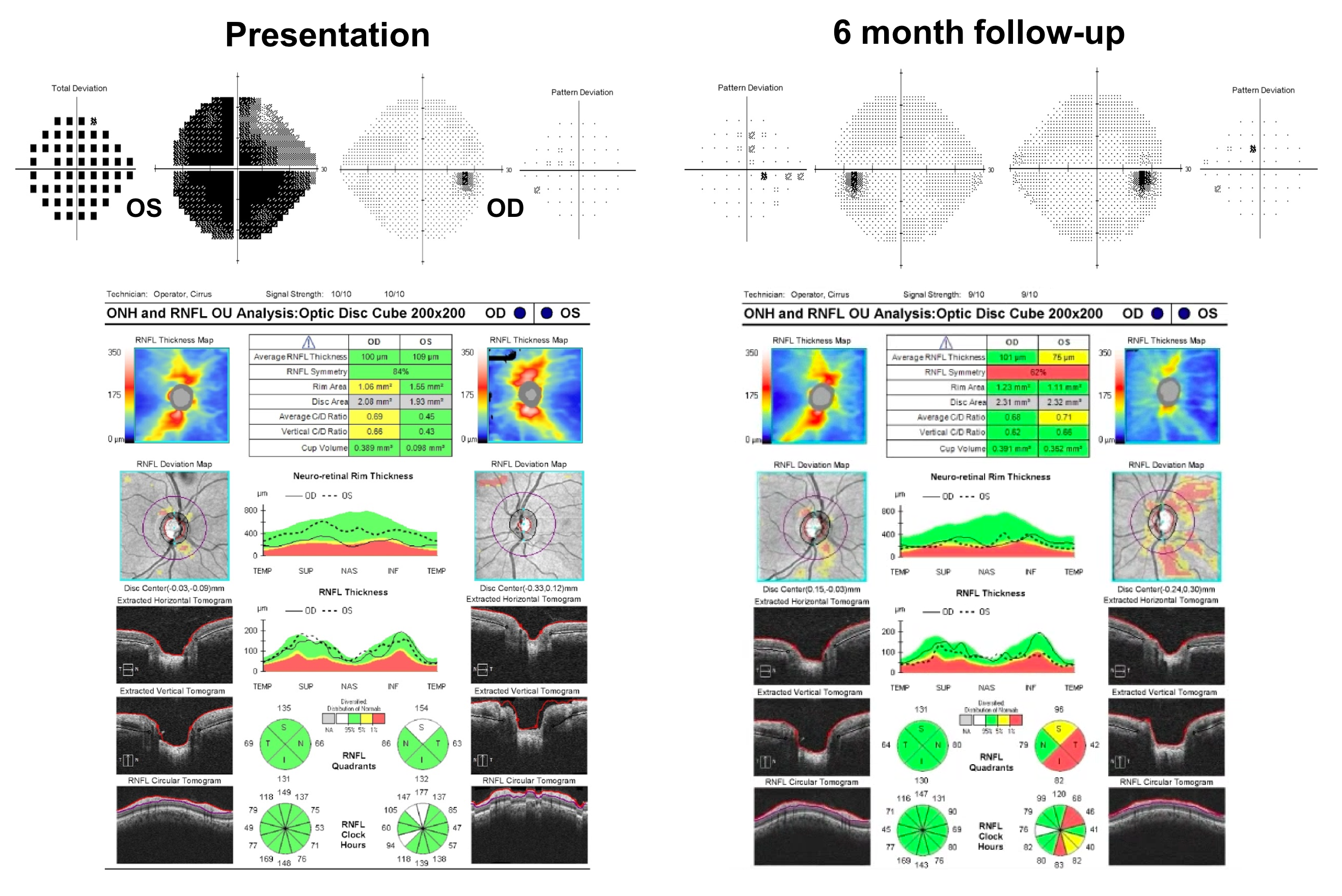
16. A patient with previous right non-arteritic anterior ischemic optic neuropathy (NAION) with an inferior visual field defect is seen in follow-up 6 months after the onset of vision loss. Her optic nerves are shown below. What do you expect the OCT of the RNFL and macular GCC to show?
- Inferior RNFL and inferior macular GCC thinning
- Superior RNFL and superior macular GCC thinning
- Inferior RNFL and superior macular GCC thinning
- Superior RNFL and inferior macular GCC thinning
16. A patient with previous right non-arteritic anterior ischemic optic neuropathy (NAION) with an inferior visual field defect is seen in follow-up 6 months after the onset of vision loss. Her optic nerves are shown below. What do you expect the OCT of the RNFL and macular GCC to show? 2. Superior RNFL and superior macular GCC thinning
In the acute stage of NAION, there is segmental or diffuse optic disc edema, which is followed by macular GCC loss and RNFL thinning in the area of the visual field defect. This patient’s right optic nerve demonstrates superior segmental optic disc pallor corresponding to atrophy of this part of the nerve. The axons from the superior part of the optic nerve correspond to retinal ganglion cell cell bodies only in the superior part of the retina (above the horizontal meridian). Optical coherence tomography is therefore expected to show superior RNFL and macular GCC thinning due to retinal ganglion cell axon and cell body death, respectively. Non-ateritic anterior ischemic optic neuropathy is discussed in more detail in Chapter 3.
17. A 25-year-old white woman develops left optic neuritis and is diagnosed with multiple sclerosis. She is treated with intravenous corticosteroids and recovers vision. Her visual field is normal at a 6 month follow-up visit. What do you expect her OCT of the RNFL to show in the left eye at the 6 month follow-up visit?
- The RNFL thickness will remain normal
- The RNFL thickness will increase
- The RNFL thickness will decrease
- The RNFL thickness will remain the same, but decrease at 12 months
17. A 25-year-old white woman develops left optic neuritis and is diagnosed with multiple sclerosis. She is treated with intravenous corticosteroids and recovers vision. Her visual field is normal at a 6 month follow-up visit. What do you expect her OCT of the RNFL to show in the left eye at the 6 month follow-up visit? 3. The RNFL thickness will decrease
Patients with optic neuritis typically recover vision with or without treatment. Although visual acuity and visual field often recover, patients notice that their vision, especially contrast sensitivity does not completely return to normal. This is because there is loss of retinal ganglion cells that begins within a few weeks of vision loss and this can be detected with OCT of the RNFL and macular GCC. Optic neuritis is discussed in more detail in Chapters 5 and 6.
18. A patient presents with blurry vision in her left eye and has an OCT of the RNFL as part of her ophthalmological assessment. Which of the following is a correct interpretation of her OCT?
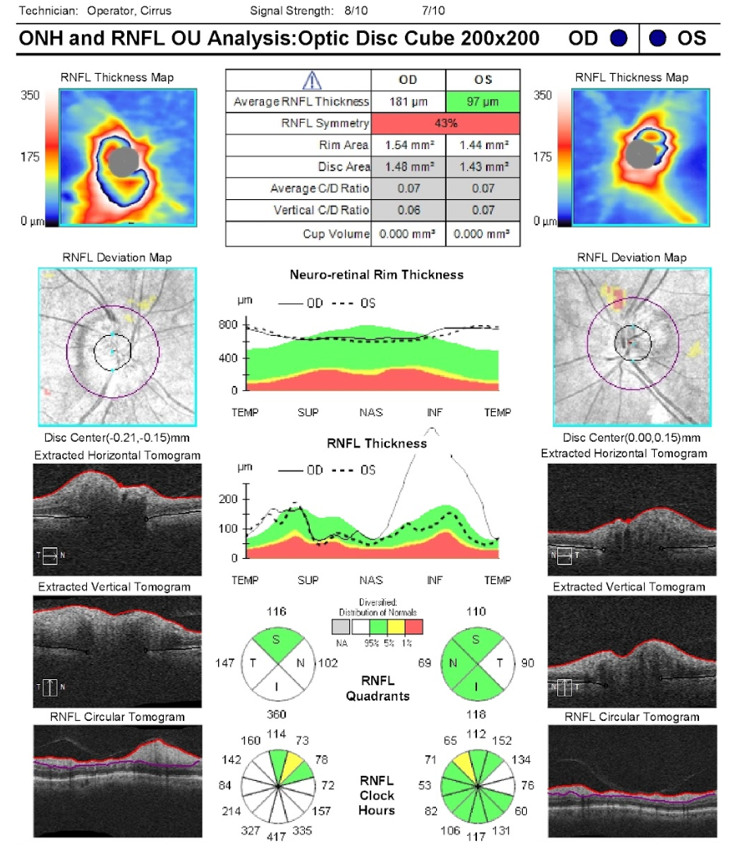
- The left eye does not have an optic neuropathy
- The left eye should have a normal visual field
- The left eye does not have a relative afferent pupillary defect (RAPD)
- The left eye may have an optic neuropathy
18. A patient presents with blurry vision in her left eye and has an OCT of the RNFL as part of her ophthalmological assessment. Which of the following is a correct interpretation of her OCT? 4. The left eye may have an optic neuropathy
This patient’s OCT demonstrates an RNFL thickness within the normal range when compared to a normative database. However, it does not give us any information about the patient’s visual function nor does it rule out an optic neuropathy. This patient’s left optic nerve is shown below and there is optic disc edema and an optic disc hemorrhage due to non-arteritic anterior ischemic optic neuropathy. Although most edematous optic nerves will demonstrate an elevated RNFL thickness, as the edema resolves and the patient develops atrophy, the RNFL thickness may fall within the normal range. Optical coherence tomography provides helpful information, but it must be interpreted in the context of the patient’s full ophthalmological assessment.
Clinical Pearl
A retinal nerve fiber thickness within the normal range does not rule out an optic neuropathy.
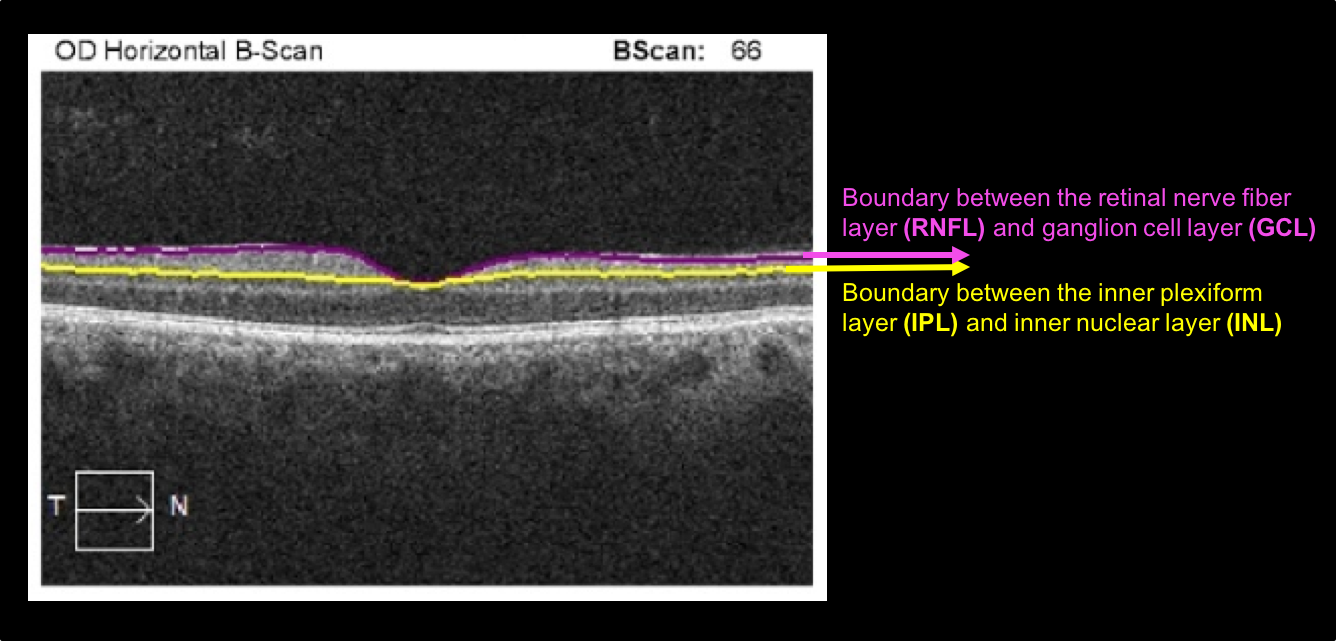
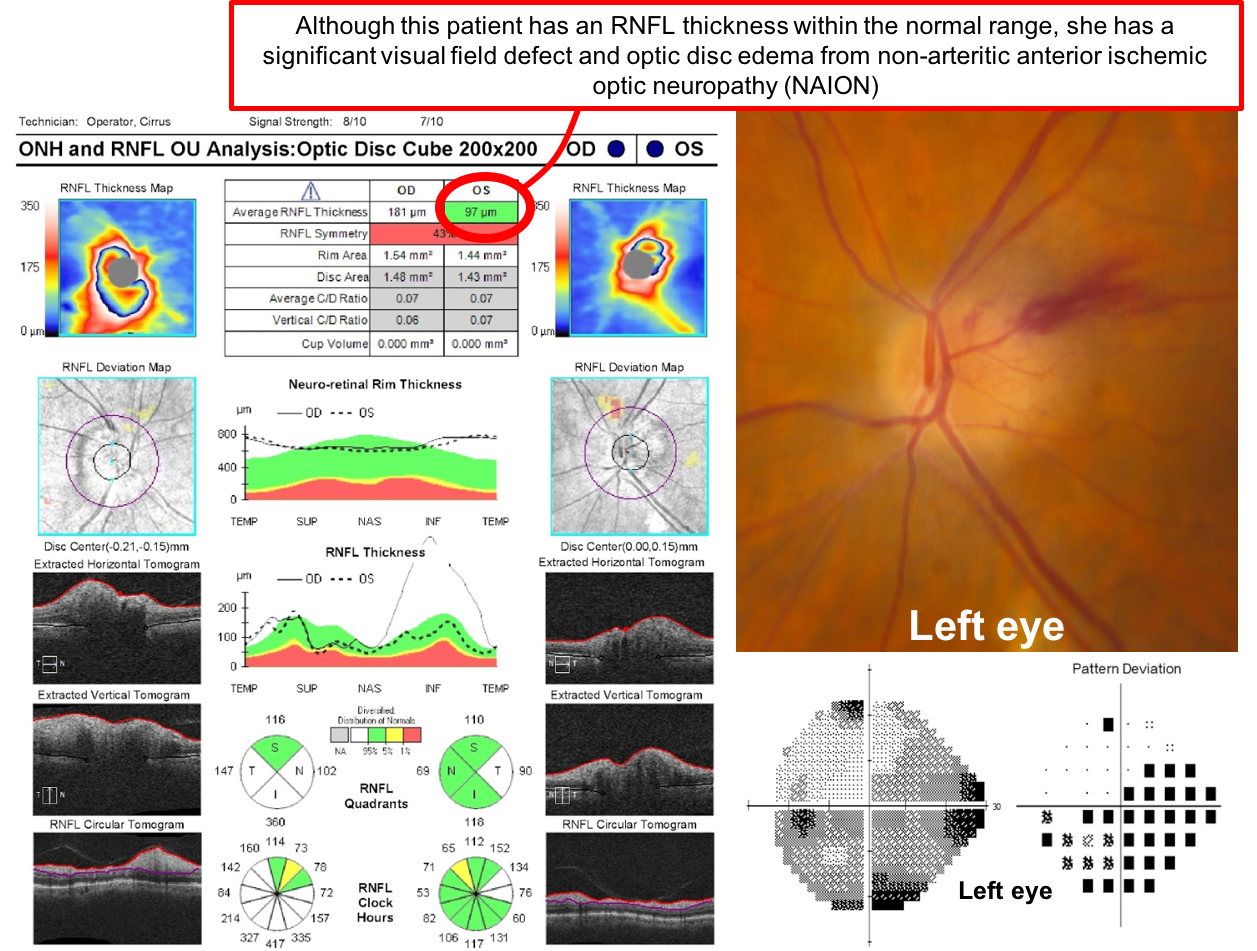
19. A patient presents with a two day history of right eye vision loss. She has a right relative afferent pupillary defect and optic disc edema. Optical coherence tomography of the RNFL and macular GCC are obtained. Which of the following is true regarding these tests?
- The patient has macular GCC atrophy in the right eye at this time
- The patient’s RNFL thickness in the right eye is lower than average
- The right optic disc edema has led to a segmentation artifact in the macular GCC
- The thickness of the right macular GCC is greater than average
19. A patient presents with a two day history of right eye vision loss. She has a right relative afferent pupillary defect and optic disc edema. Optical coherence tomography of the RNFL and macular GCC are obtained. Which of the following is true regarding these tests? 3. The right optic disc edema has led to a segmentation artifact in the macular GCC
The Cirrus OCT machine uses an automated algorithm to determine the position of the ganglion cell complex and this may fail in various contexts such as optic disc edema or macular pathology as shown below. It is important to review the Horizontal B-scans for the position of the segmentation lines to avoid misinterpreting the measurements.
20. Which of the following is true regarding OCT-angiography (OCT-A)?
- It detects leakage similar to intravenous fluorescein angiography
- It makes use of moving structures such as red blood cells as motion contrast
- It relies on the intrinsic vibration of the human body to image the entire retina
- It can only image blood vessels smaller than 5 µm due to the wavelength of visit light
20. Which of the following is true regarding OCT-angiography (OCT-A)? 2. It makes use of moving structures such as red blood cells as motion contrast
OCT-A is a noninvasive means to obtain 3-dimensional vascular mapping of the retinal microcirculation. It measures the differences in signal intensity between sequential B-scans from a given area. Static tissue will show little change whereas moving structures such as RBCs will present variations from one image to another acting as motion contrast and generating fundus angiograms. A commonly used algorithm is the split-spectrum amplitude decorrelation angiography (SSADA), which obtains 70,000 A-scans per second to obtain OCTA volumes of 304 x 304 A-scans in 2.6 seconds resulting in a cube. There are different field of views available, 3 x 3 mm, 6 x 6 mm, and 8 x 8 mm.
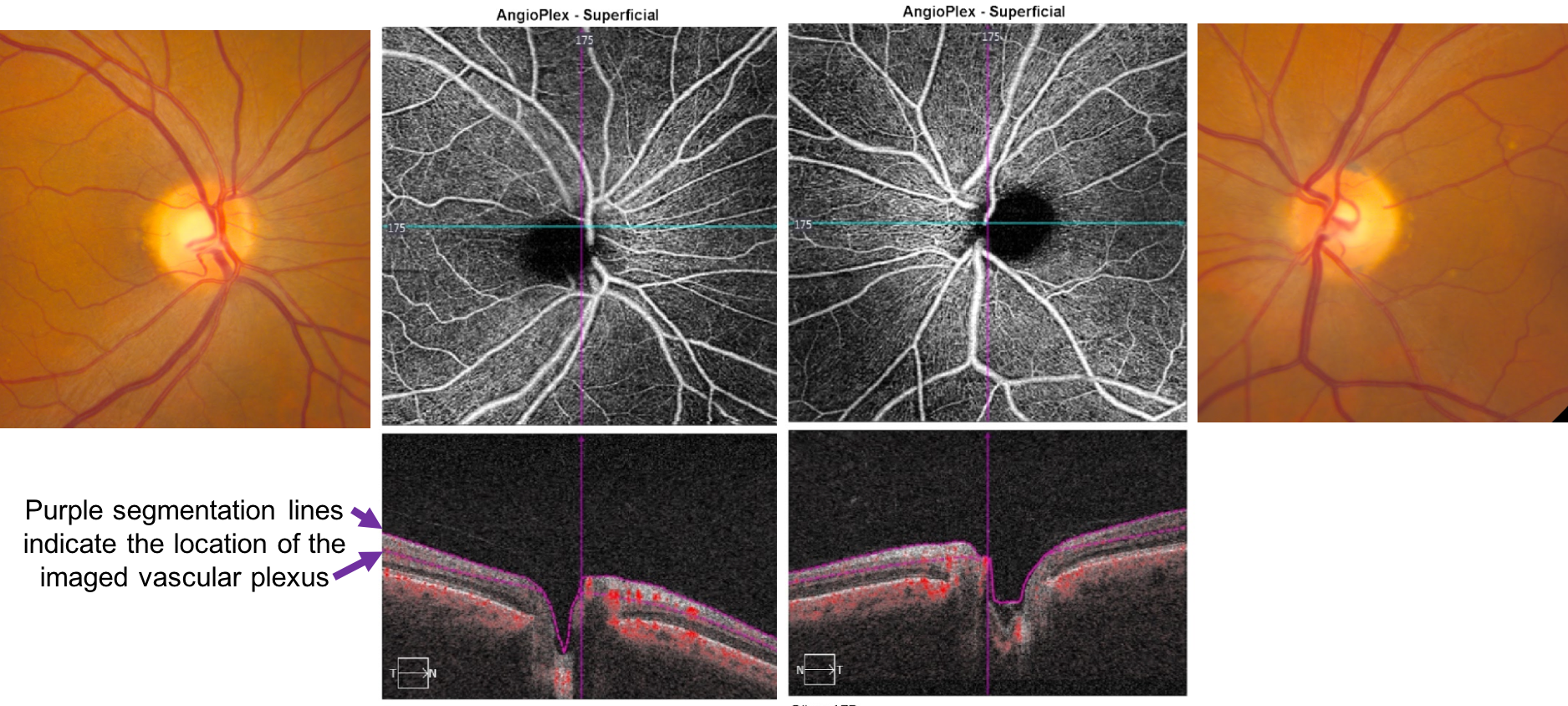
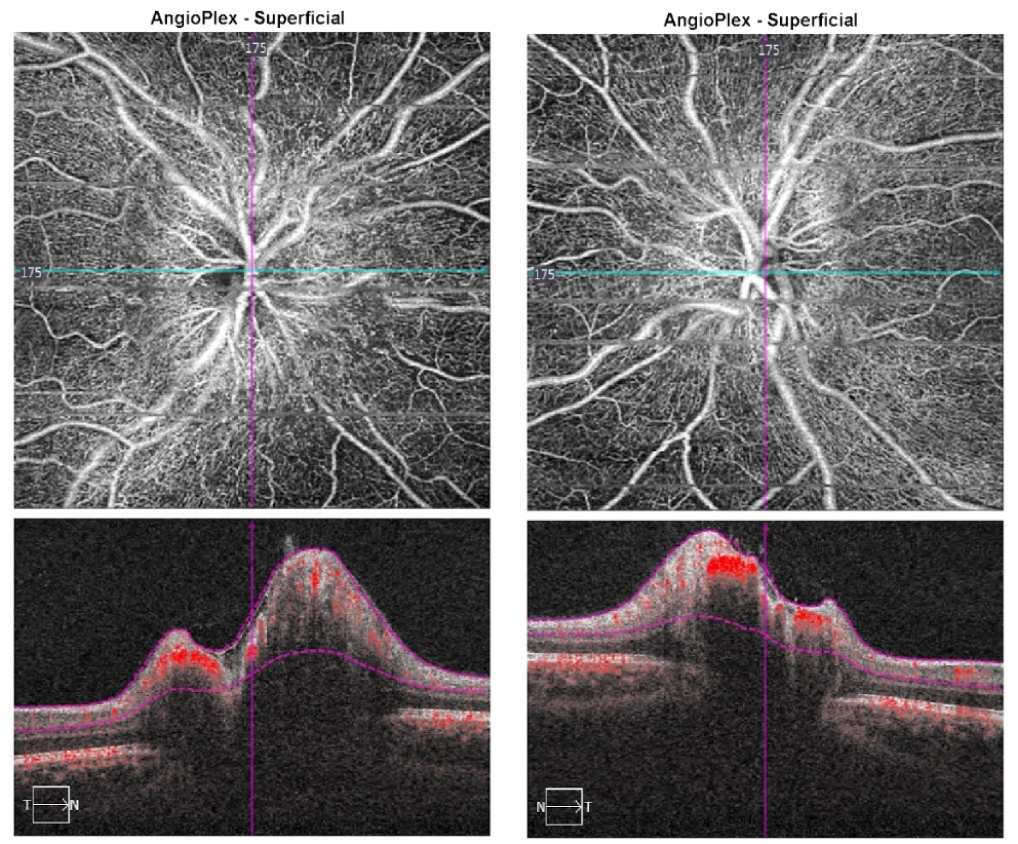
Normal OCT-A of the optic disc
A normal OCT-A of the superficial vascular plexus of the optic disc is shown below (6 x 6 mm).
21. Which of the following is true regarding the vascular layers imaged by OCT-A?
- All the vascular layers obtained with OCT-A are visible on intravenous fluorescein angiogram
- Vascular structures below the retinal pigment epithelium cannot be imaged
- The cube is divided into 4 slabs representing different segments of the retina
- All the vascular layers imaged with OCT-A are similar to those seen with indocyanine green angiography
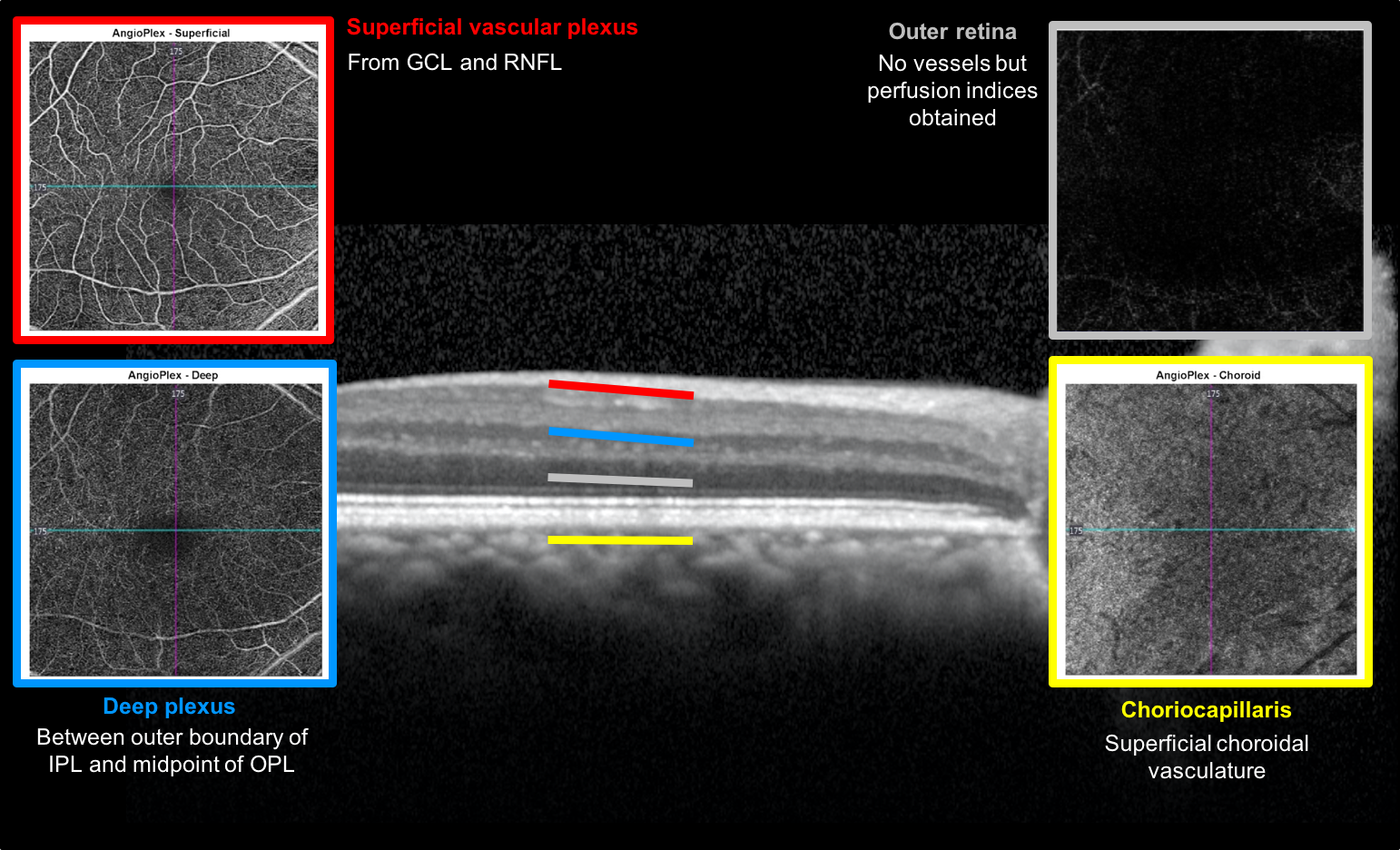
21. Which of the following is true regarding the vascular layers imaged by OCT-A? 3. The cube is divided into 4 slabs representing different segments of the retina
The cube of retina imaged with OCT-A is divided into 4 slabs representing different segments of the retina: the superficial vascular plexus (from the ganglion cell layer and retinal nerve fiber layer), deep plexus (between outer boundary of inner plexiform layer and midpoint of outer plexiform layer), outer retina (level of photoreceptors, it does not have vessels but perfusion indices are obtained), and choriocapillaris (superficial choroidal vasculature below Bruch’s membrane). The superficial vascular plexus is normally visible with intravenous fluorescein angiography whereas the deep plexus isn’t.
Vascular layers imaged with OCT-A
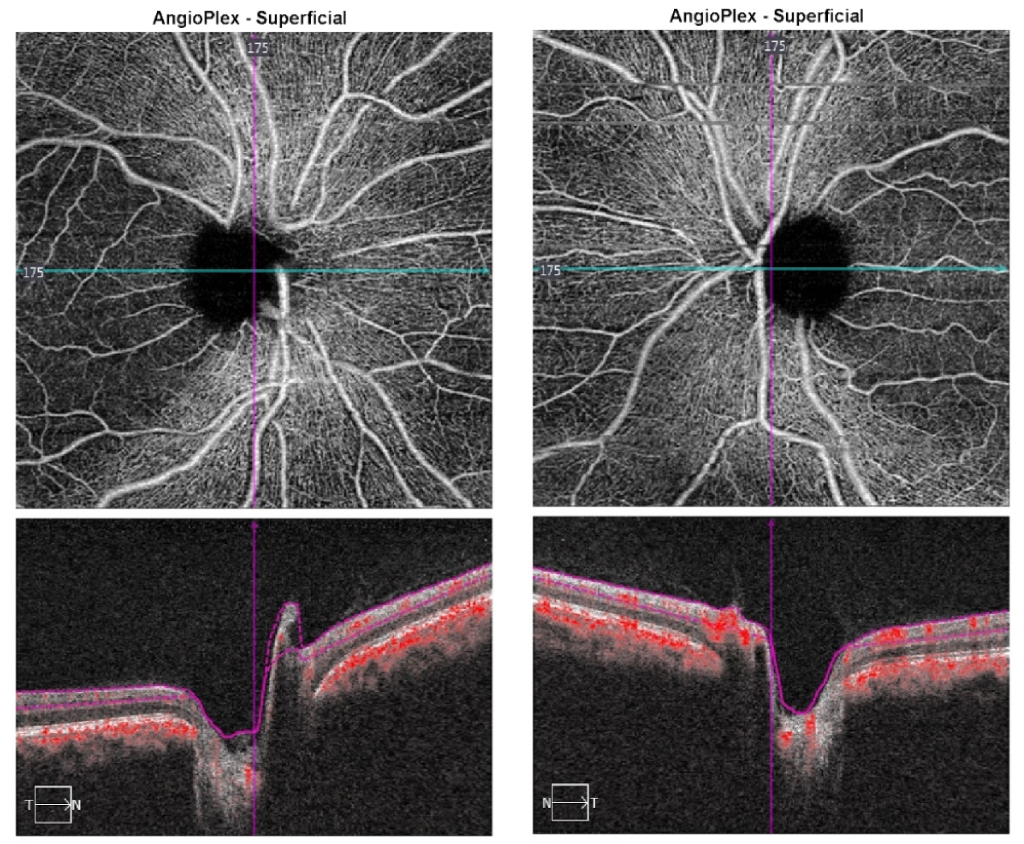
22. A 21-year-old man has a bilateral optic neuropathy that developed several years ago. What is the most pertinent finding from the OCT-A of his optic nerves? (superficial vascular plexus shown)
- Choroidal neovascularization
- Dilated retinal arterioles
- Increased microvasculature on the optic nerve head
- Vasculature dropout in the papillomacular bundle
22. A 21-year-old man has a bilateral optic neuropathy that developed several years ago. What is the most pertinent finding from the OCT-A of his optic nerves? (superficial vascular plexus shown) 4. Vasculature dropout in the papillomacular bundle
This patient has bilateral optic neuropathies from Leber’s Hereditary Optic Neuropathy (LHON) that primarily affects the papillomacular bundle. As seen on the OCT of the RNFL below, there is temporal loss of the RNFL and the superficial vascular plexus dropout mirrors the RNFL loss. The temporal part of the optic nerves appear pale due to the loss of the RNFL and microvasculature in this area. Since LHON affects the RNFL and ganglion cell layer, the deep vascular plexus in this patient is normal.
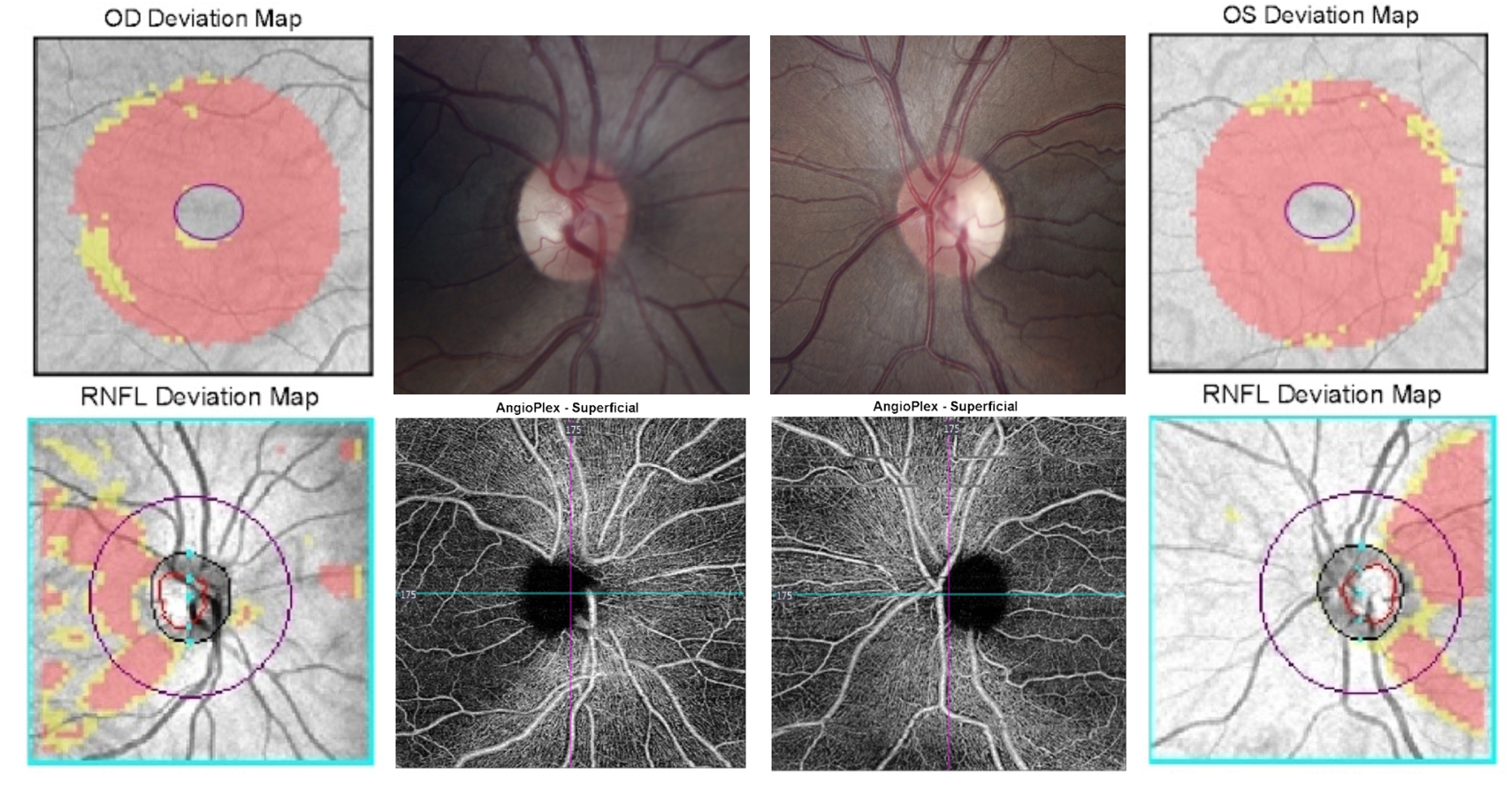
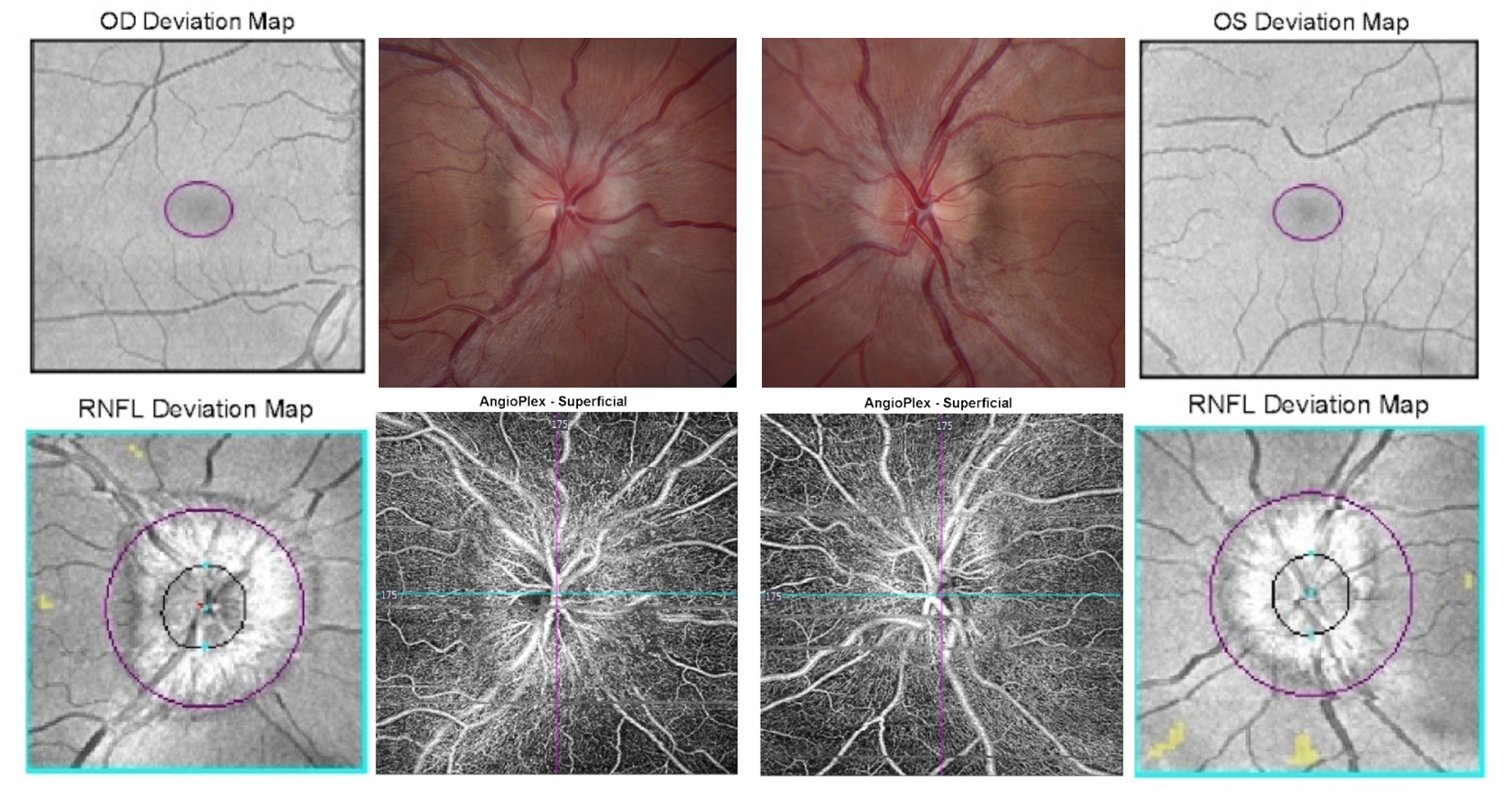
23. A 27-year-old woman was referred for an optic nerve abnormality detected on a routine eye examination. What is the most pertinent finding from the OCT-A? (superficial vascular plexus shown)
- Increased visibility of the peripapillary vascular network
- Vasculature dropout in the papillomacular bundle
- Peripapillary choroidal neovascular membrane
- Leakage from the optic disc
23. A 27-year-old woman was referred for an optic nerve abnormality detected on a routine eye examination. What is the most pertinent finding from the OCT-A? (superficial vascular plexus shown) 1. Increased visibility of the peripapillary vascular network
This patient had bilateral optic disc edema incidentally noted on a routine eye exam and was diagnosed with idiopathic intracranial hypertension (IIH). The OCT-A shows increased visibility of the peripapillary microvascular network consistent with the telangietactic blood vessels and optic disc hyperemia seen in papilledema. The microvessels on the optic disc are not visible by clinical examination or with optic disc photos.
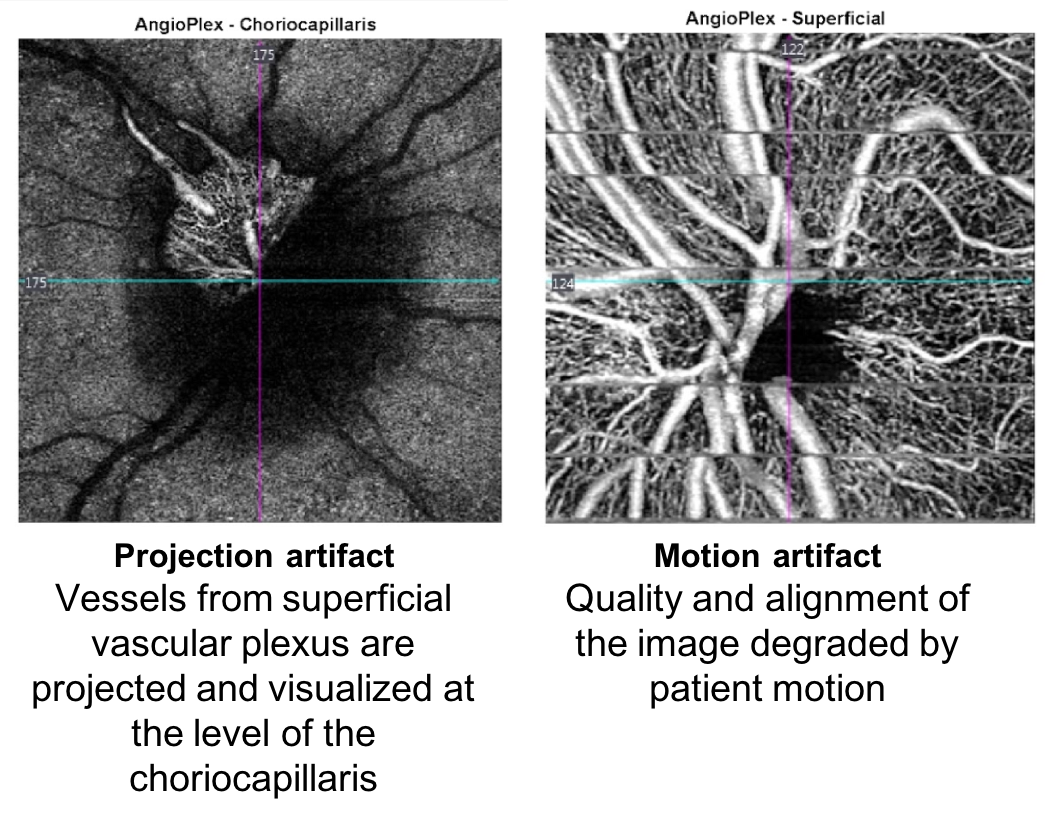
OCT-A Artifacts
Some limitations of OCT-A include:
- Extremely motion sensitive and motion artifacts may be seen
- May have errors in segmentation (can be manually delineated after scan)
- A projection artifact is when deeper layers seem to have the vasculature pattern of overlying vessels. It is due to fluctuation of light that has passed through moving blood from the inner vessels.
Further reading:
- Tao, LW, Wu Z, Guymer RH, Luu CD. Ellipsoid zone on optical coherence tomography: a review. Clin Exp Ophthalmol 2016; 44: 422–430. https://www.amedeolucente.it/public/EZ.pdf
- Spaide RF, Curcio CA. Anatomical correlates to the bands seen in the outer retina by optical coherence tomography. Retina 2011;31(8):1609-1619. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3619110/
- Ghazi NG, Tilton EP, Patel B, Knape RM, Newman SA. Comparison of macular optical coherence tomography findings between postacute retinal artery occlusion and nonacute optic neuropathy. Retina 2010 30(4):578-85. https://insights.ovid.com/crossref?an=00006982-201004000-00007
- Kardon RH. Role of the macular optical coherence tomography scan in neuro-ophthalmology. J Neuroophthalmol 2011; 31: 353-361. https://www.ncbi.nlm.nih.gov/pubmed/22089499
- Chen JJ, Kardon RH. Avoiding Clinical Misinterpretation and Artifacts of Optical Coherence Tomography Analysis of the Optic Nerve, Retinal Nerve Fiber Layer, and Ganglion Cell Layer. J Neuroophthalmol 2016; 36(4): 417-438. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5113253/