4
Case
Age: 80-year-old white woman
Reason for referral to ophthalmology: Sudden vision loss in the left eye
Past medical history: Hypertension, hypothyroidism
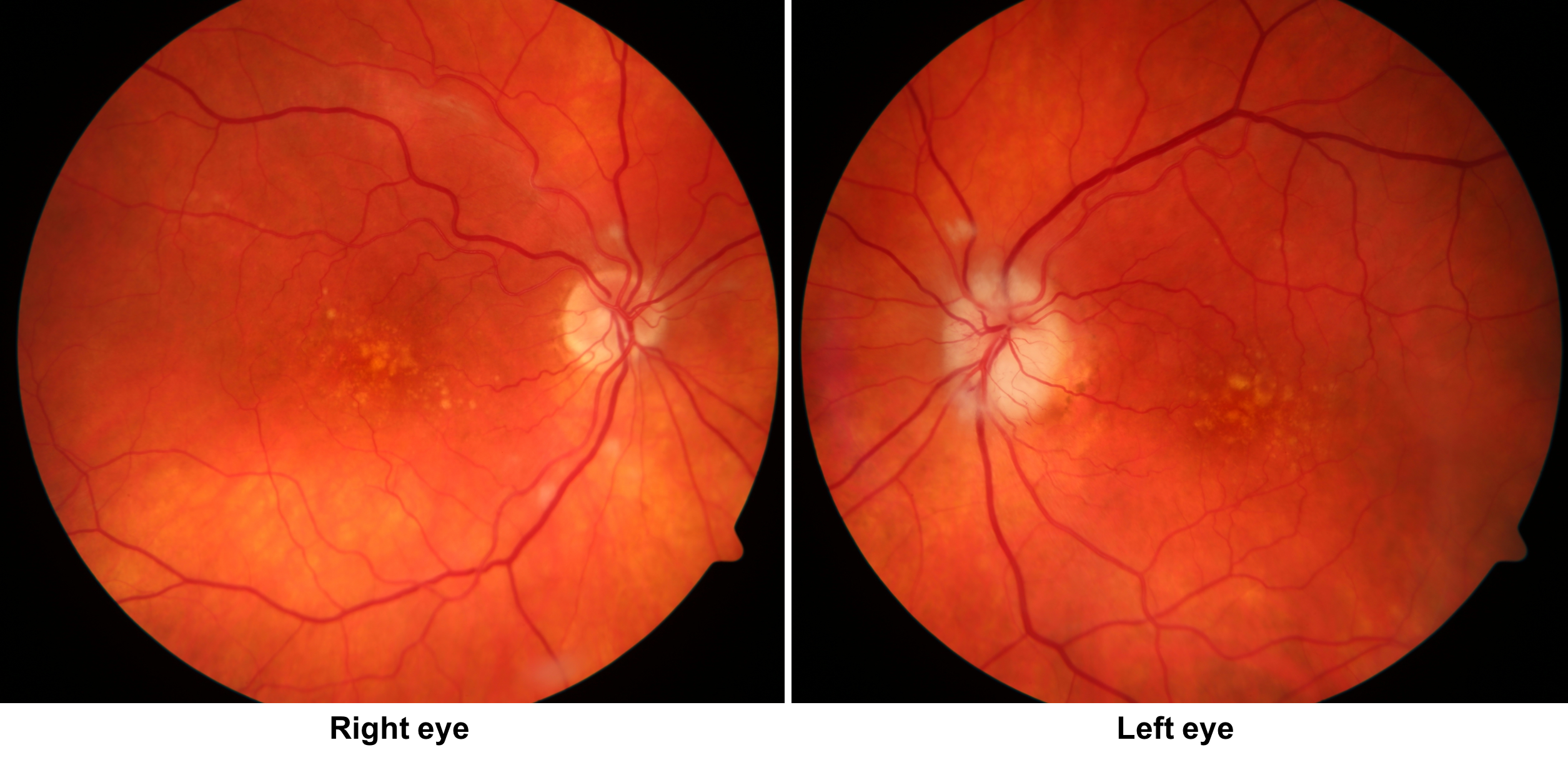
Past ocular history: non-neovascular age-related macular degeneration in both eyes
Medications: Amlodipine, levothyroxine
Habits: Non-smoker and does not drink alcohol
HPI: Yesterday while watching TV, she suddenly lost vision in her left eye. She had an episode of transient vision loss in that same eye 1 week prior, but her vision recovered after 5 minutes and she did not seek medical attention. For the past 4 weeks, she has had a temporal headache, her jaw has felt tired when she chews, and she has felt more fatigued that usual.
She presented immediately to the emergency room after her vision loss and a CT scan of the head without contrast was performed and was normal. An ophthalmology consultation was requested.
Ophthalmological examination:
Blood pressure: 156/86, heart rate 78
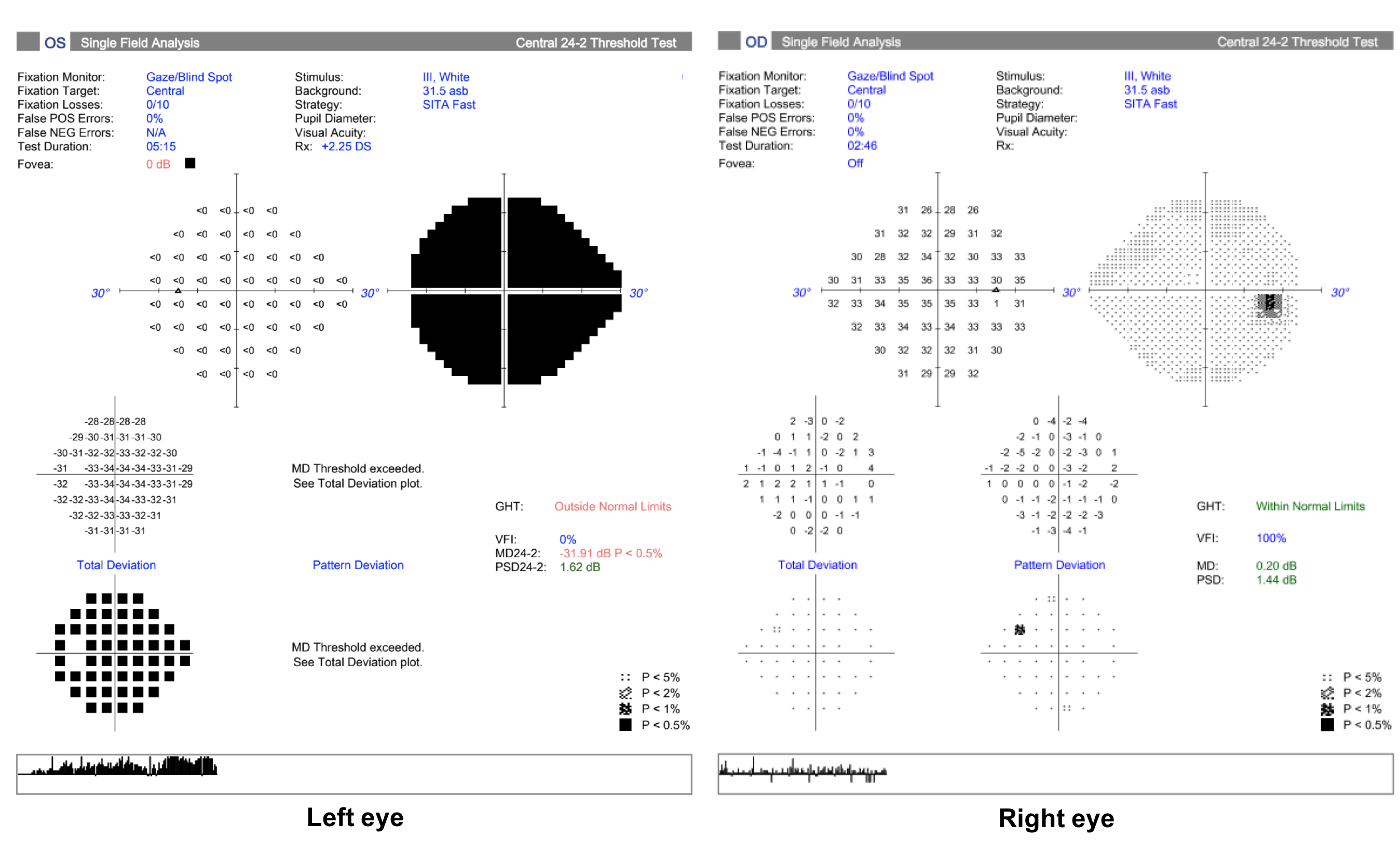
Visual acuity is 20/30 OD and hand motions OS
Pupils are equal sizes and reactive to light, there is a left RAPD
Color vision is 14/14 correct Ishihara plates OD and no control plate in the left eye
Ocular motility and alignment are normal
Slit lamp examination shows mild nuclear sclerotic cataracts in both eyes
Neurological examination is normal
1. Which of the following argues against this patient having non-arteritic anterior ischemic optic neuropathy (NAION)?
- There is pallid disc edema in the left eye
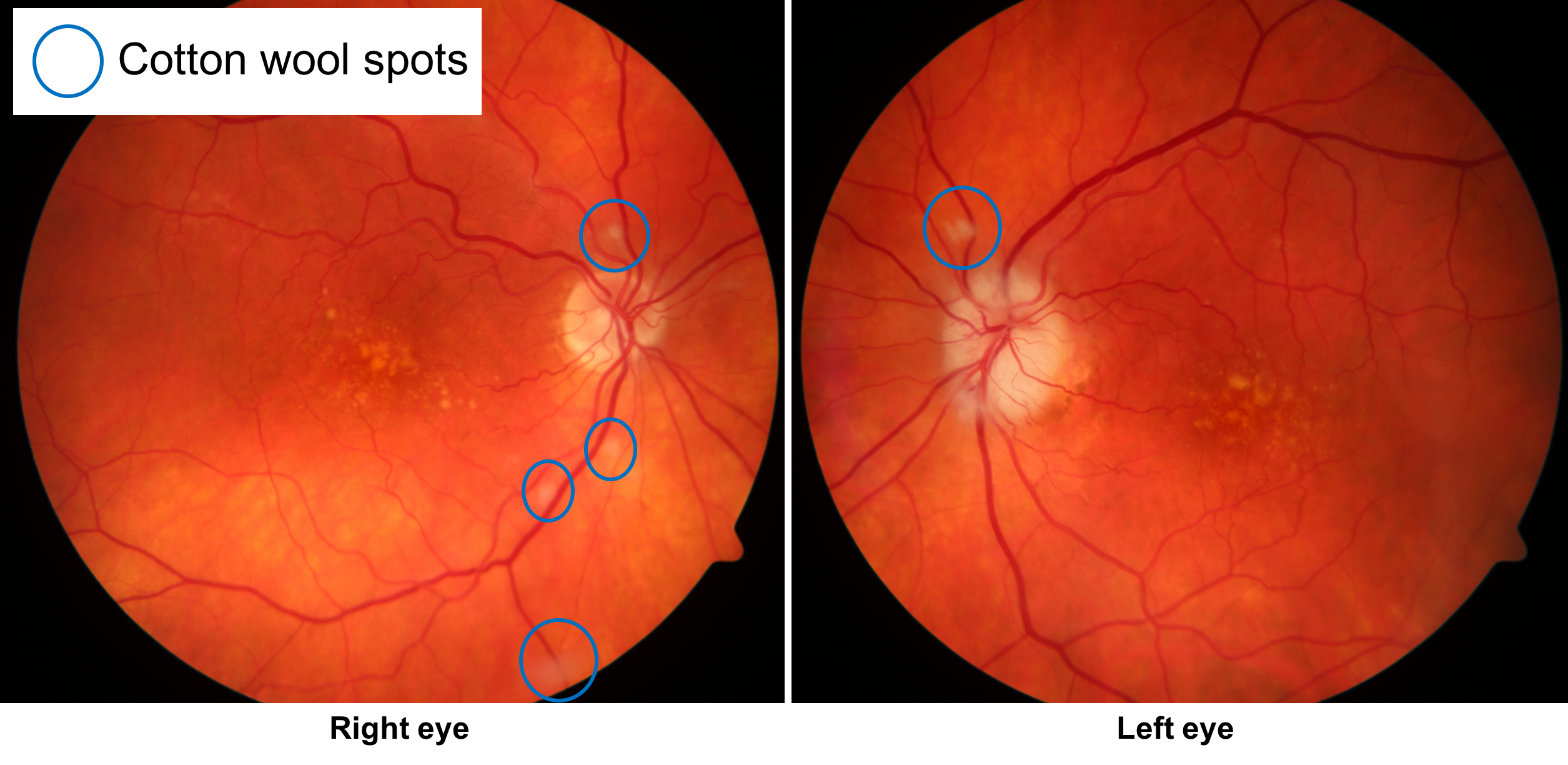
- There are cotton wool spots in the right eye
- She had an episode of transient vision loss preceding the vision loss in the left eye
- She has temporal headache, jaw claudication, and fatigue
- All of the above
1. Which of the following argues against this patient having non-arteritic anterior ischemic optic neuropathy (NAION)? 5. All of the above
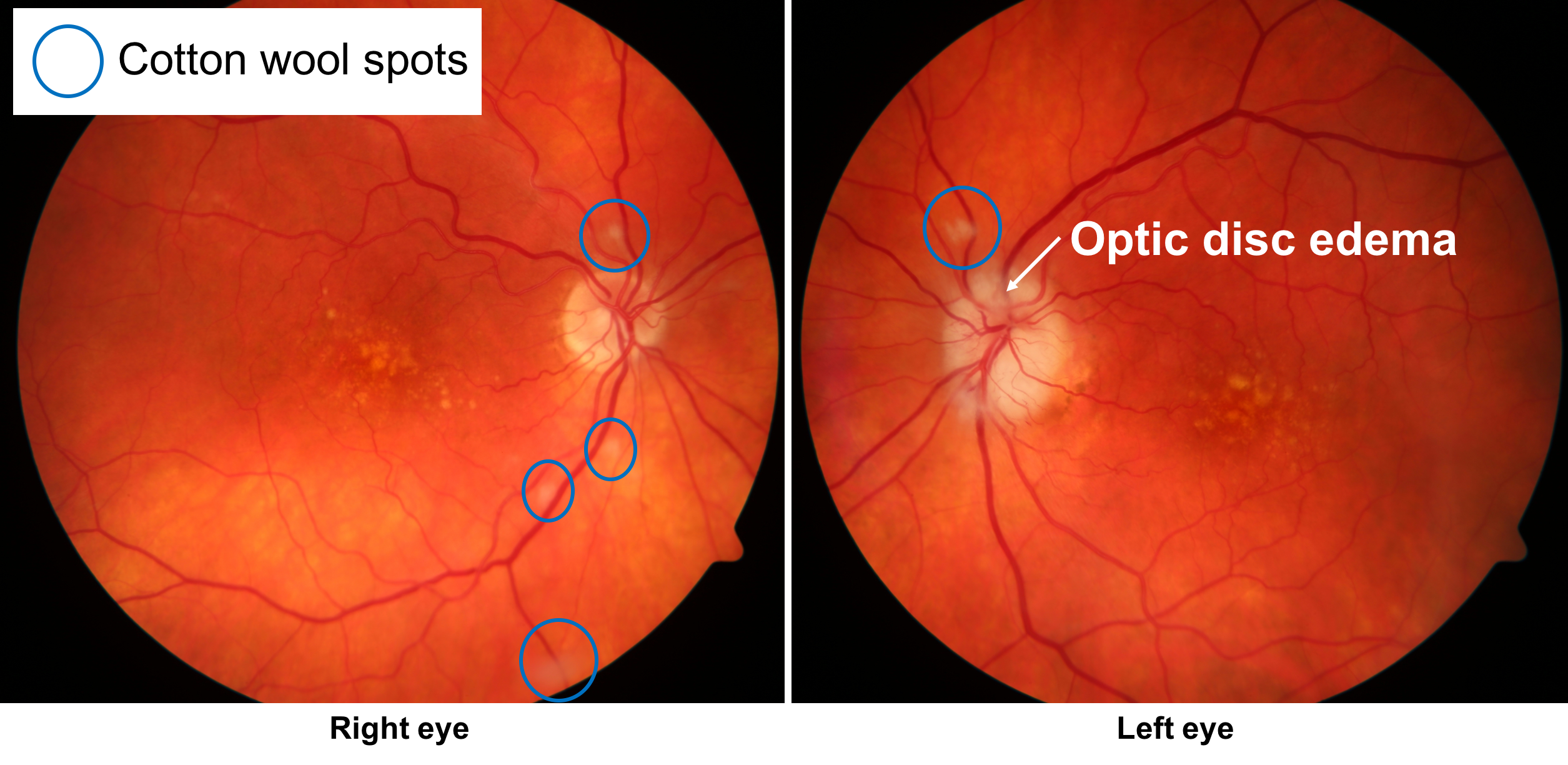
This patient had sudden vision loss in her left eye from an optic neuropathy with optic disc edema, consistent with an anterior ischemic optic neuropathy. Although there is a disc-at-risk in the right eye, there are a number of factors from the history and physical examination that support a diagnosis of arteritic anterior ischemic optic neuropathy (AAION) related to GCA. These include systemic symptoms of temporal headache, jaw claudication and fatigue, cotton wool spots away from the optic discs in both eyes (blue circles shown below), and pallid optic disc edema in the left eye. Vision loss in arteritic anterior ischemic optic neuropathy (AAION) is preceded by transient vision loss in 7-18% of patients, which this patient had.
Clinical Pearl
Systemic symptoms of giant cell arteritis include:
- Headache
- Jaw claudication
- Scalp tenderness
- Weight loss or anorexia
- Malaise, fatigue, or weakness
- Fever
- Muscle aches and morning stiffness (polymyalgia rheumatica)
2. What is the next best course of action for this patient?
- CBC, ESR, and CRP
- MRI of the brain and orbits with contrast
- CT angiogram of the head and neck
- Anticoagulation
2. What is the next best course of action for this patient? 1. CBC, ESR, and CRP
In this elderly patient with a clinical picture consistent with anterior ischemic optic neuropathy and systemic symptoms of GCA, the next best course of action is to obtain bloodwork that includes a CBC, ESR, and CRP, which are markers of systemic inflammation and are often elevated in patients with active GCA.
3. There is a high pre-test probability of GCA in this patient. What implications does this have for interpreting the ESR and CRP?
- There are no implications, the test should be interpreted based on the laboratory cutoffs
- A lower ESR and CRP may still prompt treatment and a temporal artery biopsy
- A higher ESR and CRP are required to initiate treatment and obtain a temporal artery biopsy
- A temporal artery biopsy may still be obtained if the CRP is low, the ESR must be elevated to proceed with further investigations
3. There is a high pre-test probability of GCA in this patient. What implications does this have for interpreting the ESR and CRP? 2. A lower ESR and CRP will still prompt treatment and a temporal artery biopsy
When evaluating a patient for GCA, the inflammatory bloodwork cannot be interpreted in isolation and without considering the pre-test probability of GCA. If there is a high pre-test probability of the disease, lower, or normal results may still prompt treatment and a temporal artery biopsy. If there is a low pre-test probability, then a higher cutoff is used, which may even be above the laboratory guidelines. The ESR and CRP must also be interpreted in the context of the patient’s overall health since other conditions such as infections or cancers can cause these markers to be elevated.
The results of the bloodwork are shown below:
Hemoglobin 132 g/L (normal 135-175g/L)
WBC 7.2 x 109/L (normal 4.0-11.0 x 109/L)
Platelets 456 x 109/L (normal 150-400 x 109/L) High
ESR 21 mm/h (normal is (age+10)/2)
CRP 38 mg/L (normal <5 mg/L) High
4. Based on the patient’s presentation and blood test results, what is the next best course of action for this patient?
- The ESR is normal, no further investigations are required
- Schedule a temporal artery biopsy
- Immediate high-dose intravenous methylprednisolone
- Consult rheumatology the following day
4. Based on the patient’s presentation and blood test results, what is the next best course of action for this patient? 3. Immediate high-dose intravenous methylprednisolone
Based on the history, examination and investigations, there is a high suspicion for GCA in this patient and steroids must be given as soon as possible. Given the high pre-test probability, a normal ESR is not enough to rule out the disease. Any delay in the administration of steroids risks vision loss in the fellow eye. Sometimes an oral dose of prednisone 60 to 80 mg is given immediately since it may take some time for them to get to the emergency room or hospital ward to receive intravenous steroids. Typically, intravenous methylprednisolone 1 g daily for 3 to 5 days is given in this situation when there is ischemic, end-organ damage.
5. What do you expect to happen after steroids are begun in this patient?
- There should be substantial improvement in vision
- Vision will be unchanged but the patient’s systemic symptoms will rapidly improve
- The ESR and CRP will continue to increase for 1 to 2 weeks
- No change in vision or systemic symptoms
5. What do you expect to happen after steroids are begun in this patient? 2. Vision will be unchanged but the patient’s systemic symptoms will rapidly improve
The goal of immediate, high-dose intravenous steroids, is to minimize the risk of systemic complications including vision loss in the fellow eye. After corticosteroids are initiated, systemic symptoms disappear rapidly and dramatically over hours to days in patients with GCA. Improvement in vision occurred in only 4 to 34% of patients in a large series and when it occurs is mild with visual field defects persisting. Inflammatory blood markers will also improve with steroids and this must be kept in mind when evaluating patients for GCA who are already being treated with steroids.
6. What percentage of patients with biopsy-proven GCA have normal ESR?
- < 5%
- 15-20%
- 40-50%
- 60-70%
6. What percentage of patients with biopsy-proven GCA have normal ESR? 2. 15-20%
Although most patients with active GCA have a markedly elevated ESR, the levels can be normal in approximately 15-20% of cases. Therefore, it is important to obtain ESR together with CRP and a platelet count to increase the diagnostic accuracy. The tests must also be interpreted in the context of the pre-test probability of GCA and the patient’s overall health.
Clinical Pearl
The upper limit of normal for ESR is:
- women = (age + 10)/2
- men = age/2
7. What percentage of patients with biopsy-proven GCA and vision loss have normal ESR and CRP?
- < 5%
- 5-10%
- 15-20%
- 40-50%
7. What percentage of patients with biopsy-proven GCA and vision loss have normal ESR and CRP? 1. < 5%
It is unusual, but possible, to have normal ESR and CRP in patients with biopsy-proven GCA. A study that included 177 patients with biopsy-proven GCA found that 7 patients (4%) who had no history of prior corticosteroid use had a normal ESR and CRP. Another study of 119 patients with vision loss from GCA and positive temporal artery biopsies found that the sensitivity of ESR was 76 to 86% whereas the sensitivity of CRP was 97.5%. The sensitivity of ESR and CRP together was 99% and only 1 of the 119 patients (0.8%) presented with a normal ESR and CRP. Therefore, a normal ESR and CRP makes GCA less likely, but does not completely rule it out. In a patient with a high pre-test probability, a temporal artery biopsy may be obtained even in the presence of normal inflammatory markers.
8. What is the most common cause of an extreme elevation of ESR (> 100 mm/h)?
- Giant cell arteritis
- Malignancy
- Infection
- Rheumatoid arthritis
8. What is the most common cause of an extreme elevation of ESR (> 100 mm/h)? 3. Infection
Erythrocyte sedimentation rate is a test that measures how far red blood cells have fallen after 1 hour in a vertical column of anticoagulated blood under the influence of gravity. It therefore takes a minimum of one hour to obtain this test result. The greater the distance the red blood cells fall, the higher the ESR. Normally, red blood cells have some negative charge that causes them to repel other red blood cells. Systemic inflammation increases the presence of positively charged plasma proteins such as fibrinogen and other acute phase reactants that promote erythrocyte aggregation. These aggregates fall further and result in a higher ESR.
An elevated ESR can be seen in a number of conditions, not only GCA. The most common cause of an extreme ESR elevation (> 100 mm/h) is infection, followed by malignant neoplasms, renal disease, and inflammatory disorders. The CRP may also be elevated in these situations and must be taken into account when interpreting the results in a GCA suspect.
9. What percentage of patients presenting with vision loss from GCA have no systemic symptoms?
- < 5%
- 20-25%
- 45-50%
- 70-75%
9. What percentage of patients presenting with vision loss from GCA have no systemic symptoms? 2. 20-25%
The absence of systemic symptoms of GCA such as headache, jaw or tongue claudication, scalp tenderness, fever, myalgias, weight loss and anorexia, does not rule out the disease in patients with vision loss from GCA. In a series of 85 patients with vision loss from GCA confirmed with temporal artery biopsy, 18 (21.2%) had no systemic symptoms and is sometimes referred to as “occult GCA”.
Clinical Pearl
In a patient with vision loss, the absence of systemic symptoms does not rule out giant cell arteritis as the cause.
10. What is the mechanism of jaw claudication in patients with giant cell arteritis?
- Inflammation in the temporomandibular joint (TMJ)
- Referred pain from the temporal artery
- Ischemia of the muscles of mastication
- Ischemia of the Glossopharyngeal nerve
10. What is the mechanism of jaw claudication in patients with giant cell arteritis? 3. Ischemia of the muscles of mastication
Jaw claudication refers to pain and fatigue of the muscles of mastication that improves with rest and is a result of decreased blood flow through the facial branches of the external carotid artery. Jaw claudication is a very specific sign of GCA and is a strong predictor of permanent vision loss and a positive temporal artery biopsy. In a series of 134 patients who underwent temporal artery biopsy, jaw claudication was present in 54% of those with a positive biopsy compared to only 3% of those who had a negative biopsy. Jaw claudication may also be seen in other conditions that result in decreased blood flow through the facial branches of the external carotid artery such as carotid atherosclerosis, amyloidosis, or other vasculitides.
11. Which of the following is the characteristic clinical feature of polymyalgia rheumatica?
- Pain with rotational motion of the shoulders
- Aching and stiffness of the shoulders, hips, neck and torso worse in the morning upon awakening
- Pain and stiffness of the proximal muscles worse at the end of the day
- Distal extremity pain, particularly in the joints, upon awakening in the morning
11. Which of the following is the characteristic clinical feature of polymyalgia rheumatica? 2. Aching and stiffness of the shoulders, hips, neck and torso worse in the morning upon awakening
Polymyalgia rheumatica (PMR) is a rheumatological condition characterized by aching and morning stiffness in the shoulders, hips, neck and torso that is worst in the morning upon awakening. The proximal muscle stiffness can result in difficulties with activities of daily living and patients may also have other systemic symptoms such as malaise, fatigue, low-grade fever, and anorexia. There is a prompt response to low to moderate doses of corticosteroids. Polymyalgia rheumatica is closely linked to GCA as it occurs in approximately 40-50% of patients with GCA and GCA is found in about 15% of patients with PMR. The exact nature of the relationship between GCA and PMR remains unknown. Some patients have signs and symptoms of the two conditions at the same time whereas others develop symptoms of the other over time.
12. Which of the following is a potential cause of vision loss in GCA?
- Cilioretinal artery occlusion
- Central retinal artery occlusion
- Anterior ischemic optic neuropathy
- Posterior ischemic optic neuropathy
- All of the above
12. Which of the following is a potential cause of vision loss in GCA? 5. All of the above
GCA may cause vision loss in a number of different ways. The most common reason is anterior ischemic optic neuropathy, but vision loss may also be due to central retinal artery occlusion, cilioretinal artery occlusion, posterior ischemic optic neuropathy, choroidal ischemia, and optic perineuritis. Certain presentations such as bilateral cilioretinal artery occlusions or a cilioretinal artery occlusion in combination with an optic neuropathy are highly suggestive of GCA.
13. Which of the following less common ophthalmic signs may also be seen with GCA?
- Scleritis
- Tonic pupil
- Orbital inflammation
- Horner’s syndrome
- All of the above
13. Which of the following less common ophthalmic signs may also be seen with GCA? 5. All of the above
Less common ocular manifestation of GCA include ocular inflammation such as scleritis (can be posterior or anterior), orbital inflammation and pupillary abnormalities such as Horner’s syndrome or tonic pupils. Although these are rare presentations, GCA should be considered in elderly patients presenting with these ocular conditions, particularly when there is no other explanation.
14. What histopathological finding from examination of a temporal artery biopsy supports a diagnosis of GCA?
- Fragmentation of the internal elastic lamina
- Prevalence of eosinophils
- Fibrinoid necrosis
- Amyloid deposition
14. What histopathological finding from examination of a temporal artery biopsy supports a diagnosis of GCA? 1. Fragmentation of the internal elastic lamina
The characteristic histopathologic findings of GCA include fragmentation of the internal elastic lamina, giant cells, transmural inflammation, near occlusion of vessel lumen, and focal scarring. The presence of giant cells is not required for diagnosis.
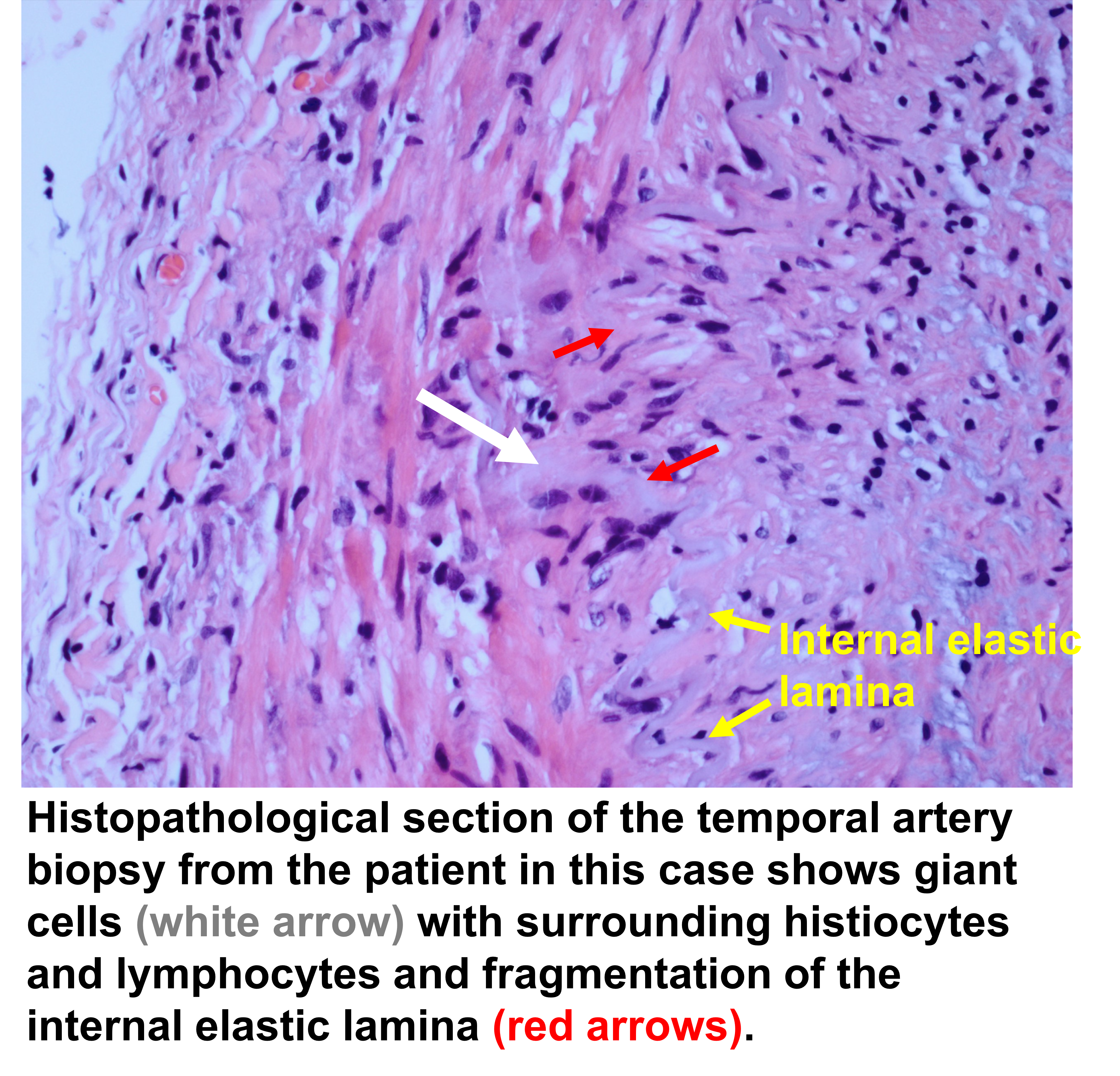
Clinical Pearl
Histopathologic findings that support a diagnosis of GCA:
- Panarteritis consisting of T-lymphocytes, macrophages, epithelioid histiocytes and multinucleated giant cells most pronounced in the media and centered near the internal elastic lamina
- Fragmentation of the internal elastic lamina
- Intimal hyperplasia and near or complete occlusion of the temporal artery lumen
15. An 84-year-old woman presents with vision loss from an anterior ischemic optic neuropathy and has characteristic systemic symptoms of GCA. A temporal artery biopsy is requested but cannot be obtained for at least 3 weeks. Which of the following is the best course of action?
- Hold off on steroid treatment until a biopsy is obtained
- Begin steroids no more than 2 weeks before the biopsy can be obtained
- Start steroids immediately and obtain a temporal biopsy as soon as possible, even if it is after 3 weeks
- Start steroids immediately and do not obtain a temporal artery biopsy since the yield will be low after 3 weeks of treatment
15. An 84-year-old woman presents with vision loss from an anterior ischemic optic neuropathy and has characteristic systemic symptoms of GCA. A temporal artery biopsy is requested but cannot be obtained for at least 3 weeks. Which of the following is the best course of action? 3. Start steroids immediately and obtain a temporal biopsy as soon as possible, even if it is after 3 weeks
Steroids should never be delayed for a temporal artery biopsy in patients who are strongly suspected of GCA since this may result in permanent, bilateral vision loss and other systemic complications. Although the temporal artery biopsy should be obtained as quickly as possible and the yield likely declines with time, histopathological evidence of GCA will persist for months in patients on treatment. In a consecutive case series of 535 patients, the positivity rates of temporal artery biopsies were similar in patients treated for more than 2 weeks compared to those treated for less than 2 weeks. In another study of 183 patients with GCA, histopathological changes of GCA were a similar frequency among patients treated for more than 4 weeks and those treated for 1 to 3 days.
16. If the patient from the original question stem’s temporal artery biopsy is negative for GCA, what is the next best course of action?
- Taper off steroids within 2-3 weeks
- Continue intravenous methylprednisolone 1 g daily for 2-3 months
- Continue steroids but at much lower dose (5-10mg daily) since there is a lower risk of GCA
- Repeat the biopsy on the contralateral side
16. If the patient from the original question stem’s temporal artery biopsy is negative for GCA, what is the next best course of action? 4. Repeat biopsy on the contralateral side
Given the high suspicion of giant cell arteritis, a repeat biopsy should be performed on the contralateral side. It is essential that the biopsy is large enough (2 to 3 cm) so that multiple thin sections can be examined. False negative biopsies may be due to “skip lesions” since GCA may affect the vessel in a discontinuous manner. Given the long-term commitment to steroids in patients with GCA it is important to have tissue confirmation of this diagnosis with a positive biopsy. Steroids should not be rapidly tapered off due to the high-risk of further vision loss and other systemic complications.
Bilateral biopsies are not required in every patient suspected of GCA. If there is a low or intermediate clinical suspicion for giant cell arteritis, a single negative biopsy is usually sufficient to rule out the diagnosis.
Clinical Pearl
Giant cell arteritis may affect the blood vessels in a discontinuous manner (“skip lesions”). This may be the reason for a negative biopsy in a patient with GCA. An adequate biopsy length (2-3 cm) helps ensure that an area of arteritis is obtained.
17. In a patient with suspected GCA, but with negative temporal artery biopsies, what other test can be considered to support the diagnosis?
- Muscle biopsy
- MRA of the aorta and large arteries
- Ultrasound of the orbit
- Skin biopsy
17. In a patient with suspected GCA, but with negative temporal artery biopsies, what other test can be considered to support the diagnosis? 2. MRA of the aorta and large arteries
In a patient suspected of GCA that has negative temporal artery biopsies, the possibility of large vessel involvement should be considered. This can be detected with MRA or CTA of the aorta and large arteries and PET-CT. Patients with large vessel GCA represent a distinct subset of patients compared to those with cranial arteritis with more upper extremity claudication as opposed to cranial symptoms. Although it is debated whether all patients with GCA should be screened for large vessel involvement, it is well recognized that patients with GCA are at higher risk of thoracic and abdominal aortic aneurysms than the general population. Thoracic aortic aneurysms may occur in 7.6 to 11% of patients with GCA, usually within 3 to 5 years of diagnosis.
18. How long is a typical treatment course of steroids for patients with GCA?
- 3-4 months
- 6-8 months
- 1-2 years
- 7-10 days
18. How long is a typical treatment course of steroids for patients with GCA? 3. 1-2 years
A 1-2 year course of steroids is typically required for patients with GCA. Corticosteroids begin to be tapered once there is disease control, meaning systemic symptoms have disappeared, visual symptoms have stabilized and ESR and CRP have been reduced to low levels. Although the tapering process must be individualized to each patient, patients are usually on about 20 mg daily at 6 months and 10 mg daily at 1 year. Any increase in systemic symptoms or laboratory parameters should prompt an increase of prednisone to its last effective dose.
19. Why are cerebral strokes uncommon in patients with GCA?
- Intracranial vessels lose their internal elastic lamina beyond the point of dural perforation
- Cerebral strokes are common in GCA
- Patients with GCA usually have less vascular risk factors compared to the general population
- Patients with GCA are usually on aspirin
19. Why are cerebral strokes uncommon in patients with GCA? 1. Intracranial vessels lose their internal elastic lamina beyond the point of dural perforation
Ischemic stroke has been reported in only 3-4% of patients with GCA and clinical and pathologic findings suggest that these events are due to involvement of extradural vertebral and carotid arteries that create high-grade stenosis. This is because the intracranial arteries lose their internal elastic lamina beyond the point of dural perforation and have very thin walls with much less elastic fibers in the media and adventitia. The internal elastic lamina is the focus of inflammation in GCA.
20. In addition to age, which of the following is a significant risk factor for the development of GCA?
- Hypertension
- Ethnicity
- Smoking
- Vitamin A deficiency
20. In addition to age, which of the following is a significant risk factor for the development of GCA? 2. Ethnicity
The greatest risk factor for GCA is age. It almost never occurs in patients younger than 50 years of age and over 80% of patients are over 70 years of age. Ethnicity is also a major factor and GCA is more common in Scandanavian countries and among Americans of Scandanavian descent. GCA is unusual in Asians, Latinos, Arabs, and African Americans. Woman are more frequently affected than men with a ratio of 3:1, consistent with other rheumatological conditions.
Clinical Pearl
Giant cell arteritis should only be considered in the differential diagnosis for the cause of vision loss in patients over 50 years of age.
Younger patients may also have arteritic vision loss, but this would be from a different vasculitis.
21. Which of the following may be considered as a steroid-sparing agent in the treatment of giant cell arteritis?
- Tocilizumab
- Methotrexate
- Cyclophosphamide
- All of the above
21. Which of the following may be considered as a steroid-sparing agent in the treatment of giant cell arteritis? 4. All of the above
In patients who have developed or are at high risk of developing steroid-related side-effects, other alternatives for treatment include tocilizumab, methotrexate and cyclophosphamide. Tocilizumab (Actemra) is an interleukin-6 receptor antagonist administered via subcutaneous injection, which has been approved by the Food and Drug Administration for the treatment of giant cell arteritis. In a double-blind prospective trial where it was administered weekly or every other week, sustained glucocorticoid-free remission at 52 weeks was significantly higher in the tocilizumab groups compared to placebo. Longer term data are needed to fully assess its efficacy and safety. In this study, there was one episode of vision loss in the the tocilizumab group administered every other week and required additional treatment with prednisone.
22. Which of the following conditions should be considered in the differential diagnosis for a patient with vision loss and systemic symptoms suggestive of GCA?
- ANCA-associated vasculitis
- Infection
- Neoplastic processes
- All of the above
22. Which of the following conditions should be considered in the differential diagnosis for a patient with vision loss and systemic symptoms suggestive of GCA? 4. All of the above
Even in patients with a seemingly classic presentation of GCA, a differential diagnosis must be considered. Other vasculitides including ANCA-associated vasculitis (small vessel vasculitis) or neoplastic processes may cause systemic symptoms that mimic GCA. The latter may cause carcinomatous meningitis and infiltrate around the optic nerves or cause a hyperviscosity syndrome resulting in ischemic vision loss. Infectious processes including invasive infections from an adjacent sinus may also cause systemic symptoms (eg. fever, loss of appetite, headache) and vision loss. This has prompted many neuro-ophthalmologists to obtain neuroimaging in all patient suspected of GCA. This also emphasizes the importance of obtaining a temporal artery biopsy to confirm the diagnosis of GCA since patients are treated with longterm corticosteroids.
Case Summary
This is an elderly woman with severe, sudden vision loss in the left eye with left optic disc edema and cotton wool spots in both eyes. She had systemic symptoms concerning for GCA, a normal ESR, but an elevated CRP and temporal artery biopsy confirmed the GCA diagnosis. She was treated with intravenous methylprednisolone for 5 days followed by oral prednisone (1 mg/kg). The patient followed with rheumatology for ongoing monitoring of her inflammatory markers and medical management. The patient did not have any new vision loss and she discontinued the steroids after 14 months of treatment.
Further reading:
- Dasgupta B, Borg FA, Hassan N, et al. BSR and BHPR guidelines for the management of giant cell arteritis. Rheumatology 2010;49:1594-1597. https://www.ncbi.nlm.nih.gov/pubmed/20371504
- Melson MR, Weyand, Newman NJ, Biousse V. The diagnosis of giant cell arteritis. Rev Neurol Dis 2007;4(3):128-142. http://europepmc.org/abstract/med/17943065
- Kermani TA, Schmidt J, Crowson CS, et al. Utility of erythrocyte sedimentation rate and C-reactive protein for the diagnosis of giant cell arteritis. Semin Arthritis Rheumatol 2012;41(6):866-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3307891/
- Parikh M, Miller NR, Lee AG, et al. Prevalence of a normal C-reactive protein with an elevated erythrocyte sedimentation rate in biopsy-proven giant cell arteritis. Ophthalmology 2006;113:1842-1845. https://www.ncbi.nlm.nih.gov/pubmed/16884778
- Hayreh SS, Podhajsky PA, Zimmerman B. Occult giant cell arteritis: ocular manifestations. Am J Ophthalmol 1998;125(4):521-6. https://www.ncbi.nlm.nih.gov/pubmed/9559738
- Guevara RA, Newman NJ, Grossniklaus HE. Positive temporal artery biopsy 6 months after prednisone treatment. Arch Ophthalmol 1998;116(9):1252-3. https://jamanetwork.com/journals/jamaophthalmology/fullarticle/263486
- Jakobsson K, Jacobsson L, Mohammad AJ, et al. The effect of clinical features and glucocorticoids on biopsy findings in giant cell arteritis. BMC Musculoskelet Disord. 2016;17(1):363. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4997683/
- Salvarani C, Giannini C, Miller DV, Hunder G. Giant cell arteritis: involvement of intracranial arteries. Arthritis Rheum 2005;55(6):985-9. https://www.ncbi.nlm.nih.gov/pubmed/17139651
- Achkar AA, Lie JT, Hunder GG, et al. How does previous corticosteroid treatment affect the biopsy findings in giant cell (temporal) arteritis? Ann Intern Med. 1994;120(12):987. https://www.ncbi.nlm.nih.gov/pubmed/8185147
- Fincher RM, Page MI. Clinical significance of extreme elevation of the erythrocyte sedimentation rate. Arch Intern Med 1986;146(8):1581-3.https://www.ncbi.nlm.nih.gov/pubmed/3729639
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of Tocilizumab in giant-cell arteritis. N Engl J Med 2017;377:317-328. https://www.ncbi.nlm.nih.gov/pubmed/28745999
- Gabriel SE, O’Fallon WM, Achkar AA, et al. The use of clinical characteristics to predict the results of temporal artery biopsy among patients with suspected giant cell arteritis. J Rheumatol. 1995;22(1):93. https://www.ncbi.nlm.nih.gov/pubmed/7699690