9
Case
Age: 23-year-old black woman
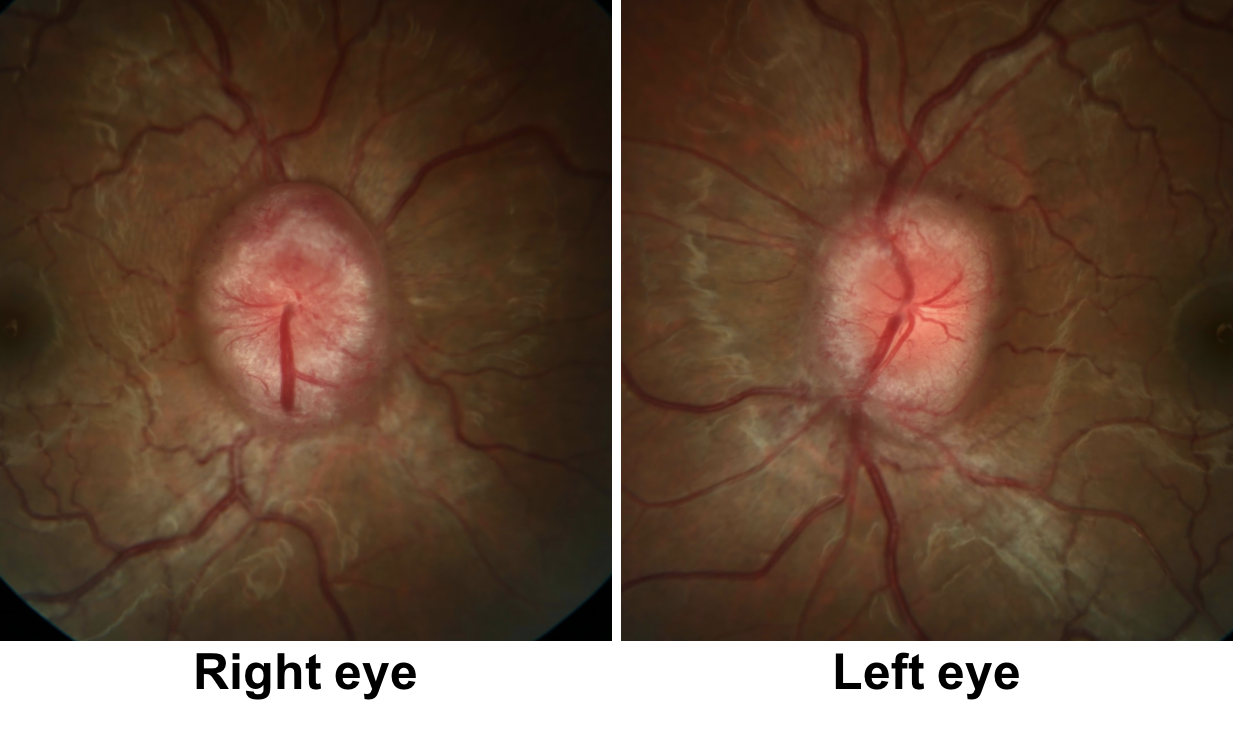
Reason for referral to ophthalmology: Bilateral optic disc edema
Past medical history: None. Body mass index is 38.5 kg/m2
Past ocular history: None
Medications: None
Habits: Smokes 1/2 pack of cigarettes per day and does not drink alcohol
HPI: She went to see an optometrist 3 days ago for a routine eye exam. At that visit, her visual acuity was 20/20 in each eye and she was found to have bilateral optic disc edema. She was urgently referred to the emergency room and an ophthalmology consultation was requested.
After further questioning, she has had mild headaches for the past 4 months that occur on almost a daily basis. She has also noticed transient blurry vision for a few seconds when she stands up from a seated position or bends over. She gained approximately 60 lbs in the past 4 months.
Ophthalmological examination:
Blood pressure: 126/84, heart rate 82
Visual acuity is 20/20 OD, 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision is 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
1. This patient most likely has:
- Bilateral optic neuropathies
- Central retinal vein occlusions
- Bilateral papilledema
- Bilateral infiltrative optic neuropathies
1. The patient most likely has: 3. Bilateral papilledema
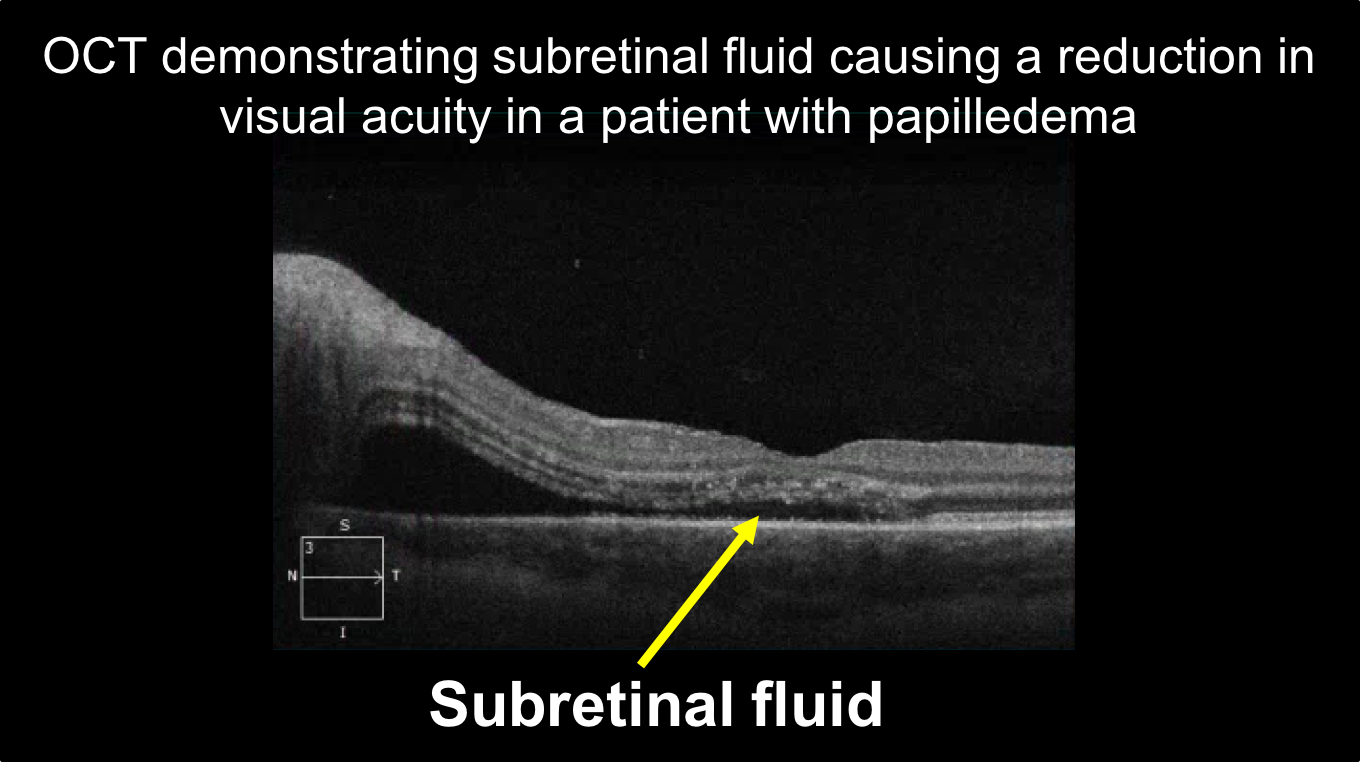
The patient has bilateral optic disc edema and the main question to consider is whether this is a bilateral optic neuropathy or papilledema, which is optic disc edema secondary to elevated intracranial pressure. Papilledema is more likely in this case because the patient has preserved visual function (her visual acuity is normal and her visual field is relatively normal). Bilateral optic neuropathies cause decreased visual acuity, visual field defects or will have a relative afferent pupillary defect. Visual acuity is reduced in papilledema when severe optic disc edema causes sub-retinal fluid in the macula or when the papilledema is long-standing and there is optic atrophy.
Clinical Pearl
Visual function is usually preserved in patients with papilledema. The most common reasons for reduced visual acuity are:
- Severe disc edema causing subretinal fluid (shown below on an OCT of the macula)
- Chronic papilledema leading to optic atrophy
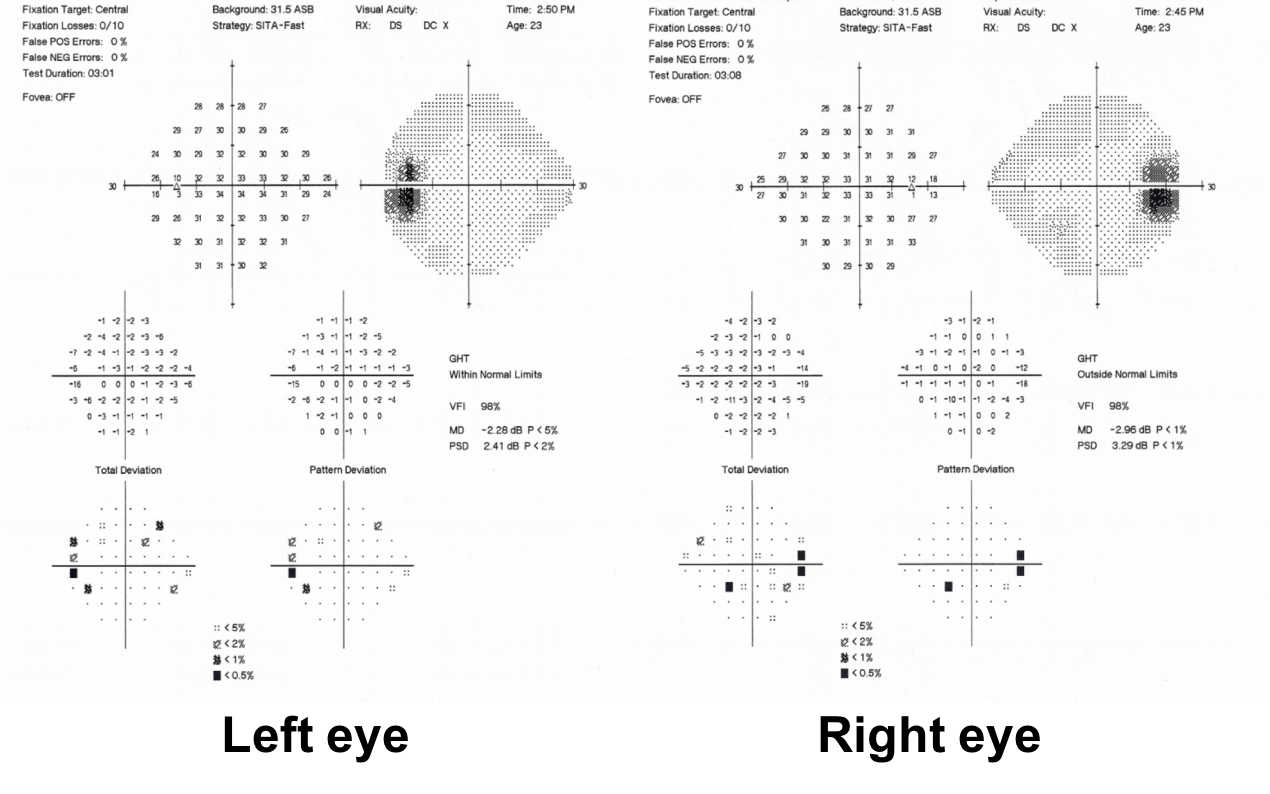
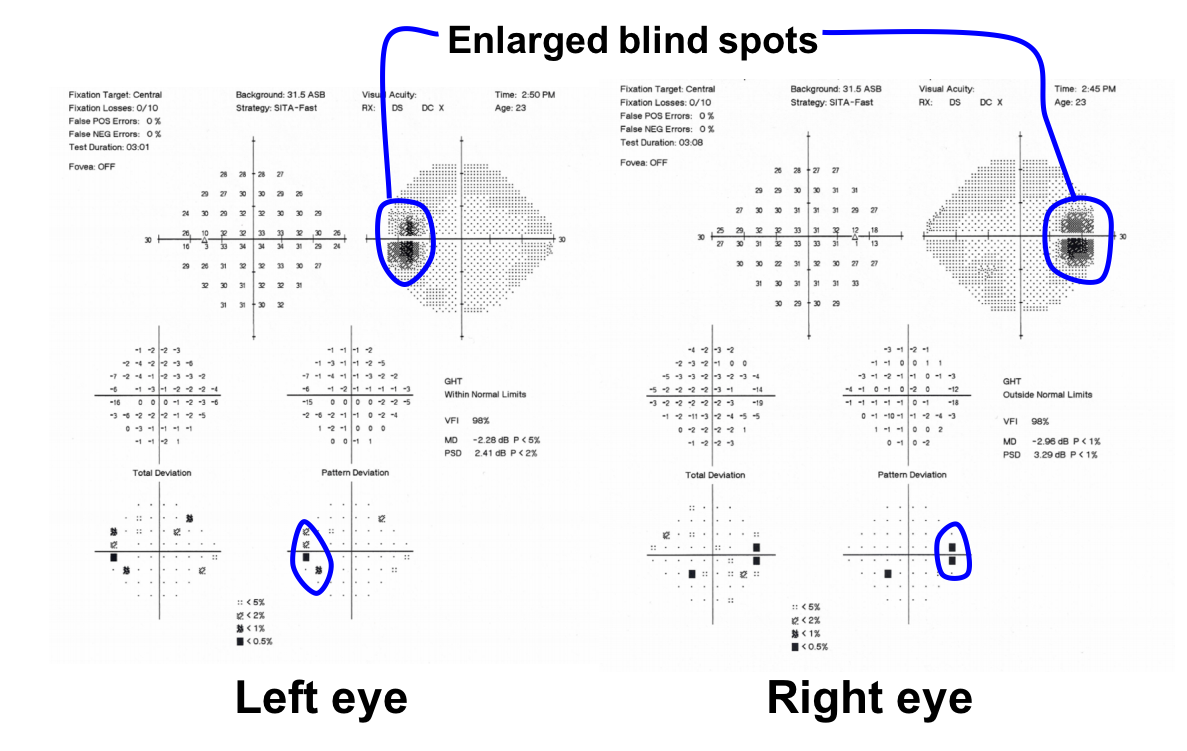
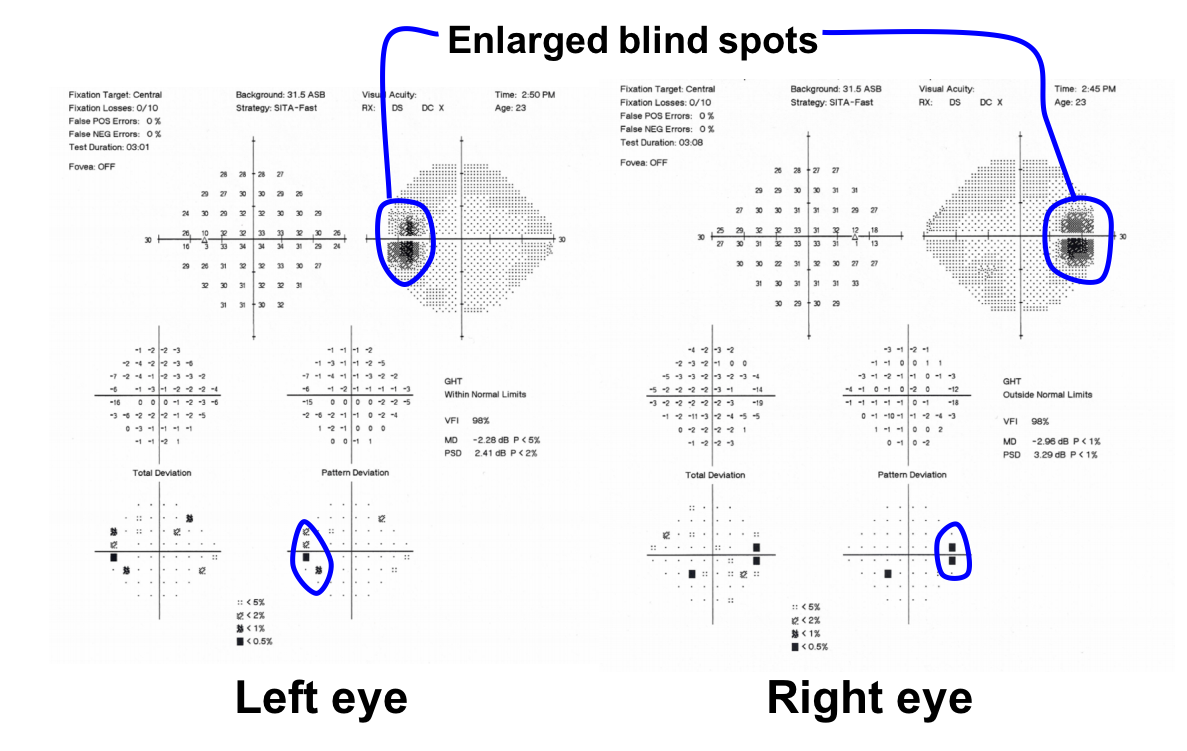
2. Visual field testing shows:
- It is unreliable and we are unable to comment
- Bitemporal hemianopia
- Homonymous visual field defects
- Enlarged blind spots in both eyes
2. Visual field testing shows: 4. Enlarged blind spots
The blind spot is normally positioned about 12 to 15 degrees temporal to the central visual axis. In this patient, the blind spot is mildly enlarged as there are depressed points in the area surrounding the blindspot on both the greyscale and pattern deviation.
3. The most appropriate next step for this patient is:
- Intravenous methylprednisolone followed by an oral steroid taper
- Lumbar puncture with opening pressure recorded
- MRI and MRV of the brain with contrast
- Observation with close follow-up
3. The most appropriate next step for this patient is: 3. MRI and MRV of the brain with contrast
Since the patient likely has papilledema, the most important next step is to ensure that there is no structural lesion causing elevated intracranial pressure. The best neuroimaging modality for this patient is an MRI of the brain with and without contrast. MRV is also included to assess for any venous sinus thrombosis since this may also lead to elevated intracranial pressure.
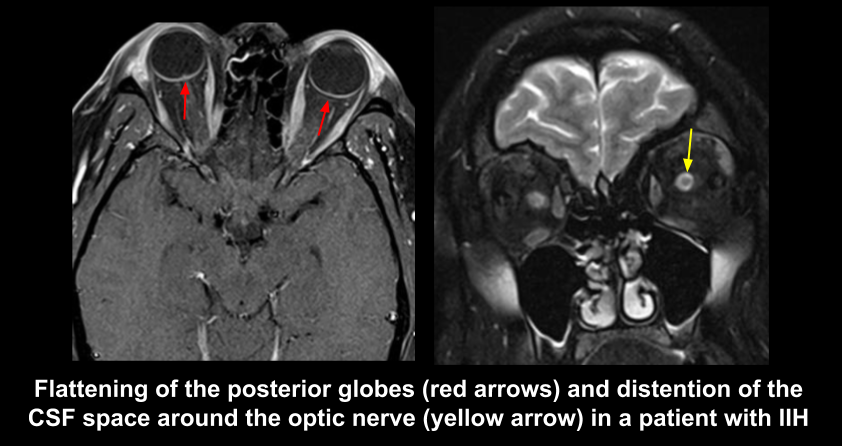
4. Which of the following is true regarding this patient’s MRI shown below?
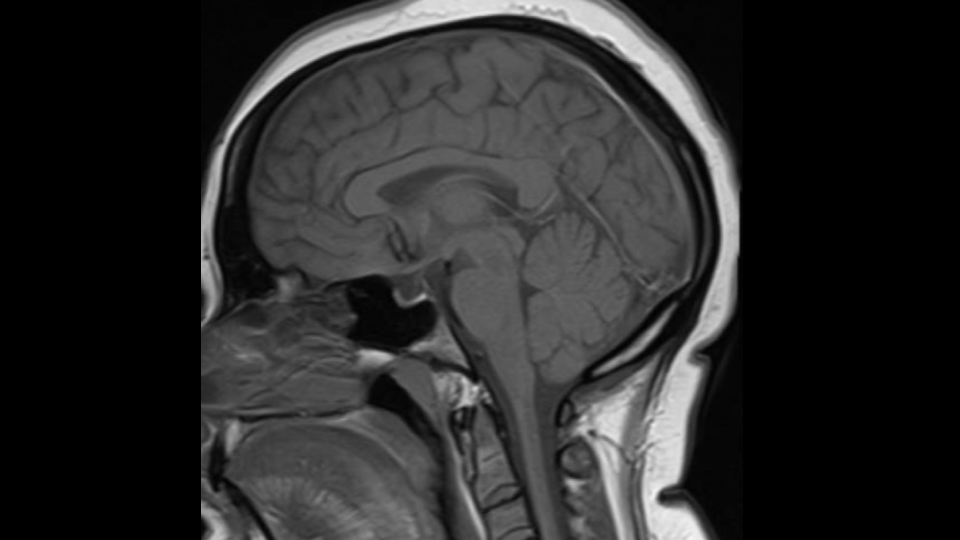
- There are no signs to suggest elevated intracranial pressure
- There is a posterior fossa mass causing obstructive hydrocephalus
- The ventricles are enlarged
- There is an empty sella and low-lying cerebellar tonsils
4. Which of the following is true regarding this patient’s MRI shown below? 4. There is an empty sella and low-lying cerebellar tonsils
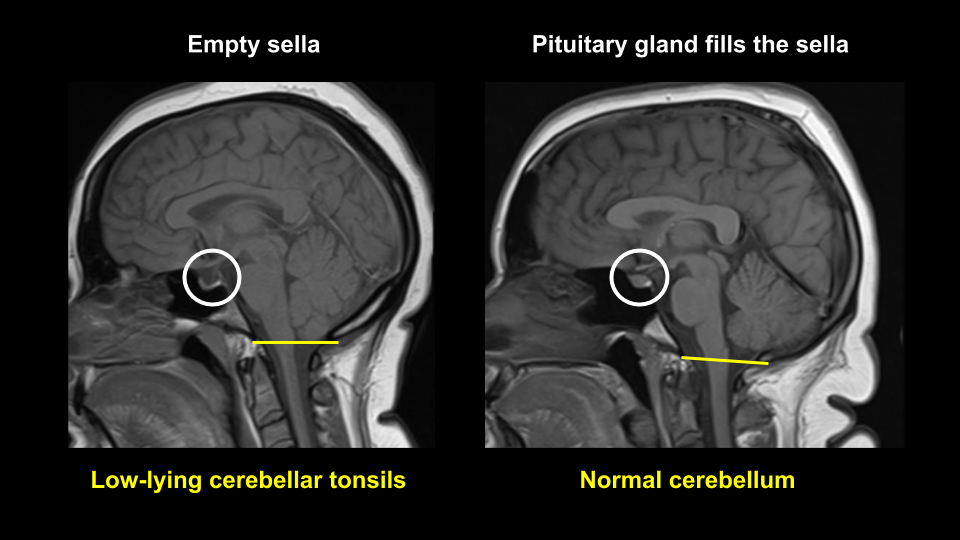
This patient has two signs of chronically elevated intracranial pressure seen on the sagittal T1 MRI image. The first is an empty sella and the second are low-lying cerebellar tonsils (they are just below the foramen magnum shown in the yellow line). Although cerebellar tonsillar herniation is the hallmark of Chiari I malformation, it may also be seen in acquired intracranial hypertension. It is hypothesized that the cerebellar tonsillar descent is due to progressive enlargement of the foramen magnum leading to secondary descent of the tonsils, but this has not been definitively proven.
5. Which of the following is true regarding an empty sella?
- It results in a flattened pituitary gland
- It is the most commonly reported imaging finding in IIH
- Most people with an empty sella do not have IIH
- It tends to persist after successful treatment of IIH, but can completely reverse
- All of the above
5. Which of the following is true regarding an empty sella? 5. All of the above
Empty sella is characterized by herniation of the arachnoid mater and CSF within the sella and is associated with varying degrees of flattening of the pituitary gland. It is thought to occur primarily because of enlargement and remodelling of the sella turcica, but compression also plays a role since an empty sella may partially or completely reverse after successful treatment of IIH. The incidence of a partially empty sella has been reported to be as high as 70 to 95% in IIH patients, but is also seen in 8 to 35% of the normal population, indicating that most people with an empty sella do not have IIH. Its sensitivity for IIH ranges from 65 to 80%.
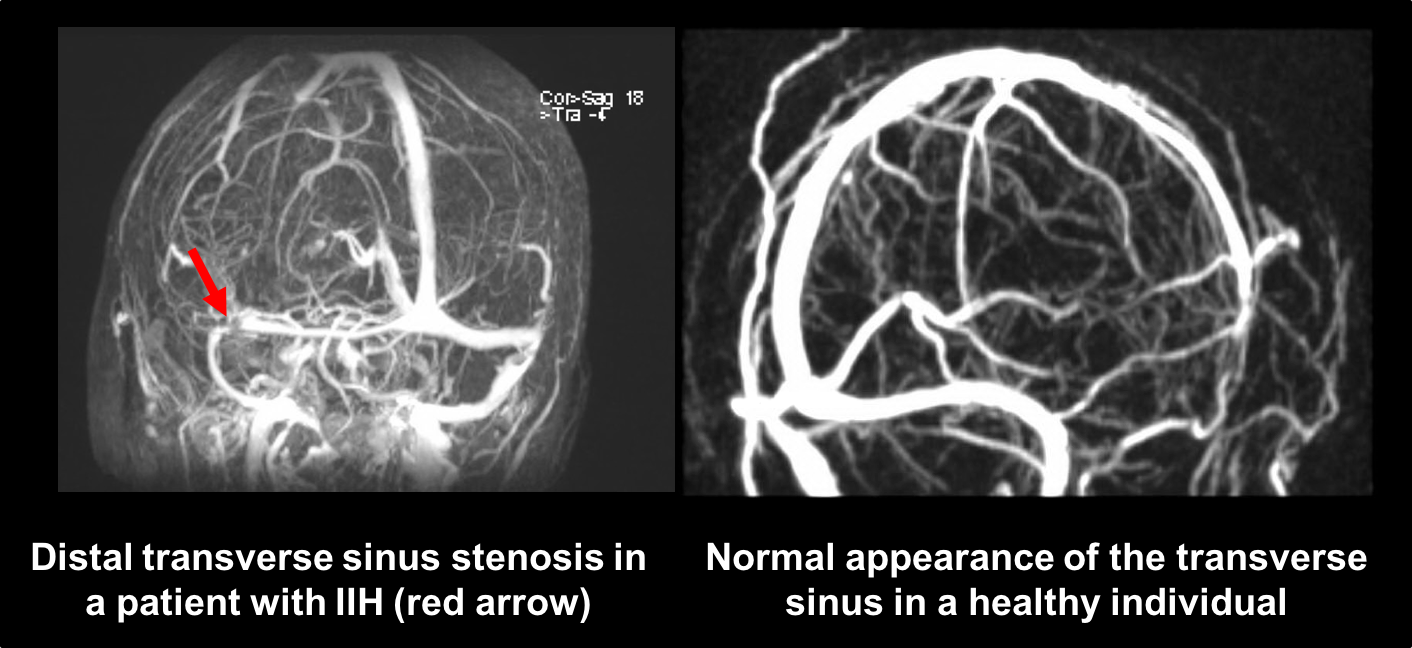
6. Which of the following is true regarding the MRV of this patient shown below?
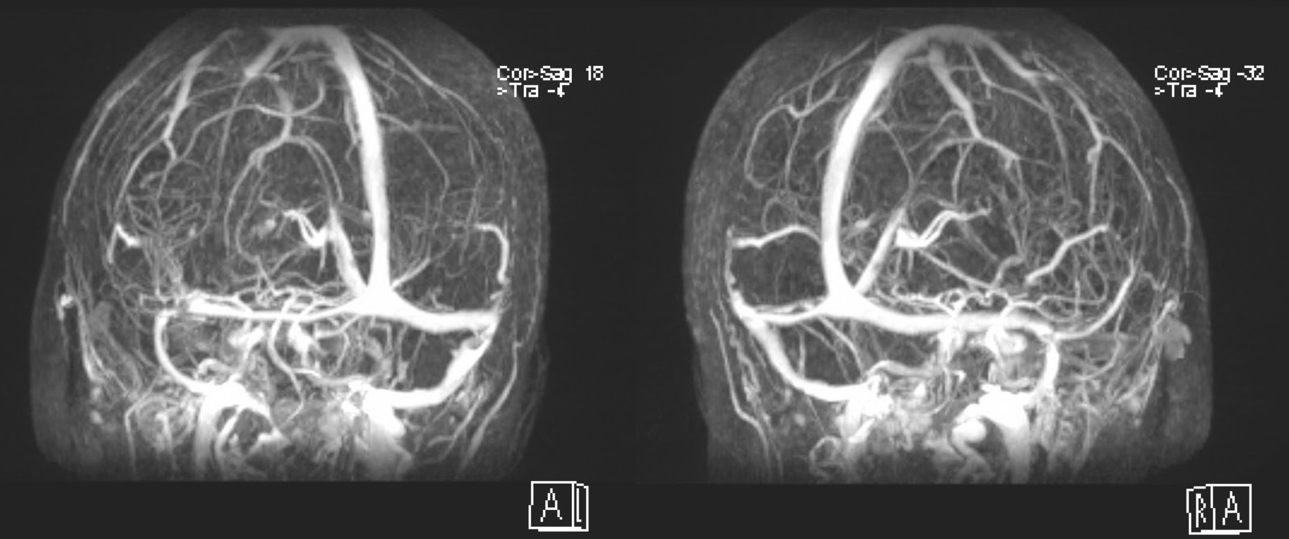
- There is bilateral distal transverse sinus stenosis
- This finding is seen in approximately 50% of IIH patients
- It is a specific finding to IIH and rarely seen in other causes of intracranial hypertension
- It has not been reported as an incidental finding in healthy individuals
- All of the above
6. Which of the following is true regarding the MRV of this patient shown below? 1. There is bilateral distal transverse sinus stenosis
Transverse venous sinus stenosis is a very sensitive finding for IIH with a sensitivity as high as 100%. Although there are varying definitions of transverse sinus stenosis and varying imaging modalities to assess the venous system, it is seen in essentially all IIH cases. However, it may also be rarely found in the normal population and in patients with elevated intracranial pressure from causes other than IIH. It has been proposed that transverse sinus stenosis contributes to the elevated intracranial pressure by impairing venous outflow drainage and furthering the external compression of the transverse sinuses by the high CSF pressure. Stenting of the transverse sinuses has been proposed as a treatment for IIH, but high quality evidence for its use is still lacking.
Clinical Pearl
MRI findings of elevated intracranial pressure include:
- Empty sella
- Flattening of the posterior globes
- Distention of the optic nerve sheaths
- Vertical tortuosity of the optic nerves
- Cerebellar tonsillar herniation
- Bony defects of the skull resulting in spontaneous CSF leaks
- Distal transverse sinus stenosis
7. Which of the following medications are associated with intracranial hypertension?
- Phosphodiesterase-5 inhibitors
- Minocycline
- Anti-hypertensive medications taken at night
- Ethambutol
7. Which of the following medications are associated with intracranial hypertension? 2. Minocycline
Certain medications are associated with intracranial hypertension and these include the tetracycline family of antibiotics (tetracycline, minocycline, doxycycline), vitamin A derivatives (isotretinoin, all-trans-retinoic acid, vitamin A), lithium carbonate, and growth hormone. Every patient suspected of elevated intracranial pressure should be asked about the use of these medications. Phosphodiesterase-5 inhibitors are associated with non-arteritic ischemic optic neuropathy and ethambutol may cause a bilateral optic neuropathy.
8. How can the diagnosis of idiopathic intracranial hypertension be confirmed in this patient?
- Repeat MRI and MRV after initiating treatment
- Intraocular fluid demonstrating normal aqueous composition
- Lumbar puncture demonstrating normal CSF contents and elevated opening pressure
- There is sufficient information to diagnosis IIH at this time
8. How can the diagnosis of idiopathic intracranial hypertension be confirmed in this patient? 3. Lumbar puncture demonstrating normal CSF contents and elevated opening pressure
The modified Dandy criteria is the diagnostic framework used for IIH diagnosis. This patient with papilledema, a normal neurological examination, and normal MRI (apart from signs of chronically elevated intracranial pressure) requires a lumbar puncture with normal CSF composition and an elevated opening pressure for diagnosis.
Clinical Pearl
The diagnostic criteria for IIH (modified Dandy criteria) for patients with papilledema includes:
- Normal neurological examination except for cranial nerve abnormalities
- No evidence of hydrocephalus, mass lesion, structural lesion, and no meningeal enhancement on MRI of the brain with gadolinium for patients in the typical demographic (female and obese). Normal MRI of the brain with contrast and normal MRV is required if not in the typical demographic.
- Normal CSF composition
- Elevated lumbar puncture opening pressure (> 25 cm of water in adults and > 28 cm of water in children)
Modified Dandy criteria: http://n.neurology.org/content/81/13/1159.long
9. Which of the following is expected immediately after the lumbar puncture?
- Improvement in the appearance of the optic discs
- Improvement in symptoms
- Improvement in pituitary function
- Sixth nerve palsy
9. Which of the following is expected immediately after the lumbar puncture? 2. Improvement in symptoms
A common finding in patients with symptomatic elevated intracranial pressure is that their symptoms improve immediately after the lumbar puncture. The appearance of the optic discs is not expected to improve immediately after the lumbar puncture since the mechanism of papilledema is stasis of axoplasmic flow (the movement of organelles and nutrients to and from the neuron’s cell body). This is a metabolic process that takes time (usually at least several days to weeks) to develop and resolve after acute changes in intracranial pressure. The symptoms of intracranial hypertension may recur after the cerebrospinal fluid re-accumulates.
Results from the lumbar puncture:
Opening pressure: 36 cm H2O (Normal < 25 cm H2O)
Nucleated cells: 1
Red blood cells: 2
Protein: normal
Glucose: normal
Given the elevated CSF opening pressure and normal CSF contents, the patient was diagnosed with IIH
10. This patient should be treated with:
- Serial lumbar punctures
- A combination of weight loss and acetazolamide
- Surgical therapy such as an optic nerve sheath fenestration or CSF shunt
- Intravenous methylprednisolone followed by an oral steroid taper
10. This patient should be treated with: 2. A combination of weight loss and acetazolamide
Even a modest amount of weight loss (approximately 6% of body weight) correlates with a reduction of papilledema in patients with IIH. The Idiopathic Intracranial Hypertension Treatment Trial (IIHTT) demonstrated that acetazolamide with a low-sodium weight-reduction diet compared with diet alone resulted in modest improvement in visual function in patients with mild vision loss. The starting dose of acetazolamide is usually 500 mg BID and can be increased to up to 4 g daily. Surgical treatment is reserved for patients with more significant vision loss.
11. What is the most common side-effect reported with acetazolamide in patients with IIH?
- Anemia
- Hypokalemia
- Depression
- Paresthesia
11. What is the most common side-effect reported with acetazolamide in patients with IIH? 4. Paresthesias
In the IIHTT, the most commonly reported side-effects were paresthesias (47.7%), nausea (30.2%), and fatigue (16.3%). The IIHTT used 250 mg tablets of acetazolamide and started at a dose of 500 mg BID, which was increased by 1 tablet per week up to 4 g daily. Thirty-eight out 86 (44.2%) patients in the acetazolamide group tolerated 4 g per day, which was reached at an average of 13 weeks after starting the medication.
12. Which of the following factors from the patient’s history put her at greatest risk for developing IIH?
- Recent weight gain
- Cigarette smoking
- Young age
- Normal blood pressure
12. Which of the following factors from the patient’s history put her at greatest risk for developing IIH? 1. Recent weight gain
Approximately 90% of patients with IIH are women of childbearing age. The most important risk factor is obesity and weight gain, of which this patient has both. Patients of normal weight, especially men, should be thoroughly investigated for secondary causes of intracranial hypertension.
13. Which of the following risk factors does the patient have that puts her at higher risk of a poor visual outcome?
- Female sex
- Black race
- Young age
- Enlarged blind spots
13. Which of the following risk factors does the patient have that puts her at higher risk of a poor visual outcome? 2. Black race
Known risk factors for a poor visual outcome in IIH include male gender, black race, coexisting hypertension, anemia, morbid obesity, and high-grade papilledema. Patients with these factors may require closer follow-up and more aggressive treatment.
14. The most important testing to obtain at follow-up visits are:
- Measurement of visual acuity
- Repeat lumbar punctures
- Formal visual fields
- Assessment of intraocular pressure
14. The most important testing to obtain at follow-up visits are: 3. Formal visual fields
Monitoring of visual function should be performed at each follow-up visit with formal visual fields (Humphrey or Goldmann visual fields). Assessing only the visual acuity is not an acceptable way to monitor visual function in IIH since visual acuity is usually preserved until very late in the disease. New visual field defects such as nasal steps and arcuate defects will be missed unless automated visual fields such as Humphrey visual fields are performed at each follow-up visit.
Clinical Pearl
Characteristic visual field changes seen in patients with papilledema:
- Enlarged blind spot
- Nasal step
- Arcuate scotoma
- Generalized constriction
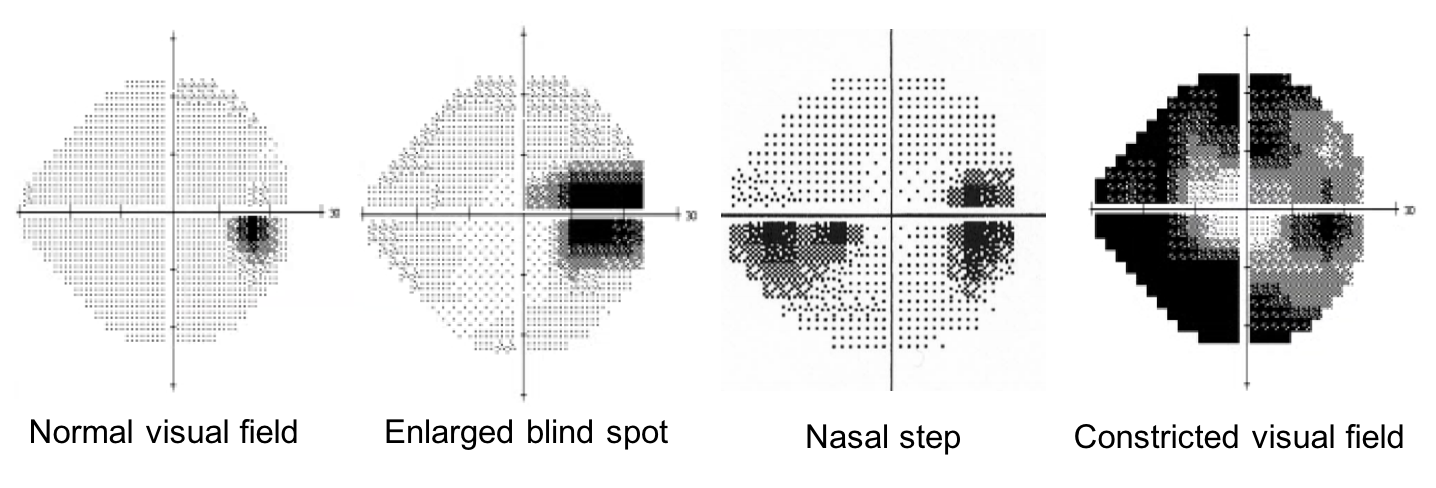
There is relative sparing of central visual acuity until the late stages of the disease.
15. A 30-year old woman develops a fulminant course of IIH with rapid onset of headache and severe vision loss. Her vision loss is progressive despite maximally tolerated acetazolamide. What is the best treatment for this patient to prevent irreversible vision loss?
- Trial of weight loss
- Intravenous methylprednisolone
- Intravenous mannitol
- Optic nerve sheath fenestration or CSF shunt
15. A 30-year old woman develops a fulminant course of IIH with rapid onset of headache and severe vision loss. Her vision loss is progressive despite maximally tolerated acetazolamide. What is the best treatment for this patient to prevent irreversible vision loss? 4. Optic nerve sheath fenestration or CSF shunt
The “fulminant” form of IIH is characterized by an acute presentation with rapidly progressive vision loss. The severe, sudden and rapidly progressive vision loss is likely related to axoplasmic flow stasis and optic nerve ischemia associated with a sudden rise in intracranial pressure. Although no controlled trial has evaluated surgical treatment in IIH, it is generally accepted that surgery, either optic nerve sheath fenestration (ONSF) or CSF shunting, is indicated in cases of progressive vision loss. The type of procedure chosen depends on the local availability of neurosurgeons or ophthalmologists who can perform these procedures. If both procedures are available, CSF shunting is usually chosen if the patient has severe headaches that respond to lumbar punctures and ONSF is preferred when there is severe vision loss from papilledema without other bothersome symptoms.
16. A patient develops fulminant IIH with a rapid onset of symptoms with visual field defects. She is currently 28 weeks pregnant. Which of the following is true regarding acetazolamide use in pregnancy?
- It is category A and there is no risk shown in human controlled studies
- It is category B and there is no risk shown in animal studies
- It is category C and risk has not been ruled out
- It is category D and there is positive evidence of human fetal risk
16. A patient develops fulminant IIH with a rapid onset of symptoms with visual field defects. She is currently 28 weeks pregnant. Which of the following is true regarding acetazolamide use in pregnancy? 3. It is category C and risk has not been ruled out
Managing IIH during pregnancy can be challenging. Treatment is guided by the degree of visual dysfunction and may include the use of acetazolamide, which is a category C medication in the Food and Drug Administration classification of pregnancy risk. This means that animal reproduction studies have shown an adverse effect on the fetus, but there are no adequate, well-controlled studies in humans. Post axial limb malformations have been produced in mice when acetazolamide was administered in high doses (human equivalent of 60-80 mg/kg) during early gestation and a case of sacrococcygeal teratoma has been reported during maternal use of acetazolamide in humans. However, retrospective studies in patients with IIH have found no convincing evidence of adverse effects even when prescribed prior to the 13th week of gestation. Other treatment options during pregnancy include serial lumbar punctures or surgical treatments such as optic nerve sheath fenestration when there is significant visual dysfunction.
17. Which cranial nerve palsies can be seen in patients with idiopathic intracranial hypertension?
- 4th nerve palsy
- 6th nerve palsy
- 7th nerve palsy
- All of the above
17. Which cranial nerve palsies can be seen in patients with idiopathic intracranial hypertension? 4. All of the above
Patients with IIH may complain of diplopia and this is most commonly due to unilateral or bilateral sixth nerve palsies and this usually improves or resolves after lumbar puncture. Less commonly, other cranial nerve palsies (cranial nerves I through VIII) may occur in the setting of IIH and this appears to be more common in prepubertal children.
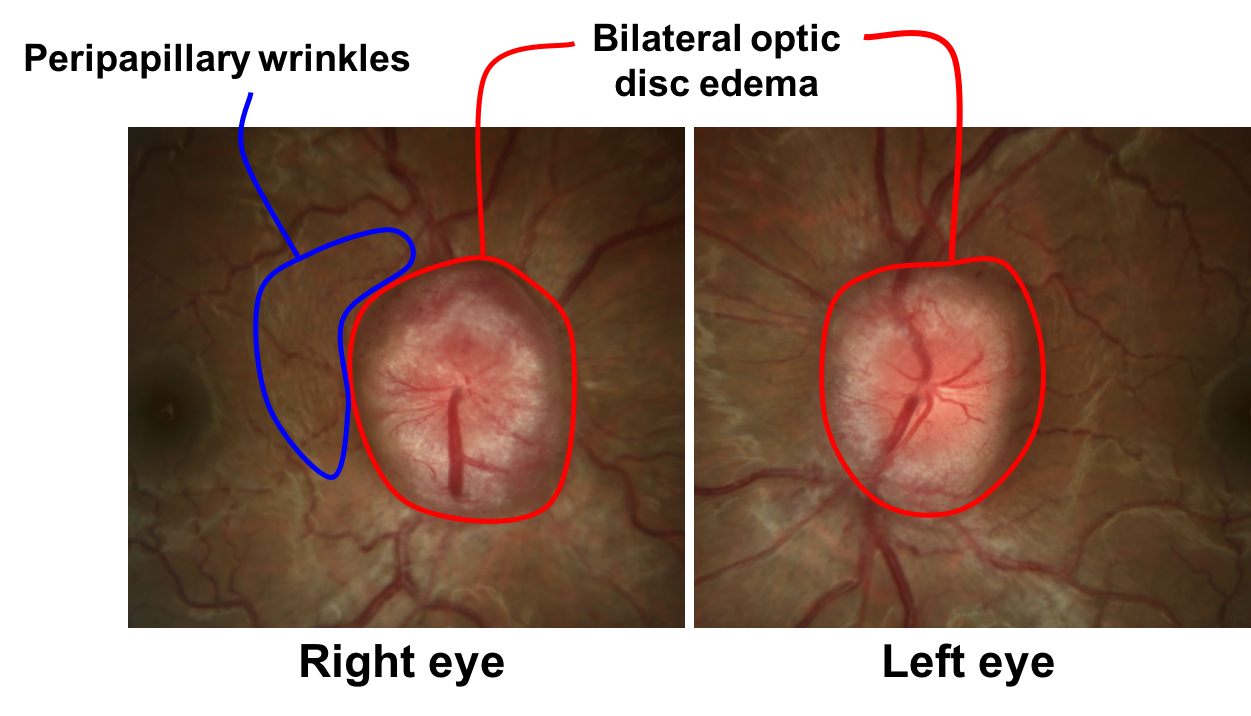
18. A 25-year-old obese woman presents with normal visual function and has the optic nerve appearance shown below. Which of the following is true?
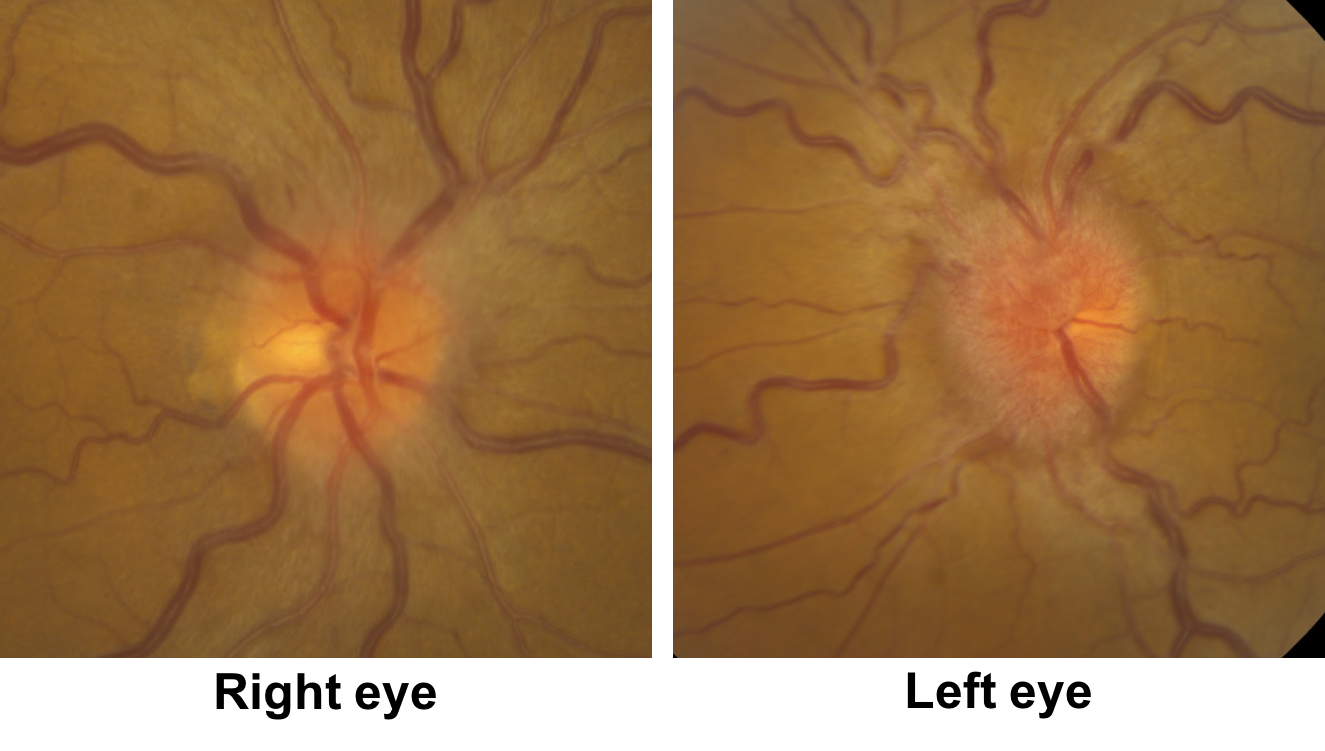
- This is unlikely to be IIH given the asymmetry between the two eyes
- This is unlikely to be IIH given the severity of the optic disc edema in the left eye
- This may represent IIH since asymmetric or even unilateral papilledema may occur
- There is a high probability of a mass lesion ipsilateral to the eye with more severe optic disc edema
18. A 25-year-old obese woman presents with normal visual function and has the optic nerve appearance shown below. Which of the following is true? 3. This may represent IIH since asymmetric or even unilateral papilledema may be seen
This patient likely has papilledema due to the preserved visual function. If there was a mass lesion compressing the left optic nerve and causing elevated intracranial pressure, there should be reduced visual function in the left eye. Although most patients with elevated intracranial pressure have symmetric papilledema, it can be asymmetric or even unilateral. Asymmetric papilledema has been reported to be due to differences in the size of the bony optic canal, with the smaller canal on the side with the lower-grade edema. This results in decreased transmission of the CSF pressure on the side with the smaller canal.
19. An asymptomatic patient is discovered to have possible bilateral optic disc edema. Her optic discs are shown below. What feature of the examination argues in favour of this being true optic disc edema rather than pseudopapilledema.
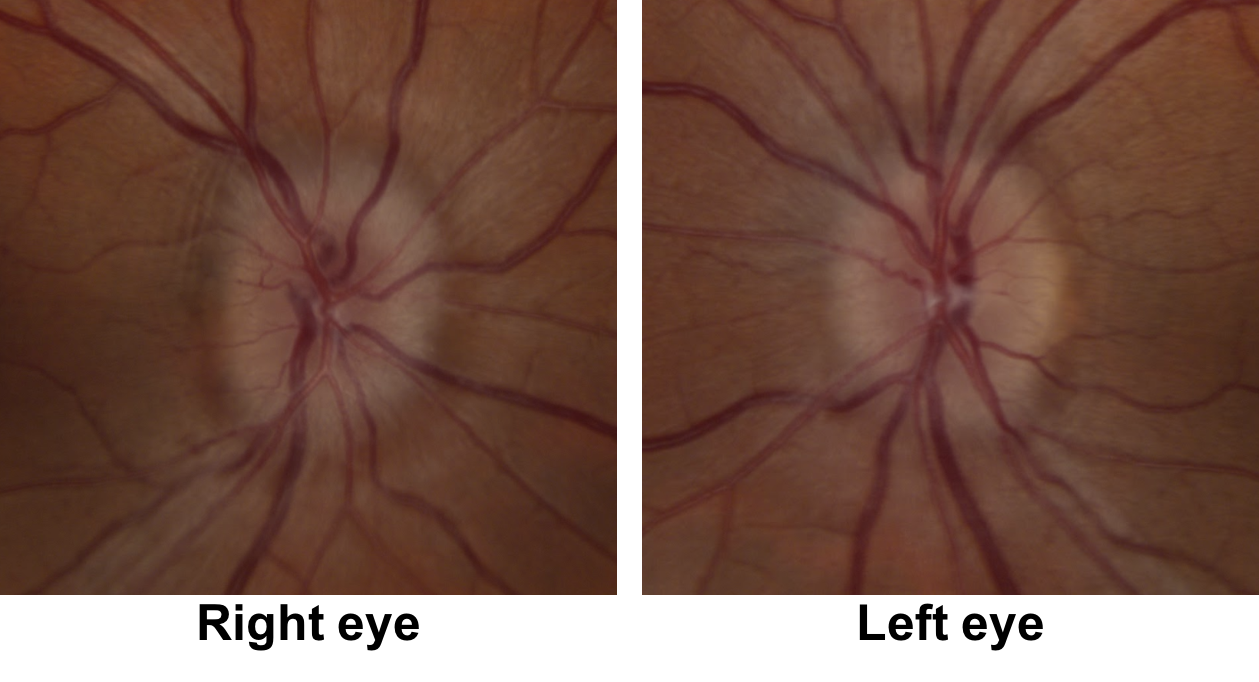
- There is blurring of the optic disc margins
- There are peripapillary wrinkles in the right eye
- There are cotton wool spots in the left eye
- There is a small cup-to-disc ratio in both eyes
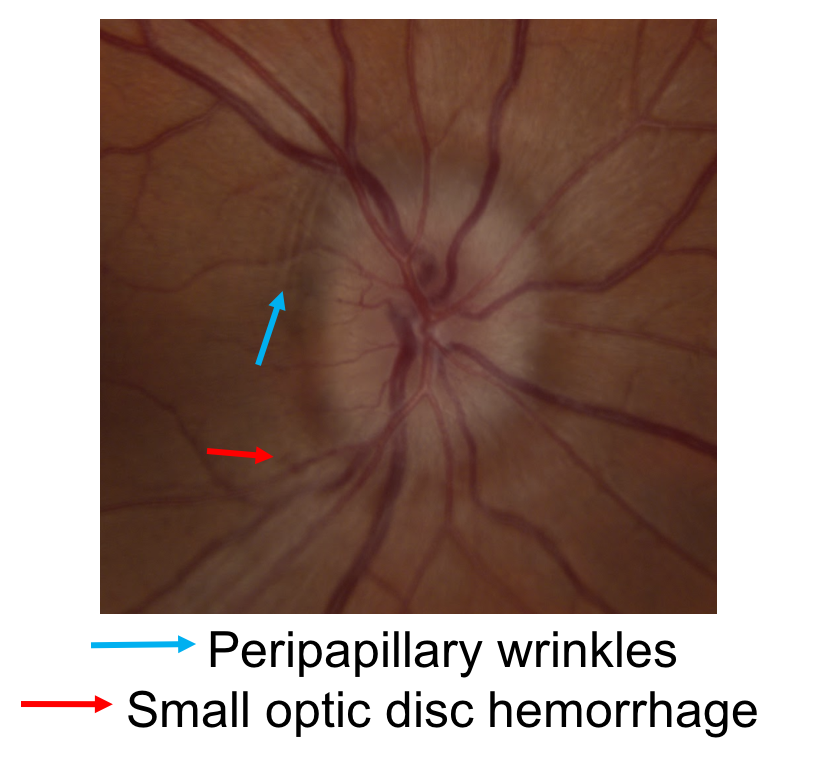
19. An asymptomatic patient is discovered to have possible bilateral optic disc edema. Her optic discs are shown below. What feature of the examination argues in favour of this being true optic disc edema rather than pseudopapilledema. 2. There are peripapillary wrinkles in the right eye
It can be difficult to differentiate true optic disc edema from pseudoedema. There are 2 subtle signs in the right eye of this patient arguing in favour of this being true, acquired disc edema. The first is the presence of peripapillary wrinkles, which are caused by the strain of the acquired disc edema on the peripapillary retina. This leads to the formation of a series of concentric folds and is almost exclusively seen in acquired cases of optic disc edema. The second sign is a small optic disc hemorrhage in the right eye, which also points to this being true optic disc edema, although it can also be seen with optic disc drusen or other congenitally anomalous discs.
20. What is the best way to confirm optic disc edema in the previous patient?
- Presence of spontaneous venous pulsations
- Intravenous fluorescein angiography
- Presence of headache
- MRI of the brain
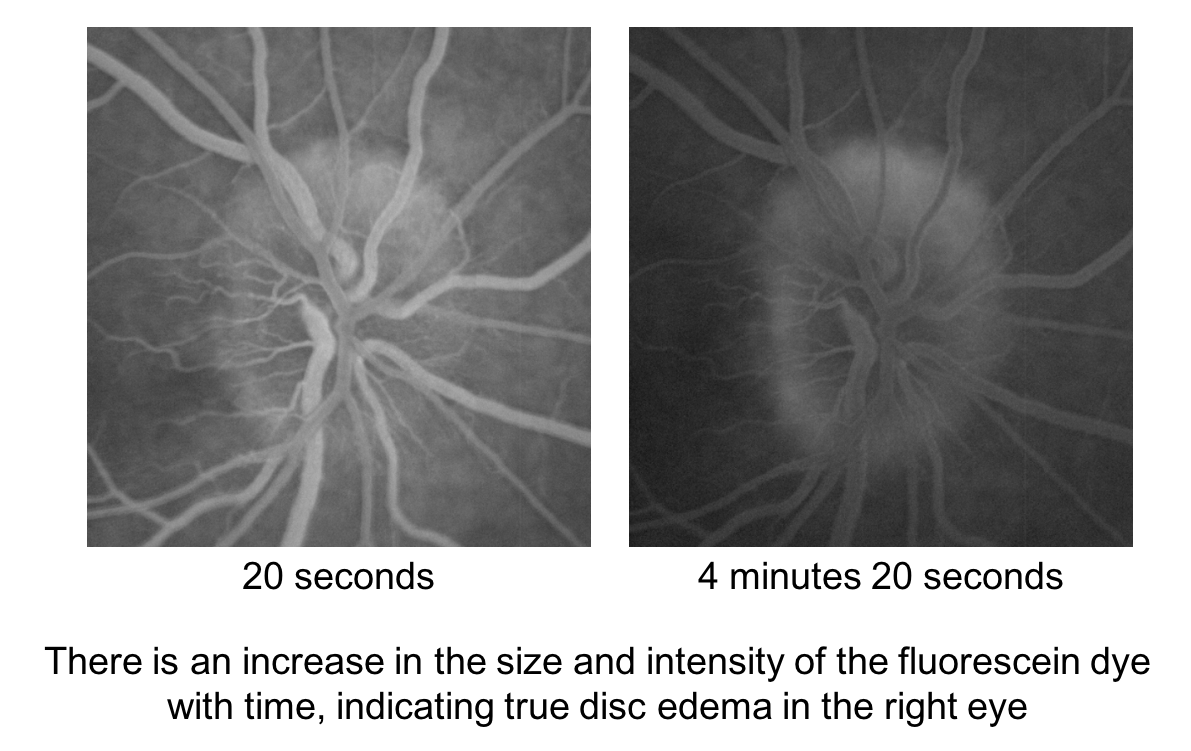
20. What is the best way to confirm optic disc edema in the previous patient? 2. Intravenous fluorescein angiography
Intravenous fluorescein angiography (IVFA) is considered the gold standard for confirming optic disc edema. An edematous optic nerve demonstrates leakage, which is an increase in the size and intensity of the fluorescein dye with time. It is a relatively easy sign to interpret and is shown below. The absence of leakage is very helpful since it confirms that there is no optic disc edema. Rarely, congenitally anomalous optic nerve or optic disc drusen may also demonstrate leakage. Other imaging modalities such as OCT, fundus photography and B-scan ultrasound are not as reliable in differentiating papilledema from pseudopapilledema when compared to IVFA. B-scan ultrasound is useful in detecting cases of optic disc drusen.
21. A patient is referred for possible optic disc edema in both eyes. Spontaneous venous pulsations are observed as the retinal veins cross the optic disc in both eyes. Which of the following is true regarding the intracranial pressure of this patient?
- It is likely elevated at this moment
- It has been elevated for at least 7 days
- It is likely within the normal range at this moment
- It has been within the normal range for at least 7 days
21. A patient is referred for possible optic disc edema in both eyes. Spontaneous venous pulsations are observed as the retinal veins cross the optic disc in both eyes. Which of the following is true regarding the intracranial pressure of this patient? 3. It is likely within the normal range at this moment
Spontaneous venous pulsations are seen as subtle variations in the caliber of the retinal veins as they cross the optic disc and are caused by variations in pressure as the retinal vein traverses the lamina cribrosa. As the intracranial pressure rises to equal the intraocular pulse pressure, the spontaneous venous pulsations cease. This cessation is a sensitive marker of elevated intracranial pressure. However, marked fluctuations of intracranial pressure may occur in patients with intracranial hypertension including patients with IIH. Although the presence of spontaneous venous pulsations during the examination suggests that the intracranial pressure is less than 20 cm of water at that time, this may represent the trough of the pressure wave and does not completely rule out the diagnosis of IIH. Moreover, 10-20% of the normal population does not have spontaneous venous pulsations and their presence is therefore more helpful than their absence.
22. A patient had the sudden onset of the “worse headache of his life” 6 hours ago. He was diagnosed with a subarachnoid hemorrhage and a lumbar puncture showed an opening pressure of 35 cm of water (normal less than 25). What do you expect his optic discs to show at this moment?
- Papilledema
- Pseudopapilledema
- Normal
- Optic atrophy
22. A patient had the sudden onset of the “worse headache of his life” 6 hours ago. He was diagnosed with a subarachnoid hemorrhage and a lumbar puncture showed an opening pressure of 35 cm of water. What do you expect his optic discs to look like at this moment? 3. Normal
Papilledema in patients with an acute elevation of intracranial pressure is an uncommon finding. A previous study examined the optic discs of 37 patients with elevated intracranial pressure from a subarachnoid hemorrhage every 12 to 24 hours for 7 consecutive days. Only 1 patient was found to have papilledema. Papilledema is a time-dependent process that is due to stasis of axoplasmic flow and typically takes at least several days for it to develop in the majority of patients with elevated intracranial pressure. Papilledema may persist for several days after an acute intervention such as a CSF shunt and is not a good indication of shunt function in the early post-operative period.
Case Summary
She had incidentally discovered bilateral optic disc edema with preserved visual function, which was highly suggestive of papilledema. MRI and MRV of the brain were normal apart from signs of elevated intracranial pressure. Lumbar puncture showed an elevated opening pressure and there were normal CSF contents, leading to the diagnosis of idiopathic intracranial hypertension. Acetazolamide was initiated at a dose of 500 mg BID in conjunction with weight loss strategies and a 1 month follow appointment was arranged. She tolerated acetazolamide well and lost 3 lbs at her follow-up appointment. The optic disc edema was stable and her Diamox was gradually increased to 1 g BID. After 10 months, her optic disc edema resolved with the combination of weight loss and Diamox.
Further reading:
-
NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA 2014;311(16):1641-51. https://jamanetwork.com/journals/jama/fullarticle/1861803
-
Bidot S, Saindane AM, Peragallo JH, Bruce BB, Newman NJ, Biousse V. Brain imaging in idiopathic intracranial hypertension. J Neuroophthalmol 2015;35(4):400-11. https://www.ncbi.nlm.nih.gov/pubmed/26457687
-
Biousse V, Bruce BB, Newman NJ. Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry 2012;83(5):488-94. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3544160/
-
Steffen H, Eifert B, Aschoff A, Rolling GH, Volcker HE. The diagnostic value of optic disc evaluation in acute elevated intracranial pressure. Ophthalmology 1996;103(8):1229-32. https://www.ncbi.nlm.nih.gov/pubmed/8764791
-
Falardeau J, Lobb BM, Golden S, Mayfield SD, Tanne E. The use of acetazolamide during pregnancy in intracranial hypertension patients. J Neuroophthalmol 2013;33(1):9-12. https://www.ncbi.nlm.nih.gov/pubmed/22635167
-
ten Hove MW, Friedman DI, Patel AD, Archer I, Wall M, McDermott MP, NORIC Idiopathic Intracranial Hypertension Study Group. Safety and tolerability of acetazolamide in the idiopathic intracranial hypertension treatment trial. J Neuroophthalmol 2016;36(1):13-9. https://www.ncbi.nlm.nih.gov/pubmed/26587993
-
Thambisetty M, Lavin PJ, Newman NJ, Biousse V. Fulminant idiopathic intracranial hypertension. Neurology 2007;68:229-232. https://www.ncbi.nlm.nih.gov/pubmed/17224579
-
Carta A, Favilla S, Prato C, et al. Accuracy of funduscopy to identify true edema versus pseudoedema of the optic disc. Invest Ophthalmol Vis Sci 2012;53:1-6. https://iovs.arvojournals.org/article.aspx?articleid=2126594