24
Case
Age: 50-year-old man
Reason for referral to ophthalmology: Dilated pupil
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and does not drink alcohol
HPI: A few months ago, he started to notice that his pupil sizes were different and this was more pronounced in the light. His co-workers also started to comment on the difference. He went to see an optometrist and his right pupil was not reactive to light and he was then referred immediately to the emergency room. A CT scan of the head without contrast was normal and an ophthalmology consultation was requested.
Ophthalmological examination:
Blood pressure: 126/85, heart rate 72
Visual acuity: 20/20 OD, 20/20 OS
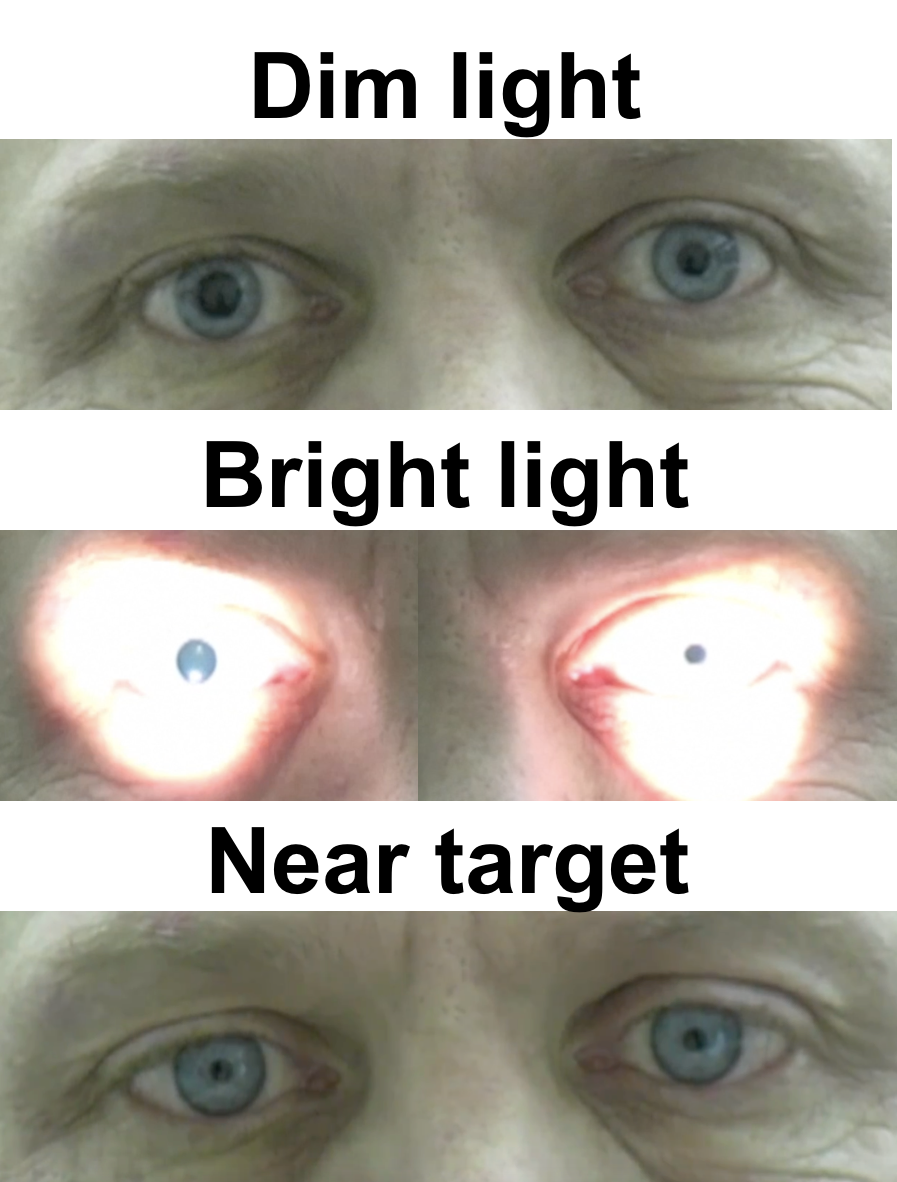
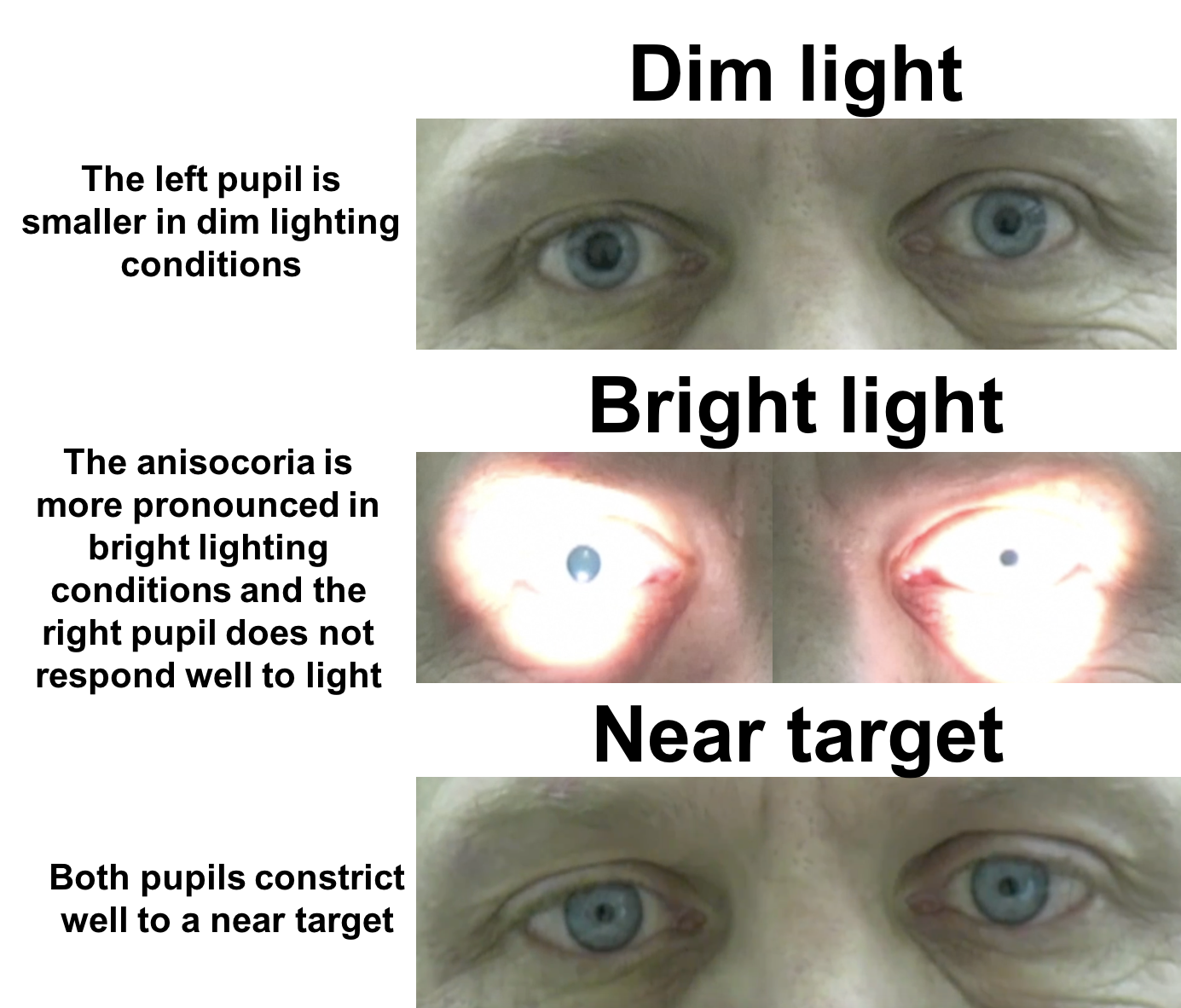
Pupils examination is shown below.
Color vision: 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal. The patient is orthophoric primary position, left, right, up and down gaze.
Neurological examination is otherwise normal
1. What causes anisocoria that increases in bright light?
- Third nerve palsy due to a compressive lesion
- Pharmacological mydriasis
- Adie’s tonic pupil
- All of the above
1. What causes anisocoria that increases in bright light? 4. All of the above
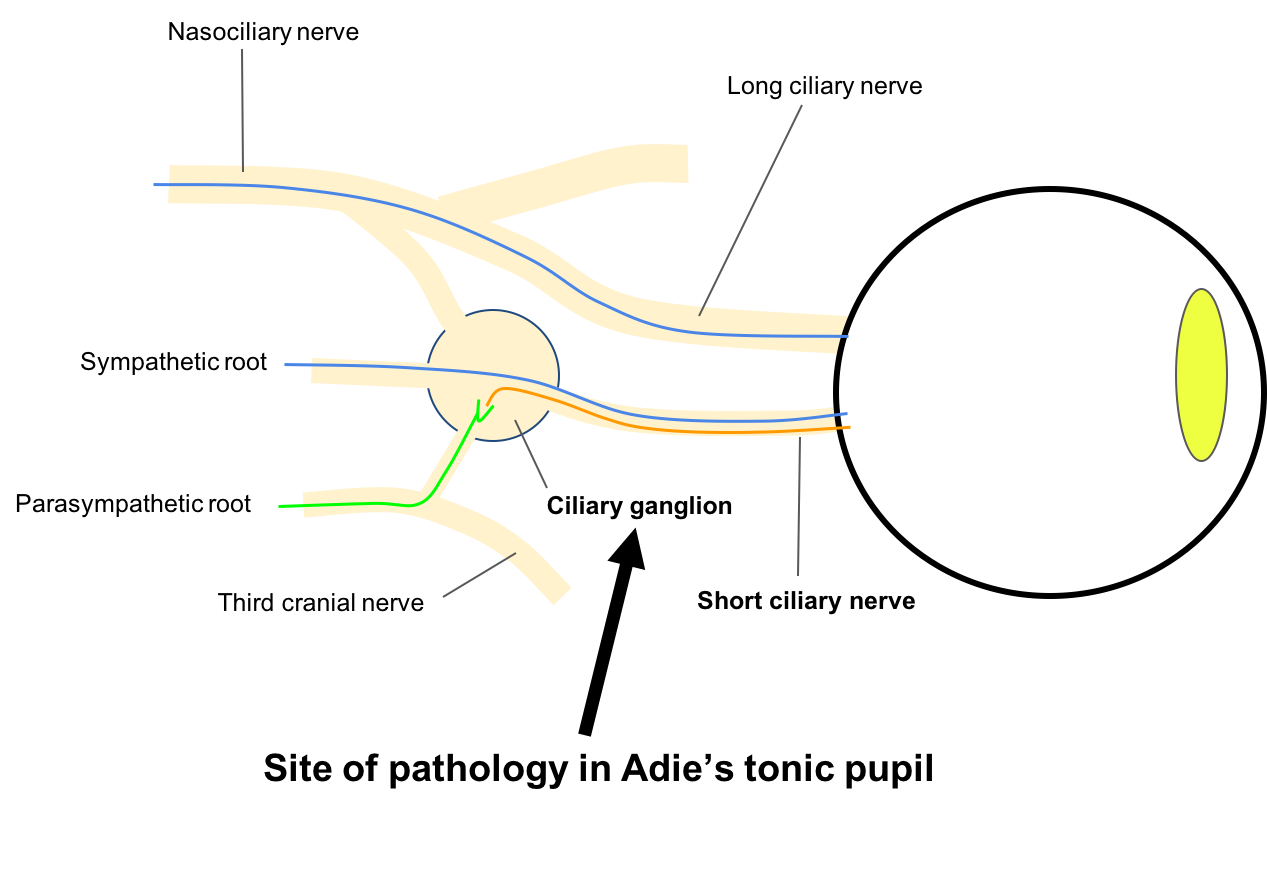
When anisocoria (different pupil sizes) increases in bright light, the larger pupil is abnormal. The parasympathetic pathway for pupillary constriction begins in the Edinger-Westphal nucleus in the midbrain and continues via the 3rd cranial nerve to the ciliary ganglion. Post-ganglionic impulses are carried through the short ciliary nerves to the iris sphincter. The differential diagnosis for the abnormal, larger pupil is summarized below.
Clinical Pearl
The differential diagnosis for anisocoria that is greater in the light includes:
- Pre-ganglionic lesions: 3rd nerve palsy (compression, inflammation, trauma)
- Post-ganglionic lesions: Tonic pupil (Adie’s tonic pupil, iatrogenic damage to posterior ciliary nerves)
- Pharmacological mydriasis: anti-cholinergic or sympathomimetic drugs
- Direct damage to the iris sphincter: intraocular surgery, trauma, uveitis, ischemia
2. This patient does not have pharmacological mydriasis because:
- The left pupil constricts to light
- The left pupil constricts to a near target
- The right pupil constricts to a near target
- The right pupil does not constrict to light
2. This patient does not have pharmacological mydriasis because: 3. The right pupil constricts to a near target
The patient has anisocoria that is worse in the light, indicating that the larger, right pupil is abnormal. The right pupil does not react to light, but constricts to a near target. If the patient had pharmacological mydriasis, the pupil should remain dilated in response to both light and a near target.
3. Which of the following is true regarding further investigations?
- The patient should have an urgent CTA to rule out a compressive aneurysm causing a 3rd nerve palsy
- The patient should have an MRI of the brain to rule out a brainstem lesion
- The patient should have an MRA of the head and neck to rule out a carotid dissection
- No neuroimaging is required
3. Which of the following is true regarding further investigations? 4. No neuroimaging is required
The patient has an isolated dilated pupil with full extraocular movements and without ptosis. A 3rd nerve palsy caused by an intracranial aneurysm can cause a fixed, dilated pupil, but there will be other signs such as ptosis or at least some limitation of extraocular movements. Although a dilated pupil may be a harbinger of a compressive lesion of the 3rd cranial nerve in an uncooperative or comatose patient, it is extremely unlikely in an alert patient with normal ocular alignment, motility, and eyelid position. Thus, a patient with an isolated dilated pupil and normal extraocular motility does not need to be investigated for a 3rd nerve palsy.
4. What would be expected if Pilocarpine 0.1% was instilled in both eyes?
- No response in either eye
- Exaggerated constriction in the right pupil
- Exaggerated constriction in the left pupil
- Similar degree of constriction in both eyes
4. What would be expected if Pilocarpine 0.1% was instilled in both eyes? 2. Exaggerated constriction in the right pupil
This is an otherwise healthy patient that has a right tonic pupil without an identifiable cause, which is called Adie’s tonic pupil. It is a result of injury to the ciliary ganglion in the retrobulbar space. Within a few days of injury, cholinergic supersensitivity develops and the pupil becomes very sensitive to dilute pilocarpine. Testing with dilute pilocarpine is a useful way to differentiate direct damage/dysfunction of the iris sphincter (cholinergic under-sensitivity) from other post-ganglionic lesions. Only the latter will demonstrate cholinergic supersensitivity and have an exaggerated constriction with dilute pilocarpine.
5. What should be seen with slit lamp examination of the right eye?
- Intraocular inflammation
- Posterior subcapsular cataract
- Corneal guttata
- Segmental contraction of the iris sphincter
5. What should be seen on slit lamp examination of the right eye? 4. Segmental contraction of the iris sphincter
Adie’s tonic pupil is caused by acute denervation of the ciliary body and iris sphincter. Under the slit lamp, segmental contractions of the iris sphincter are seen in about 90% of Adie’s pupils and are due to contraction of the remaining areas of normally innervated iris sphincter. The denervated areas appear flat and do not respond to light.
6. Why may a patient with Adie’s tonic pupil have trouble with reading vision in the acute stage of this condition?
- Excess light entering through the pupil
- Accommodative paresis
- Increased constriction of the left pupil
- Iris transillumination defects
6. Why may a patient with Adie’s tonic pupil have trouble with reading vision in the acute stage of this condition? 2. Accommodative paresis
In the acute stage of Adie’s pupil, there is moderate to severe paresis of accommodation due to the loss of parasympathetic fibers innervating the ciliary muscle. This will improve over several months as the ciliary muscle becomes reinnervated. A near add in glasses may be helpful during this time.
7. Why is there light-near dissociation in Adie’s tonic pupil?
- Aberrant reinnervation
- There is a tactile stimulus involved in accommodation
- There is bilateral innervation of accommodation from the cerebral cortex
- There are equal number of fibers innervating the ciliary muscle and iris sphincter
7. Why is there light-near dissociation in Adie’s tonic pupil? 1. Aberrant reinnervation
After the initial damage to the ciliary ganglion, the surviving fibers in the ciliary ganglion start to regrow. Because the fibers to the ciliary muscle greatly outnumber those to the iris sphincter (97:3), there is a greater chance of survival of the fibers to the ciliary muscle. These fibers will appropriately reinnervate the ciliary muscle but also inappropriately re-innervate the iris sphincter, resulting in greater pupillary constriction with accommodation.
8. Where is the ciliary ganglion located?
- Between the optic nerve and lateral rectus
- Between the optic nerve and medial rectus
- Between the lateral rectus and the lateral orbital wall
- Between the medial rectus and the medial orbital wall
8. Where is the ciliary ganglion located? 1. Between the optic nerve and lateral rectus
The ciliary ganglion is located about 1 cm in front of the annulus of Zinn, on the lateral side of the ophthalmic artery between the optic nerve and the lateral rectus muscle. This has implications for orbital and strabismus surgery since it is vulnerable to damage during surgery in this area. Only the parasympathetic motor fibers synapse in the ganglion, whereas the sympathetic fibers pass through without synapsing to innervate the dilator muscle of the pupil.
9. In what other conditions is light-near dissociation seen?
- Horner’s syndrome
- Severe vision loss due to an optic neuropathy
- Temporal lobe tumor
- One-and-a-half syndrome
9. In what other conditions is light-near dissociation seen? 2. Severe vision loss due to an optic neuropathy
Light-near dissociation may be seen in a number of conditions including severe loss of afferent input to the eyes by an optic neuropathy. This is because there is severe loss of retinal ganglion cells that bring light information into the pupillary pathway, but the fibers to accommodation remain intact. The differential diagnosis of light-near dissociation includes:
- Severe loss of afferent input due to damage to anterior visual pathways (eg. severe optic neuropathy or retinopathy)
- Iatrogenic damage to the short posterior ciliary nerves (eg. panretinal photocoagulation, cryotherapy, orbital surgery)
- Peripheral neuropathy leading to diffuse axonal loss including the short posterior ciliary nerves (eg. diabetic neuropathy, Charcot-Marie Tooth disease)
- Damage to the ciliary ganglion (eg. Adie’s pupil)
- Aberrant regeneration of the 3rd nerve (aberrant reinnervation of the iris sphincter by neurons initially innervating the medial rectus)
- Loss of pre-tectal light input to the Edinger-Westphal nucleus (eg. Dorsal midbrain syndrome)
10. In a patient with an isolated dilated pupil with no reaction to light or a near stimulus, what pharmacological agent can be used to confirm a suspicion of a pharmacologically dilated pupil?
- Pilocarpine 0.1%
- Pilocarpine 1%
- Apraclonidine 1%
- Cocaine 10%
10. In a patient with an isolated dilated pupil with no reaction to light or a near stimulus, what pharmacological agent can be used to confirm a suspicion of a pharmacologically dilated pupil? 2. Pilocarpine 1%
A unilateral dilated pupil can be the result of exposure to a number of pharmacological agents such as atropine, scopolamine or amphetamines. Failure of the pupil to respond to pilocarpine 1% is usually sufficient to confirm the diagnosis of a pharmacologically dilated pupil. Full-strength pilocarpine will usually not overcome the effect of the pharmacological agent, but it will cause constriction of a dilated pupil from other causes of a dilated pupil in the differential diagnosis. Ocular conditions such as acute angle closure glaucoma may cause a mid-dilated, fixed pupil that does not constrict with pilocarpine due to ischemia of the iris sphincter. However, these patients usually have a red eye, significant ocular pain, and elevated intraocular pressure.
Clinical Pearl
A pharmacologically dilated pupil will not respond to pilocarpine 1%.
11. How does the response to dilute pilocarpine differ in a pre-ganglionic lesion (such as a 3rd nerve palsy) and a post-ganglionic lesion (such as Adie’s pupil)?
- There will be less constriction in the pre-ganglionic lesion since super-sensitivity does not occur
- There will be more constriction in the pre-ganglionic lesion since super-sensitivity does occur
- There will be a similar amount of constriction since super-sensitivity occurs in both
- There will not be any constriction in either since super-sensitivity does not develop
11. How does the response to dilute pilocarpine differ in a pre-ganglionic lesion (such as a 3rd nerve palsy) and a post-ganglionic lesion (such as Adie’s pupil)? 3. There will be a similar amount of constriction since super-sensitivity occurs in both
Super-sensitivity develops in both pre- and post-ganglionic lesions, so its presence is not helpful in localizing the lesion. An explanation for this is trans-synaptic degeneration of post-ganglionic fibers when the pre-ganglionic neuron is affected. Fortunately, there are other signs that differentiate a 3rd nerve palsy from post-ganglionic lesions. The main reason to use pharmacological testing is to differentiate denervation from post-ganglionic lesions and direct damage or dysfunction to the iris sphincter itself. Only the former will develop super-sensitivity.
12. How is Adie’s tonic pupil expected to change over many years?
- It will remain in a dilated state
- It will become slightly smaller (decrease in size by less than 1 mm)
- It will become much smaller and may become smaller than the normal pupil in the fellow eye
- It will become more dilated
12. How is Adie’s tonic pupil expected to change over many years? 3. It will become much smaller and may become smaller than the normal pupil in the fellow eye
The size of an Adie’s pupil decreases by 2-3 mm over several years and in some people it can become the smaller pupil (“little old Adie’s pupil”). As reinnervation increases with time, it is thought that the constant volley of impulses by accommodative fibers in darkness keeps the iris sphincter in a greater state of contraction compared to the normal pupil that does not receive these impulses. This, in addition to the continued increase in reinnervated segments, works to decrease the size of the pupil over time.
Case Summary
He noticed that his right pupil was larger for the past several months without diplopia or ptosis. There was no concern for a 3rd nerve palsy since examination showed normal position of the eyelids, normal ocular motility and alignment. There was segmental contraction of the iris sphincter and an exaggerated constriction to dilute pilocarpine, confirming the diagnosis of Adie’s tonic pupil. He was reassured and no further investigations were recommended. His pupil gradually decreased in size over the next several years and the anisocoria became less noticeable.
Further reading:
-
Gross JR, McClelland CM, Lee MS. An approach to anisocoria. Curr Opin Ophthalmol 2016;27(6):486-492. https://www.ncbi.nlm.nih.gov/pubmed/27585208
-
Moeller JJ, Maxner CE. The dilated pupil: an update. Curr Neurol Neurosci Rep 2007;7(5):417-22. https://www.ncbi.nlm.nih.gov/pubmed/17764632
-
Jacobson DM, Vierkant RA. Comparison of cholinergic supersensitivity in third nerve palsy and Adie’s syndrome. J Neuroophthalmol 1998;18(3):171-5. https://www.ncbi.nlm.nih.gov/pubmed/9736199
-
Kardon RH, Corbett JJ, Thompson HS. Segmental denervation and reinnervation of the iris sphincter as shown by infrared videographic transillumination. Ophthalmology 1998;105:313-321. https://www.ncbi.nlm.nih.gov/pubmed/9479293