6
Case
Age: 36-year-old white woman
Reason for referral to ophthalmology: Bilateral vision loss and pain with eye movements
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and drinks alcohol socially
HPI: One week ago, she had vision loss and pain with eye movements in the right eye that worsened over a period of 2 days. Two days ago, she noticed blurry vision in her left eye with mild ocular pain. This morning she developed hiccups with nausea that lasted the entire day. She presented to the emergency room and an ophthalmology consultation was requested.
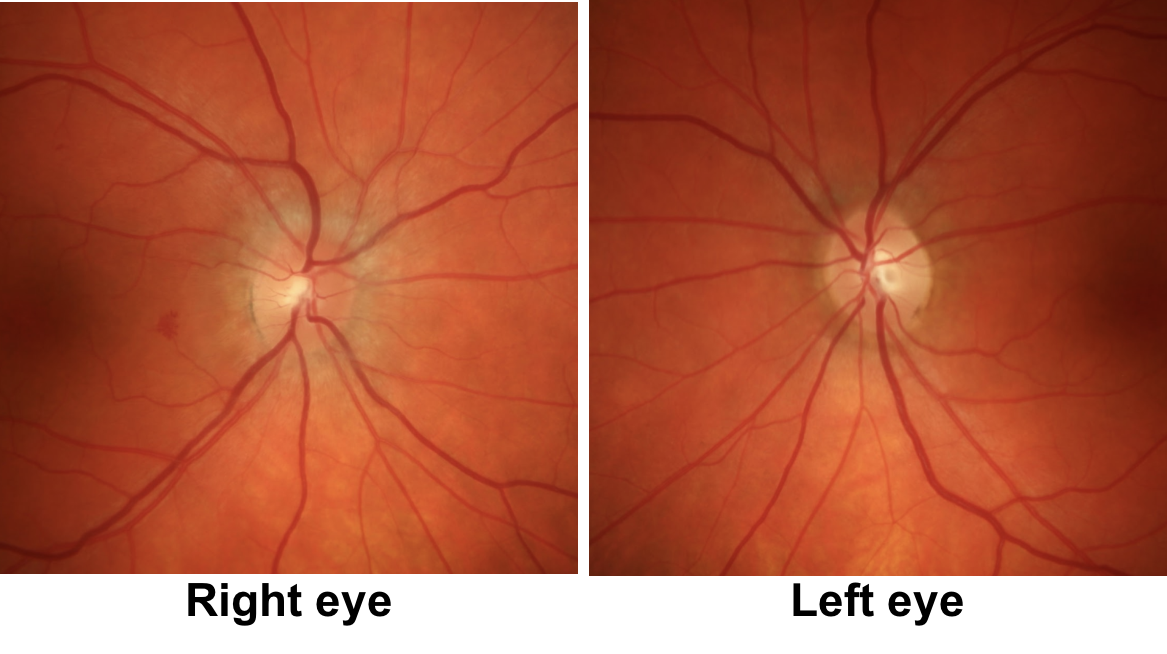
Ophthalmological Examination:
Blood pressure: 118/82, heart rate 75
Visual acuity is Hand Motions OD, 20/200 OS
Pupils are equal sizes and there is a mild right RAPD
Color vision is 0/14 OD and 0/14 OS correct Ishihara color plates
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
1. What aspect of this patient’s presentation is atypical for optic neuritis?
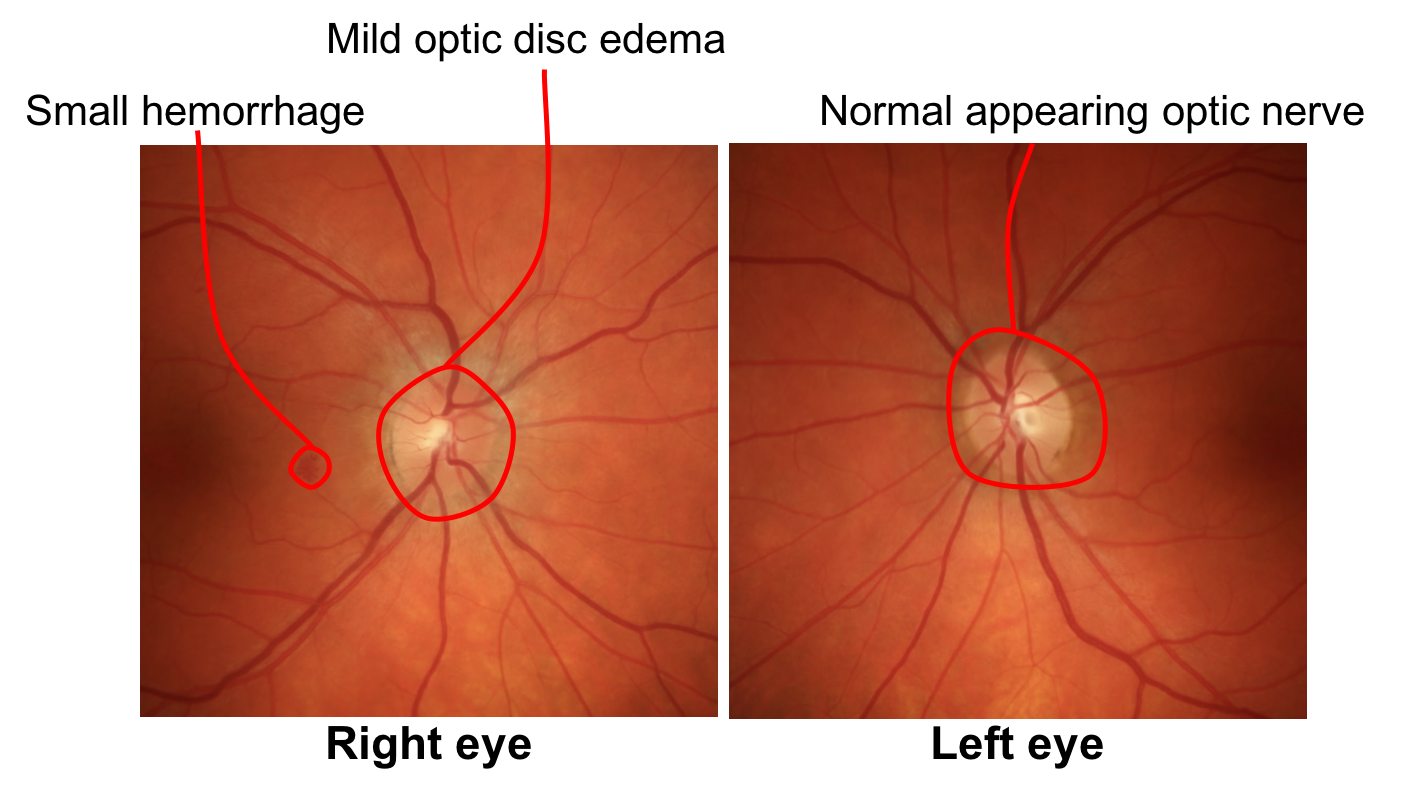
- Mild disc edema in the right eye and absent disc edema in the left eye
- Reduced colour vision
- Sequential bilateral vision loss
- Age above 30 years
1. What aspect of this patient’s presentation is atypical for optic neuritis? 3. Sequential bilateral vision loss
The rapidly sequential vision loss in both eyes in this patient is an atypical feature of optic neuritis. Mild or absent disc edema, reduced colour vision and age between 20 and 50 years or age are typically seen with optic neuritis. Atypical features of optic neuritis from the history, examination, or response to treatment are summarized below.
Clinical Pearl
Atypical features of optic neuritis include aspects from the history, examination, and response to treatment.
History:
- Younger or older age (less than approximately 15 or older than 50 years old)
- Absence of pain
- Sudden vision loss
- Simultaneous bilateral or rapidly sequential vision loss
Examination:
- Severe optic disc edema
- Presence of vitreous cells or retinal vasculitis
- Presence of optic disc hemorrhages
Response to treatment:
- Rapid recovery of vision with steroids
- No or minimal improvement of vision
2. What does the new onset of hiccups and nausea suggest?
- Acute gastritis
- Gastroesophageal reflux disease
- Corticosteroids are contraindicated in this patient
- Area postrema syndrome
2. What does the new onset of hiccups and nausea suggest? 4. Area postrema syndrome
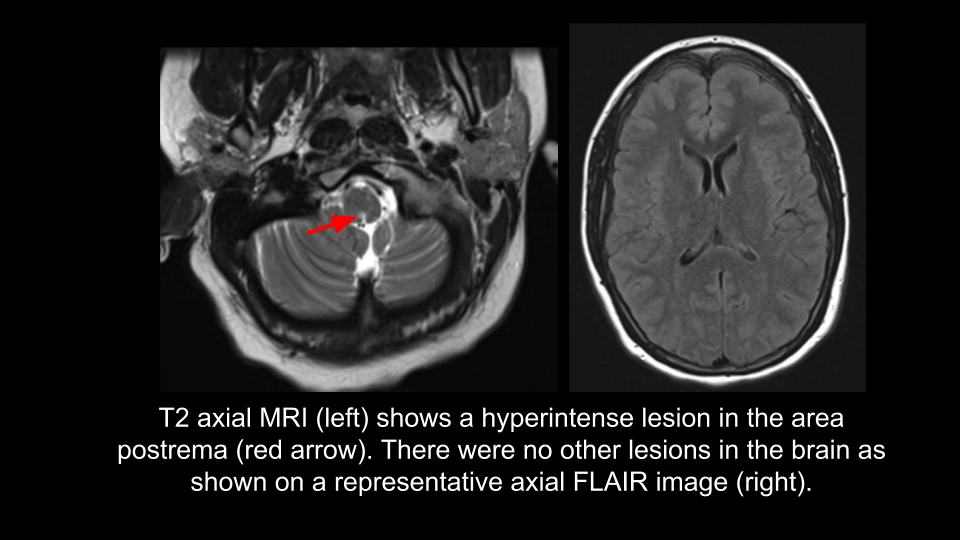
The presence of hiccups and nausea in a patient with bilateral optic neuritis is highly suggestive of area postrema syndrome. The area postrema is located in the medulla at the floor of the fourth ventricle and is a chemoreceptor trigger zone for vomiting. It lacks a blood-brain diffusion barrier to large polar molecules and is in an anatomical position that allows it to detect emetic toxins in the blood and CSF. Area postrema syndrome presents with hiccups that are sometimes intractable, nausea, and vomiting and is a clinical phenotype highly specific for neuromyelitis optica (NMO) spectrum disorder. Area postrema syndrome associated with medullary lesions on MRI occur with an incidence of 16 to 43% in NMO spectrum disorder.
3. What is the next best course of action for this patient?
- MRI of the brain
- MRI of the spine
- MRI of the orbits
- Serum NMO (AQP4) and MOG antibodies
- All of the above
3. What is the next best course of action for this patient? 5. All of the above
In this patient with severe vision loss and pain with eye movements suggestive of optic neuritis and clinical features of area postrema syndrome there is a high clinical suspicion for NMO spectrum disorder. This patient should be evaluated with an MRI of the brain, orbits and spine with contrast and serologic testing for AQP4 and myelin oligodendrocyte glycoprotein (MOG) antibodies. Since MRIs take a relatively long time to perform, MRI brain and orbits are often performed at a different time than the spine. MOG antibodies may also be seen in patients with AQP4-negative, NMO spectrum disorder phenotypes and are discussed in the box below.
Myelin Oligodendrocyte Glycoprotein (MOG) antibody: what is it?
MOG is a minor myelin component expressed on the surface of myelin sheaths and oligodendrocyte processes and its function is not completely understood. Intravenous injection of MOG antibodies in a mouse model that most closely resembles inflammatory demyelinating diseases in man increases the severity and duration of clinical signs of demyelination.
In patients with optic neuritis, positivity for MOG antibodies is helpful since it indicates that:
- The patient does not have multiple sclerosis
- NMO-IgG (aquaporin-4 antibodies) will be negative
- The patient will likely have a steroid-dependent, relapsing or recurrent course
Although MOG antibodies have a better prognosis than aquaporin-4 antibodies, a minority of patients will have incomplete recovery of vision despite aggressive treatment. Chronic immunosuppression in MOG-associated optic neuritis is considered if there is incomplete visual recovery or a recurrent/relapsing course. Testing for MOG antibodies should be considered in every patient with optic neuritis or those with NMO spectrum disorder in full or limited form.
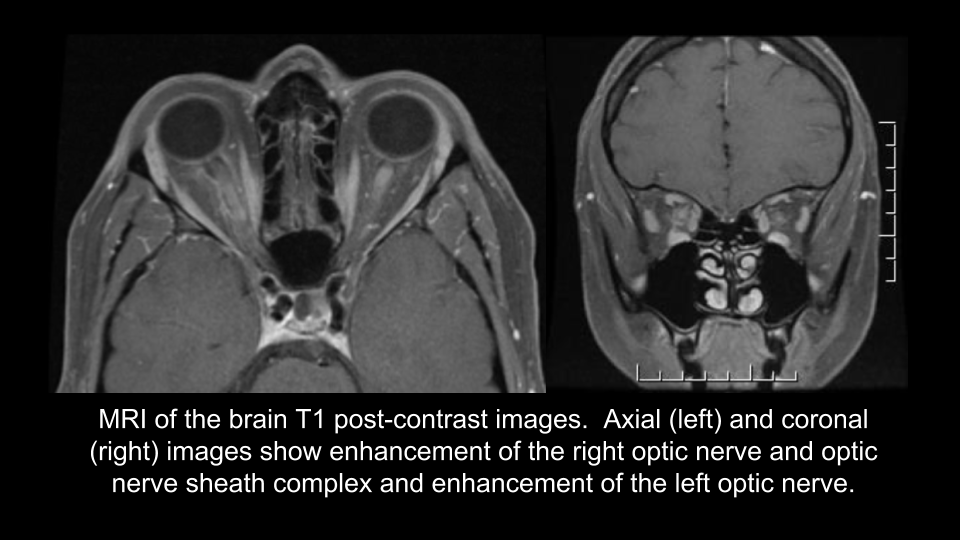
MRI of the brain and orbits with contrast is shown below.
MRI of the spine was normal.
Aquaporin-4 antibodies were positive
MOG antibodies were negative
4. Which of the following is true regarding this patient’s diagnosis?
- She does not meet the diagnostic criteria for NMO spectrum disorder since she does not have transverse myelitis
- She does not meet the diagnostic criteria for NMO spectrum disorder since she only has one core clinical characteristic
- She meets the diagnostic criteria for NMO spectrum disorder since she is AQP4-IgG positive and has at least one core clinical characteristic
- She meets the diagnostic criteria for NMO spectrum disorder since she has a bilateral optic neuritis with enhancement of both optic nerves on MRI
4. Which of the following is true regarding this patient’s diagnosis? 3. She meets the diagnostic criteria for NMO spectrum disorder since she is AQP4-IgG positive and has at least one core clinical characteristic
In a patient positive for AQP4-IgG, the NMO spectrum disorders diagnostic criteria requires the presence of at least one core clinical characteristic and the exclusion of alternative diagnoses.
Diagnostic criteria for Neuromyelitis Optica Spectrum Disorders (2015):
Aquaporin-4-IgG positive:
1. At least one core clinical characteristic
2. Exclusion of alternative diagnoses
Aquaporin-4-IgG negative or unknown status:
1. At least two core clinical characteristics occurring as a result of one or more clinical attacks and meeting the following requirements:
a. At least one core clinical characteristic must be optic neuritis, acute myelitis with longitudinally extensive transverse myelitis, or area postrema syndrome
b. Dissemination in space (two or more different core clinical characteristics)
c. Fulfillment of additional MRI requirements
2. Exclusion of alternative diagnoses
Core clinical characteristics:
- Optic neuritis
- Acute myelitis
- Area postrema syndrome
- Acute brainstem syndrome
- Symptomatic narcolepsy or acute diencephalic clinical syndrome with NMOSD-typical diencephalic MRI lesions
- Symptomatic cerebral syndrome with NMOSD-typical brain lesions
5. What would the CSF be expected to show in this patient during the acute phase before treatment is initiated?
- Normal leukocyte count, normal protein level, absent oligoclonal bands
- Normal leukocyte count, elevated protein level, presence of oligoclonal bands
- Elevated leukocyte count, normal protein level, presence of oligoclonal bands
- Elevated leukocyte count, elevated protein level, absence of oligoclonal bands
5. What would the CSF be expected to show in this patient during the acute phase before treatment is initiated? 4. Elevated leukocyte count, elevated protein level, absence of oligoclonal bands
Cerebrospinal fluid-specific oliglclonal bands are usually absent in NMO (70 to 85% of cases) unlike multiple sclerosis. This is because in NMO there is a specific antigen target (aquaporin-4) thus the bands are usually monoclonal rather than oligoclonal as in MS where there isn’t a specific antigen target. This can be a helpful differentiating factor, especially before the results of serology for AQP4 and MOG are available. Pleocytosis (increased cell count) and elevated protein in the CSF are common findings during the acute phase in NMO. Pleocytosis is detected in 14 to 79% of patients and a leukocyte count over 50 cells/mm3 has been reported in 13 to 35% of patients. Monocytes, lymphocytes or neutrophils may predominate.
6. Which treatment should be started immediately in this patient?
- Low-dose oral prednisone (0.5 mg/kg)
- Oral prednisone (1 mg/kg)
- Intravenous methylprednisolone 1 g daily
- Intravenous immunoglobulin (IVIG)
6. Which treatment should be started immediately in this patient? 3. Intravenous methylprednisolone 1 g daily
Acute attacks in NMO should be promptly treated with high dose methylprednisolone 1 g daily for 5 days with almost all patients receiving a slow taper of oral prednisone afterwards.
7. The patient has no improvement in her vision after 5 days of intravenous methylprednisolone 1 g daily. Her hiccups resolved. What other treatment should be considered at this time for optic neuritis?
- Methotrexate
- Plasma exchange (PLEX)
- Mycophenolate
- Rituximab
7. The patient has no improvement in her vision after 5 days of intravenous methylprednisolone 1 g daily. Her hiccups resolved. What other treatment should be considered at this time for optic neuritis? 2. Plasma exchange (PLEX)
Given the patient’s severe visual deficit and lack of improvement with intravenous methylprednisolone, PLEX should be strongly considered for this patient. This should be started as soon as possible and ideally within 10-15 days from symptom onset. Only about one-third of NMO patients are placed on corticosteroids alone in the acute phase with two-thirds requiring an additional treatment, which is most often PLEX. Typically 5 cycles of PLEX (1 to 1.5 volumes of blood) are given daily or every other day, which removes over 90% of circulating antibodies and other inflammatory components. Remission and improvement of symptoms are seen in about two-thirds of patients treated in this manner. In patients that do not improve, other considerations for treatment include cyclophosphamide or other chemotherapies.
8. Does the patient require longterm immunosuppression to prevent relapses?
- No, relapses are rare
- No, longterm immunosuppression is considered only if there is a relapse
- Yes, longterm immunosuppression should be initiated since relapses are common
- Yes, longterm immunosuppression should be initiated, but only after her vision returns to normal
8. Does the patient require longterm immunosuppression to prevent relapses? 3. Yes, longterm immunosuppression should be initiated since relapses are common
Neuromyelitis optica spectrum disorders carry considerable morbidity and longterm immunosuppression is universally recognized. Around 80% of patients experience a second attack within 2 years and relapses are highly correlated with disability. The most commonly used agents include azathioprine, methotrexate, mycophenolate, and rituximab. There is still uncertainty regarding the relative effectiveness of these medications and the duration of treatment. Most experts recommend longterm, if not, lifelong treatment to prevent relapses.
Clinical Pearl
Chronic immunosuppressive medications are recommended for patients with NMO spectrum disorder to prevent the morbidity associated with recurrent relapses.
9. The patient is seen in follow-up 3 months after the onset of vision loss. What do you expect her optic nerves to look like?
- Unchanged from the initial examination
- Persistent optic disc edema in the right eye and normal appearance in the left eye
- Optic disc pallor in the eye that had disc edema (right eye) and normal appearance in the left eye
- Optic disc pallor in both eyes
9. The patient is seen in follow-up 3 months after the onset of vision loss. What do you expect her optic nerves to look like? 4. Optic disc pallor in both eyes
After the acute phase of optic neuritis, optic disc pallor is expected in both eyes regardless of the initial appearance of the optic nerves. This becomes apparent approximately 6-8 weeks after the onset of vision loss.
10. A new patient has the onset of severe bilateral optic neuritis and longitudinally extensive transverse myelitis. Is it preferable to test the patient for serum or CSF Aquaporin-4 antibodies?
- Serum Aquaporin-4 IgG
- CSF Aquaporin-4 IgG
- They are both equivalent
- CSF is more sensitivity and specific only if there are leukocytes present in the CSF
10. A patient has the new onset of severe bilateral optic neuritis and longitudinally extensive transverse myelitis. Is it preferable to test the patient for serum or CSF Aquaporin-4 antibodies? 1. Serum Aquaporin-4 IgG
Previous studies have shown that patients that are positive for CSF Aquaporin-4 (AQP4)-IgG are almost always also positive for serum AQP4-IgG and testing for CSF AQP-4-IgG is of limited benefit. This is because AQP4 is expressed in astrocytes and the glial-endothelial interface and local blood-brain-barrier disturbances are sufficient to render the antigen directly accessible to serum antibodies.
11. Which of the following is true regarding the epidemiology of NMO spectrum disorders?
- It is more common in men than women
- It is more common than multiple sclerosis in non-white populations (Africans, Asians, Latinos)
- The median age of onset is between 60 and 80 years of age
- All of the above
11. Which of the following is true regarding the epidemiology of NMO spectrum disorders? 2. It is more common than multiple sclerosis in non-white populations (Africans, Asians, Latinos)
The reported incidence of NMO is up to 10 times higher in women than in men, although the monophonic form has approximately equal sex predilection. The median age of onset is between 32 and 41 years, but can occur in younger and older individuals. The incidence and prevalence is higher in non-white populations (Africans, Asians, Latinos) in which conventional multiple sclerosis is much less common.
12. Which of the following is true regarding MRI of the brain in patients with NMO?
- It is normal in a majority of patients
- Brain lesions are typically in areas with high aquaporin-4 expression such as the central medulla, diencephalon and hypothalamus
- There may be lesions in the subcortical white matter
- It may occasionally meet the diagnostic criteria for dissemination in space for multiple sclerosis
- All of the above
12. Which of the following is true regarding MRI of the brain in patients with NMO? 5. All of the above
MRI of the brain is normal in the majority of patients (55 to 84%) with a new presentation of NMO. In patients with brain lesions, they may be distributed throughout the white and grey matter and have been described in areas of high aquaporin-4 expression (central medulla, diencephalon, and hypothalamus), consistent with the pathogenesis of the disease. Brain involvement has also been reported to develop over time in up to 85% of patients and patients may even meet the diagnostic criteria for dissemination in space for multiple sclerosis.
Case Summary
She presented with sequential, bilateral vision loss and intractable hiccups, which was highly suggestive of optic neuritis and area postrema syndrome from NMO spectrum disorder. This was confirmed with a positive serum AQP4 antibody. Magnetic resonance imaging of the orbits showed enhancement of both optic nerves and MRI of the brain showed a lesion in the area postrema. She was treated with intravenous methylprednisolone 1 g daily for 5 days followed by plasma exchange. She was also started on rituximab to prevent relapses. Her vision recovered to 20/20 in both eyes 2 months later and she did not have any further relapses.
Further reading:
- Akaishi T, Nakashima I, Sato DK, Takahashi T, Fujihara K. Neuromyelitis optica spectrum disorders. Neuroimaging Clin N Am 2017;27(2):251-265. https://www.ncbi.nlm.nih.gov/pubmed/28391784
- Jarius S, Franciotta D, Paul F, et al. Cerebrospinal fluid antibodies to aquaporin-4 in neuromyelitis optica and related disorders: frequency, origin, and diagnostic relevance. J Neuroinflammation 2010;7:52. https://www.ncbi.nlm.nih.gov/pubmed/20825655
- Pittock SJ, Lennon VA, Krecke K, et al. Brain abnormalities in neuromyelitis optica. Arch Neurol 2006;63(3):390-396. https://jamanetwork.com/journals/jamaneurology/fullarticle/790890
-
Papadopoulos MC, Bennett JL, Verkman AS. Treatment of neuromyelitis optical: state-of-the-art and emerging treatments. Nat Rev Neurol 2014;10(9):493-506. https://www.ncbi.nlm.nih.gov/pubmed/25112508
-
Jarius S, Ruprecht K, Kleiter I, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: Frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin. J Neuroinflammation 2016;13(1):279.https://www.ncbi.nlm.nih.gov/pubmed/27788675
-
Merle H, Olindo S, Jeannin S, et al. Treatment of optic neuritis by plasma exchange (add-on) in neuromyelitis optica. Arch Ophthalmol 2012;130(7):858-62. https://www.ncbi.nlm.nih.gov/pubmed/22776923
-
Flanagan EP, Cabre P, Weinshenker BG, et al. Epidemiology of aquaporin-4 autoimmunity and neuromyelitis optica spectrum. Ann Neurol 2016. doi: 10.1002/ana.24617. https://www.ncbi.nlm.nih.gov/pubmed/22776923