17
Case
Age: 68-year-old man
Reason for referral to ophthalmology: Sudden-onset ptosis in the left eye
Past medical history: Hypertension, type 2 diabetes, dyslipidemia
Past ocular history: None
Medications: Metoprolol, valsartan, metformin, rosuvastatin
Habits: Non-smoker and occasional drinker (less than 1 glass per day)
HPI: Three days ago while watching TV he started to have pain around his left eye and double vision with objects separated horizontally. The double vision resolved if he covered either eye. A few hours later, he noticed his left eyelid started to droop and the double vision went away. He waited a few days to see if it would resolve, but it persisted and he went to the emergency room. A CT scan of the head without contrast was performed and was normal and an ophthalmology consultation was requested.
Ophthalmological examination:
Blood pressure: 152/86, heart rate 84
Visual acuity: 20/25 OD, 20/25 OS
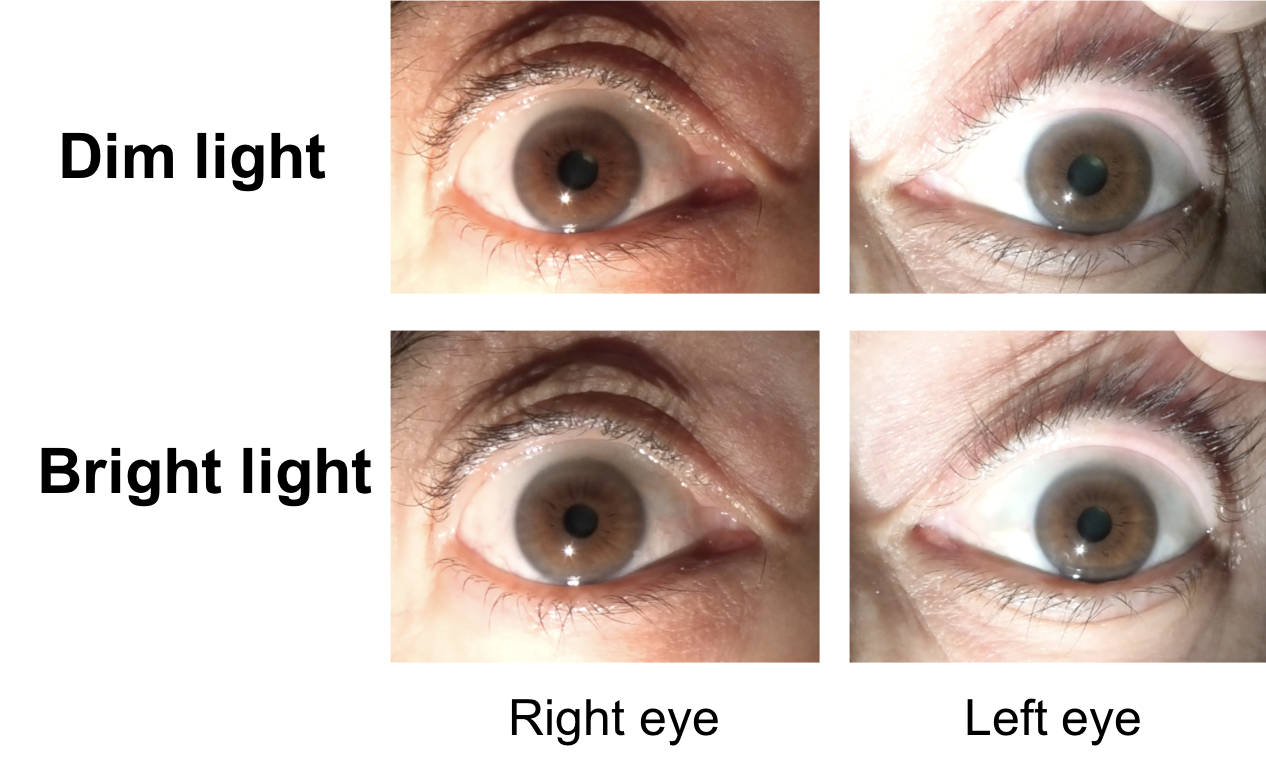
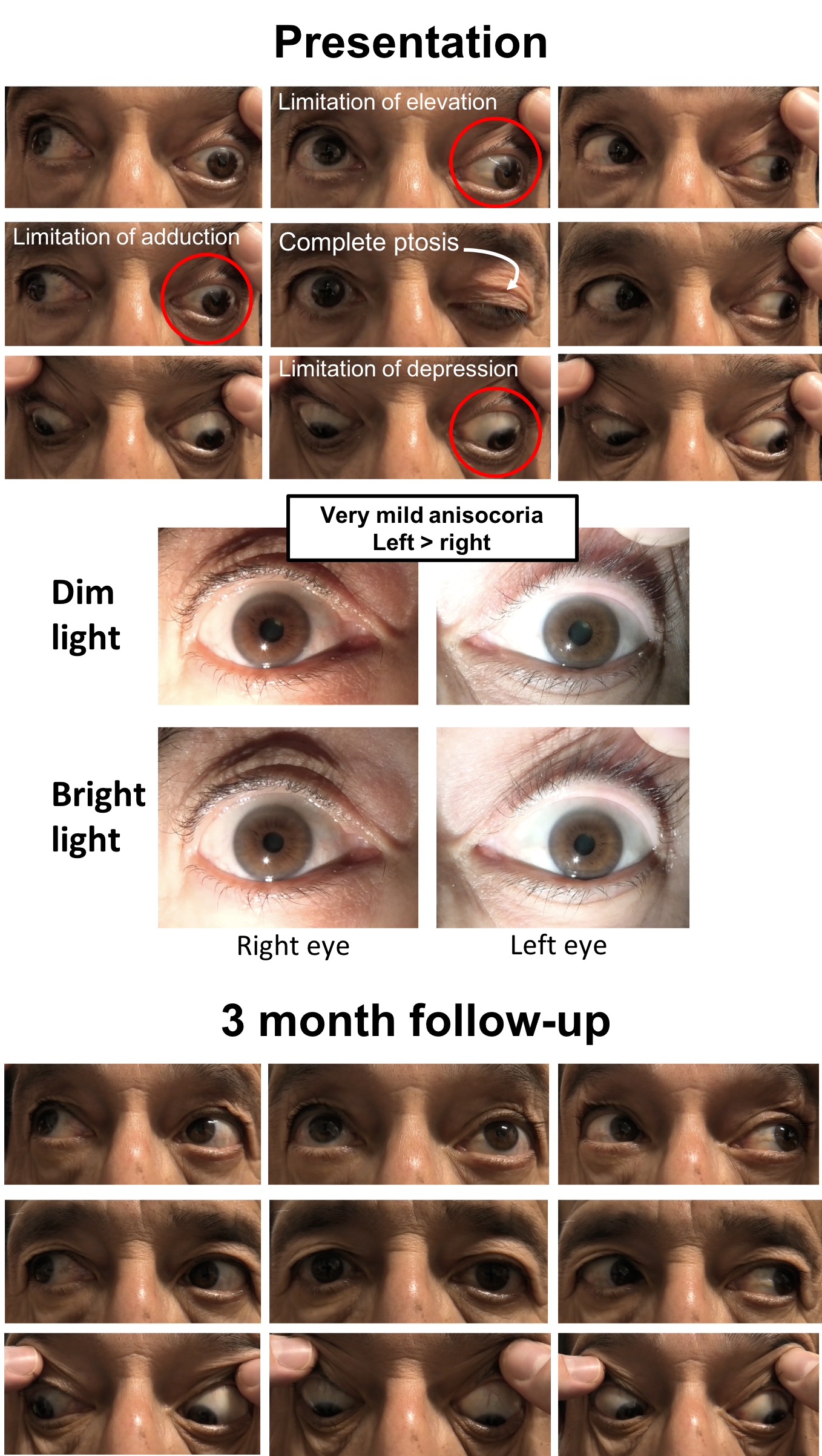
Pupils show a very mild anisocoria (<1 mm) slightly greater in bright light as shown below, there was no RAPD
Color vision: 14/14 OD and 14/14 OS correct Ishihara plates
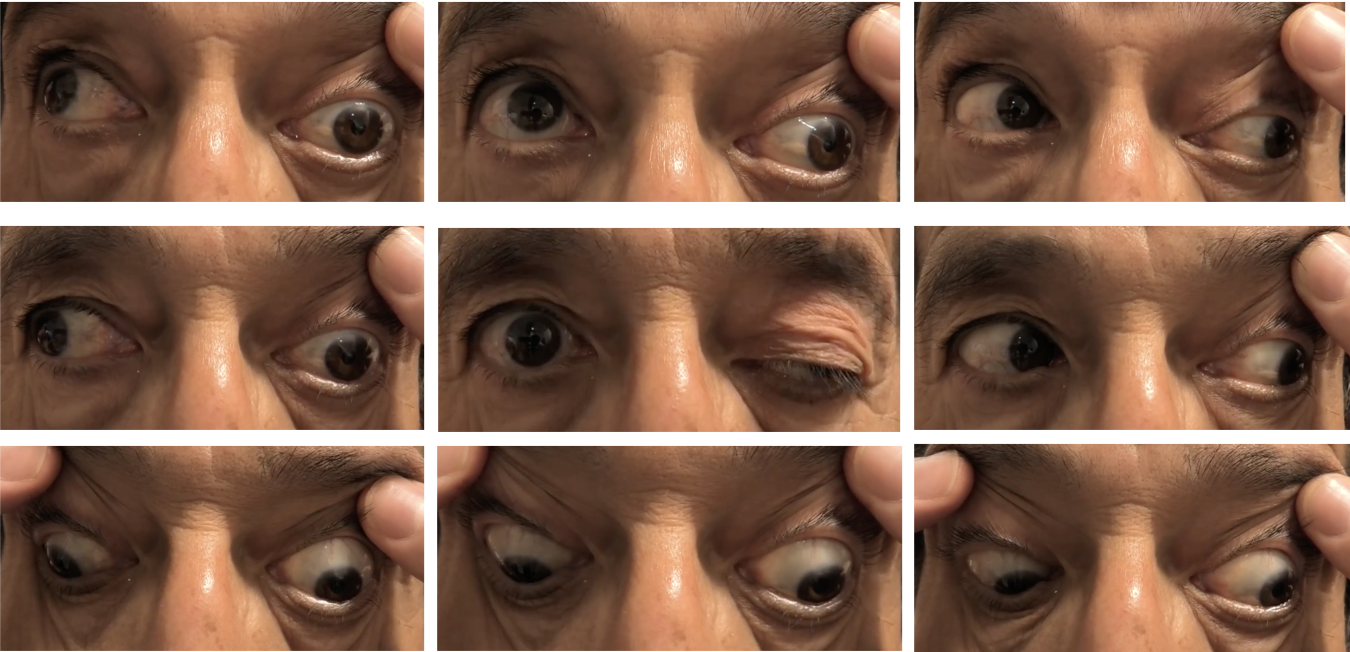
Ocular motility and alignment are shown below
Slit lamp examination shows mild nuclear sclerotic cataracts and dilated examination is normal.
Neurological examination is normal apart from the finding shown below
1. What is the most likely diagnosis?
- Left 4th and 6th nerve palsy
- Left 3rd and 6th nerve palsy
- Isolated left 3rd nerve palsy
- Thyroid eye disease
1. What is the most likely diagnosis? 3. Isolated left 3rd nerve palsy
The patient has left complete ptosis with an inability to adduct, elevate, and depress the left eye. The 3rd cranial nerve innervates the levator palpebrae superioris, medial rectus, superior rectus and inferior rectus muscles, which are all affected in this patient.
2. Where in the brainstem is the 3rd cranial nerve nucleus located?
- Midbrain at the level of the superior colliculus
- Midbrain at the level of the inferior colliculus
- Pons
- Medulla
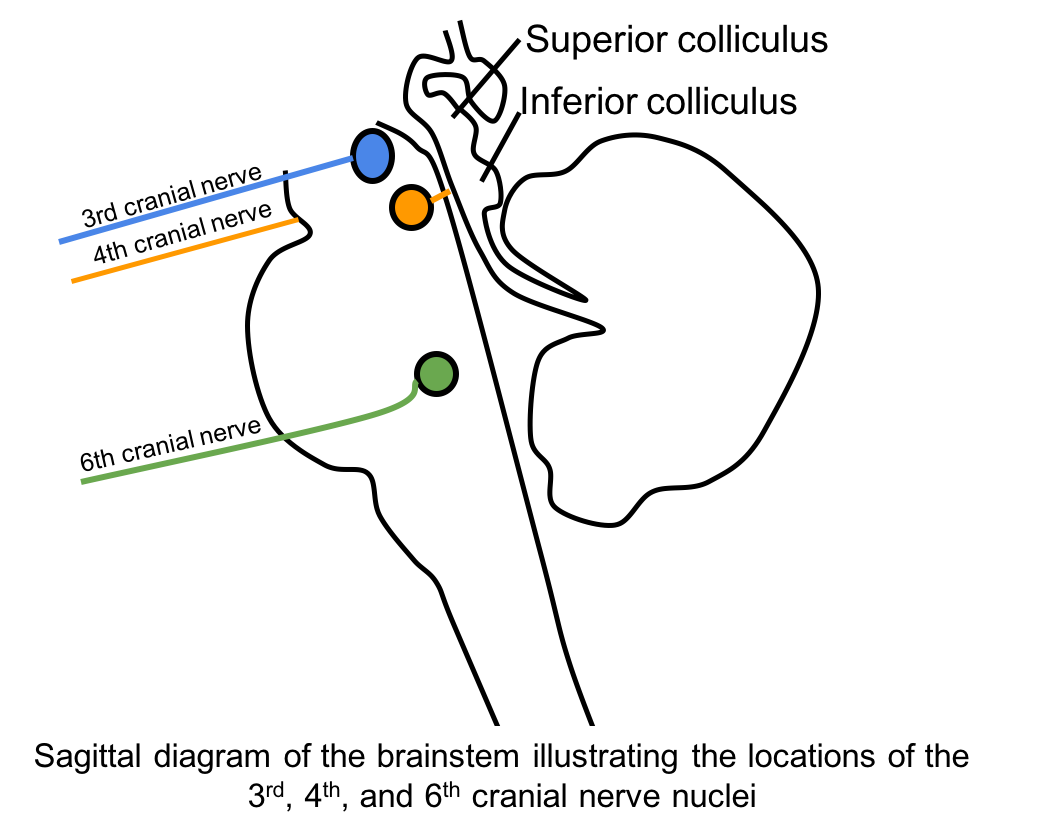
2. Where in the brainstem is the 3rd cranial nerve nucleus located? 1. Midbrain at the level of the superior colliculus
The 3rd nerve nucleus is located in the midbrain at the level of the superior colliculus ventral to the cerebral aqueduct and dorsal to the medial longitudinal fasciculus.
3. Why is a lesion of the 3rd cranial nerve nucleus not suspected in this patient?
- He does not have an altered level of consciousness
- He has a preserved corneal reflex
- His right eye has normal ocular motility and no ptosis
- Cranial nerve 4 and 6 are intact
3. Why is a lesion of the 3rd cranial nerve nucleus not suspected in this patient? 3. His right eye has normal ocular motility
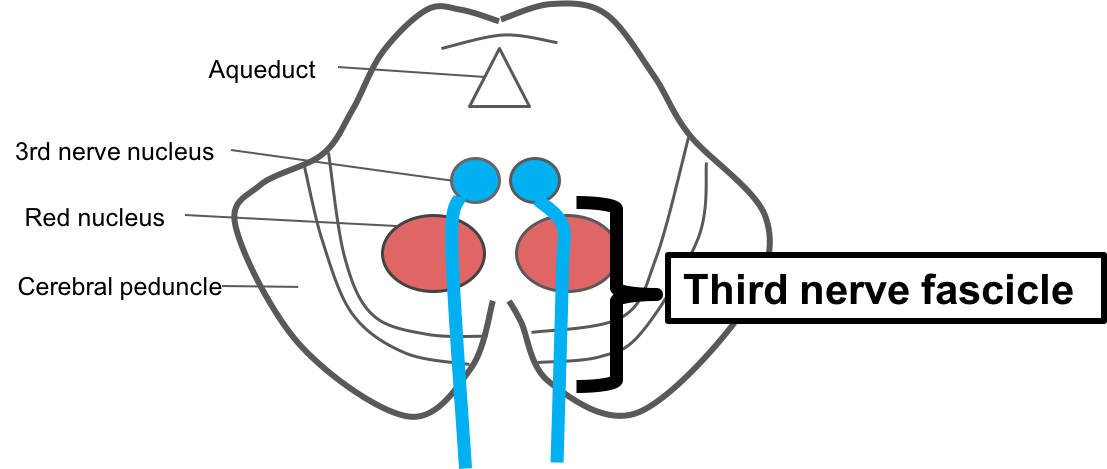
There are typically bilateral findings when the 3rd nerve nucleus is affected because of the unique anatomy of its subnuclei. A diagram of the 3rd nerve nucleus complex is shown below:
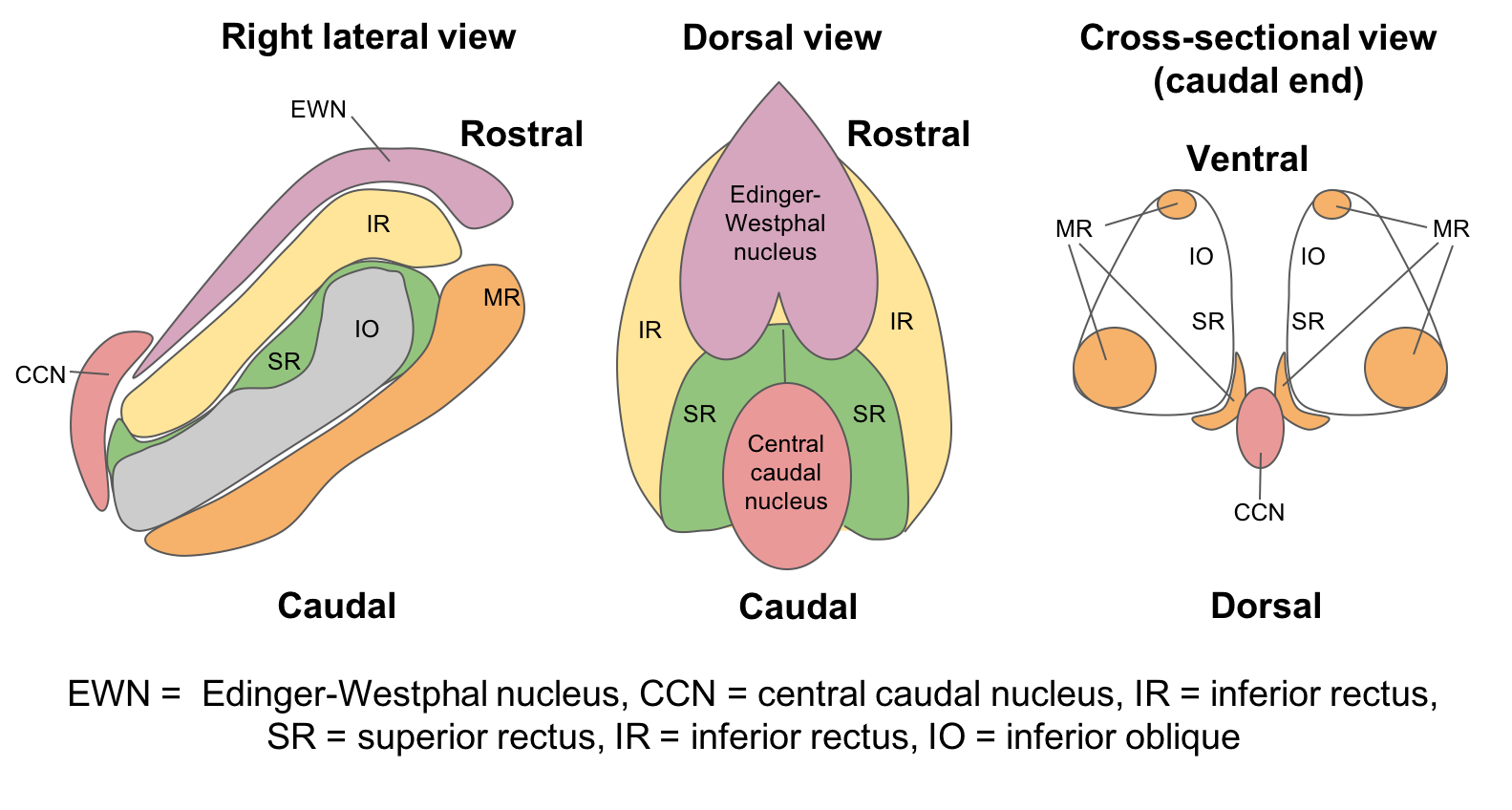
- Central caudal nucleus (CCN): There is only one, unpaired CCN, which supplies the levator palpebrae superiorus. It may be selectively affected, resulting in bilateral ptosis. Unilateral ptosis is therefore not consistent with a nuclear 3rd nerve palsy.
- Superior rectus subnuclei: There are two paired superior rectus subnuclei, which innervate the contralateral superior rectus muscle. However, axons from one superior rectus subnucleus pass through the other superior rectus subnucleus, resulting in bilateral elevation deficits. Consequently, a 3rd nerve palsy with normal elevation in the fellow eye is not consistent with a nuclear 3rd nerve palsy.
- Medial rectus subnuclei: They lie in various distinct locations within the 3rd nerve nucleus complex and therefore a lesion cannot individually affect these distinct locations while sparing the other structures within the nucleus. Therefore, isolated adduction weakness is not consistent with a nuclear 3rd nerve palsy.
Clinical Pearl
A nuclear 3rd nerve palsy presents with bilateral findings such as bilateral ptosis or elevation deficits.
4. A patient presents with a unilateral 3rd nerve palsy and contralateral hemiparesis. Where is the lesion?
- Third nerve nucleus
- Third nerve fascicle in the midbrain
- Third nerve in the subarachnoid space
- Third nerve in the cavernous sinus
4. A patient presents with a unilateral 3rd nerve palsy and contralateral hemiparesis. Where is the lesion? 2. Third nerve fascicle in the midbrain
A 3rd nerve palsy may be caused by a lesion in the 3rd nerve fascicle, which are the nerve fibers located in the midbrain after they have left the 3rd nerve nucleus. A fascicular 3rd nerve palsy will affect the eye ipsilateral to the lesion and often has associated neurological signs due to the proximity of other brainstem structures such as the red nucleus, cerebral peduncle and cerebellar peduncle. Ischemia is the most common cause of fascicular 3rd nerve palsies.
5. What is the syndrome of a 3rd nerve palsy and contralateral tremor called?
- Benedikt’s syndrome
- Weber’s syndrome
- Nothnagel’s syndrome
- Claude’s syndrome
5. What is the syndrome of a 3rd nerve palsy and contralateral tremor called? 1. Benedikt’s syndrome
The 3rd nerve fascicle syndromes are summarized below. The contralateral tremor suggests involvement of the red nucleus and Benedikt’s syndrome as shown below.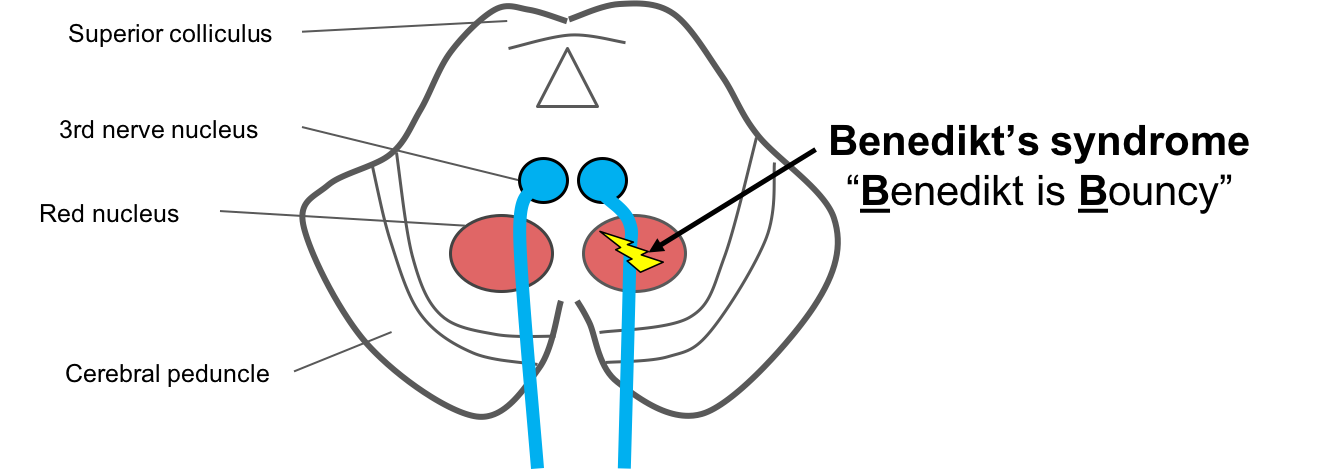
- Benedikt’s syndrome is due to involvement of the 3rd nerve fascicle and the red nucleus, leading to an ipsilateral 3rd nerve palsy and contralateral tremor, hemichorea, hemiathetosis, or hemiballismus (Remember “Benedickt is Bouncy”).
- Weber’s syndrome is due to involvement of the 3rd nerve fascicle and cerebral peduncle leading to an ipsilateral 3rd nerve palsy and contralateral hemiparesis or hemiplegia (“Weber is Weak”).
- Nothnagel’s syndrome is due to involvement of the 3rd nerve fascicle and the superior cerebellar peduncle leading to an ipsilateral 3rd nerve palsy and ipsilateral cerebellar ataxia (“Nothnagel is Not crossed”).
- Claude’s syndrome is due to involvement of the 3rd nerve fascicle and the superior cerebellar peduncle and often the red nucleus leading to an ipsilateral 3rd nerve palsy, ipsilateral cerebellar ataxia and contralateral tremor (Benedikt + Nothnagel).
6. What is the next most appropriate course of action for the patient described at the beginning of the chapter?
- Assessment of hemoglobin A1c and optimization of vascular risk factors
- CTA or MRA of the head
- MRI of the orbits with contrast
- TSH and free T4
6. What is the next most appropriate course of action for the patient described at the beginning of the chapter? 2. CTA or MRA of the head
The most serious cause of an isolated 3rd nerve palsy is a compression from an intracranial aneurysm, most commonly an aneurysm of the posterior communicating artery. A change in morphology of an unruptured aneurysm large enough to cause symptoms signals an impending rupture and is a medical emergency. When an aneurysm ruptures, it causes a devastating subarachnoid hemorrhage with an extremely high morbidity and mortality. Approximately 15% of patients die even before hospital admission, another 40% die in hospital, and more than one-third of survivors have permanent neurological deficits. Initial investigations should be directed towards ruling out an intracranial aneurysm in a patient with a new onset 3rd nerve palsy and this is best done with non-invasive angiography, either a CTA or MRA. The choice of imaging will depend on the availability and comfort of the neuro-radiologist in interpreting each type of scan.
Clinical Pearl
All patients with a new onset 3rd nerve palsy require a CTA or MRA of the head to rule out an intracranial aneurysm, particularly a posterior communicating artery aneurysm.
7. The posterior communicating artery connects which two intracranial blood vessels?
- Internal carotid artery and superior cerebellar artery
- Internal carotid artery and posterior cerebral artery
- Posterior cerebral artery and superior cerebellar artery
- Posterior cerebrala artery basilar artery
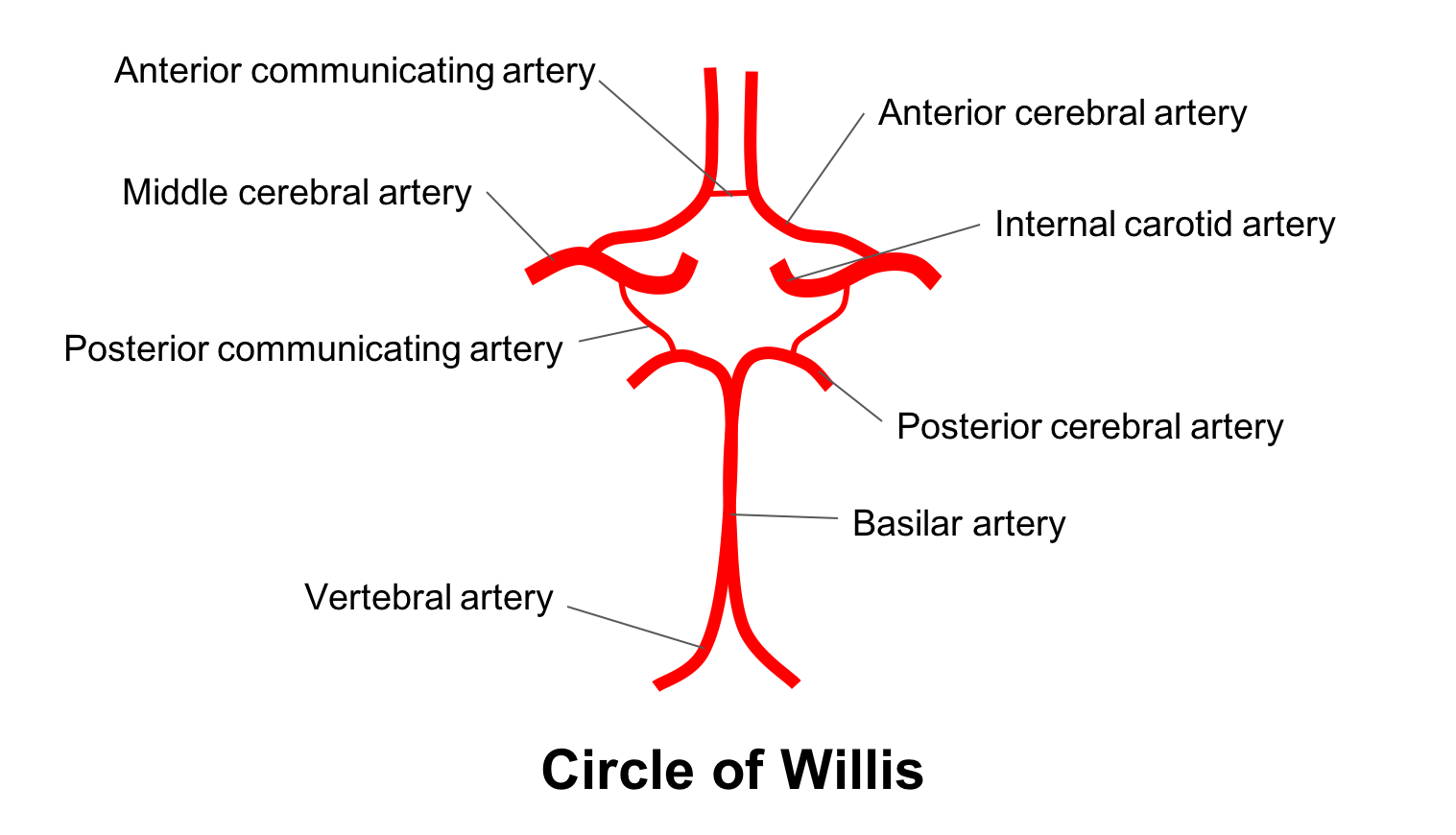
7. The posterior communicating artery connects which two intracranial blood vessels? 2. Internal carotid artery and posterior cerebral artery
The posterior communicating artery connects the internal carotid artery (anterior circulation) with the posterior cerebral artery (posterior circulation). It supplies the thalamus, hypothalamus, optic chiasm and mamillary bodes. The anatomy of the Circle of Willis is summarized below.
8. Aneurysms in which intracranial arteries may lead to a 3rd nerve palsy?
- Posterior communicating artery
- Basilar artery
- Superior cerebellar artery
- Internal carotid artery
- All of the above
8. Aneurysms in which intracranial arteries may lead to a 3rd nerve palsy? 5. All of the above
Aneurysms are usually found at the junctions, bifurcations or abrupt vascular angles where excessive hemodynamic stress is exerted on vessel walls. The most common location for an aneurysm affecting the 3rd nerve is the posterior communicating artery at the junction of the internal carotid artery. The 3rd nerve travels lateral to the posterior communicating artery as it approaches the cavernous sinus. As seen in the diagram below, the 3rd nerve passes through the posterior cerebral artery and superior cerebellar artery as it exits the brainstem near the basilar artery and aneurysms in these vessels, although less common, have also been reported to also cause a 3rd nerve palsy. Common sites of lesions affecting the 3rd nerve are summarized below.
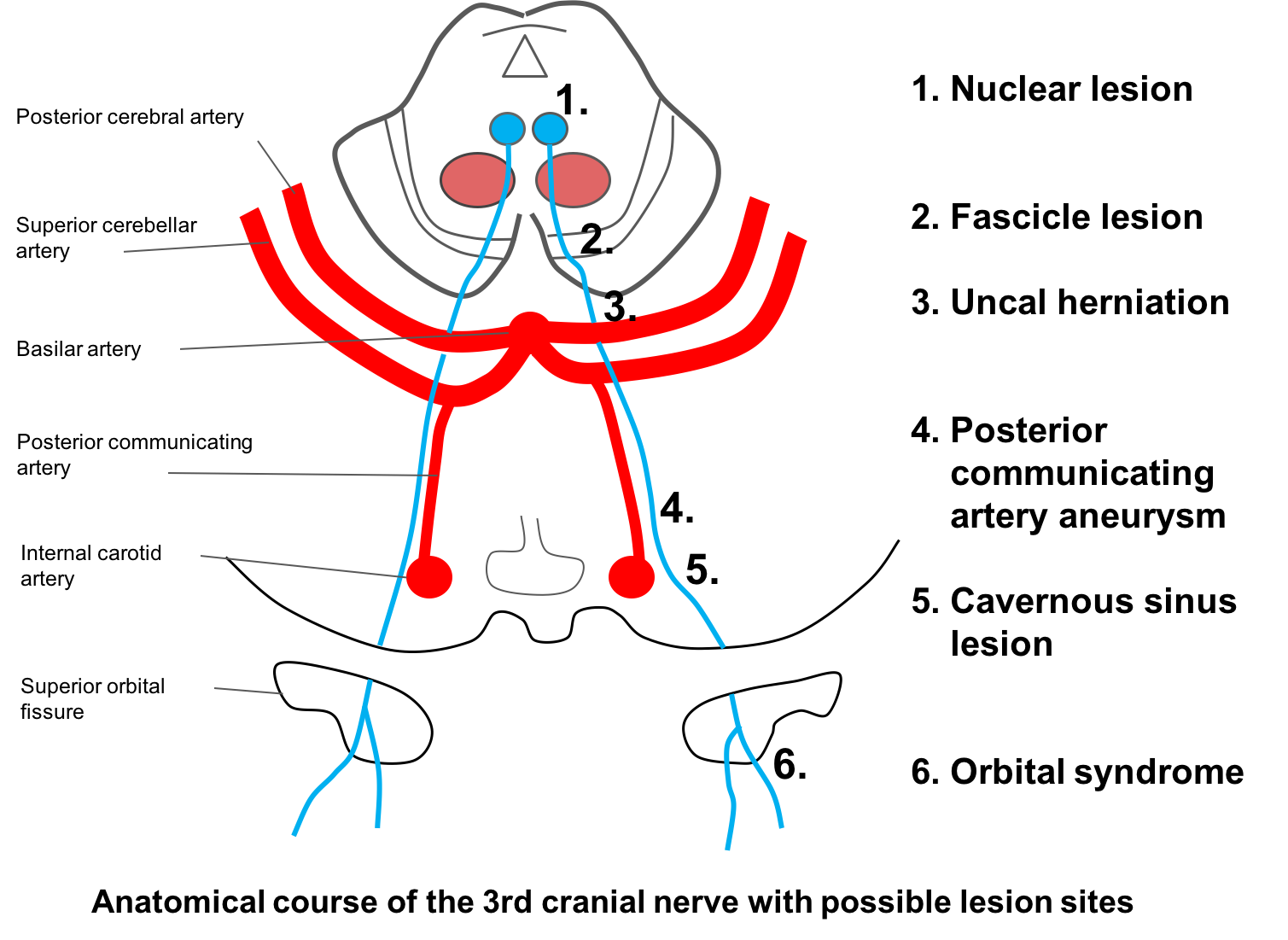
9. To cause a 3rd nerve palsy, an aneurysm of the posterior communicating artery should be at least:
- 4 mm
- 6 mm
- 8 mm
- 10 mm
9. To cause a 3rd nerve palsy, an aneurysm of the posterior communicating artery should be bigger than what size? 1. 4 mm
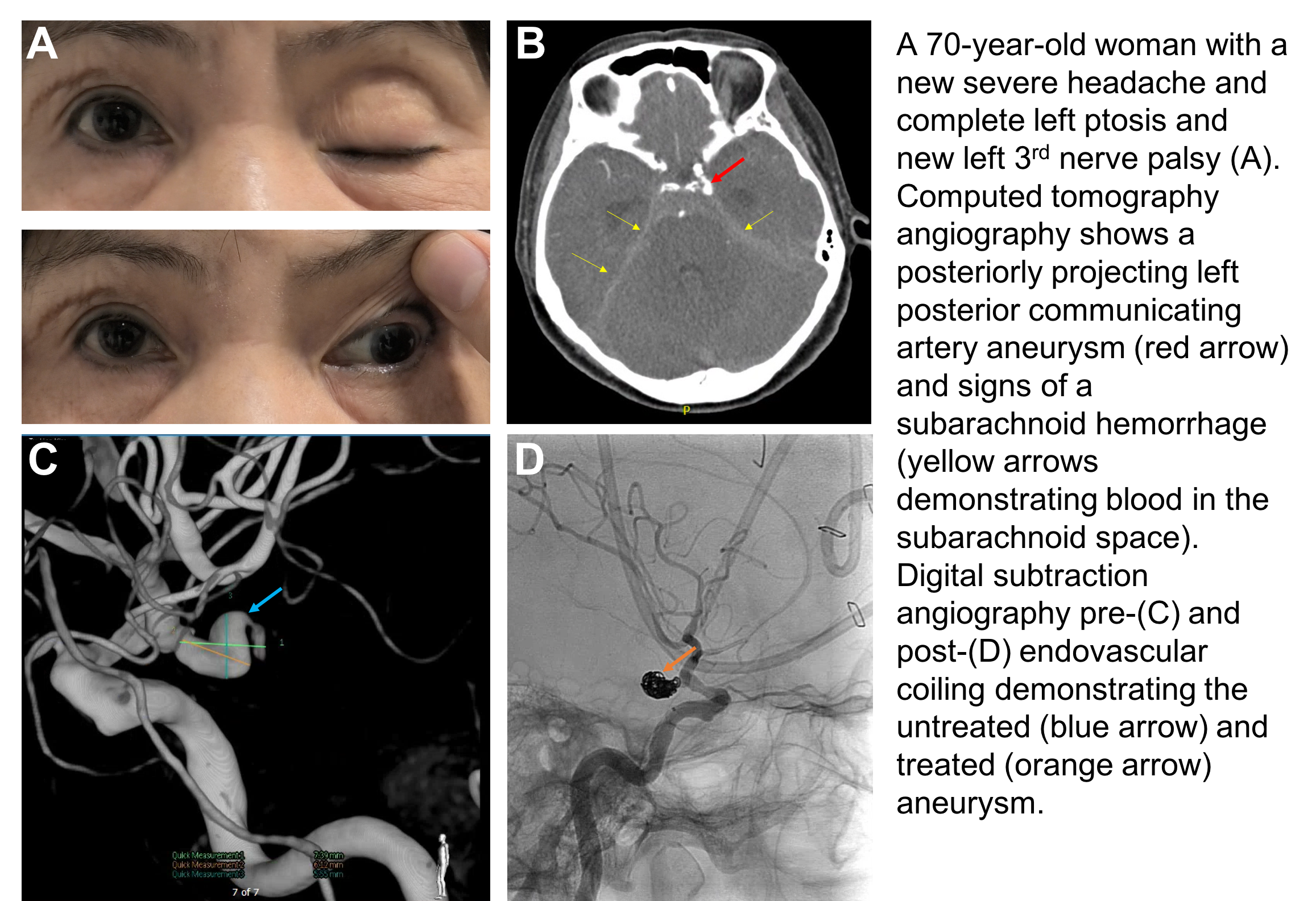
The smallest aneurysms reported to cause a 3rd nerve palsy were at least 4 mm in size. This is important because CTA and MRA have advanced to the point where aneurysms large enough to cause a 3rd nerve palsy can be detected in essentially all cases with these imaging modalities. A patient with a 7 mm posterior communicating artery aneurysm and subarachnoid hemorrhage seen on CTA is shown below. Digital subtraction angiography was performed before and after treatment with endovascular coiling.
10. In the region of the anterior cavernous sinus and superior orbital fissure, the 3rd nerve separates into a superior and inferior division. Which of the following is innervated by the inferior division?
- Levator palpebrae superioris
- Superior rectus muscle
- Superior oblique muscle
- Pupillary fibers destined for the pupillary sphincter
10. In the region of the anterior cavernous sinus and superior orbital fissure, the 3rd nerve separates into a superior and inferior division. Which of the following is innervated by the inferior division? 4. Pupillary fibers destined for the pupillary sphincter
The branches of the inferior division of the 3rd cranial nerve innervate the inferior rectus, medial rectus and inferior oblique muscle. It also transmits parasymphathetic fibers to the ciliary ganglion, which synapse and accompany the fibers to the inferior oblique before innervating the iris sphincter muscle.
Clinical Pearl
The superior division of the 3rd cranial nerve innervates the levator palpaebrae superioris and the superior rectus muscle.
11. A patient with a complete 3rd nerve palsy has a pupil of normal size and reactivity. This:
- Rules out a compressive lesion
- Makes a compressive lesion more likely
- Makes a compressive lesion less likely
- Means the underlying cause is diabetes
11. A patient with a complete 3rd nerve palsy has a pupil of normal size and reactivity. This: 3. Makes a compressive lesion less likely
A 3rd nerve palsy should first be characterized as partial or complete. Complete means that there is complete closure of the eyelid and the muscles innervated by the 3rd cranial nerve are severely affected. Only if the 3rd nerve palsy is complete and isolated, can one apply the “rule of the pupil”, which states that when aneurysms compress the 3rd cranial nerve, the iris sphincter will be impaired leading to a dilated or sluggishly reactive pupil.
The pupillary fibers run superior and medial on the outer part of 3rd nerve. Since the posterior communicating artery is also superior and medial relative to the 3rd nerve, an inferolaterally extending posterior communicating artery aneurysm will affect the pupillary fibers. This patient has a complete left 3rd nerve palsy, but relative sparing of the pupil (there is only minimal, subtle anisocoria), making a compressive lesion such as an aneurysm less likely. However, it does not completely rule it out since aneurysmal 3rd nerve palsies have been reported when the pupil is spared or pupil involvement may develop later on in the course of the condition. Basilar artery aneurysms may compress the 3rd nerve from below and spare the pupil. It is generally accepted that all patients with a 3rd nerve palsy should have a CTA or MRA of the head, regardless of the status of the pupil.
12. What is the most likely cause of the 3rd nerve palsy of the patient seen at the beginning of this chapter?
- Microvascular ischemia
- Intracranial aneurysm
- An unrecognized pituitary tumor
- Brainstem herniation
12. What is the most likely cause of the 3rd nerve palsy of the patient seen at the beginning of this chapter? 1. Microvascular ischemia
The most likely cause of the left 3rd nerve palsy is microvascular ischemia, which classically causes a complete, pupil sparing 3rd nerve palsy. The patient also has vascular risk factors to support this diagnosis. Microvascular ischemia is a result of injury to the very small blood vessels that supply the 3rd cranial nerve (vaso nervorum) mostly seen in diabetic or hypertensive patients. These small blood vessels are too small to be seen with neuroimaging techniques and are too small to be affected by an embolus. The reason the pupil is usually spared in these cases is because the affected micro-vessels are located in the center of the 3rd nerve and the parasympathetic pupil fibers are located in the periphery of the nerve and receive blood from other collateral vessels. Overall, microvascular ischemia is the most common cause of 3rd nerve palsies.
Microvascular 3rd nerve palsies may have some pupil involvement in up to 38% of cases, but this anisocoria is usually mild (less than 1 mm) and the pupil still has some degree of reactivity.
Neuroimaging results:
CTA of the head and MRI of the brain with contrast were normal and there was no evidence of an intracranial aneurysm.
He was diagnosed with a 3rd nerve palsy secondary to microvascular ischemia.
13. What is the natural history of microvascular ischemic 3rd nerve palsies?
- Stable over many years
- May worsen in 6 months
- Resolution within 3 months
- Resolution in 1 to 2 weeks
13. What is the natural history of microvascular ischemic 3rd nerve palsies? 3. Resolution within 3 months
Microvascular 3rd nerve palsies have a good prognosis; improvement usually begins within several weeks and complete resolution occurs within 3 months. The ptosis usually improves first and patients often become diplopic again before complete resolution. This can be treated symptomatically by occluding one eye with a patch or placing a piece of tape over an eyeglass lens until it resolves. If the 3rd nerve palsy does not resolve during this time period, further investigations to look for other causes should be considered.
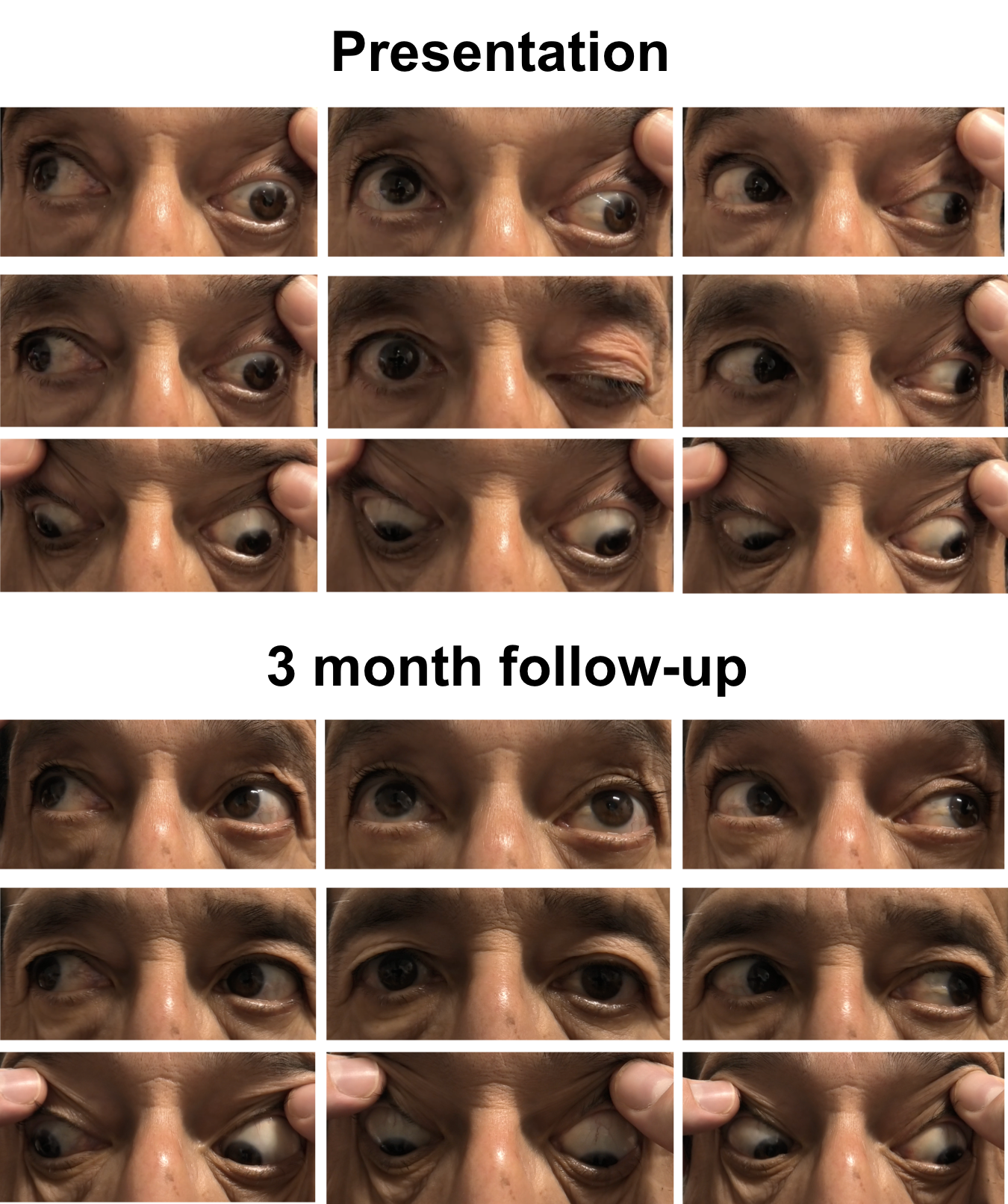 The natural history of microvascular ischemic third nerve palsies is one of complete resolution within 3 months of onset as shown in this patient.
The natural history of microvascular ischemic third nerve palsies is one of complete resolution within 3 months of onset as shown in this patient.14. What other investigations should be performed in an 80-year-old woman with a 3rd nerve palsy and a normal MRI and MRA of the brain?
- Abdominal ultrasound
- ESR and CRP
- Bartonella serology
- Lyme serology
14. What other investigations should be performed in an 80-year-old woman with a 3rd nerve palsy and a normal MRI and MRA of the brain? 2. ESR and CRP
Giant cell arteritis must be considered in any elderly patient presenting with isolated or multiple cranial nerve palsies. This should be evaluated with a thorough history, examination and bloodwork that includes a CBC, ESR, and CRP.
Clinical Pearl
Giant cell arteritis should be considered in any patient over 50 years of age presenting with an isolated or multiple cranial nerve palsies
15. A patient is diagnosed with a 3rd nerve palsy and at a follow-up visit, his eyelid is noted to elevate when he depresses his eye (red box below). Which of the following was not the cause of his 3rd nerve palsy?

- Trauma
- Aneurysm
- Microvascular ischemia
- Pituitary tumor
15.A patient is diagnosed with a 3rd nerve palsy and at a follow-up visit, his eyelid is noted to elevate when he depresses his eye. Which of the following was not the cause of his 3rd nerve palsy? 3. Microvascular ischemia
The patient has signs of aberrant regeneration of the 3rd nerve. This is a synkinesis thought to be due to misdirection of regenerated axons in the nerve or brain stem and in this case, axons that originally innervated the inferior rectus were misdirected to the levator muscle. There are several signs that may develop after aberrant regeneration:
- Lid-gaze dyskinesis. “Pseudo-von Graefe sign”: lid retraction when the patient looks down. “Inverse Duane syndrome”: lid retraction when the patient adducts the eye
- Pupil-gaze dyskinesis. “Pseudo Argyll Robinson pupil”: pupillary constriction during convergence or adduction. Pupillary constriction with infraduction may also be seen.
Aberrant regeneration not only occurs weeks to months after the initial 3rd nerve palsy, but may also seen primarily with insidious development of a 3rd nerve palsy and with accompanying signs of misdirection. The latter is seen with slow-growing lesions of the cavernous sinus such as aneurysms or meningiomas. Aberrant regeneration is not seen in microvascular 3rd nerve palsies and if this original diagnosis was given it must be reconsidered if signs of aberrant regeneration are present.
16. A patient has a 3rd nerve palsy with pain behind his eye. This means that the 3rd nerve palsy:
- Must be due to an aneurysm
- May be due to microvascular ischemia
- Must be secondary to trauma
- Should have a temporal artery biopsy as part of the workup
16. A patient has a 3rd nerve palsy with pain behind his eye. This means that the 3rd nerve palsy: 2. May be due to microvascular ischemia
Microvascular ischemic 3rd nerve palsies are frequently accompanied by pain and this is thought to be due to the 3rd nerve containing sensory fibers from trigeminal ganglion cells. Pain may also be seen in traumatic, aneurysmal, and arteritic 3rd nerve palsies and is not a particularly helpful differentiating feature.
17. A 60-year-old man has ptosis and limitation of elevation, depression and adduction in the left eye and a left 3rd nerve palsy secondary to microvascular ischemia is diagnosed. Pupils are equal sizes and CTA and MRI of the head are normal. At a 3-month follow-up visit, the left ptosis has improved, but there is also right ptosis. The ocular motility of the left eye is mildly improved. Which of the following tests should be considered at this point?
- CT scan of the brain without contrast
- MRI of the spine
- NMO antibodies
- Acetylcholine receptor antibodies
17. A 60-year old man has ptosis and limitation of elevation, depression and adduction in the left eye and a left 3rd nerve palsy secondary to microvascular ischemia is diagnosed. Pupils are equal sizes and CTA and MRI of the head are normal. At a 3-month follow-up visit, the left ptosis has improved, but there is right ptosis. The ocular motility of the left eye is mildly improved. Which of the following tests should be considered at this point? 4. Acetylcholine receptor antibodies
A 3rd nerve palsy from microvascular ischemia should resolve after 3 months. Since it has not, other diagnoses must be considered. The new right ptosis raises the question of a disorder of the neuromuscular junction such as ocular myasthenia gravis, which has a predilection for the extraocular muscles innervated by the 3rd cranial nerve. Clinical testing such as an ice or sleep test and laboratory workup with acetylcholine receptor antibodies are indicated.
18. A 58-year-old man is urgently referred for a unilateral dilated pupil that he noticed when he woke up in the morning. Examination reveals no ptosis and normal ocular motility. Which of the following is true?
- There is a high likelihood that this is the presenting sign of a 3rd nerve palsy and an urgent CTA of the head should be performed to rule out an intracranial aneurysm
- There is a high likelihood that this is the presenting sign of a 3rd nerve palsy and a CT of the head without contrast should be performed first
- There is an extremely low likelihood that this is the presenting sign of a 3rd nerve palsy and pharmacologic testing should be considered
- There is an extremely low likelihood that this is the presenting sign of a 3rd nerve palsy, but a CT scan of the orbits should be performed to rule out an orbital process
18. A 58-year-old man is urgently referred for a unilateral dilated pupil that he noticed when he woke up in the morning. Examination reveals no ptosis and normal ocular motility. Which of the following is true? 3. There is an extremely low likelihood that this is the presenting sign of a 3rd nerve palsy and pharmacologic testing should be considered
An isolated, dilated pupil is extremely unlikely to be the sole manifestation of a 3rd nerve palsy in otherwise normal patients. A compressive or other lesion of the 3rd nerve would be associated with at least some eye movement abnormality or ptosis. The position of the eyelid and ocular alignment and motility need to be closely examined in these situations since the associated changes may be subtle. More likely considerations for this patient include pharmacological mydriasis or local causes leading to dysfunction of the iris sphincter. If pharmacological mydriasis is suspected, then full strength pilocarpine testing can be performed. A pharmacologically dilated pupil should not constrict to this concentration of pilocarpine.
Case Summary
He presented with new onset diplopia and complete ptosis with an inability to elevate, adduct or depress his left eye, consistent with a left 3rd nerve palsy. There was subtle anisocoria with the left pupil being slightly larger than the right, which was more obvious in bright lighting conditions. A CTA and MRI of the brain, ESR and CRP were normal. His history of diabetes, hypertension and dyslipidemia supported the diagnosis of a left non-arteritic microvascular ischemic 3rd nerve palsy. At his 3-month follow-up appointment, his ptosis and diplopia resolved.
Further reading:
-
Wong, GK, Boet R, Poon WS, Yu S, Lam JM. A review of isolated third nerve palsy without subarachnoid hemorrhage using computed tomographic angiography as the first line of investigation. Clin Neurol Neurosurg 2004;107(1):27-31. https://www.ncbi.nlm.nih.gov/pubmed/15567549
-
Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol 2007;25:257-268. https://www.ncbi.nlm.nih.gov/pubmed/17577867
-
Newman NJ, Biousse V. Third nerve palsies – Less frequent but just as concerning. JAMA Ophthalmol 2017;135(1):29-30. https://www.ncbi.nlm.nih.gov/pubmed/27892993
-
Micieli JA, Newman NJ, Barrow DL, Biousse V. Intracranial aneurysms of neuro-ophthalmologic relevance. J Neuroophthalmol 2017;37(4):421-439. https://www.ncbi.nlm.nih.gov/pubmed/28665866