1
1. Which of the following is true regarding the principles of Magnetic Resonance Imaging (MRI)?
- MRI does not use ionizing radiation
- One of the most important factors determining signal intensity on MRI is the concentration of protons in the tissue
- T1 and T2 relaxation times define the way protons return to their original resting state after being stimulated by the magnetic field
- Blood flow in the vessels produces a flow void on MRI
- All of the above
1. Which of the following is true regarding the principles of Magnetic Resonance Imaging (MRI)? 5. All of the above
Magentic resonance imaging is a non-invasive imaging method that uses the magnetic spin property of protons (Hydrogen ions) to generate diagnostic images. Protons normally spin around their axes, which have random orientations. In a strong magnetic field, the protons’ axes all line up and radio frequency pulses are used to push the aligned protons to a higher energy level. When the radio frequency source is turned off, the magnetic vector returns to its resting state and this causes a signal to be emitted, which is used to make the MRI images. T1 relaxation is the time taken for the magnetic vector to return to its resting state and T2 relaxation is the time needed for the axial spin to return to its resting state. Since different tissues have different proton densities and relaxation times, they can be identified separately. MRI does not use ionizing radiation.
2. What MRI sequence is shown below?
- T1
- T2
- FLAIR
- None of the above
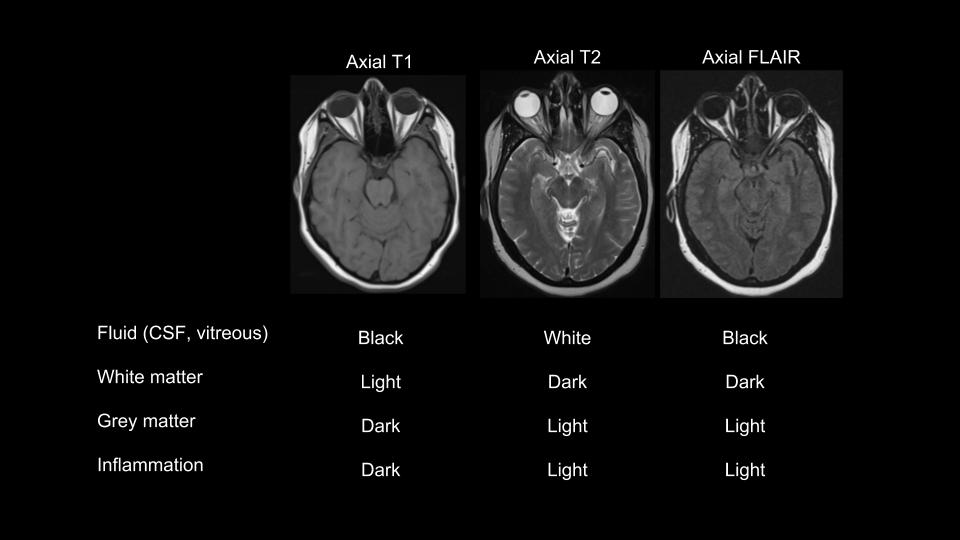
2. What MRI sequence is shown below? 2. T2
By looking at the color of fluid (cerebrospinal fluid (CSF) or vitreous) and the white and grey matter, the MRI sequence can be easily determined. Fluid is dark on a T1 image and bright on a T2 image. Fluid attenuation inversion recovery (FLAIR) is an MRI sequence that is derived from T2, but suppresses the high fluid signal. Therefore, both T1 and FLAIR will have dark fluid signals. The way to differentiate between T1 and FLAIR is to look at the color of the white and grey matter. On T1, the white matter is lighter than the outer grey matter whereas on a FLAIR image, the grey matter is a lighter color than the white matter as shown in the images below.
3. A Coronal T2 MRI is shown below. Which letter represents the right optic nerve?
- a
- b
- c
- d
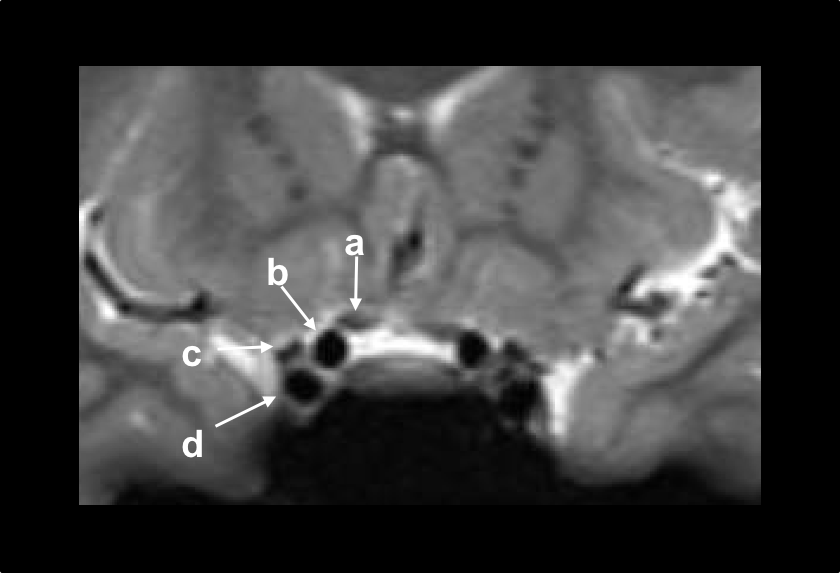
3. A Coronal T2 MRI is shown below. Which letter represents the right optic nerve? 1. a
The right optic nerve is represented by the white arrow labelled (a) and is located above the carotid flow voids (letters b and d). This coronal cross-section image shows the pre-chiasmatic optic nerves.
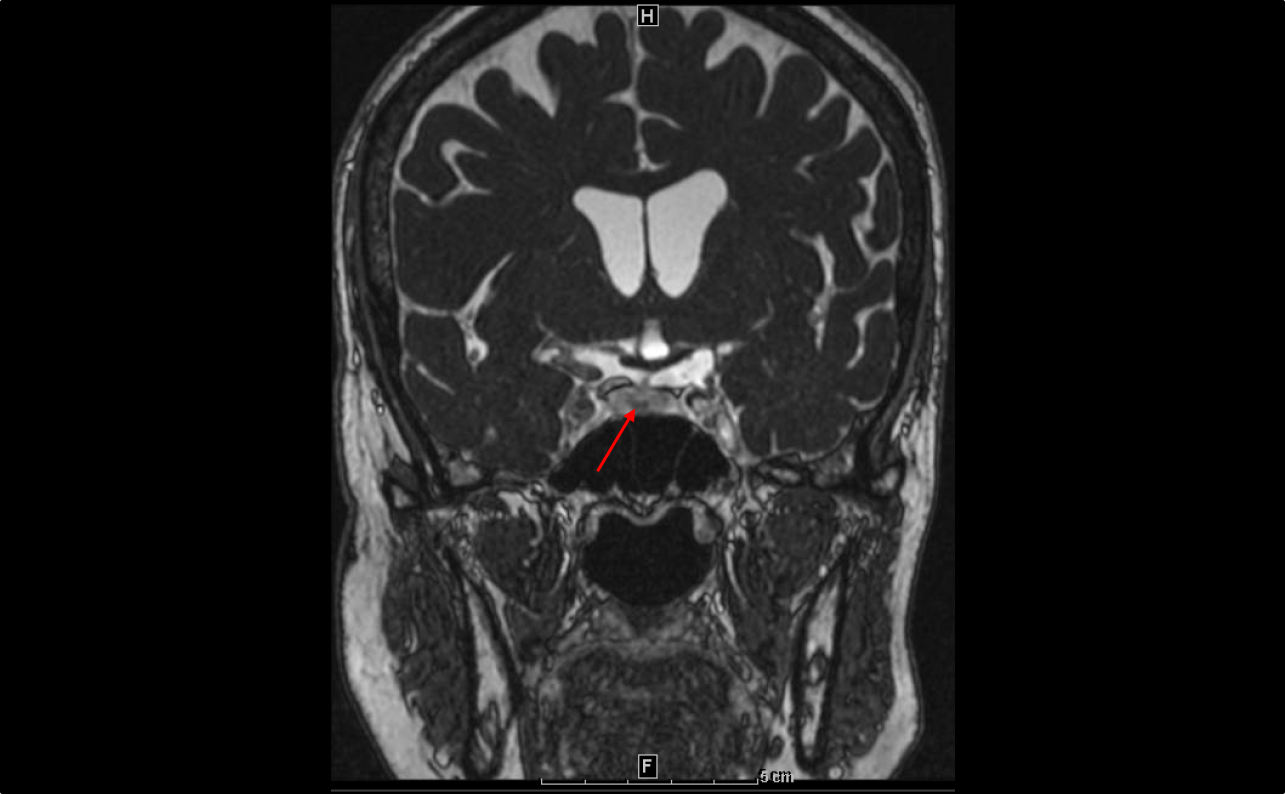
4. A Coronal T2 MRI of the brain is shown below. What structure is indicated by the red arrow?
- Internal carotid artery aneurysm
- Craniopharyngioma
- Pituitary gland
- Sellar cyst
4. A Coronal T2 MRI of the brain is shown below. What structure is indicated by the red arrow? 3. Pituitary gland
The pituitary gland lies below the optic chiasm. It is important to be familiar with the sellar and suprasellar structures since tumors such as pituitary adenomas may arise from this area and compress the anterior visual pathways.
5. What is the difference between these two MRI sequences?
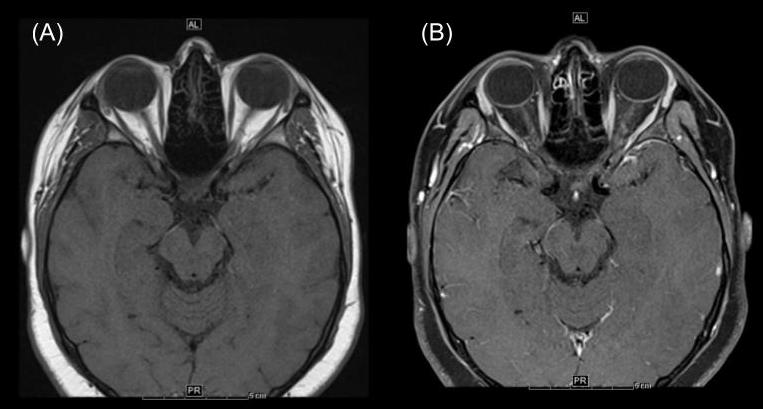
- MRI (A) is T1 and MRI (B) is T2
- MRI (A) is T1 and MRI (B) is FLAIR
- MRI (A) is T1 with contrast and MRI (B) is T1 without contrast
- MRI (A) is T1 and MRI (B) is T1 with fat suppression
5. What is the difference between these two MRI sequences? 4. MRI (A) is T1 and MRI (B) is T1 with fat suppression
The two MRI images are similar in that vitreous and CSF are dark, white matter is lighter and grey matter is darker. The most obvious difference between the images is that the bright orbital fat in MRI (A) is dark in MRI (B) since the fat signal is suppressed. Both MRIs are T1, but MRI (B) has fat suppression. This is one of the most important MRI sequences in neuro-ophthalmology since the suppression of the high fat signal is very helpful in determining whether the optic nerve is enhancing. Enhancement of the optic nerve is seen as a bright signal within the optic nerve after administration of gadolinium due to breakdown of the blood-optic nerve barrier.
Clinical Pearl
Enhancement of the optic nerves is best assessed on T1 MRI of the orbits with gadolinium and fat suppression.
6. A patient has an acute bilateral optic neuropathy. Which of the following is the best neuroimaging test for this patient?
- MRI of the brain without contrast
- MRI of the brain with contrast
- MRI of the brain and orbits without contrast and repeated on another day with contrast if the non-contrast scan is abnormal
- MRI of the brain and orbits with contrast
6. A patient has an acute bilateral optic neuropathy. Which of the following is the best neuroimaging test for this patient? 4. MRI of the brain and orbits with contrast
MRI of the orbits is a very important imaging modality used to evaluate patients with optic neuropathies since it includes fine cuts (typically 3mm) through the orbits allowing for the orbital contents and anterior visual pathways to be assessed in detail. MRI of the brain does include some views of the orbits, but these are typically thick slices (usually 5mm) and may miss important orbital changes. Gadolinium-containing contrast should be given in almost all cases since it allows for the assessment of optic nerve enhancement and the detection of subtle changes around the optic nerve. Small compressive lesions such as optic nerve sheath meningiomas may be missed if MRI of the orbits is performed without contrast.
7. A patient presents with bilateral optic disc edema. What is the pertinent finding in the MRI of the orbits with gadolinium shown below?
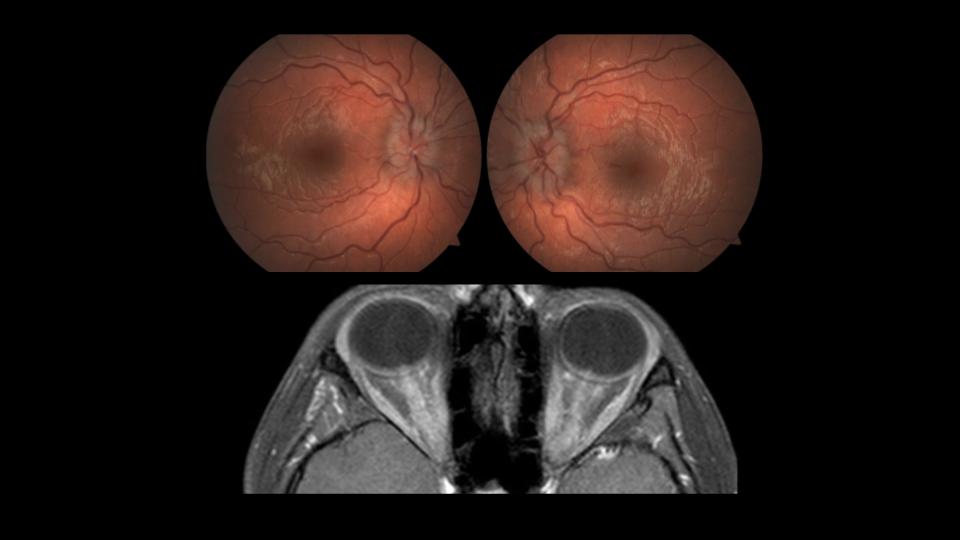
- Enlargement of the extraocular muscles
- Compression of the optic nerves by an intraorbital mass
- Post-surgical changes in the orbit
- Enhancement of both optic nerves
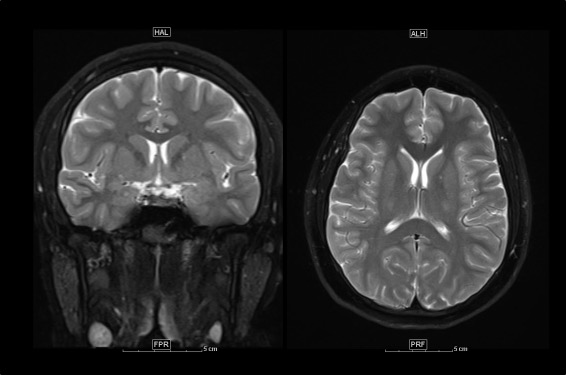
7. A patient presents with bilateral optic disc edema. What is the pertinent finding in the MRI of the orbits with gadolinium shown below? 4. Enhancement of both optic nerves
In this patient with bilateral optic disc edema, there is significant enhancement of both optic nerves (whitish appearance of both optic nerves). This is due to bilateral optic neuritis, which causes breakdown of the blood-optic nerve barrier and allows gadolinium contrast to enter the optic nerve substance.
Clinical Pearl
Optic nerve enhancement is a characteristic feature seen in patients with optic neuritis.
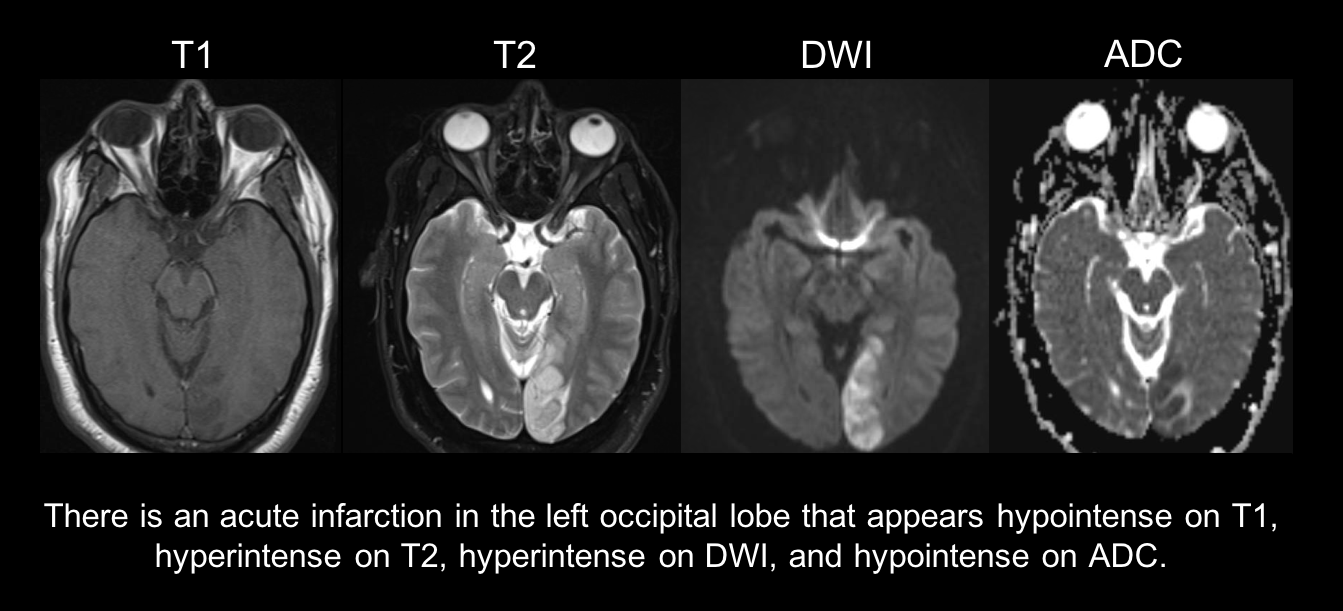
8. A patient has sudden loss of vision on the right side of his visual field in both eyes due to a left occipital lobe ischemic stroke. How do you expect the signal in the area of the stroke to appear on the various MRI sequences if it was acquired 3 days after vision loss? (DWI: diffusion weighted imaging, ADC: apparent diffusion coefficient)
- T1: hyperintense, T2: hyperintense, DWI: hyperintense, ADC: hypointense
- T1: hypointense, T2: hypointense, DWI: hyperintense, ADC: hyperintense
- T1: hypointense, T2: hyperintense, DWI: hyperintense, ADC: hypointense
- T1: hyperintense, T2: hyperintense, DWI: hypointense, ADC: hyperintense
8. A patient has sudden loss of vision on the right side of his visual field in both eyes due to a left occipital lobe ischemic stroke. How do you expect the signal in the area of the stroke to appear on the various MRI sequences if it was acquired 3 days after vision loss? 3. T1: hypointense, T2: hyperintense, DWI: hyperintense, ADC: hypointense
Diffusion weighted imaging (DWI) is a form of MRI that makes use of the random microscopic motion of water protons (Brownian motion). In the setting of acute cerebral ischemia, water enters the cell due to failure of the cell membrane ion pump leading to cytotoxic edema and restricted diffusion. This manifests as a high signal on DWI and a low signal on apparent diffusion coefficient (ADC), which is a measure of the magnitude of diffusion within the tissue. T1 images show a hypointense signal and T2 images show a hyperintense signal in the area of infarction as demonstrated below. Increased T2 signal due to vasogenic edema and can “shine through” on DWI images making it difficult to distinguish vasogenic from cytotoxic edema. It is therefore important to look at the ADC map since cytotoxic edema from an ischemic stroke will appear hypointense due to decreased water diffusion whereas vasogenic edema will appear as a hyperintense signal.
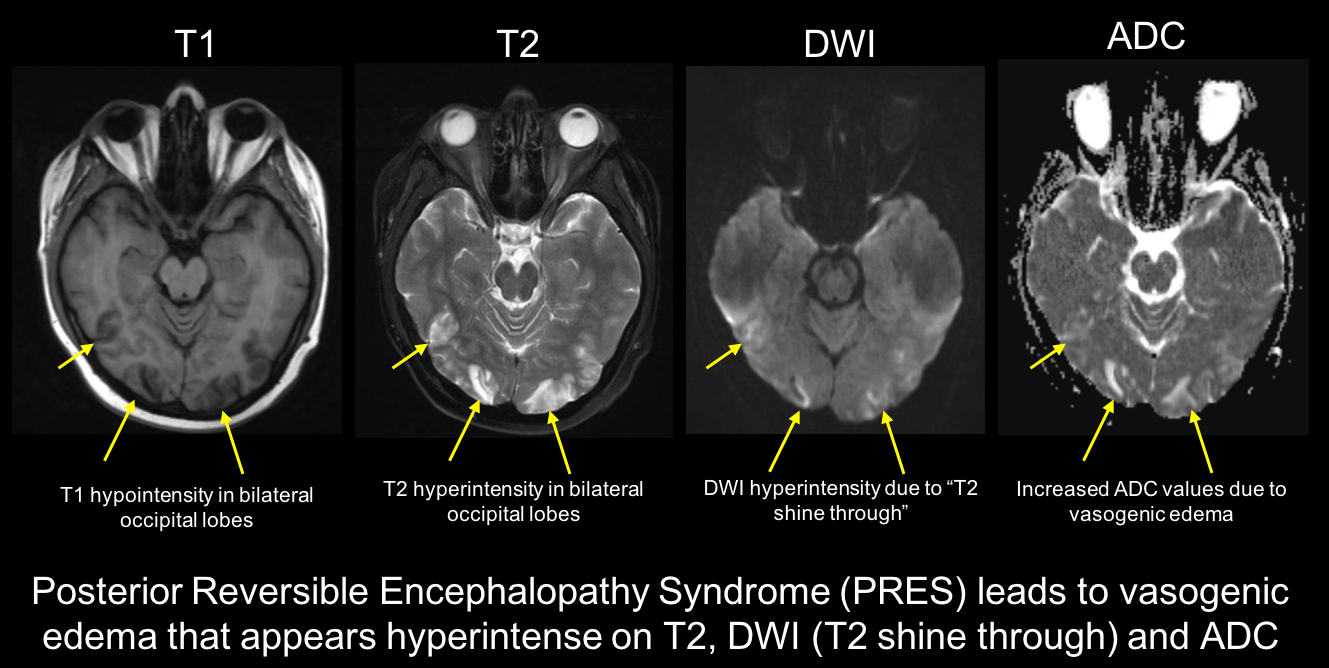
9. A patient taking tacrolimus after a bone marrow transplant has a severe, sudden onset headache and bilateral vision loss. Her dilated fundus examination is normal and her pupils are reactive. MRI of the brain is shown below. What is the most likely diagnosis?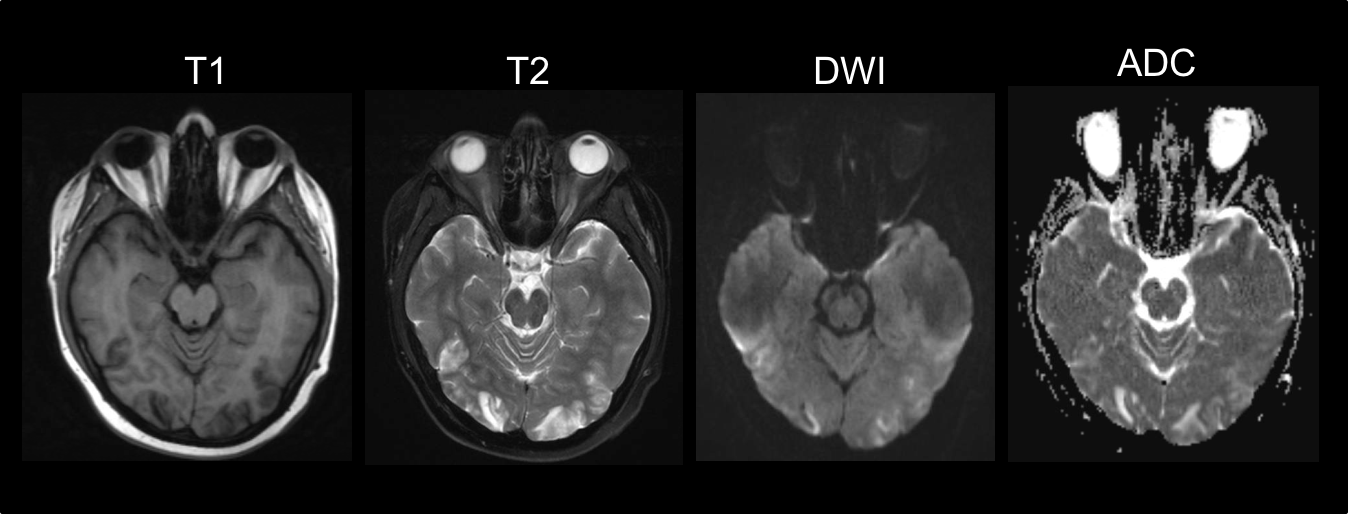
- Bilateral occipital lobe infarcts
- Posterior reversible encephalopathy syndrome
- Bilateral occipital lobe hemorrhage
- Carbon monoxide poisoning
9. A patient taking tacrolimus after a bone marrow transplant has a severe, sudden onset headache and bilateral vision loss. Her dilated fundus examination is normal and her pupils are reactive. MRI of the brain is shown below. What is the most likely diagnosis? 2. Posterior reversible encephalopathy syndrome
This patient has posterior reversible encephalopathy syndrome (PRES), which is a syndrome characterized by headaches, vision loss, seizures and confusion. It is thought to be a result of disordered cerebral autoregulation and endothelial function mainly in the posterior circulation. Presdisposing factors include cytotoxic immunosuppressive therapy, hypertension and eclampsia. MRI of the brain demonstrates vasogenic edema, which is visualized as increased signal on T2, hypo- or iso-intense lesions on DWI (although may be hyperintense due to T2 shine through) and increased signal on ADC maps as shown below. There is a good prognosis and the condition usually fully reverses within days to weeks.
10. Which of the following is true regarding the use of gadolinium during pregnancy?
- It is category A and controlled human studies show no risk
- It is category B and there is no evidence of risk in studies
- It is category C and risk cannot be ruled out
- It is category D and there is positive evidence of risk
10. Which of the following is true regarding the use of gadolinium during pregnancy? 3. It is category C and risk cannot be ruled out
Gadolinium is the contrast agent most commonly used with MRI. It crosses the placenta, is excreted by the fetus into the amniotic fluid, and may be swallowed and reabsorbed into the fetal circulation where it has a long half life. It is classified as Category C, meaning that animal reproduction studies have shown an adverse effect on the fetus, but there are no adequate well-controlled studies in humans. The largest human study comparing gadolinium MRI during pregnancy (n = 397) compared to no MRI (n = 1,418,451) reported that gadolinium use at any time during pregnancy was associated with an increased risk of inflammatory, rheumatological or infiltrative skin conditions (adjusted Hazard ratio 1.36, 95% CI 1.09-1.69) and still births and neonatal deaths (adjusted relative risk 3.70, 95% CI 1.55-8.85). It is therefore not recommended during pregnancy unless the benefit outweighs the potential risk to the fetus.
11. A patient has chronic renal failure and is on hemodialysis. What condition is she at higher risk for after receiving a gadolinium-containing contrast agent for an MRI of the brain and orbits?
- Multiple sclerosis
- Nephrogenic systemic fibrosis
- Rheumatoid arthritis
- Chronic Obstructive Pulmonary Disease
11. A patient has chronic renal failure and is on hemodialysis. What condition is she at higher risk for after receiving a gadolinium-containing contrast agent for an MRI of the brain and orbits? 2. Nephrogenic systemic fibrosis
Nephrogenic systemic fibrosis (NSF) is a fibrosing disorder characterized by thickening and hardening of the skin overlying the trunk and extremities, which occurs only in patients with renal failure. Gadolinium-containing contrast agents are excreted exclusively by the kidney and have been implicated in the development of NSF. The latent period between exposure to gadolinium and onset is usually 2 to 4 weeks. The risks, benefits, and alternatives should be discussed with a patient with renal failure who must have an MRI with gadolinium. The patient’s nephrologist should be informed and it is recommended, especially in patients with a low estimated glomerular filtration rate, that a hemodialysis session occur as soon as possible after gadolinium administration.
Clinical Pearl
Gadolinium should be used with caution in patients with renal failure and in consultation with the patient’s nephrologist.
12. Which of the following is true regarding the principles of computed tomography (CT) imaging?
- It uses non-ionizing radiation
- It uses x-rays to build cross-sectional images of the body
- The higher the attenuation of the x-ray beam, the darker it appears on CT images
- Bone and calcification typically appear dark whereas air and fat appear white
12. Which of the following is true regarding the principles of computed tomography (CT) imaging? 2. It uses x-rays to build cross-sectional images of the body
CT is a diagnostic imaging modality that uses x-rays to build cross-sectional images of the body. As the x-rays pass through the patient, they are attenuated by each type of tissue. The higher the attenuation of the x-ray beam, the brighter the tissue appears on a CT image. Bone and calcifications significantly attenuate the x-ray beam and appear white whereas air causes little attenuation and appears black.
13. Which of the following is the best indication for a CT scan of the orbits?
- A patient with a suspected orbital floor fracture
- A patient with suspected bilateral optic neuritis
- A patient with suspected ischemic optic neuropathy
- A patient with monocular diplopia
13. Which of the following is the best indication for a CT scan of the orbits? 1. A patient with a suspected orbital floor fracture
CT scanning is very helpful in assessing bony anatomy and would be the initial imaging choice for a patient with a suspected orbital bone fracture (see image below). CT scanning would not typically be used for evaluating patients with optic neuropathies such as optic neuritis since this is best evaluated with an MRI of the orbits with contrast. Monocular diplopia does not require neuroimaging since it is a result of ocular changes.

14. What abnormality is seen on the CT scan of the head shown below in this patient with vision loss on the right side of his visual field?
- There is hydrocephalus
- There is a left occipital acute/subacute infarct
- There is a right parietal acute/subacute infarct
- The CT scan is normal and a detailed eye examination should be performed
14. What abnormality is seen on the CT scan of the head shown below? 2. There is a left occipital acute/subacute infarct
This is a patient that presented with acute loss of vision on the right side of his visual field due to a left occipital stroke. The CT scan performed 24 hours after the vision loss shows an area of cortical hypodensity (red arrows) in the left occipital lobe. This corresponds to the area of hyperintensity seen on the DWI MRI (blue arrows).
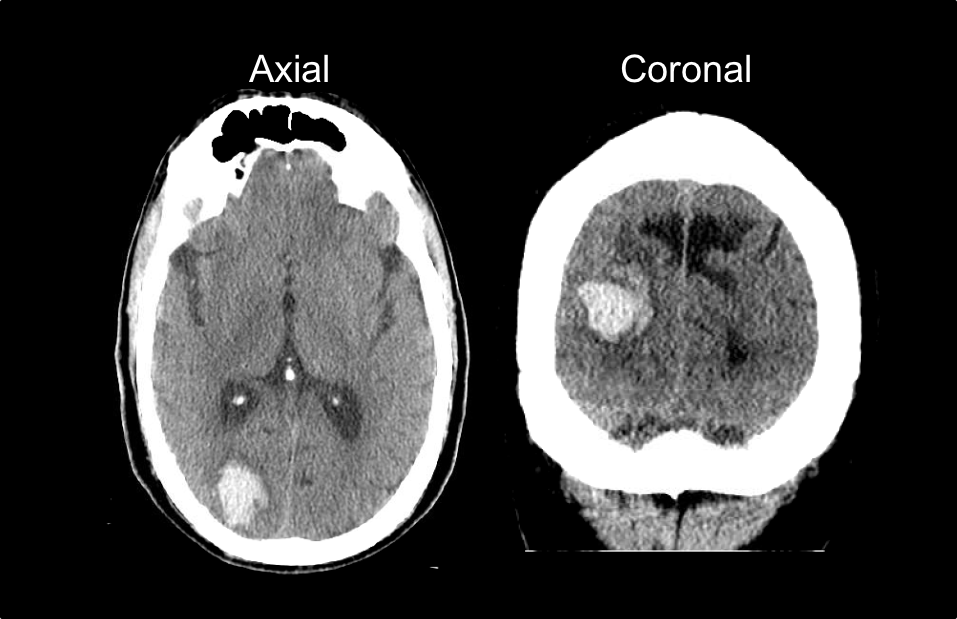
 15. A patient has sudden loss of vision on the left side of his visual field in both eyes. What is the most pertinent finding on his CT scan shown below?
15. A patient has sudden loss of vision on the left side of his visual field in both eyes. What is the most pertinent finding on his CT scan shown below?
- Right occipital foreign body
- Subarachnoid hemorrhage
- Right occipital intraparenchymal hemorrhage
- Right subdural hemorrhage
15. A patient has sudden loss of vision on the left side of his visual field in both eyes. What is the most pertinent finding on his CT scan shown below? 3. Right occipital intraparenchymal hemorrhage
CT scan is almost always the first imaging modality used in patients with suspected stroke. Acute blood appears markedly hyperdense compared to the surrounding brain parenchyma. This patient has a right occipital intraparenchymal hemorrhage that is causing a left homonymous hemianopia. Potential reasons for this bleed include hypertension, infarction with hemorrhagic conversion, underlying mass lesion or a vascular malformation.
16. A patient presents to the ED with a sudden onset severe headache. What is the most important finding from the CT scan shown below?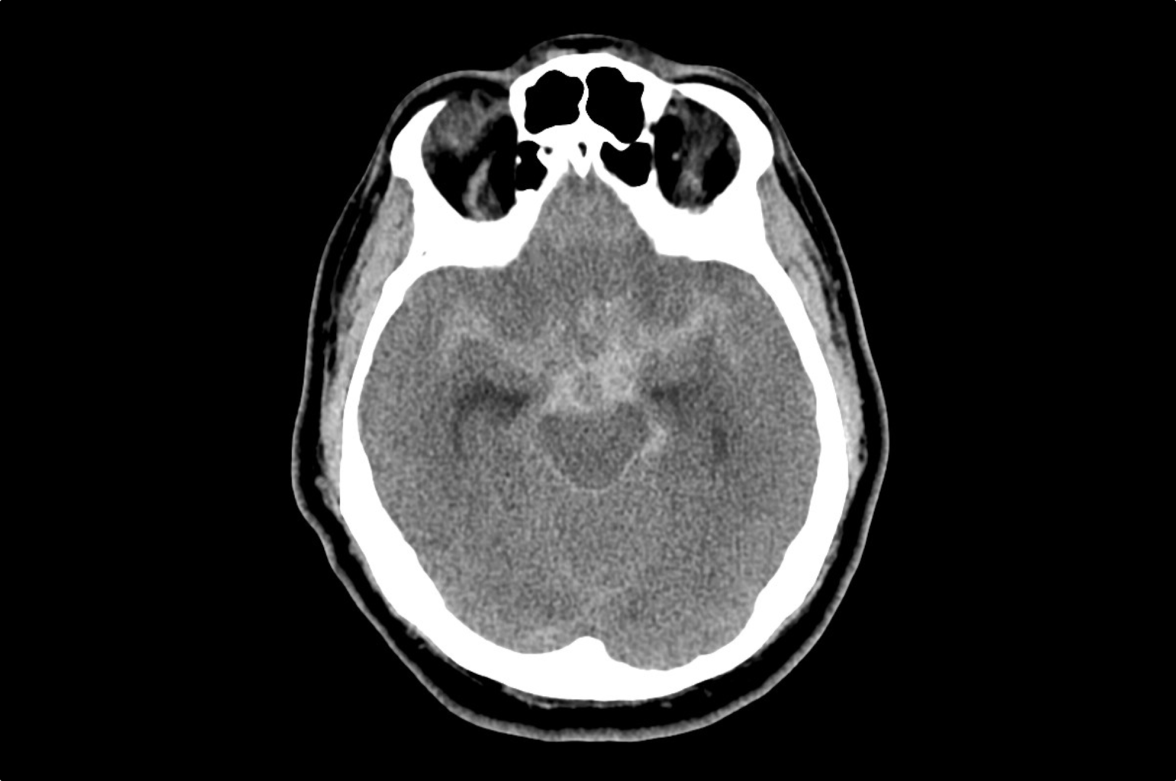
- Pituitary apoplexy
- Midline shift
- Subarachnoid hemorrhage
- Subdural hemorrhage
16. A patient presents to the ED with a sudden onset severe headache. What is the most important finding from the CT scan shown below? 3. Subarachnoid hemorrhage
A subarachnoid hemorrhage is bleeding into the subarachnoid space, which is the area between the arachnoid and and pia mater surrounding the brain. The most common causes are trauma and rupture of an intracranial aneurysm. An unenhanced head CT is the imaging of choice in a patient suspected of a subarachnoid hemorrhage. When it is performed within the first 24 hours, CT has a sensitivity of 95%, but this falls to approximately 50% after 7 days. It appears as a hyperdensity in the subarachnoid spaces and usually involves the basal cisternae, inter-hemispheric sulci and lateral sulci. There is a high morbidity and mortality associated with subarachnoid hemorrhage. 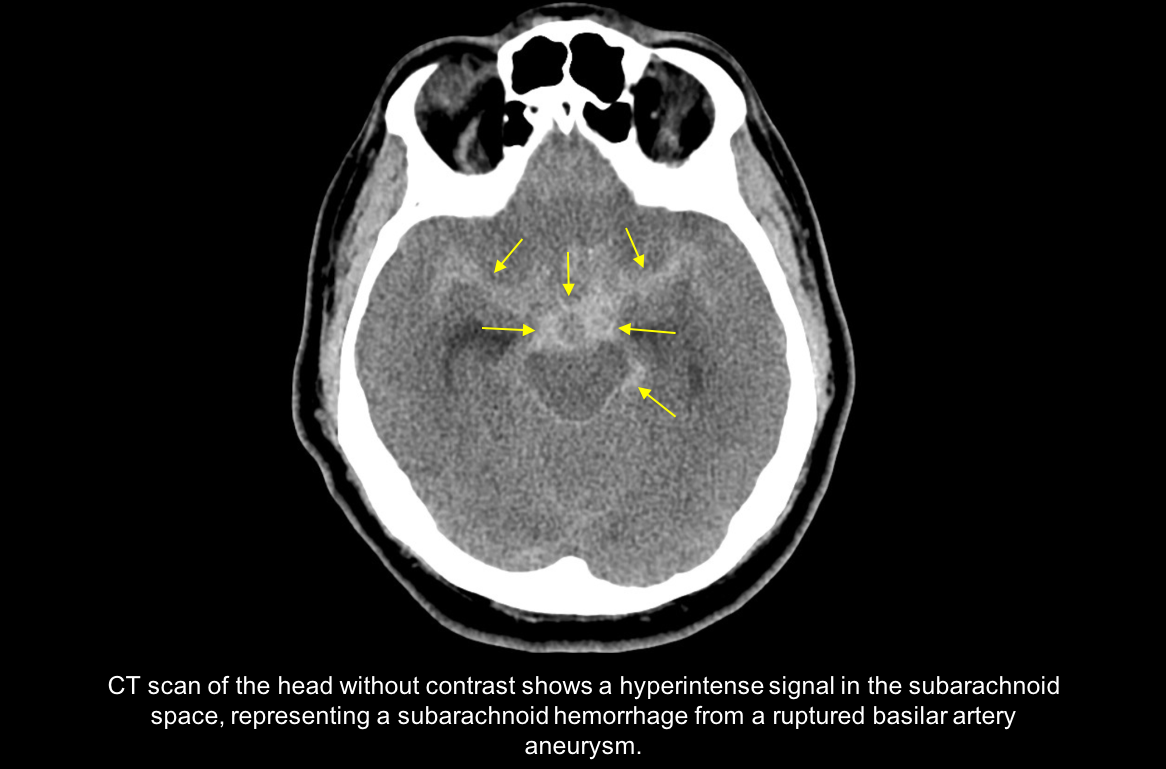
17. An eye examination is requested on the previous patient with the subarachnoid hemorrhage. After dilation, the fundus cannot be well-visualized due to a vitreous hemorrhage. The combination of a vitreous hemorrhage and subarachnoid hemorrhage is called?
- Miller-Fisher syndrome
- Terson syndrome
- Millard-Gubler syndrome
- Parson’s syndrome
17. An eye examination is requested on the patient with the subarachnoid hemorrhage. After dilation, the fundus cannot be well-visualized due to a vitreous hemorrhage. The combination of this vitreous hemorrhage and subarachnoid hemorrhage is called? 2. Terson syndrome
Terson syndrome is the combination of a subarachnoid hemorrhage and any intraocular hemorrhage (vitreous, subretinal, intraretinal, and subhyaloid). It is thought that the sudden rise of intracranial pressure leads to orbital venous hypertension and rupture of peripapillary, papillary, or retinal capillaries. Terson syndrome is associated with worse outcomes in patients with subarachnoid haemorrhages.
18. A magnetic resonance angiography (MRA) image is shown below. Which structure is indicated by the red arrow?
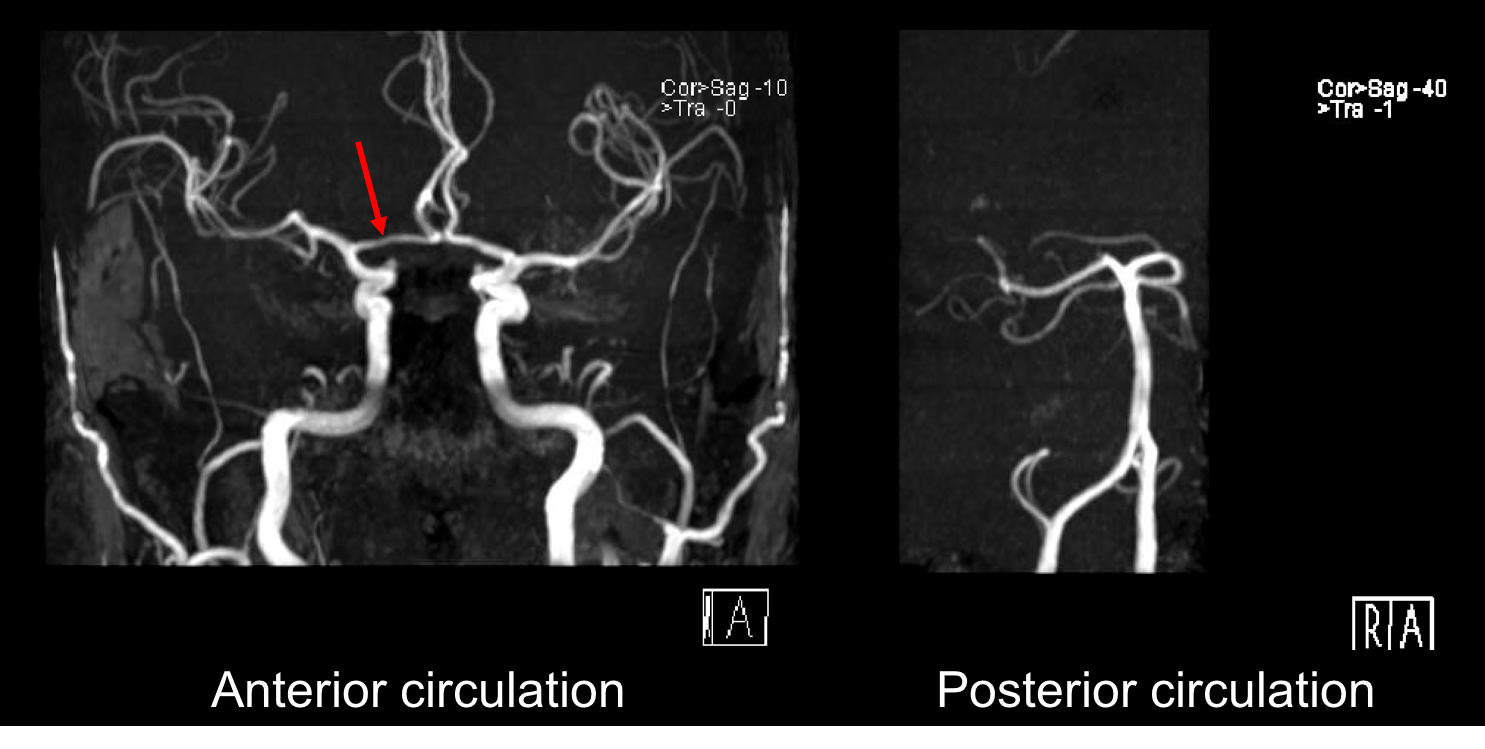
- Anterior communicating artery
- Posterior communicating artery
- Anterior cerebral artery
- Posterior cerebral artery
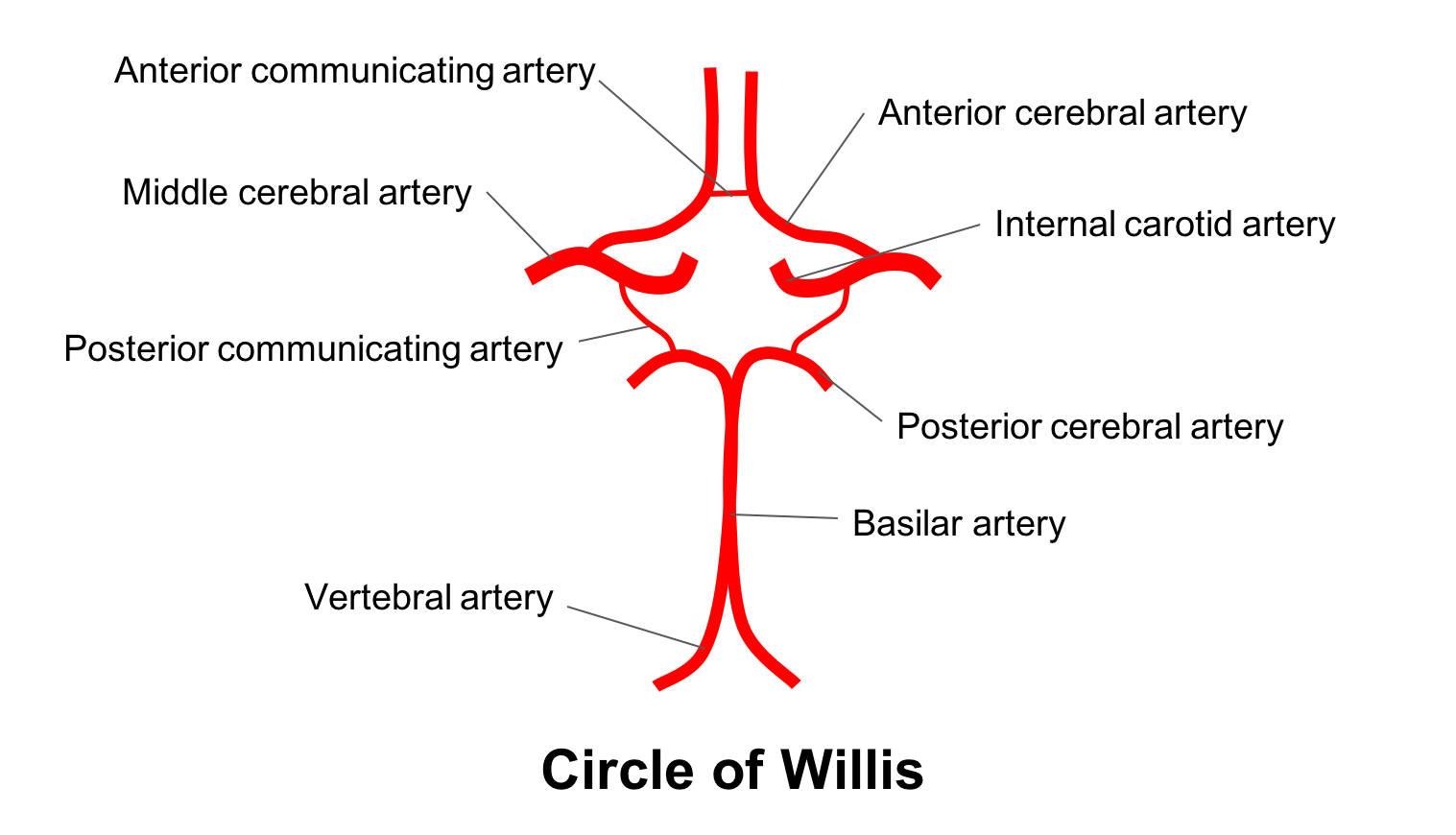
18. A magnetic resonance angiography (MRA) image is shown below. Which structure is indicated by the red arrow? 3. Anterior cerebral artery
MRA is a useful test for assessing the intracranial arterial circulation. This is of particular importance when an intracranial aneurysm, dural arteriovenous fistula or carotid stenosis is suspected. The red arrow is pointing to the A1 segment of the anterior cerebral artery. The anatomy of the circle of Willis is summarized below.
19. Which of the following is true regarding the detection of intracranial aneurysms by MRA and CTA?
- MRA is superior to CTA and should be obtained when possible
- MRA and CTA have similar diagnostic results
- MRA is a faster test to obtain and is generally preferable to CTA
- CTA does not use contrast and is preferred in patients with renal failure
19. Which of the following is true regarding the detection of intracranial aneurysms by MRA and CTA? 2. MRA and CTA have similar diagnostic results
Magnetic resonance angiography and CTA are generally accepted to have similar diagnostic results for the detection of intracranial aneurysms, although CTA has slightly higher spatial resolution. Both can reliably detect aneurysms greater than 3 mm. There are advantages and disadvantages to each imaging modality. Computed tomography angiography can obtain images faster and is preferred in the acute setting such as trauma, but uses ionizing radiation. Magnetic resonance angiography can be obtained at the same time as MRI of the brain, which is often required for patients with neuro-ophthalmic conditions. Ultimately, the decision to obtain an MRA or CTA will depend on the availability of each and the preference of the neuroradiologist interpreting the images.
20. Which of the following is the best indication for the imaging test shown below?
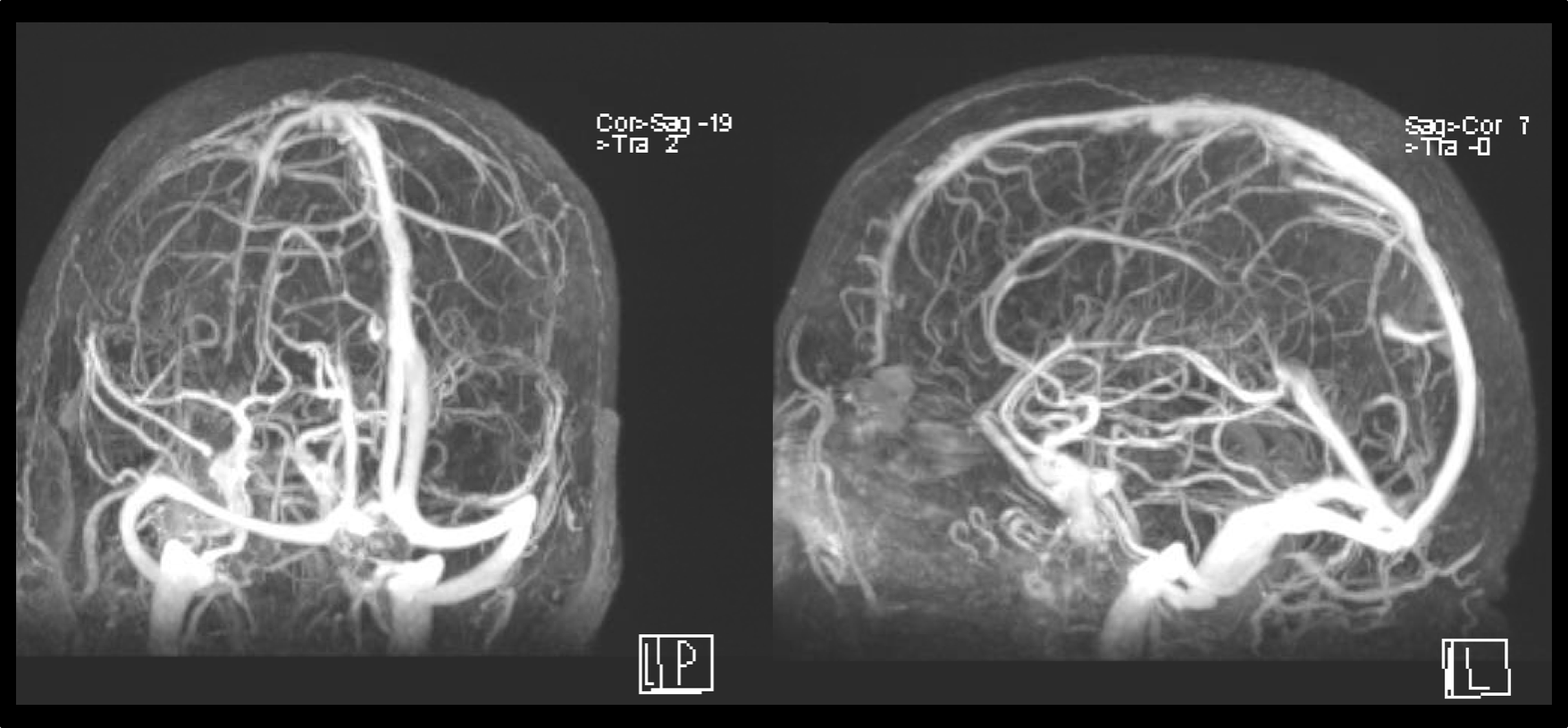

- Acute 3rd nerve palsy
- Papilledema
- Eyelid retraction
- Acute 4th nerve palsy
20. Which of the following is the best indication for the imaging test shown below? 2. Papilledema
The imaging test shown in the figure is a magnetic resonance venogram (MRV) of the head, which is used to visualize the veins and venous sinuses in the head. In neuro-ophthalmology, it is typically obtained in patients with papilledema or other signs of elevated intracranial pressure since dural venous sinus thrombosis may lead to impairment of cerebrospinal fluid resorption and intracranial hypertension. The anatomy of the venous sinuses seen on MRV is summarized below.
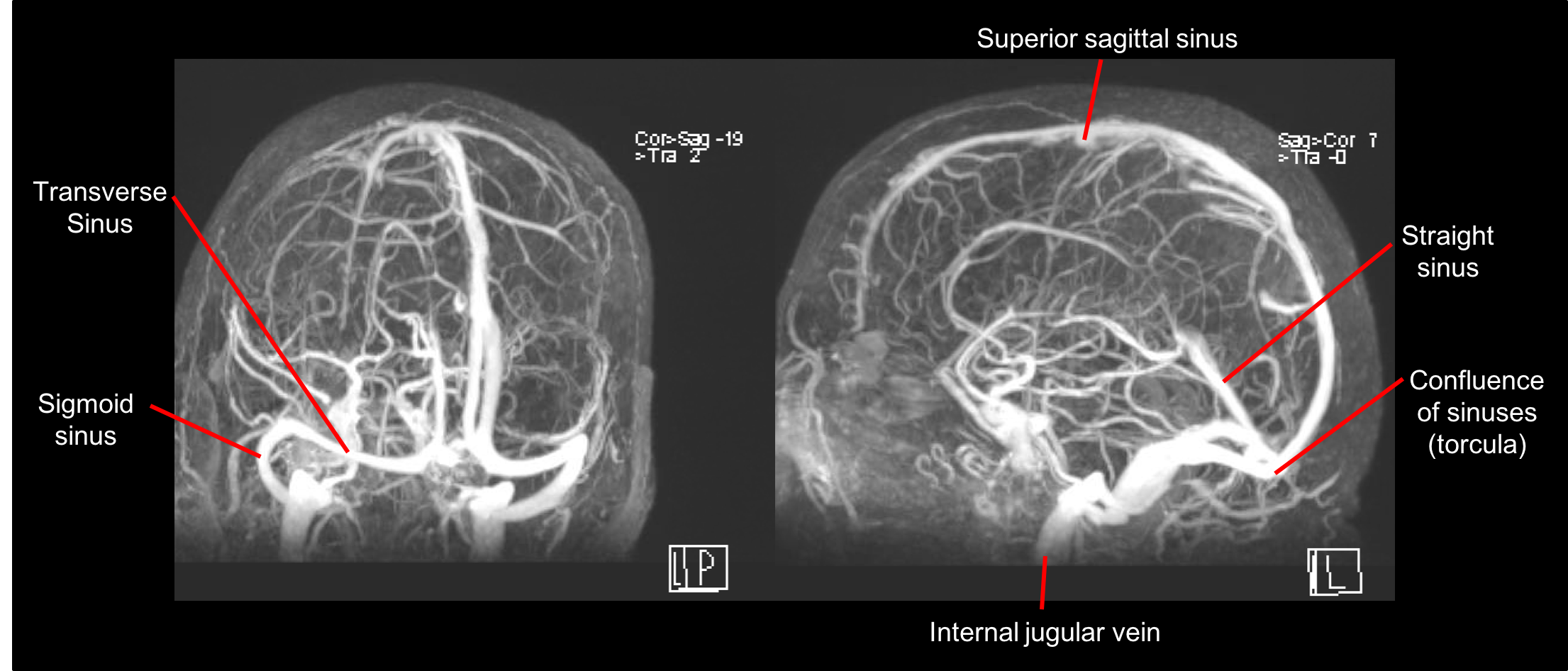
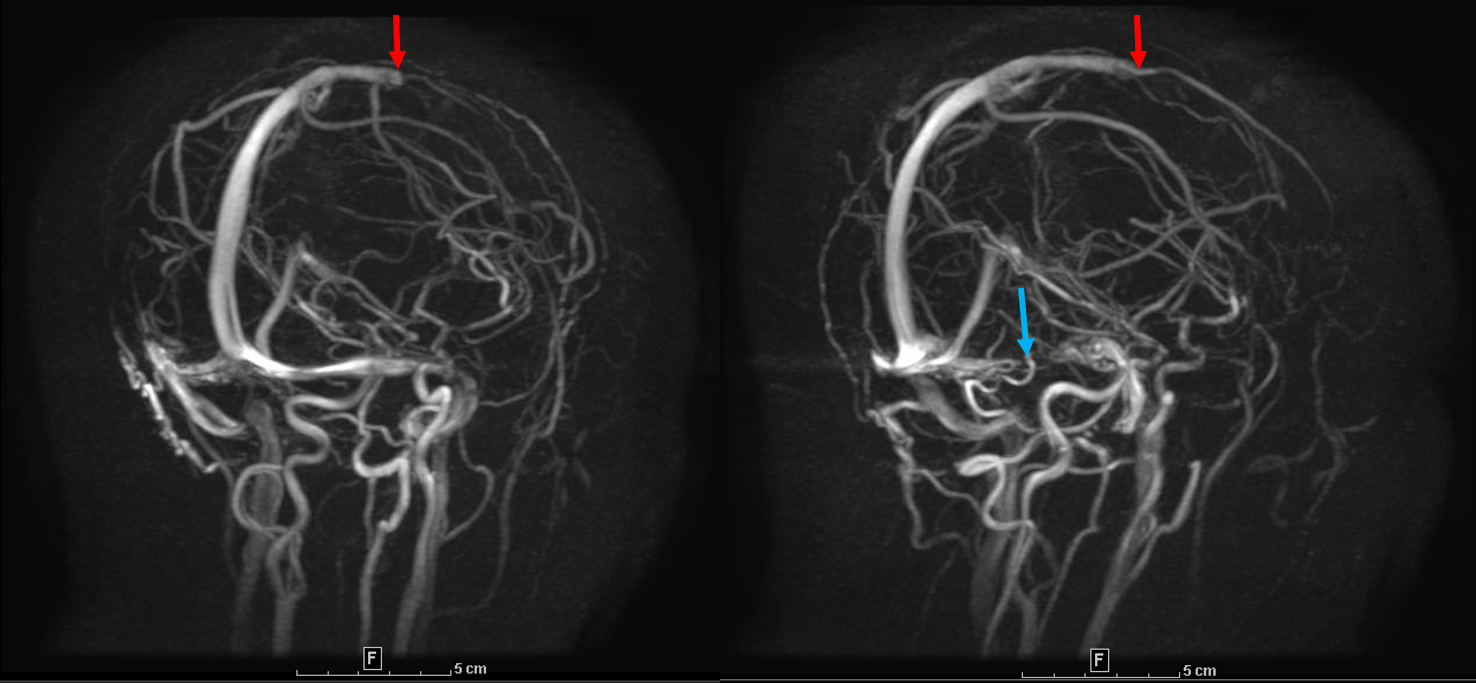
21. A patient presents with headache, papilledema and a 6th nerve palsy. What is the most prominent finding in the MRV from this patient shown below?
- Venous sinus thrombosis
- Venous sinus stent
- Arteriovenous malformation
- Venous sinus aneurysm
21. A patient presents with headache, papilledema and a 6th nerve palsy. What is the most prominent finding in the MRV from this patient shown below? 1. Venous sinus thrombosis
This patient has a filling defect consistent with venous sinus thrombosis in the superior sagittal (red arrow) and transverse (blue arrow) sinuses. Risk factors for venous sinus thrombosis include inherited thrombophilias, malignancy, medications, infection, pregnancy and head trauma. In neuro-ophthalmology, an MRV is usually obtained in patients with papilledema or other signs of intracranial hypertension to assess for venous sinus thrombosis.
Clinical Pearl
Magnetic resonance venography (MRV) should be performed in patients with papilledema or other signs of intracranial hypertension.
Further reading:
- Ray JG, Vermeulen MJ, Bharatha A, Montanera WJ, Park AL. Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA 2016;316(9):952. https://www.ncbi.nlm.nih.gov/pubmed/27599330
- Kuo PH, Kanal E, Abu-Alfa AK, Cowper SE. Gadolinium-based MR contrast agents and nephrogenic systemic fibrosis. Radiology 2007;242(3):647-9. https://www.ncbi.nlm.nih.gov/pubmed/17213364
- Costello FE, Goyal M. Neuroimaging in neuro-ophthalmology. Neurol Clin 2010;28:757-787. https://www.ncbi.nlm.nih.gov/pubmed/?term=PMID%3A+20637999
- Currie S, Hoggard N, Craven IJ, et al. Understanding MRI: basic MR physics for physicians. Postgrad Med J 2013;89:209-223. http://pmj.bmj.com/content/postgradmedj/89/1050/209.full.pdf
- Edijali M, Rodriguez-Regent C, Hodel J, et al. Subarachnoid hemorrhage in ten questions. Diagn Interv Imaging. 2015;96(7-8):657-66. https://www.ncbi.nlm.nih.gov/pubmed/?term=PMID%3A+26141485
- International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362(9378):103-110. https://www.ncbi.nlm.nih.gov/pubmed/12867109
- Nael K, Villablanca JP, Mossaz L, et al. 3-T contrast-enhanced MR angiography in evaluation of suspected intracranial aneurysm: comparison with MDCT angiography. AJR Am J Roentgenol. 2008;190:389–95. https://www.ajronline.org/doi/10.2214/AJR.07.2297