23
Case
Age: 42-year-old woman
Reason for referral to ophthalmology: Anisocoria
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and does not drink alcohol
HPI: Earlier in the morning, she was in a car accident and her neck was suddenly forced backwards and then forwards, but she did not lose consciousness and did not seek medical attention. Later that day, when she looked in the mirror, she noticed that her right pupil was smaller than the left. She has also had a right-sided headache and neck pain since the car accident, which prompted her to go to the emergency room and an ophthalmology consultation was requested. She showed a picture from her cell phone that showed her pupils were equal sizes the day before the accident.
Ophthalmological examination:
Blood pressure: 125/79, heart rate 80
Visual acuity: 20/20 OD, 20/20 OS
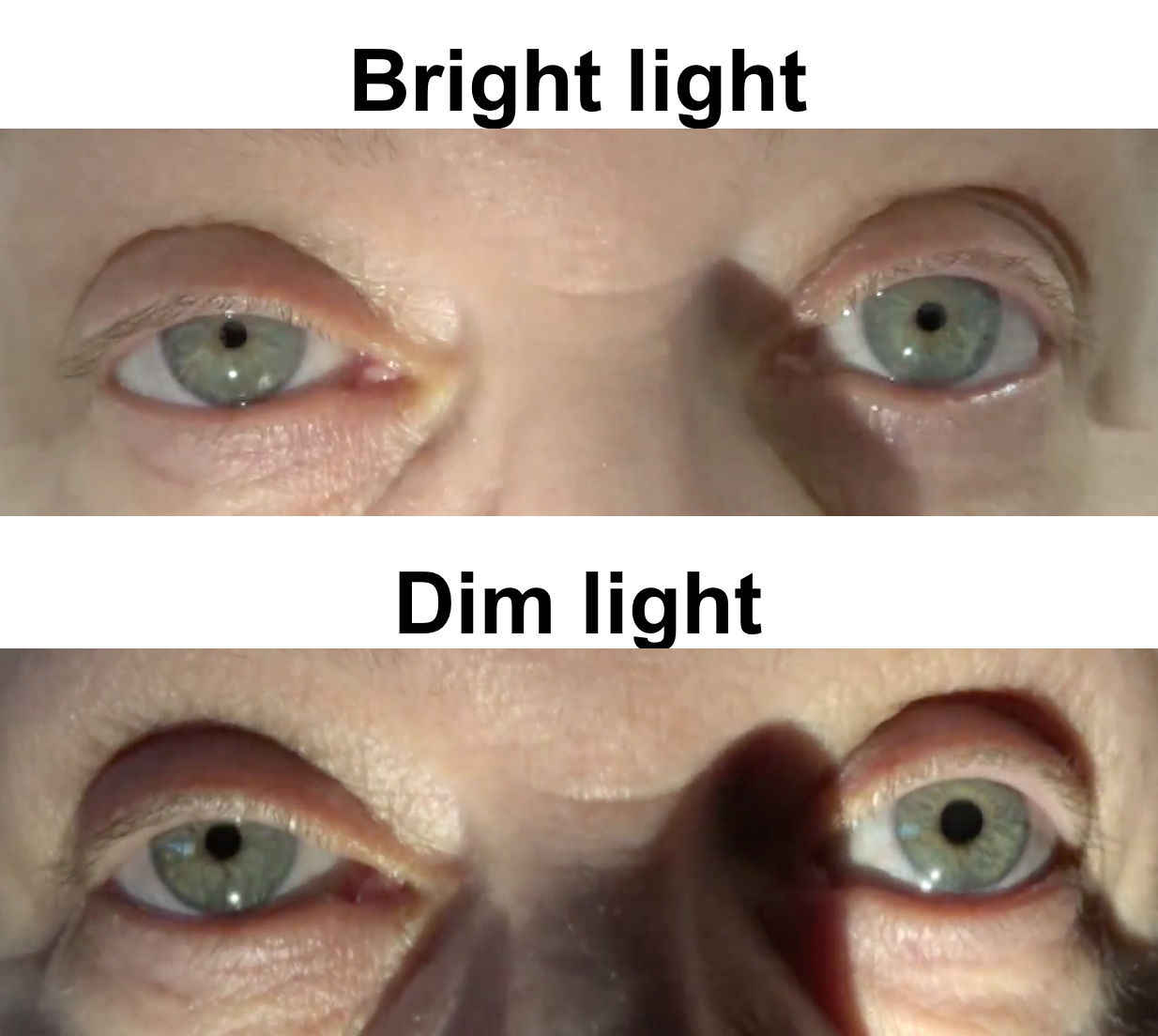
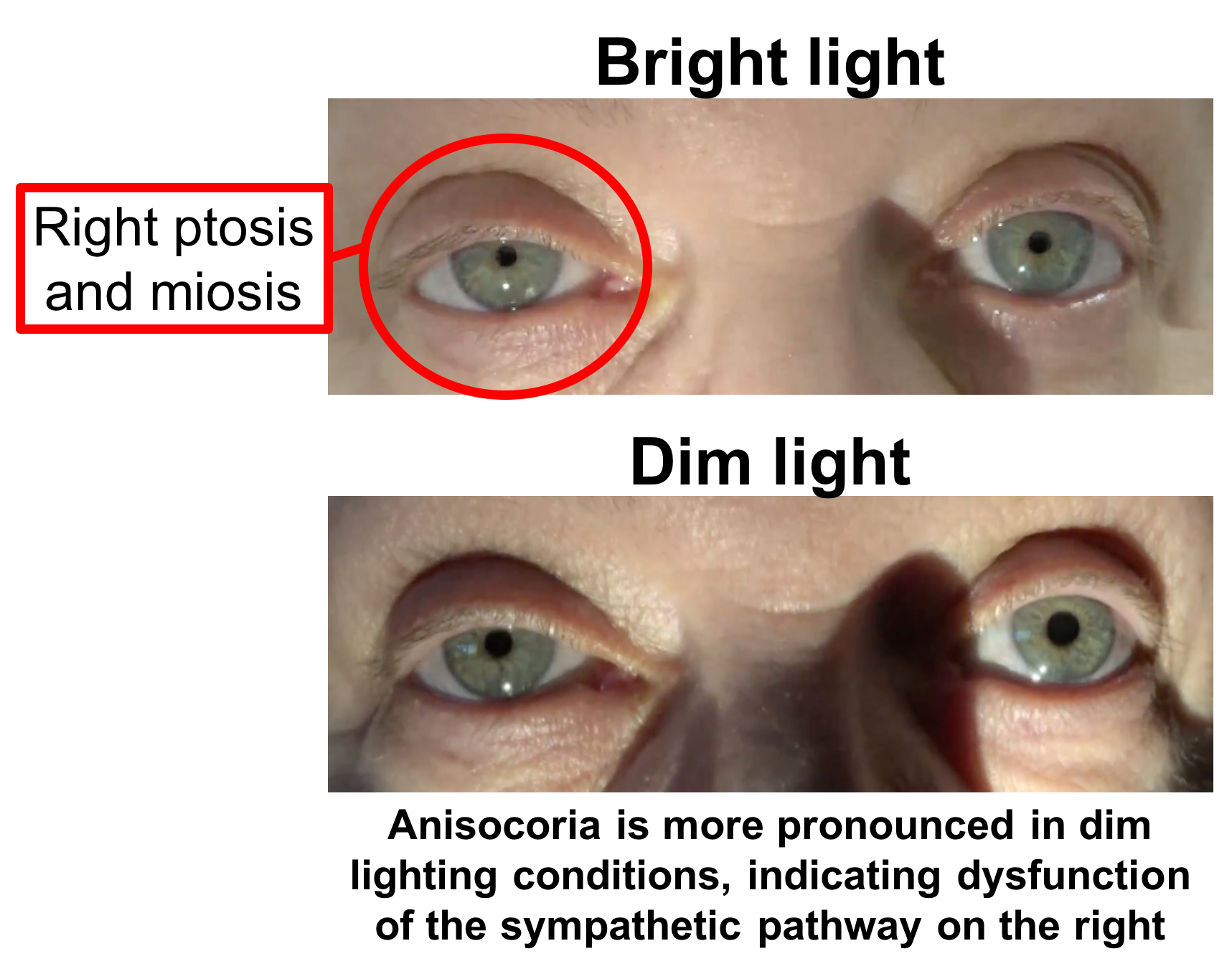
Pupillary examination is shown below
Color vision: 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is otherwise normal
1. What causes anisocoria that increases in the dark?
- Ocular conditions such as uveitis
- Horner’s syndrome
- Topical medications
- All of the above
1. What causes anisocoria that increases in dim light? 4. All of the above
When a patient presents with anisocoria (different pupil sizes), the most important next step is to determine which pupil is abnormal. This can be determined by measuring the degree of anisocoria in bright and dim light. If the difference is greater in dim light, the small pupil is abnormal. The differential diagnosis for this situation includes Horner’s syndrome (oculosympathetic paresis), ocular conditions (uveitis, pseudoexfoliation, pigment dispersion syndrome), or related to topical medications (Brimonidine used for unilateral glaucoma). Physiologic anisocoria may also sometimes cause anisocoria that is slightly greater in the dark.
Clinical Pearl
The differential diagnosis for anisocoria that increases in the dark includes:
- Horner’s syndrome
- Medication induced (Brimonidine, Pilocarpine)
- Ocular conditions (uveitis, pseudoexfoliation, pigment dispersion syndrome)
*Physiologic anisocoria may sometimes be slightly greater in the dark
2. Which eye do you expect to have a prominent relative afferent pupillary defect (RAPD)?
- Right eye since the pupil is larger
- Left eye since the pupil is smaller
- No prominent RAPD expected
- Both eyes will have an RAPD
2. Which eye do you expect to have a prominent relative afferent pupillary defect (RAPD)? 3. No prominent RAPD expected
The patient presents with anisocoria, which is a problem of the efferent pupillary pathway (sympathetic or parasympathetic pathway). An RAPD is present when there is a problem with the afferent pathway that carries the signal from the eye to the brainstem. Since the patient does not have vision loss or any other signs of an optic neuropathy, an RAPD is not expected in this case. Anisocoria may cause a trace RAPD in the eye with the smaller pupil since less light enters the visual pathway, but this is clinically insignificant (0.1 log unit for every 1 mm).
3. What examination finding would support a diagnosis of right Horner’s syndrome?
- Intraocular inflammation
- Dilation lag
- Iris transillumination defects
- Cogan’s lid twitch
3. What examination finding would support a diagnosis of right Horner’s syndrome? 2. Dilation lag
The signs of Horner’s syndrome include ptosis of the upper and lower eyelids (the upper lid is at lower position and the lower lid is a higher position), miosis and dilation lag. Dilation lag is impaired pupillary movement during dilation. After the lights are turned off, there is an initial increase in the anisocoria as the normal pupil is stimulated by a burst of sympathetic activity, but the Horner pupil, devoid of sympathetic impulses, hardly moves. The Horner pupil later catches up as parasympathetic tone decreases.
Clinical Pearl
Signs of Horner’s syndrome include:
-
- Ptosis of upper lid
- Reverse ptosis of lower lid
- Miosis
- Dilation lag
- Anhidrosis
4. What pharmacological agent can be used to confirm the diagnosis in this patient at this time in the emergency room?
- Apraclonidine 0.5%
- Phenylephrine 10%
- Pilocarpine 0.1%
- None of the above
4. What pharmacological agent can be used to confirm the diagnosis at this time in the emergency room? 4. None of the above
Apraclonidine is a pharmacological agent that has strong alpha-2 and weak alpha-1 agonist activity. Apraclonidines’s alpha-2 effect stimulates the pre-synaptic adrenergic nerve and inhibits the release of norephinephrine, which may cause a small amount of constriction in a normal pupil. When sympathetic nerve stimulation is interrupted (Horner’s syndrome), there is denervation supersensitivity of the alpha-1 receptors in the iris and apraclonidine’s alpha-1 effect predominates and causes dilation of the pupil. A positive response to apraclonidine is “reversal of anisocoria” as the Horner’s pupil dilates due to denervation supersensivity and the normal pupil has a small amount of constriction as the alpha-2 effect causes inhibition of norepinephrine release. However, denervation supersensitivity usually takes at least 24 hours and typically about 3-7 days to develop and apraclonidine would not be helpful in this patient at this time who developed anisocoria less than 12 hours prior to presentation.
5. What is the next most appropriate investigation for this patient?
- Reassurance
- Blood pressure measurement
- Computed tomography or magnetic resonance angiography of the head and neck
- Chest x-ray
5. What is the next most appropriate investigation for this patient? 3. Computed tomography or magnetic resonance angiography of the head and neck
Carotid artery dissection can disrupt the sympathetic fibers ascending around the wall of the internal carotid artery leading to an ipsilateral Horner’s syndrome. In a patient presenting with an acute Horner’s syndrome with neck or head pain, carotid dissection must be urgently ruled out. Computed tomography angiography or MRA are the imaging modalities or choice with the former being preferred in the setting of trauma. Less commonly, a transient Horner’s syndrome may also be a sign of a carotid dissection.
Clinical Pearl
Carotid dissection must be ruled out in a patient with an acute Horner’s syndrome and neck or facial pain.
The patient had a CTA of the head and neck and a right carotid artery dissection was seen (red arrow).
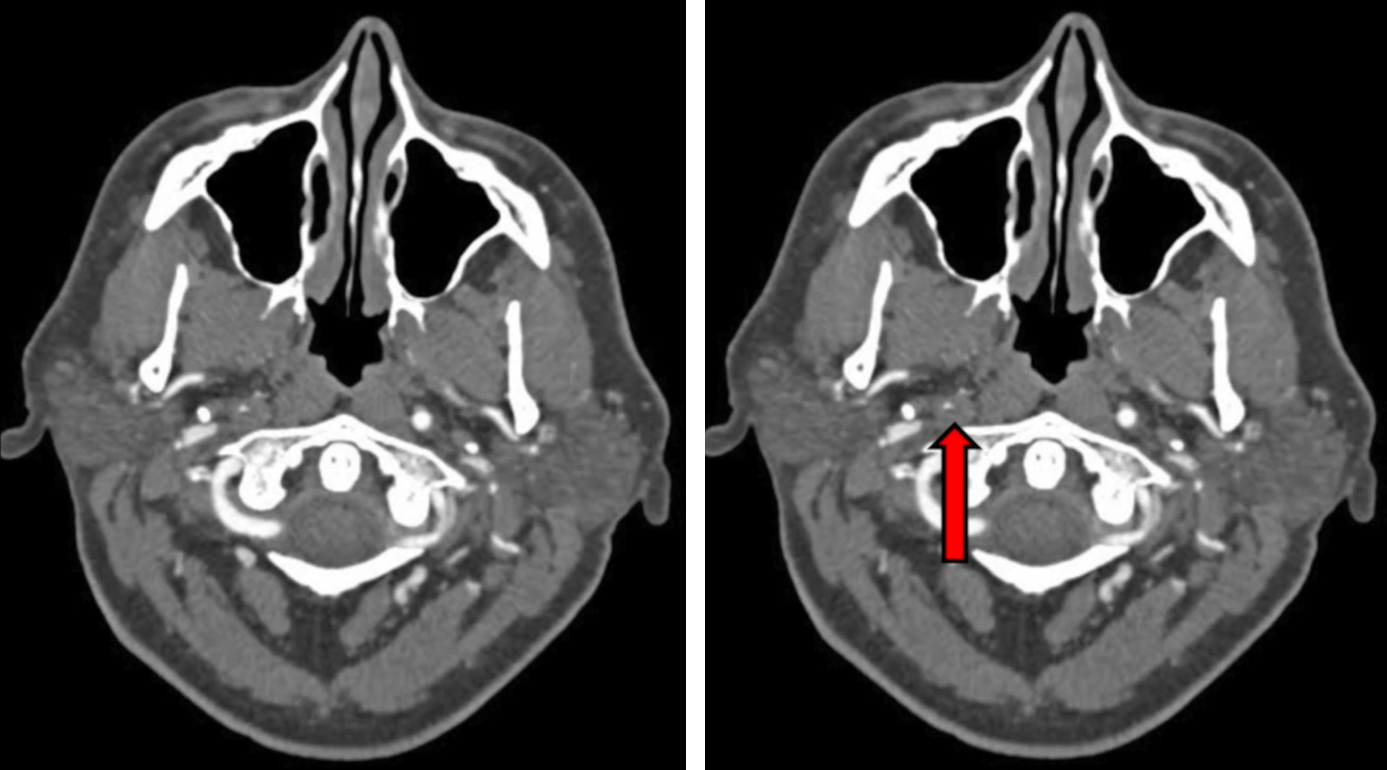
Final diagnosis: Right Horner’s syndrome secondary to a right internal carotid artery dissection.
6. How should this patient be treated?
- Carotid endarterectomy
- Anticoagulation or antiplatelet agents
- Topical eye drops
- No treatment required
6. How should this patient be treated? 2. Anticoagulation or antiplatelet agents
A carotid dissection occurs when there is a tear in the wall of the artery, leading to an intrusion of blood within the layers of the artery and the formation of an intramural hematoma. The majority of dissections heal spontaneously and treatment is aimed at preventing thromboembolism, which is the major cause of neurological complications that may occur. Patients with acute carotid dissection are at high risk for cerebral infarction, which usually occurs within the first days to weeks after the onset of dissection with the highest risk within 10 days of the dissection. The dissection will usually re-canalize and the risk of stroke becomes negligible 30 days after the dissection.
7. This patient’s Horner’s syndrome is due to dysfunction of the:
- First-order neuron
- Second-order neuron
- Third-order neuron
- None of the above
7. This patient’s Horner’s syndrome is due to dysfunction of the: 3. Third-order neuron
The sympathetic tract originates in the hypothalamus and contains a three-neuron pathway:
- First-order neuron: originates in the hypothalamus and courses down the brainstem to the C8-T2 level of the spinal cord (ciliospinal center of Budge). First order neurons may be affected by strokes, tumors and demyelinating lesions.
- Second-order neuron: leaves the spinal cord, courses over the apex of the lung and synapses in the superior cervical ganglion. Second-order neurons may be affected by chest lesions (carcinoma of the lung apex, “Pancoast tumor”), neck lesions (lymphadenopathy, thyroid cancer), or surgery.
- Third–order neuron: ascend with the internal carotid artery and enter the orbit through the superior orbital fissure and innervate the pupil and Müller’s muscle. Third-order neurons may be affected by cavernous sinus lesions (aneurysm or carotid-cavernous sinus fistula) or internal carotid artery dissection.
8. Anhidrosis in this patient would be expected on the:
- Entire ipsilateral face
- Entire ipsilateral body
- Small patch on the forehead
- Contralateral face
8. Anhidrosis in this patient would be expected on the: 3. Small patch on the forehead
The distribution of anhidrosis depends on the location of the sympathetic lesion. If the preganglionic neuron is affected (first or second order neuron), the entire side of the head, face and neck down to the clavicle are usually involved, whereas only a small patch on the forehead and medial side of the nose are involved when the post-ganglionic neuron is affected (third order neuron). Since this patient has a post-ganglionic lesion, only a small patch on the forehead is expected to be affected and this usually goes unnoticed by the patient.
Clinical Pearl
In first- or second-order lesions, anhidrosis is present on the ipsilateral head, face, and neck.
In third-order lesions, anhidrosis is minimal and may be present on a small patch on the forehead and and medial side of the nose.
9. The patient returns for a follow-up in 6 weeks and the following pharmacological test is performed:
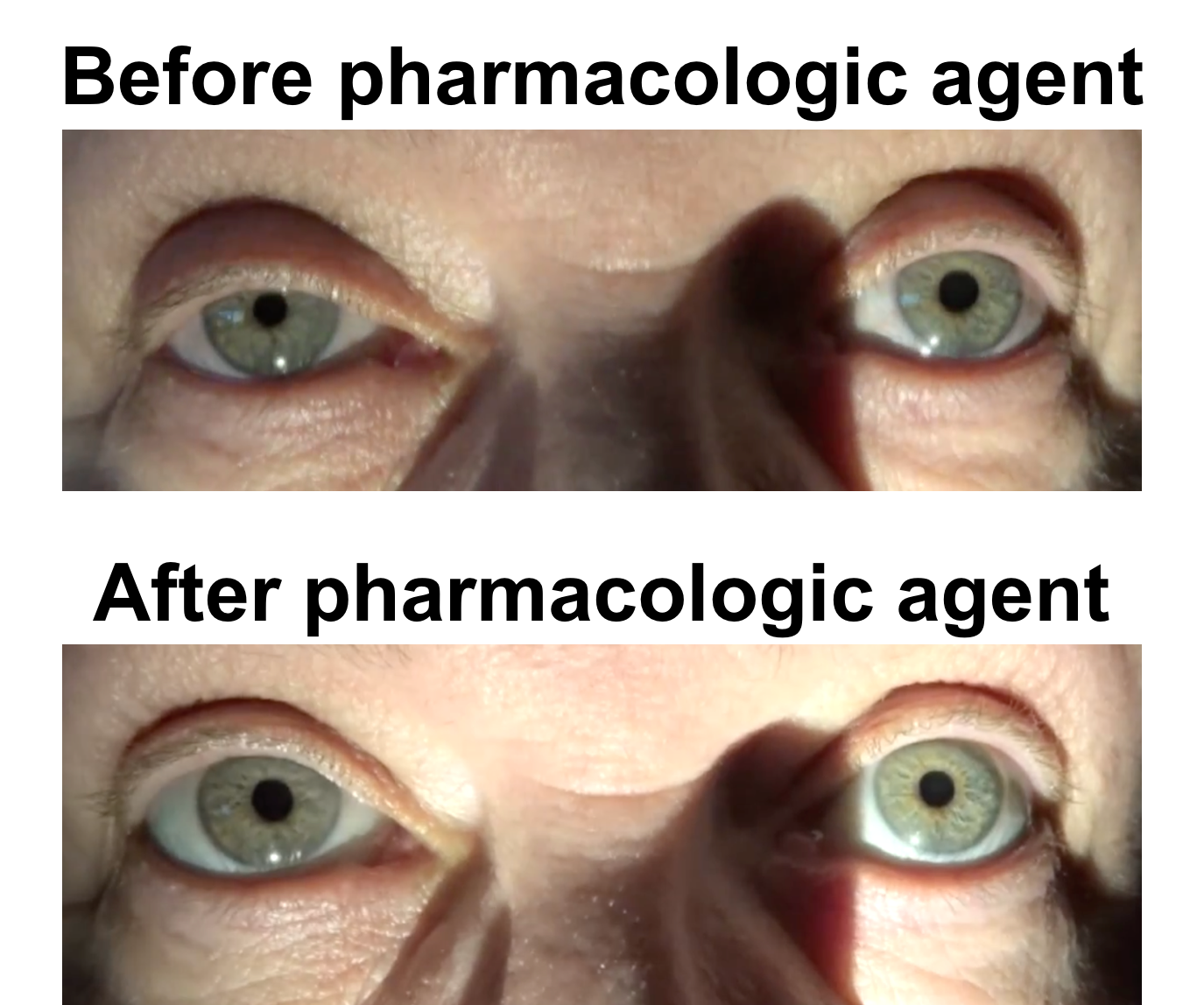
What drop was used?
- Cocaine 10%
- Apraclonidine 0.5%
- Pilocarpine 0.1%
- Phenylephrine 2.5%
9. What drop was used? 2. Apraclonidine 0.5%
Due to denervation super-sensitivity, apraclonidine’s weak alpha-1 activity caused smooth muscle contraction resulting in mydriasis of the right eye after 30 minutes and reversal of ptosis after less than 5 minutes. The normal pupil has also had a small degree of constriction leading to “reversal of anisocoria” and a positive test.
10. What group of patients should apraclonidine testing not be performed in?
- Elderly
- Glaucoma patients
- Infants
- Dry eye patients
10. What group of patients should apraclonidine testing not be performed in? 3. Infants
Apraclonidine should be avoided in young infants (less than 1 year of age) due to central nervous system depression or respiratory arrest that may occur due to immaturity of the blood-brain barrier.
11. What is considered a positive test result with cocaine 10% drops in Horner’s syndrome?
- Reversal of anisocoria
- Post-cocaine anisocoria of at least 1 mm
- Increase in dilation of abnormal pupil of 2 mm
- Increase in dilation of normal pupil of 2 mm
11. What is considered a positive test result with cocaine 10% drops in Horner’s syndrome? 2. Post-cocaine anisocoria of at least 1 mm
Cocaine blocks re-uptake of the norepinephrine that is continuously released from sympathetic nerve endings, leading to an accumulation of norepinephrine and pupillary dilation in a normal eye. Since there is sympathetic dysfunction in Horner’s syndrome there is no longer spontaneous release of norepinephrine and cocaine has no effect. It has been found that simply measuring the anisocoria 60 minutes after instillation of cocaine 10% in both eyes is a better predictor of Horner’s syndrome than taking the trouble to calculate the net change in anisocoria. If the difference in pupil size is 1mm or more 60 minutes after cocaine drops, there is a 5990:1 mean odds the patient has Horner’s syndrome.
12. In a patient with a cavernous sinus lesion causing a right Horner’s syndrome, what would be expected 45 minutes after instillation of hydroxyamphetamine hydrobromide 1% (Paredrine)?
- Dilation of right and left pupils
- Dilation of the right pupil only
- Dilation of the left pupil only
- No dilation of either pupil
12. In a patient with a cavernous sinus lesion causing a right Horner’s syndrome, what would be expected 45 minutes after instillation of hydroxyamphetamine hydrobromide 1% (Paredrine)? 3. Dilation of the left pupil only
Hydroxyamphetamine causes the release of stored norepinephrine from adrenergic nerve endings. It can therefore differentiate between post-ganglionic (third-order) and pre-ganglionic (first or second-order) neurons causing Horner’s syndrome. If the lesion is after the superior cervical ganglion (post-ganglionic) as in this case, there will be loss of the nerve terminals that store norepinephrine and hydroxyamphetamine will have no effect. Contrarily, if a pre-ganglionic neuron is implicated, the third-order neuron will be intact and hydroxyamphetamine will cause mydriasis. Hydroxyamphetamine hydrobromide 1% (Paredrine) is typically used for this test and results are evaluated 45 minutes after instillation. Since Paredrine is difficult to obtain, it is not commonly used in clinical practice.
13. Why is a 6th nerve palsy and Horner’s syndrome due to a cavernous carotid artery aneurysm less of an emergency than a 3rd nerve palsy from a posterior communicating artery aneurysm?
- There is less risk of rupture and the consequences of rupture are different
- A 6th nerve palsy causes less diplopia
- The sympathetic lesion is protective against aneurysm rupture
- There are multiple cranial nerves in the cavernous sinus
13. Why is a 6th nerve palsy and Horner’s syndrome due to a cavernous carotid artery aneurysm less of an emergency than a 3rd nerve palsy from a posterior communicating artery aneurysm? 1. There is less risk of rupture and the consequences of rupture are different
When an intradural aneurysm such as a posterior communicating artery aneurysm ruptures, it causes a devastating subarachnoid hemorrhage with an extremely high morbidity and mortality. Cavernous carotid aneurysms (CCAs) are much less prone to rupture, which may be due to the local microenvironment of the cavernous sinus. The International Study of Unruptured Intracranial Aneurysms (ISUIA) found that CCAs 13-24mm in size had a 3% risk of rupture within 5 years and asymptomatic CCAs > 25 mm had a 6.4% rupture risk within 5 years. Moreover, since CCAs are extradual, rupture will not cause a subarachnoid hemorrhage, but rather a carotid-cavernous sinus fistula (CCF).
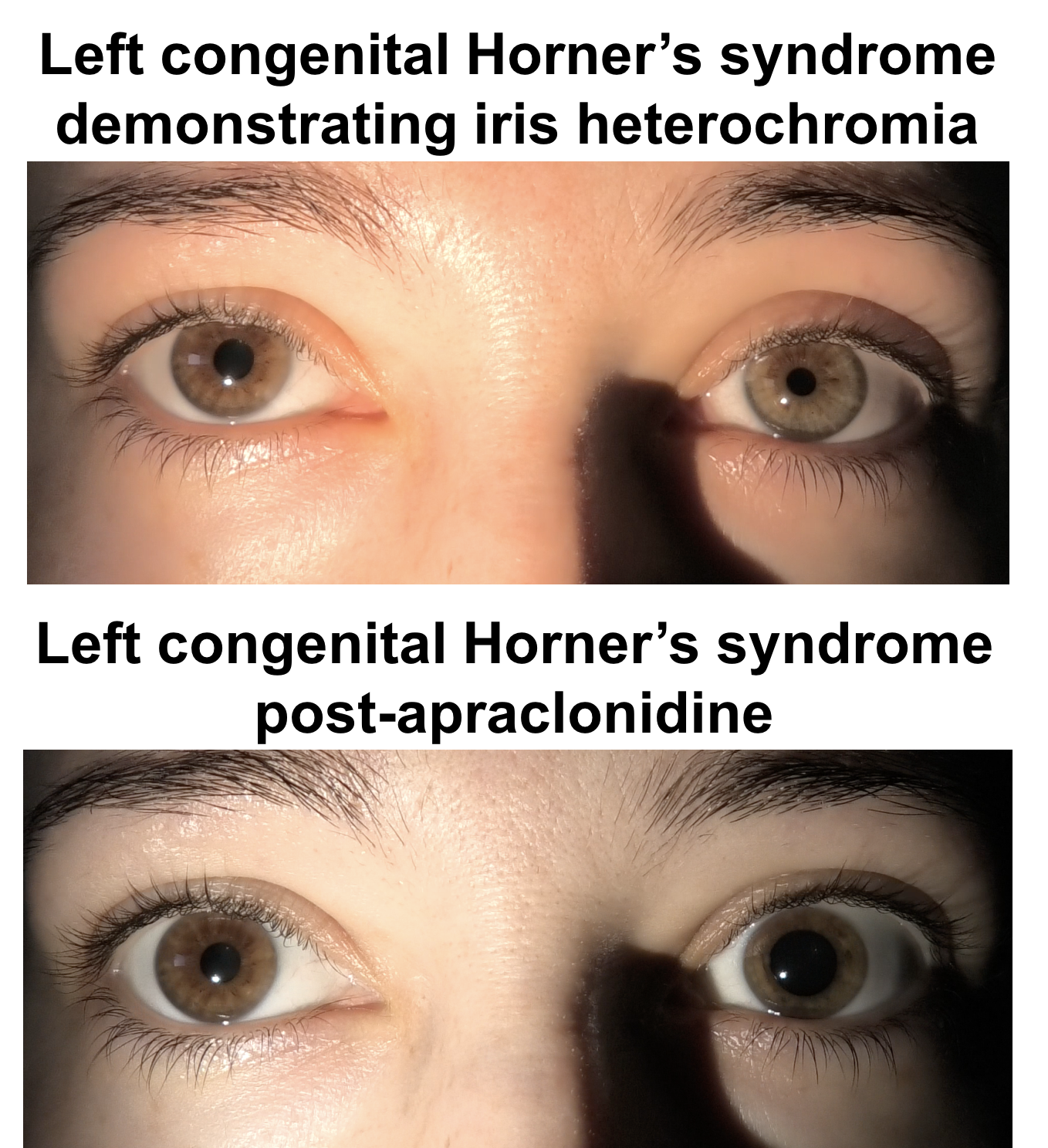
14. Which of the following is an expected finding in congenital Horner’s syndrome?
- Mydriasis
- Hypochromia of the affected iris
- Curlier hair on the side of the lesion
- Lid retraction
14. Which of the following is an expected finding in congenital Horner’s syndrome? 2. Hypochromia of the affected iris
Patients with congenital Horner’s syndrome have miosis, ptosis, facial anhydrosis and hypochromia of the affected iris. Parents may report that the affected side of the face does not flush when the infant is crying and children with naturally curly hair may have straighter hair on the side of the lesion. The affected iris is a lighter color since there is an attrition of the normal melanocyte population following sympathetic denervation. The most common cause of congenital Horner’s syndrome is birth trauma.
15. In a 10-month old child with new Horner’s syndrome, what investigations should be performed?
- Apraclonidine testing
- CT scan of the head and neck
- MRI of the brain, neck, and chest and urinary catecholamine metabolite testing
- Observation since likely due to birth trauma
15. In a 10-month old child with new Horner’s syndrome, what tests should be performed? 3. MRI of the brain, neck, and chest and urinary catecholamine metabolite testing
Acquired Horner’s syndrome in a child may be the presenting sign of neuroblastoma, which is a malignant neuroendocrine tumor of the sympathetic nervous system. Children presenting with Horner’s syndrome without a known diagnosis require further investigations to exclude a neoplastic process such as neuroblastoma. MRI of the head, neck, and chest with and without contrast in addition to random urine studies for catecholamine metabolites homovanillic acid (HVA) and vanillylmandelic acid (VMA) should be obtained.
Case Summary
She had the new onset of right ptosis and miosis with facial pain. Examination confirmed a right Horner’s syndrome and a carotid dissection was suspected in the context of a recent motor vehicle accident, facial pain and new Horner’s syndrome. This was confirmed with a CTA of the neck and she was started on anticoagulation. The patient was followed by a stroke neurologist. She did not develop any neurological sequelae from the carotid dissection and her examination remained stable.
Further reading:
-
Kardon RH, Denison CE, Brown CK, Thompson S. Critical evaluation of the cocaine test in the diagnosis of Horner’s syndrome. Arch Ophthalmol 1990;108:384-387. https://www.ncbi.nlm.nih.gov/pubmed/2310339
-
McCartney AC, Riordan-Eva P, Howes RC, Spalton DJ. Horner’s syndrome: an electron microscopic study of a human iris. Br J Ophthalmol 1992;76(12):746-749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC504397/
-
Mahoney NR, Liu GT, Menacker SJ, Wilson MC, Hogarty MD, Maris JM. Pediatric Horner syndrome: etiologies and roles of imaging and urine studies to detect neuroblastoma and other responsible mass lesions. Am J Ophthalmol 2006;142:651-659. https://www.ncbi.nlm.nih.gov/pubmed/17011859
-
Reede DL, Garcon E, Smoker WR, Kardon R. Horner’s syndrome: clinical and radiographic evaluation. Neuroimaging Clin N Am 2008;18(2):369-85. https://www.ncbi.nlm.nih.gov/pubmed/18466837