16
Case
Age: 24-year-old white woman
Reason for referral to ophthalmology: Sudden vision loss in the left eye
Past medical history: None
Past ocular history: None
Medications: Oral contraceptive pill
Habits: Non-smoker and does not drink alcohol
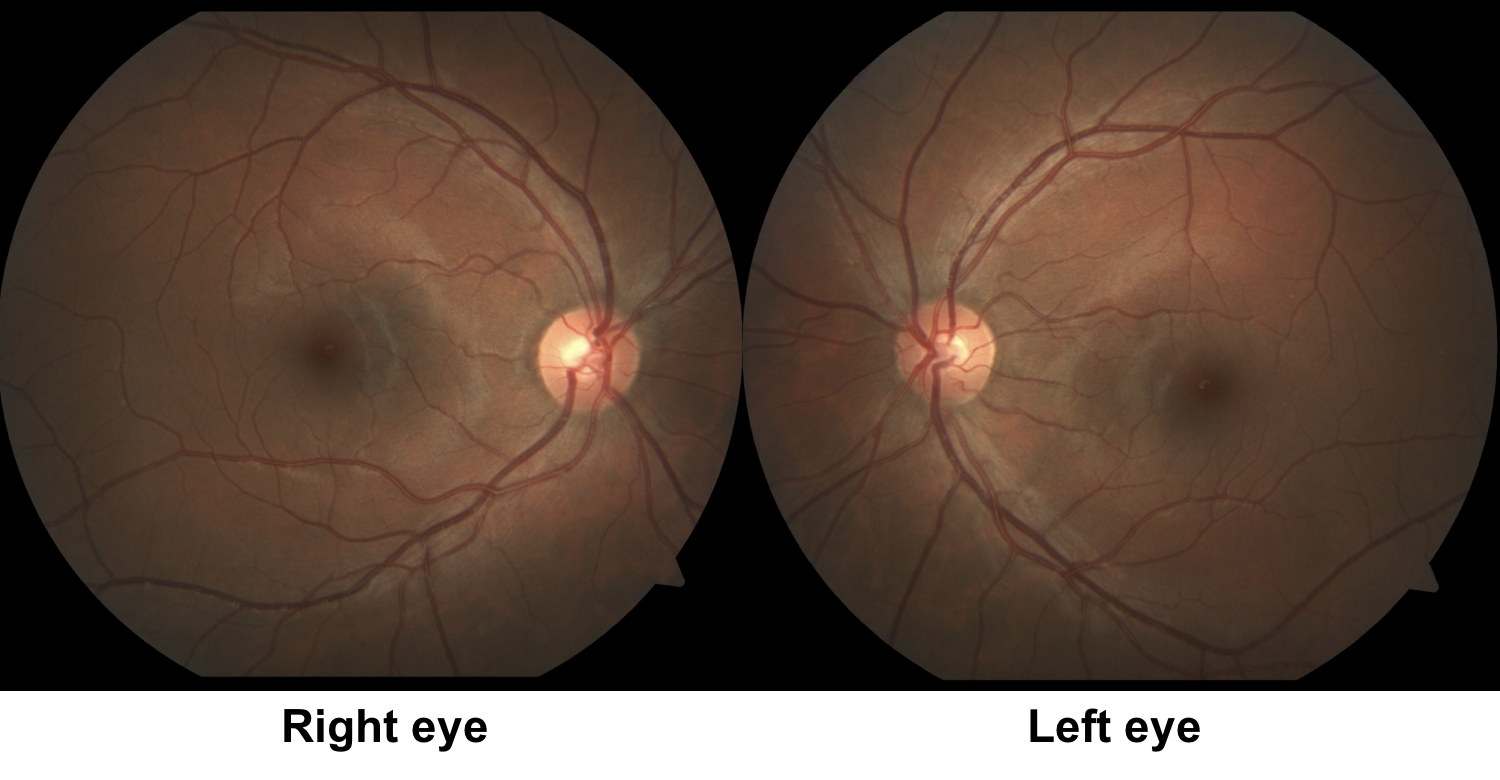
HPI: Two days ago, she had sudden painless vision loss in the left eye to the point where she could no longer see light. She saw her optometrist and her visual acuity was 20/20 OD, NLP OS and the remainder of her examination was normal. She had a normal examination and an urgent ophthalmology consultation was requested. A report from her optometrist was included that showed she had 20/20 vision in both eyes at her last examination, 1 year ago.
Ophthalmological examination:
Blood pressure: 116/78, heart rate 78
Visual acuity: 20/20 OD, NLP OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision: 14/14 correct Ishihara plates in the right eye, control plate not seen in the left eye
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
1. Which of the following is the strongest argument against this patient having a left optic neuropathy?
- Absence of left optic disc edema
- Absence of left optic disc pallor
- Normal OCT of the retinal nerve finer layer and ganglion cell complex
- Absence of a left RAPD
1. Which of the following is the strongest argument against this patient having a right optic neuropathy? 4. Absence of a left RAPD
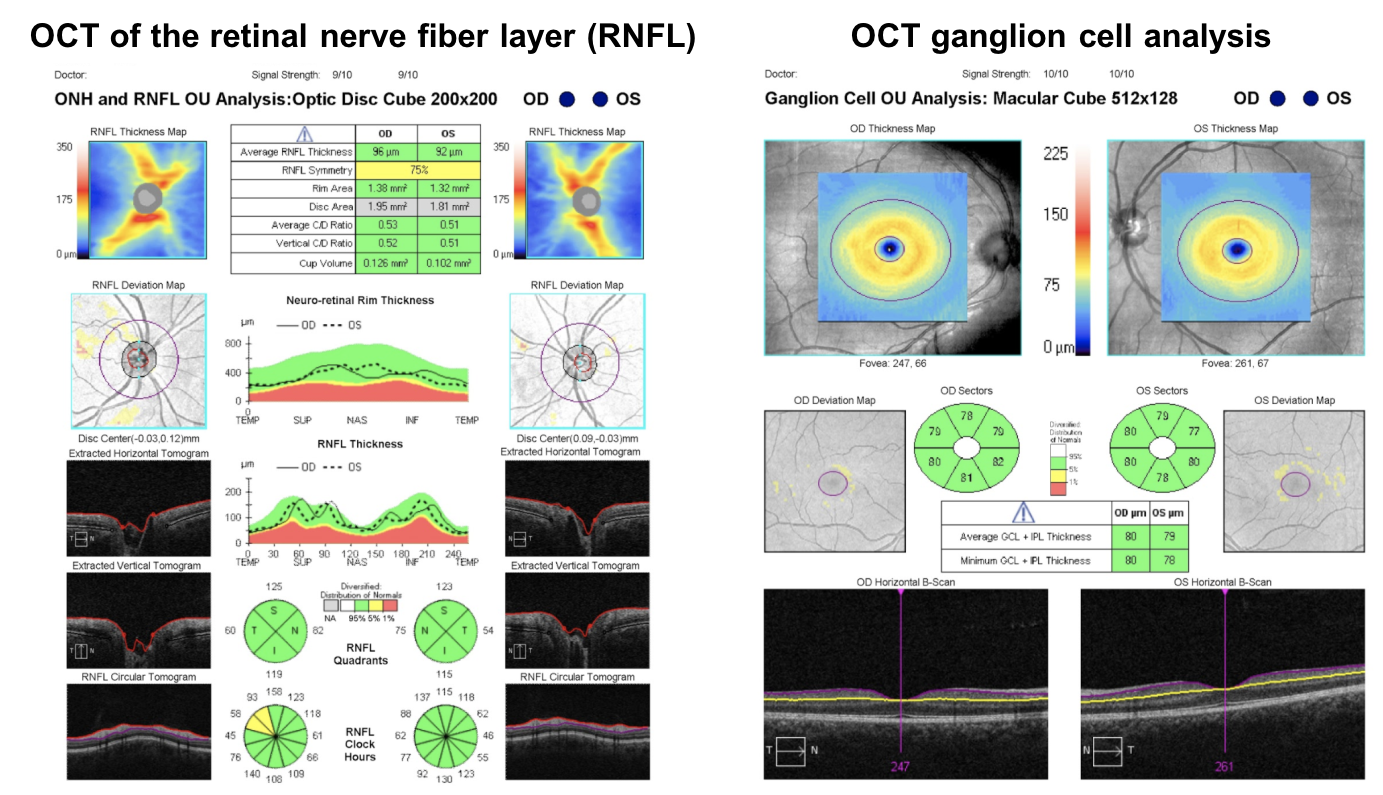
The absence of a left RAPD is a strong argument against this patient having a left optic neuropathy since essentially every unilateral optic neuropathy has an RAPD. In a patient with NLP vision in the left eye, there should be an obvious left RAPD if the vision loss is from an optic neuropathy. The rare exception is Leber’s Hereditary Optic Neuropathy (LHON), which may sometimes present with unilateral vision loss, a normal fundus examination, and the absence of an RAPD. The absence of optic disc edema does not rule out an optic neuropathy, since some optic neuropathies such as optic neuritis or compressive optic neuropathies may be retrobulbar and will not have optic disc edema. Optic disc pallor takes approximately 6-8 weeks to be seen after an acute insult to the optic nerve and will not be seen in the acute phase. Similarly, thinning of the RNFL or macular ganglion cell complex on OCT takes several weeks to develop and the OCT will not show thinning in the acute phase of an optic neuropathy.
Clinical Pearl
A unilateral optic neuropathy will have an RAPD in the that eye. The rare exception is Leber’s Hereditary Optic Neuropathy (LHON), which may sometimes have a subtle or absent RAPD.
2. The patient’s right eye is patched and an optokinetic nystagmus (OKN) drum is rotated in front of the patient. Optokinetic nystagmus is observed in the patient, indicating that the visual acuity in the left eye is at least:
- 20/20
- 20/50
- 20/100
- 20/400
2. The patient’s right eye is patched and an optokinetic nystagmus (OKN) drum is rotated in front of the patient. Optokinetic nystagmus is observed in the patient, indicating that the visual acuity in the right eye is at least: 4. 20/400
Testing for optokinetic nystagmus is useful in patients suspected of nonorganic vision loss. If there is a positive response and optokinetic nystagmus is observed, the visual acuity is at least 20/400. If the patient reports unilateral vision loss, the good eye is patched and an OKN drum or strip should be shown to the patient. If bilateral vision loss is reported then both eyes can be tested at the same time. This test is not helpful in patients with visual acuities better than 20/400 suspected of nonorganic vision loss.
3. The patient’s stereo vision is tested using the Titmus test and found to be 40 seconds of arc (9/9 Titmus circles correctly identified). You can conclude with 95% certainty that the patient’s visual acuity in the worse eye is better than:
- 20/20
- 20/25
- 20/30
- 20/40
3. The patient’s stereo vision is tested using the Titmus test and found to be 40 seconds of arc (9/9 Titmus circles correctly identified). You can conclude with 99% certainty that the patient’s visual acuity is better than: 4. 20/40
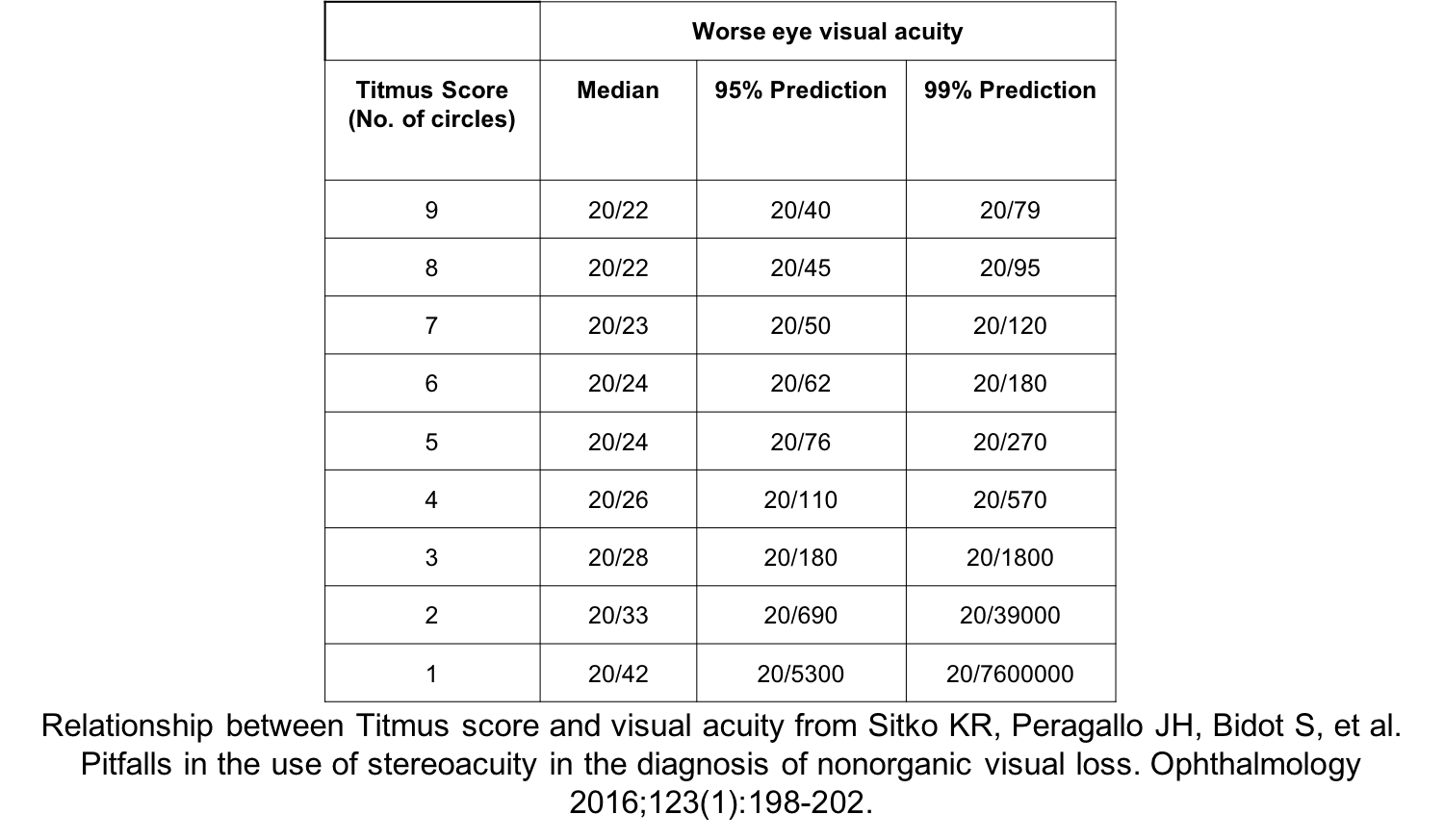
Testing stereo vision is one of the most useful tests in a patient suspected of unilateral nonorganic vision loss. Classically, from a paper published in 1974, a relationship between stereopsis and visual acuity in each eye was reported as shown below:
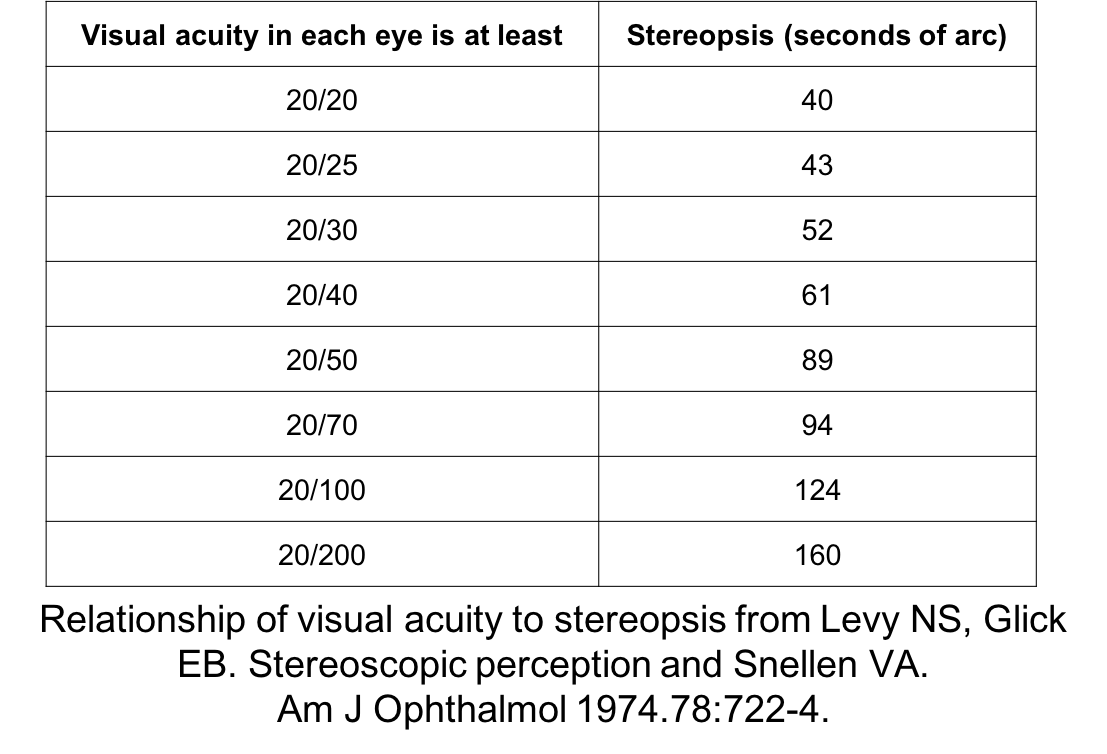
However, a more recent study from a tertiary neuro-ophthalmology center found that this table overestimated visual acuity based on stereopsis. A new table was reported and is shown below.
4. A 4 prism diopter (base out) prism is placed over the patient’s left eye and she is asked to look at the 20/50 line. Which of the following would be observed if the patient had normal vision in the left eye?
- No movement would be observed in either eye
- Movement of both eyes towards the apex of the prism followed by a convergence movement of the right eye
- Movement of only the left eye towards the base of the prism followed by a divergence movement of the right eye
- Movement of both eyes towards to the base of the prism followed by a convergence movement in both eyes
4. A 4 prism diopter (base out) prism is placed over the patient’s left eye and she is asked to look at the 20/50 line. Which of the following would be observed if the patient had normal vision in the left eye? 2. Movement of both eyes towards the apex of the prism followed by a convergence movement of the right eye
A prism shift test can be used to test a patient with suspected unilateral nonorganic vision loss since it requires binocular vision. If the patient sees the letters with the eye under the base out prism, then there will be a compensatory movement of both eyes towards the apex of the prism followed by a convergence movement of the fellow eye as the patient attempts to suppress diplopia.
5. How can the phoropter be used to test whether the vision in the left eye is better than NLP?
- Fog both eyes with a plus lens and check the vision in the left eye
- Fog the left eye with a plus lens and test visual acuity
- Fog the right eye with a plus lens and test visual acuity
- Fog both eyes with a minus lens and test visual acuity
5. How can the phoropter be used to test whether the vision in the left eye is better than NLP? 3. Fog the right eye with a plus lens and test visual acuity
The phoropter is an instrument used for refraction and contains a number of lenses of various powers that can be dialled in for each eye. Placing plus lenses over an eye “fogs” the patient since it blurs the image and cannot be overcome with accommodation. Usually the patient will not be aware which eye is being fogged since both eyes are open. If the good eye is fogged and the patient reads the Snellen chart, it demonstrates that the vision is better than claimed in this patient.
There is a positive OKN response in the left eye when the right eye was patched
Stereopsis is 40 seconds of arc
Visual acuity was 20/20 when the right eye was fogged with a +7.00 lens
The prism shift test showed a shift of both eyes towards the apex and a compensatory convergence movement of the right eye
Since it was demonstrated that the patient’s vision was 20/20, the patient has nonorganic vision loss.
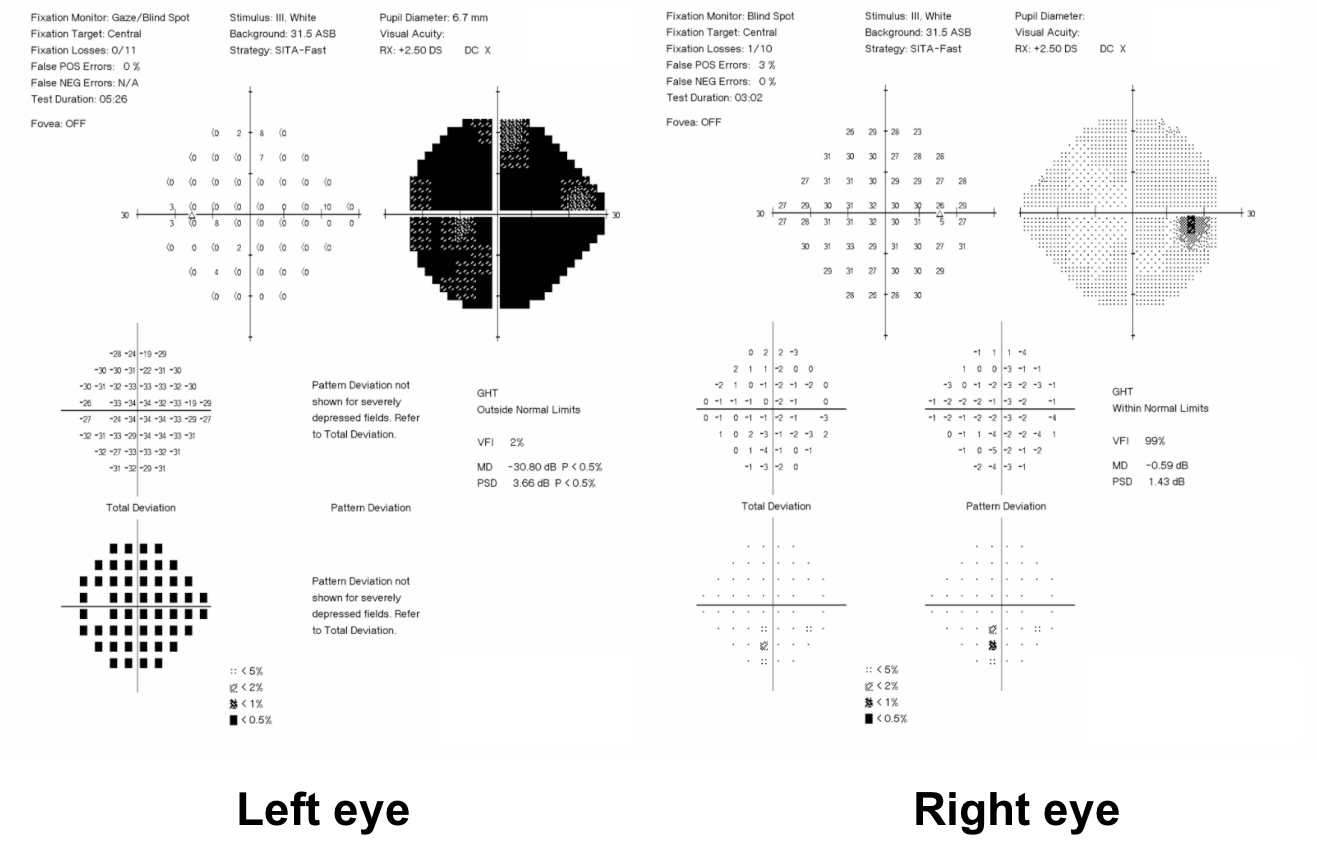
6. The patient returns for an examination in 3 months and her examination is unchanged and visual acuity is still claimed to be NLP in the left eye. OCT of the RNFL is also unchanged. Which of the following is most accurate?
- The patient does not have an optic neuropathy since there has been no RNFL loss at this time
- The patient may have an optic neuropathy and the OCT should be repeated in 6 months
- OCT changes of the RNFL is not a reliable indicator in optic neuropathies
- None of the above
6. The patient returns for an examination in 3 months and her examination is unchanged and visual acuity is still claimed to be NLP in the left eye. OCT of the RNFL is also unchanged. Which of the following is most accurate? 1. The patient does not have an optic neuropathy since there has been no RNFL loss at this time
If the RNFL thickness measured by OCT is the same 3 months after an acute loss of vision, then the vision loss is not due from an optic neuropathy. There must be RNFL loss at this time and this is typically seen in the first few weeks after vision loss and certainly by 6-8 weeks.
7. What other technique that makes use of the Snellen chart can be used if nonorganic vision loss is suspected in one eye?
- While occluding the good eye, start with the 20/400 line and slowly proceed down the chart
- While occluding the good eye, start with the 20/10 line and proceed very slowly up the chart
- While occluding the bad eye, start one to two lines above the 20/20 line
- Test visual acuity with both eyes open and observe the patient
7. What other technique that makes use of the Snellen chart can be used if nonorganic vision loss is suspected in one eye? 2. While occluding the good eye, start with the 20/10 line and proceed very slowly up the chart
If visual acuity is assessed starting with very small letters, the patient may perceive that relatively larger letters (such as those on the 20/40 or 20/50 line) are actually very big and will read them. By continuing to encourage the patient, but moving only very slowly up the chart, the patient may become frustrated and begin to read the letters so that they can move on with the examination.
8. How is proprioception affected in patients with severe vision loss in one eye from an optic neuropathy?
- Proprioception will be significantly affected
- Proprioception will be reduced on the side of the vision loss
- Proprioception will be reduced on the side contralateral to the vision loss
- Proprioception will not be affected
8. How is proprioception affected in patients with severe vision loss in one eye from an optic neuropathy? 4. Proprioception will not be affected
Proprioception is the ability to sense body position and does not require intact vision. Patients with severe vision loss will be able to perform proprioceptive tasks such as bringing the tips of their index fingers together. Patients with nonorganic vision loss are often unable to touch the tips of their fingers together properly since they are unaware of the independence of proprioception and vision. The inability to perform proprioceptive tasks suggests that there may be nonorganic vision loss.
9. A patient claiming no light perception vision in both eyes has a visual evoked potential that is abnormal. This test:
- Proves that there is a component of organic vision loss
- Does not prove organic vision loss
- Proves there is organic vision loss if it can be reproduced on a second occasion
- None of the above
9. A patient claiming no light perception vision in both eyes has a visual evoked potential that is abnormal. This test: 2. Does not prove organic vision loss
Visual evoked potential (VEP) is an electrophysiologic test that plays a limited role in evaluating a patient with possible nonorganic vision loss. Visual evoked potentials are measurements of the electrical signal recorded at the scalp over the occipital cortex in response to a visual signal. An abnormal VEP in itself does not lead to a diagnosis of organic vision loss since a variety of techniques such as inattention, lack of concentration or meditation can suppress the visual evoked response.Visual evoked potentials of normal and symmetric amplitude and latency in a patient such as this with profound monocular vision loss provides confirmatory evidence of nonorganic vision loss.
10. A mirror is rotated and moved up and down in front of a patient with suspected nonorganic vision loss claiming light perception vision in both eyes. What will be observed in the eyes of the patient with the mirror test if there is nonorganic vision loss?
- The eyes will not move
- The patient will develop an exotropia
- The patient will follow their own image in the mirror
- The patient will develop and esotropia
10. A mirror is rotated and moved up and down in front of a patient with suspected nonorganic vision loss claiming light perception vision in both eyes. What will be observed in the eyes of the patient with the mirror test if there is nonorganic vision loss? 3. The patient will follow their own image in the mirror
The mirror test is a useful test in patients claiming no light perception or light perception vision. Patients with nonorganic vision loss will be unable to avoid following their own image in the mirror that is held close to their face and rotated or moved up and down. They will demonstrate a nystagmoid movement of the eyes since they cannot avoid following their moving reflection in the mirror.
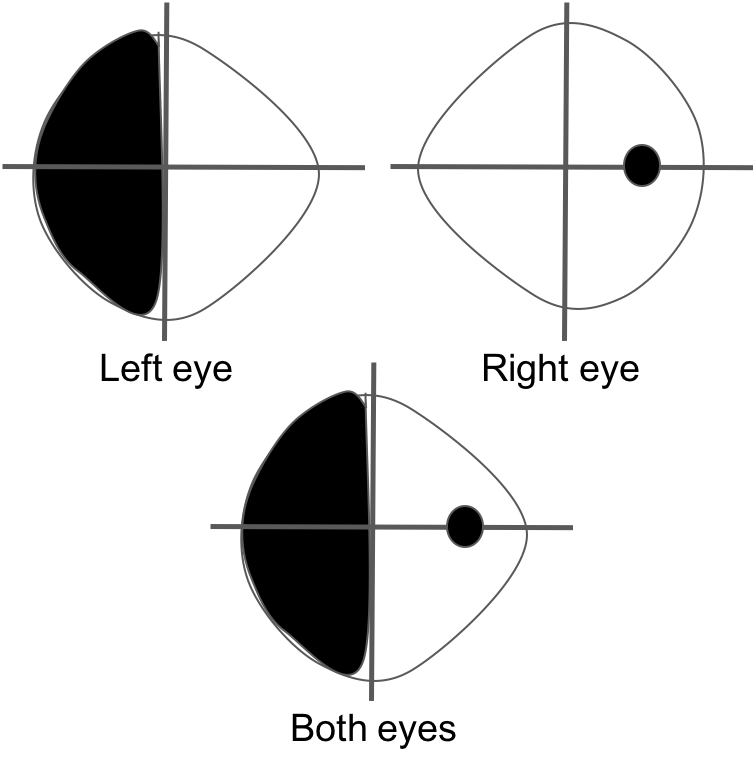
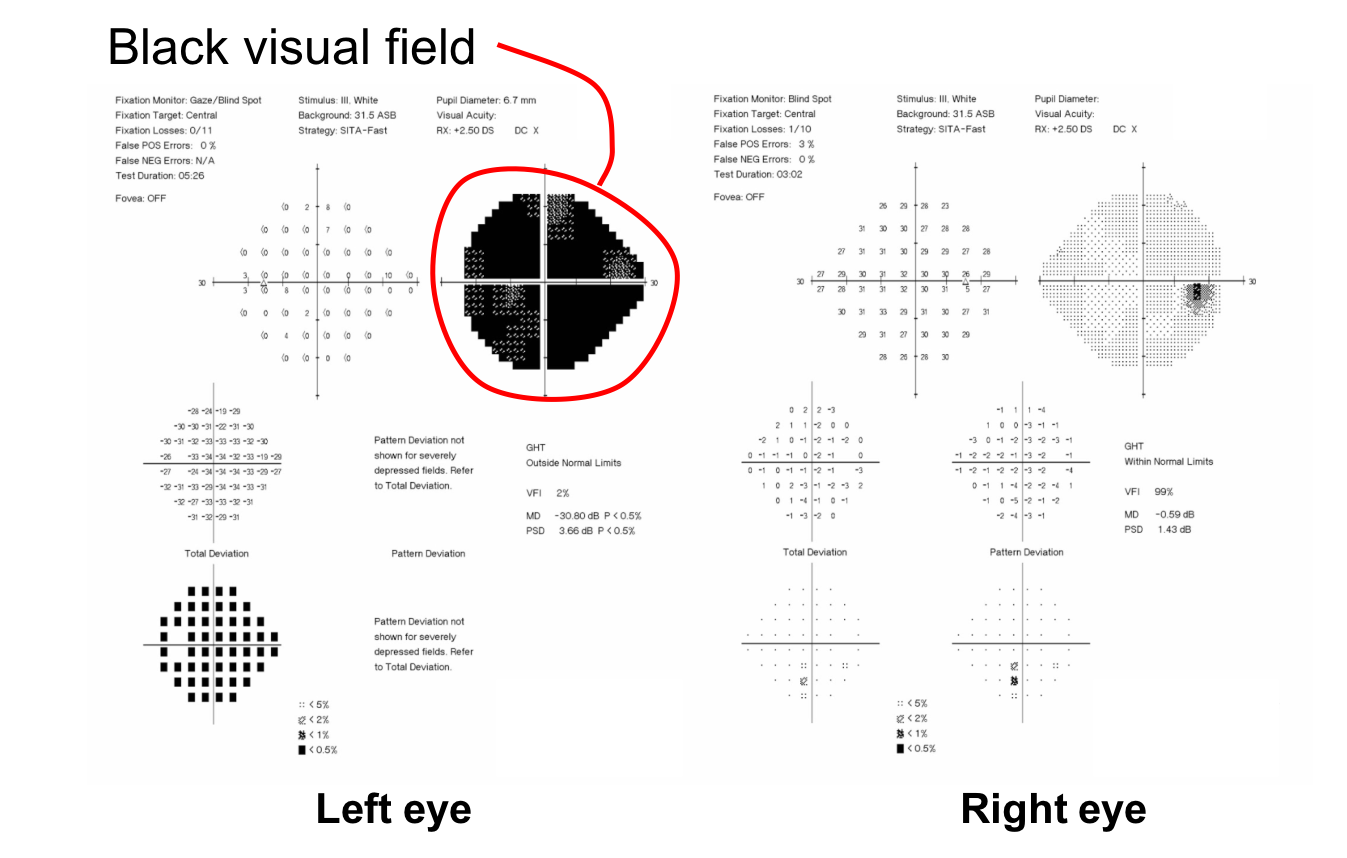
11. A patient complains of a visual field defect in the left eye. Visual field testing of each eye individually and a binocular visual field are shown below:
Which of the following is true?
- There is a bitemporal hemianopia
- The visual field pattern is consistent with a left optic neuropathy
- The visual field pattern is not consistent with organic disease
- There is a homonymous visual field defect
11. Which of the following is true? 3. The visual field pattern is not consistent with organic disease
The patient has a complete temporal hemianopia in the left eye, but this is still present when both eyes are tested together. Since the nasal visual field of the right eye is normal, the binocular visual field should also be normal. The binocular visual field suggests nonorganic vision loss.
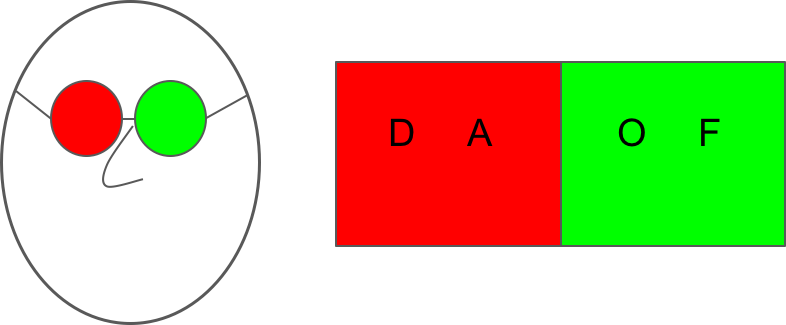
12. A patient presents with unilateral vision loss in the right eye suspected to be nonorganic in nature. The patient is shown the following chart and wears the glasses shown below. If she reads all the letters on the line shown below, what does this mean?
- The right eye read some letters
- The left eye read all the letters
- The left eye must be functioning well
- None of the above
12. A patient presents with unilateral vision loss in the right eye suspected to be nonorganic in nature. The patient is shown the following chart and wears the glasses shown below. If she reads all the letters on the line shown below, what does this mean? 1. The right eye read some letters
Red-green glasses with a duochrome chart can be used to assess a patient suspected to have nonorganic vision loss. The eye with the green lens will only see the letters on the green side of the chart and the red lens will see only the letters on the red side of the chart. Therefore, if there was organic vision loss in the right eye, then only the “O” and “F” will be read. Since the patient read all of the letters, the right eye must have seen the “D” and “A”.
13. A patient presents with oscillopsia and possible nystagmus. Which of the following supports the diagnosis of voluntary nystagmus?
- Fluttering of the eyelids
- Strained facial expression
- Convergence of the eyes during the episode
- All of the above
13. A patient presents with oscillopsia and possible nystagmus. Which of the following supports the diagnosis of voluntary nystagmus? 4. All of the above
Voluntary nystagmus can be produced by some people in the normal population. Patients usually complain of oscillopsia and reduced vision. Signs that suggest voluntary nystagmus include fluttering of the eyelids, strained facial expressions during the episodes of nystagmus, and the tendency of the eyes to converge during the nystagmus.
14. A patient suspected of nonorganic vision loss in the right eye has a visual acuity of counting fingers OD and 20/20 OS. He has a positive OKN response in the right eye and after 10 minutes of encouragement, he is able to read the 20/400 line in the right eye. There is no RAPD. What is your diagnosis?
- Nonorganic vision loss
- Retrobulbar optic neuritis
- Optic nerve sheath meningioma
- The patient should be further assessed and the differential diagnosis includes an occult maculopathy or Leber’s Hereditary Optic Neuropathy
14. A patient suspected of nonorganic vision loss in the right eye has a visual acuity of counting fingers OD and 20/20 OS. He has a positive OKN response in the right eye and after 10 minutes of encouragement, he is able to read the 20/400 line in the right eye. There is no RAPD. What is your diagnosis? 4. The patient should be further assessed and the differential diagnosis includes an occult maculopathy or Leber’s Hereditary Optic Neuropathy
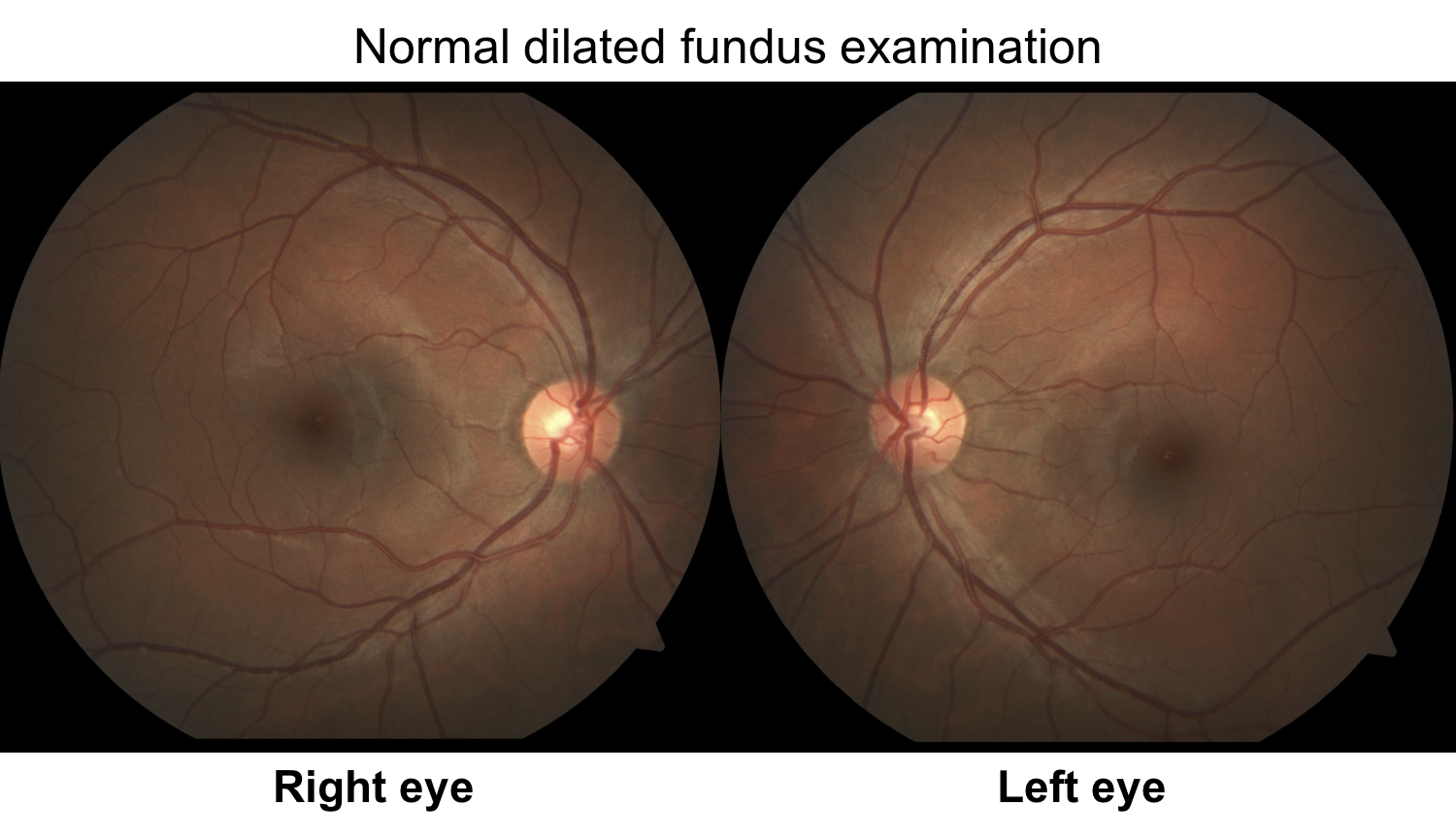
This patient may have vision better than initially claimed, but normal vision has not been established. Nonorganic vision loss should not be diagnosed unless normal vision has been demonstrated. There are many occult conditions including a number of maculopathies and Leber’s Hereditary Optic Neuropathy that may raise a suspicion for nonorganic vision loss because of a normal examination. A normal dilated examination, does not rule out ocular pathology and many conditions only become evident later in their clinical course or with more detailed testing (for eg. multifocal electroretinogram). Be very careful of labelling someone as nonorganic when they do not demonstrate normal vision with techniques employed for nonorganic vision loss.
Clinical Pearl
Nonorganic vision loss should only be diagnosed after normal visual function has been demonstrated.
15. A patient presents to an ophthalmologist with a visual complaint, but no organic disease was found. Why might the patient be presenting in this way?
- Conversion disorder
- Malingering
- Body dysmorphic disorder
- All of the above
15. A patient presents to an ophthalmologist with a visual complaint, but no organic disease was found. Why might the patient be presenting in this way? 4. All of the above
Nonorganic disturbances may be due to psychogenic disturbances, malingering or Munchausen syndrome. Psychogenic disturbances include conversion disorder, which occurs subconsciously for either primary (eg. reduction of stress) or secondary (eg. increased attention) gain. Malingerers consciously and voluntarily fake illness for secondary gain (eg. disability benefits or time off work). Body dysmorphic disorder is seen in patients who are obsessed with a physical sign (eg. ptosis or mild anisocoria) that is minimal or even absent to an objective observer. Patients with Munchausen syndrome intentionally induce damage to themselves and may manifest with ocular signs (conjunctival injection, eyelid swelling). It may be related to malingering or an underlying psychological illness.
It is important during the examination to get some sense of why the patient is presenting with nonorganic disease, which will help in directing the patient to the appropriate resources or professionals.
Case Summary
She presented with acute loss of vision in the left eye and her visual acuity was claimed to be no light perception vision in that eye. However, she had briskly reactive pupils, no RAPD, and a normal examination. When the right eye was patched, she had a positive OKN response, indicating that the vision in the left eye was better than 20/400. When the right eye was fogged with a +7.00 lens, she read the 20/20 line, indicating that her vision was better than claimed. The patient was reassured that no concerning abnormality was found on her examination and that the vision should improve with time. She had many stressors at home and at work and she was referred to her primary care physician and other specialists to explore avenues to help her cope with these stressors.
Further reading:
-
Dattilo M, Biousse V, Bruce BB, Newman NJ. Functional and simulated visual loss. Handb Clin Neurol 2016;139:329-341. https://www.ncbi.nlm.nih.gov/pubmed/27719853
-
Bruce BB, Newman NJ. Functional visual loss. Neurol Clin 2010;28(3):789-802. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907364/
-
Levy NS, Glick EB. Stereoscopic perception and Snellen VA. Am J Ophthalmol 1974.78:722-4. https://www.ncbi.nlm.nih.gov/pubmed/4415892
-
Sitko KR, Peragallo JH, Bidot S, et al. Pitfalls in the use of stereoacuity in the diagnosis of nonorganic visual loss. Ophthalmology 2016;123(1):198-202. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695302/