15
Case
Age: 50-year-old white woman
Reason for referral to ophthalmology: Transient visual disturbances
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and does not drink alcohol
HPI: For the past few years she has had episodes of flashing lights and shapes in a zig-zag pattern that always occurs in the same location on the right side of her visual field in both eyes. The episodes last several minutes and then completely resolve. Initially, they occurred every 1 to 2 months, but have become more frequent and associated with headaches, nausea and photophobia lasting several hours. She saw her primary care provider and an ophthalmology consultation was arranged. She does not have a history of migraines or motion sickness.
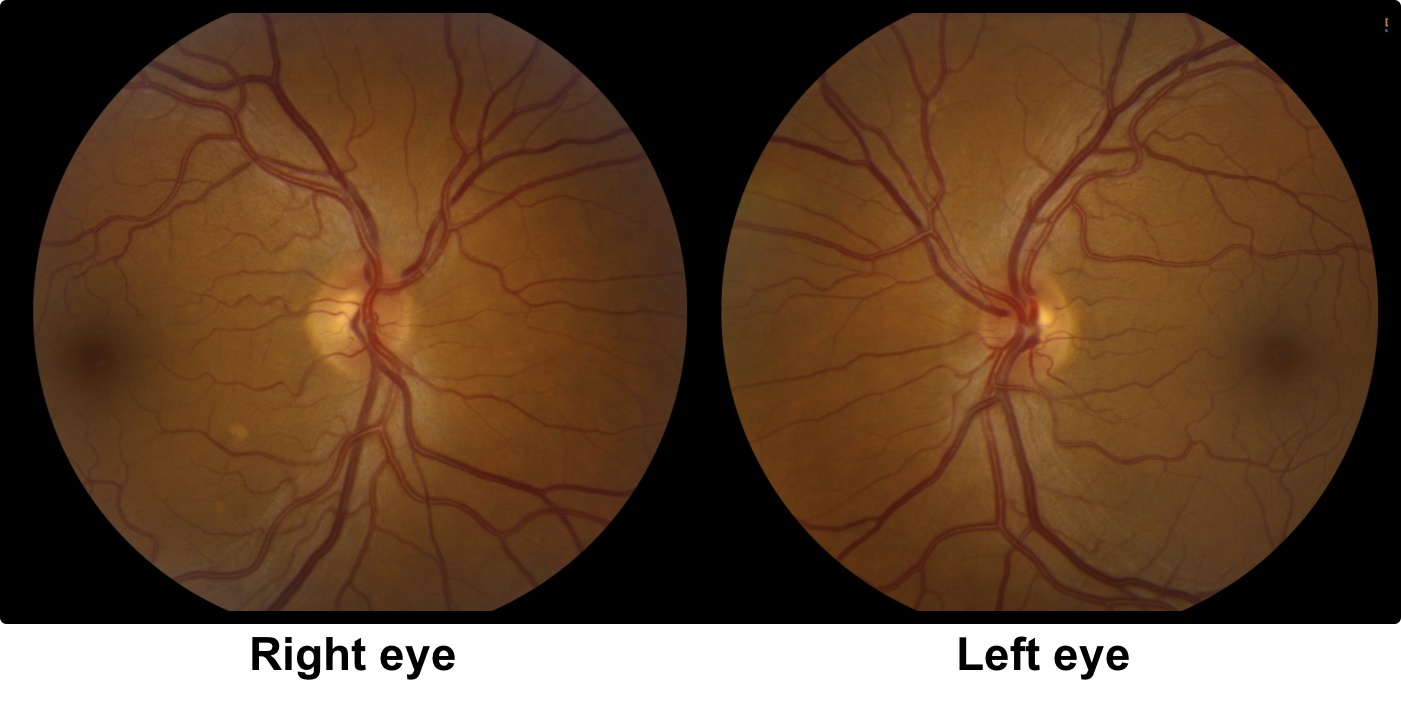
Ophthalmological examination:
Blood pressure: 118/83, heart rate 72
Visual acuity is 20/20 OD and 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision: 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
1. Which of the following may produce binocular positive visual phenomena?
- Migraine
- Occipital seizures
- Ischemia
- All of the above
1. Which of the following may produce binocular positive visual phenomena? 4. All of the above
Binocular positive visual phenomena are associated with migraine auras in the vast majority of cases, but may also be seen with occipital lobe seizures and transient ischemia or infarction. Migraine-like visual aura and visual seizures may be secondary to an underlying structural lesion such as a neoplasm or vascular malformation.
2. How long do visual auras from migraine usually last?
- Less than 5 minutes
- 10 to 30 minutes
- 1 to 2 hours
- Greater than 2 hours
2. How long do visual auras from migraine usually last? 2. 10 to 30 minutes
The visual aura associated with migraine typically lasts 10 to 30 minutes and is followed by a headache, although headache is not present in about 5% of cases. According to The International Classification of Headache Disorders, 3rd edition, the aura should spread gradually over > 5 minutes and lasts 5 to 60 minutes. Positive visual phenomena lasting less than 5 minutes or greater than 60 minutes are considered atypical for migraine.
Clinical Pearl
Clinical features that should raise doubts about a migraine diagnosis:
- Brief visual aura lasting seconds or less than 5 minutes
- Older age without a past history of migraines
- Visual aura without headache
3. What clinical feature from this patient’s history cast doubt on a migraine diagnosis?
- Zigzag pattern
- Seen in both eyes
- Always in the same location the right side of the visual field
- Occurred every 1 to 2 months
3. What other feature from this patient’s history is atypical for migrainous visual phenomena? 3. Always in the same location on the right side of the visual field
Patients who have very stereotyped visual auras that always occur in the same location in the visual field may harbour a cerebral lesion in the contralateral visual cortex. In migraine, the visual auras have variability and usually do not occur in the same location and with the exact same duration. It is reassuring when the visual aura occurs in both hemifields since this is rarely a sign of an underlying cortical lesion.
Clinical Pearl
Patients who have positive visual phenomena that always occur in the same location require neuroimaging.
4. The origin of the patient’s positive visual disturbance is most likely the:
- Right retina
- Left retina
- Right occipital lobe
- Left occipital lobe
4. The origin of the patient’s positive visual disturbance is most likely the : 4. Left occipital lobe
The patient sees the visual disturbances in both eyes and on the right side of the visual field. This localizes to the retrochiasmal visual pathways on the left since the left cerebral hemisphere is responsible for vision on the right side of the visual field. Considering that the patient has no other neurological symptoms other than visual changes, her visual changes most likely originate in the left occipital lobe.
5. What other test available in the eye clinic would be most useful in this patient?
- Optical coherence tomography
- Multifocal ERG
- Humphrey visual field
- Corneal topography
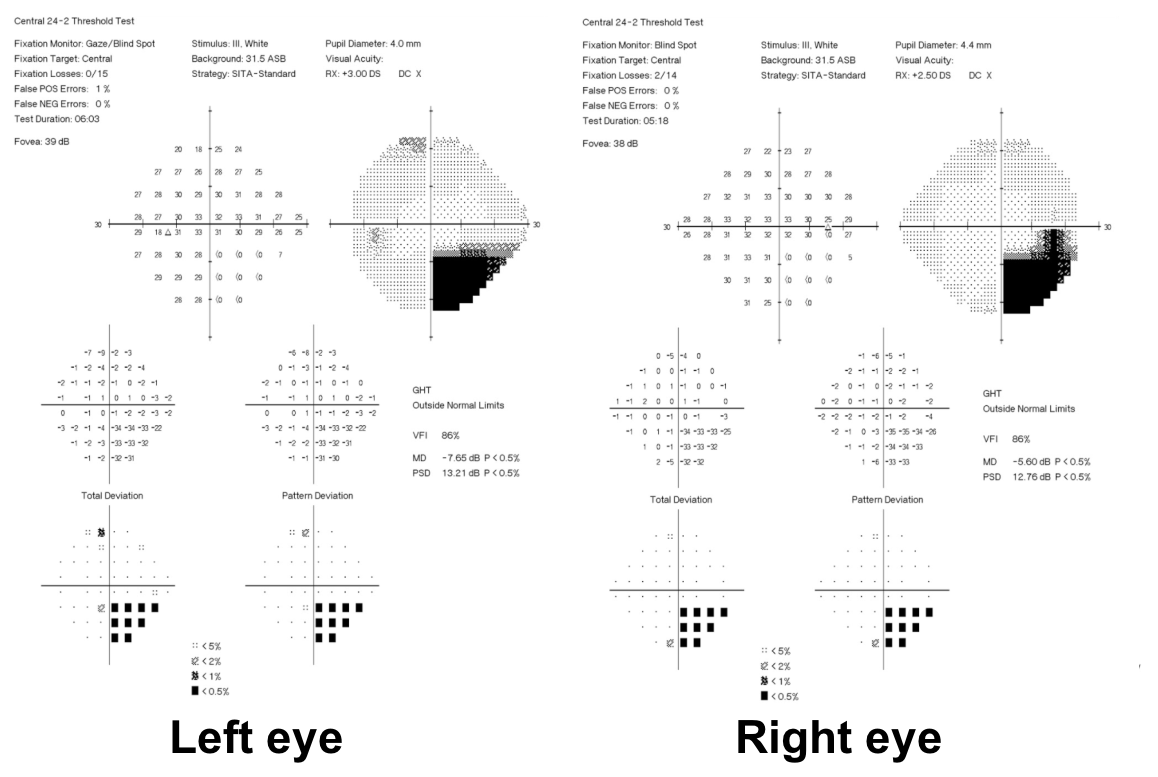
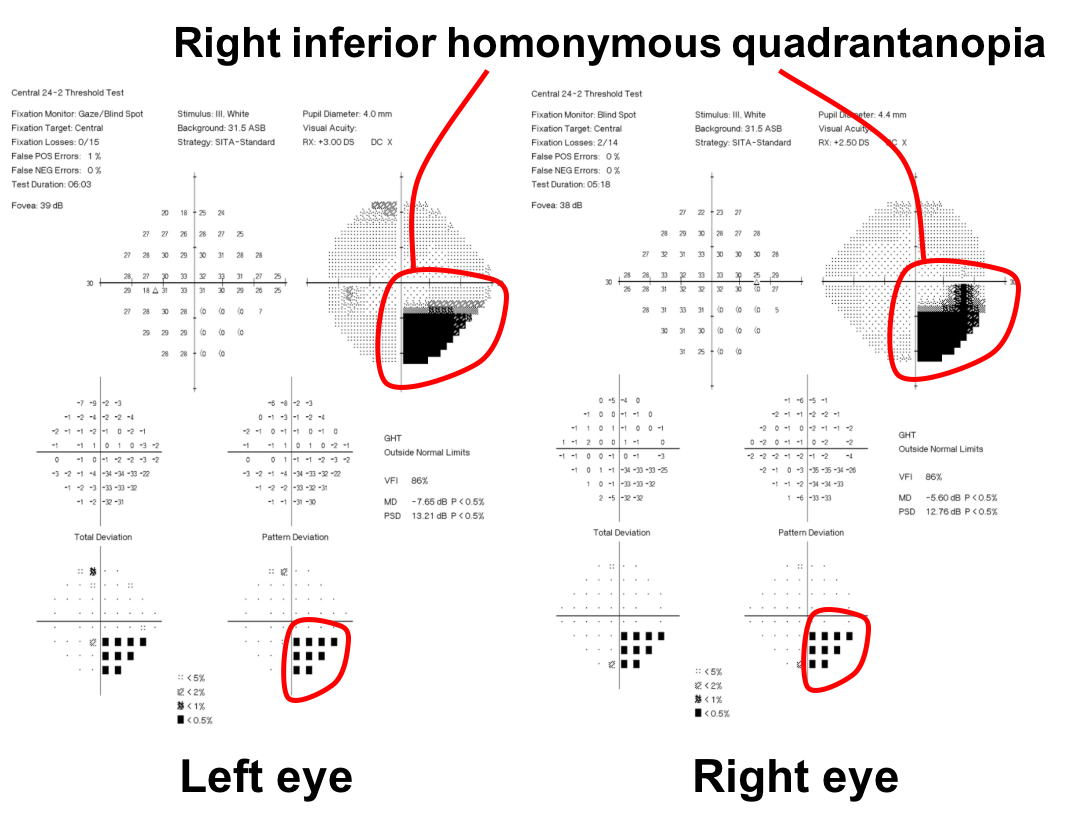
5. What other test available in the eye clinic would be most useful in this patient? 3. Humphrey visual field
Since this patient always has her visual symptoms on the right side of the visual field, there is concern for a migraine-like visual aura due to a focal cerebral lesion in the left occipital lobe. This may be secondary to an underlying cortical lesion and a visual field is important in this case to assess for a right homonymous visual field defect. This patient’s visual field is shown below.
Clinical Pearl
Formal visual field testing may be helpful in patients with positive visual disturbances, particularly when there are atypical migraine features.
6. What is the best description of this patient’s visual field?
- Right incongruous inferior homonymous quadrantanopia
- Right congruous inferior homonymous quadrantanopia
- Right congruous inferior heteronymous quadrantanopia
- Right incongruous inferior heteronymous quadrantanopia
6. What is the best description of this patient’s visual field? 2. Right congruous inferior homonymous quadrantanopia
The visual field defect is on the right side in both eyes (homonymous), is exactly the same in both eyes (congruous), and is inferior. It is not heteronymous, which means it is on different sides in both eyes.
7. What is the next best course of action for this patient?
- Close monitoring of the visual field defect to ensure it does not worsen
- Carotid dopplers
- MRI of the brain with contrast
- MRI of the orbits with contrast
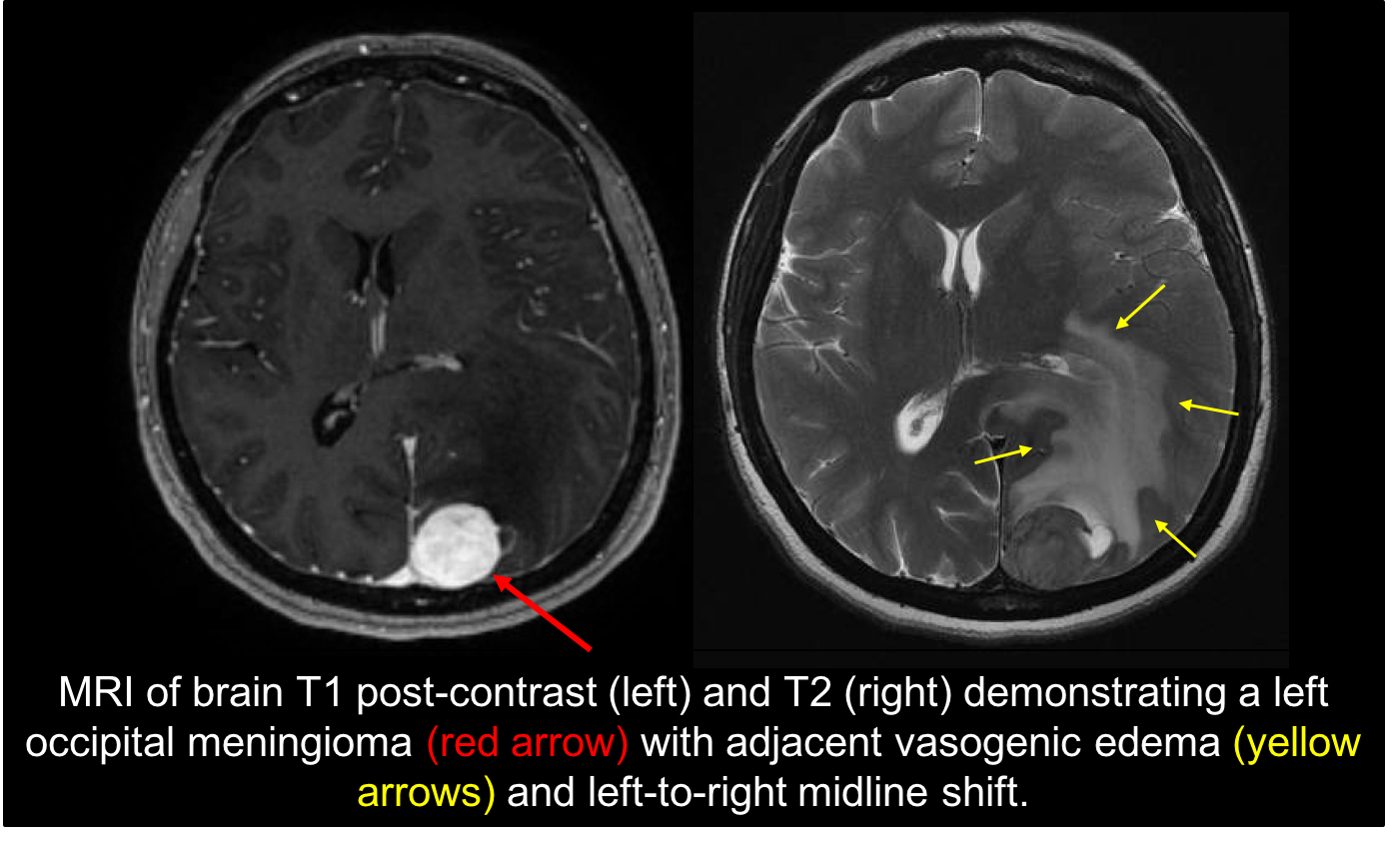
7. What is the next best course of action for this patient? 3. MRI of the brain with contrast
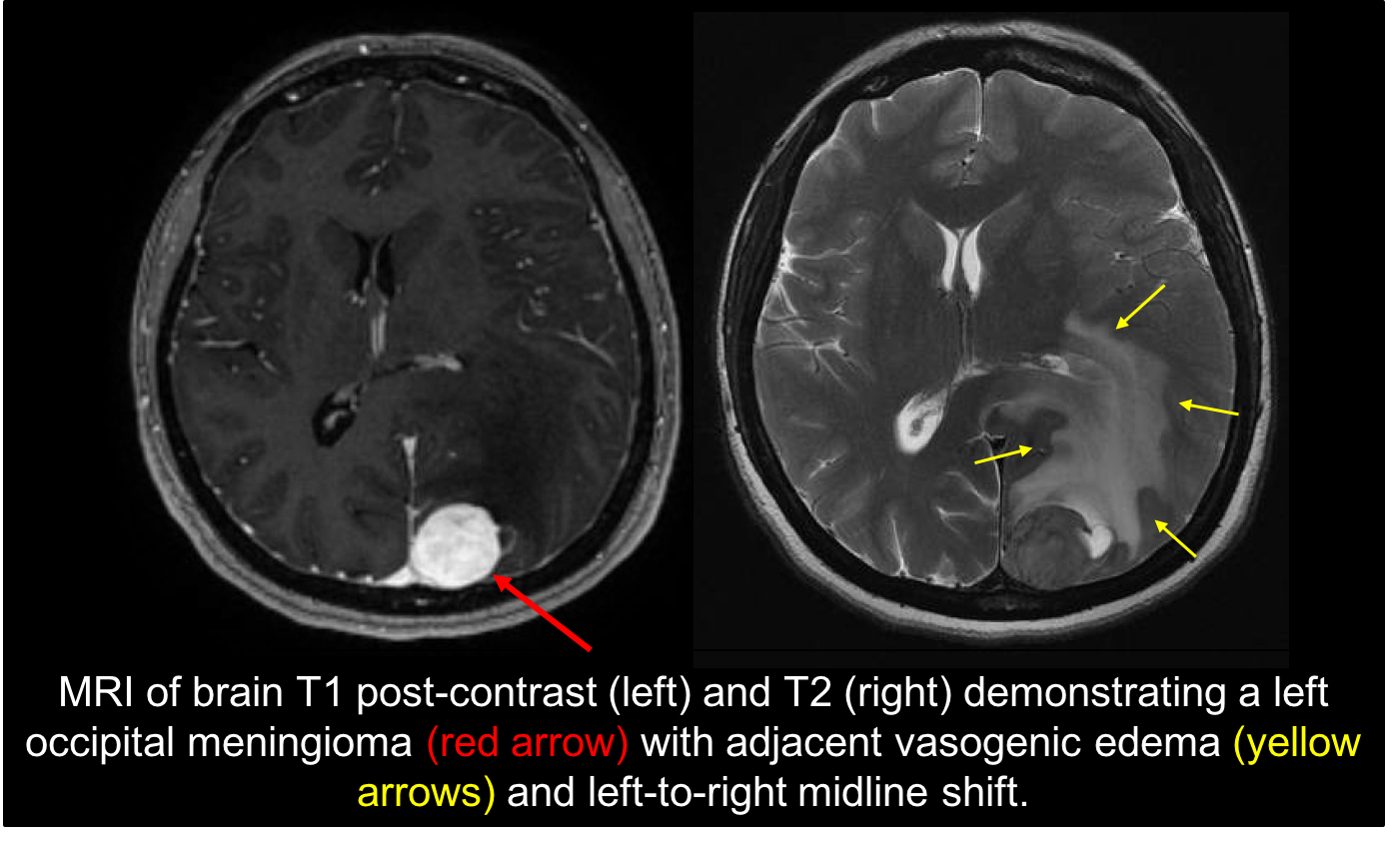
The patient has a right homonymous visual field defect localizing the process to the left retrochiasmal visual pathways. An MRI of the brain with contrast is needed to assess these pathways and the result is shown below. There is a left occipital meningioma, indicating that her visual disturbances were a result of an underlying focal cerebral lesion. This lesion likely created a state of neuronal hyperexcitability that increased her susceptibility of developing cortical spreading depression, which is a self-propagating wave of electrophysiological hyperactivity followed by a wave of inhibition.
8. Which of the following is true regarding patients with migraine-like visual auras due to focal cerebral lesions?
- There is always a visual field defect
- The lesion is always in the occipital lobe
- Routine EEG is always abnormal
- The lesion may be a congenital vascular malformation
8. Which of the following is true regarding patients with migraine-like visual auras due to focal cerebral lesions? 4. The lesion may be a congenital vascular malformation
Patients with visual seizures from underlying lesions may not always have visual field defects. This is because they may have a developmental anomaly such as a cavernoma that is present at the same time as visual cortex development. The visual cortex develops around this lesion and presumably keeps its normal spatial organization. Lesions in the cortex outside the occipital lobe may also cause visual seizures by the spread of neuronal depolarization into the visual cortex. A single routine EEG has a low sensitivity and specificity for the detection of interictal epileptiform discharges (20 to 50 percent) in patients with epilepsy.
9. In a patient with longstanding visual auras, which of the following features should prompt further investigations?
- Increase in the frequency of the aura
- Change in the features of the aura
- Co-existence of seizures
- Persistent visual field defect after the aura
- All of the above
9. In a patient with longstanding visual auras, which of the following features should prompt further investigations? 5. All of the above
It is not unusual for cerebral lesions to be discovered after a patient with presumed migraine aura has a change in the frequency or characteristics of the aura. This is similar to the concern raised in a longstanding migraineur who has a change in the characteristics of their headache. The coexistence of seizures or persistent visual fields defects are additional findings that warrant an MRI of the brain.
10. Which of the following visual fields is the best choice to be performed in patients with neuro-ophthalmic complaints such as this patient with a suspected lesion in the retrochiasmal visual pathways?
- Confrontation visual fields
- Binocular 120 degree visual field
- 24-2 SITA-Fast
- 10-2 SITA-Fast
10. What type of visual field is the best choice to be performed in patients with neuro-ophthalmic complaints such as this patient with suspected visual seizures? 3. 24-2 SITA-Fast
The Humphrey 24-2 program tests a grid of 52 points that cover the central 24 degrees whereas the 30-2 program tests a grid of 76 points over the central 30 degrees of the visual field. Since the 24-2 test strategy tests fewer points there is usually less variability and better reliability compared to the 30-2 program due to the decreased testing time. The information provided by the 24-2 program is comparable to 30-2 and is typically the test of choice for neuro-ophthalmic complaints. The 10-2 program does not include enough peripheral points and binocular fields may miss visual field defects only in one eye.
11. Which of the following are associated with the fortification spectrum associated with migraine?
- Zigzag or jagged lines
- Gradually spreads from the center to periphery or vice versa
- Convex shape
- Followed by absolute or relative scotomas
- Binocular
- All of the above
11. Which of the following is true regarding the fortification spectrum associated with migraine? 6. All of the above
The term fortification spectrum comes from the resemblance of the zigzags to the fortified, star-shaped walls of medieval town walls. The classic description of the fortification spectrum is a zigzag pattern that appears near fixation, builds up over minutes, gradually spreads from the center to the periphery, and takes on a convex shape. It may leave areas of absolute or relative scotomas in its path. It lasts less than 60 minutes and is present in both eyes, although it may be perceived as monocular in the eye ipsilateral to the temporal defect. It is explained by cortical spreading depression, which is a slowly propagating wave of depolarization followed by suppression of cortical activity.
12. Which of the following visual disturbances other than fortification spectra are associated with migraine?
- Micropsia
- Alice in Wonderland syndrome
- Palinopsia
- Scintillating scotoma
- All of the above
12. Which of the following visual disturbances other than fortification spectra are associated with migraine? 5. All of the above
Migraineurs may experience a variety of episodic or persistent visual disturbances in addition to the classic fortification spectrum. These include micropsia (objects appear too small), Alice in Wonderland syndrome (episodes of distorted body image), palinopsia (persistence of visual images), and scintillating scotomas (negative scotoma in the middle of fortification spectra), and “visual snow” (persistent television-like static). Persistent positive visual phenomena such as visual snow are often not responsive to prophylactic treatment with migraine medication.
13. Which of the following is true regarding the relationship between ischemia and migrainous visual phenomena?
- Acute ischemia can provoke typical migraine attacks in patients without a history of migraine
- Changes in the frequency of visual aura associated with migraine may be due to ischemia
- A migraine attack may lead to an infarction
- All of the above
13. Which of the following is true regarding the relationship between ischemia and migrainous visual phenomena? 4. All of the above
Ischemia, such as that caused by a dissection or significant arterial stenosis, may present as new migraines with aura in patients without a history of migraines or may lead to a change in the frequency or characteristics of the aura in patients with a history of migraine with aura. Severe vasoconstriction as a pathologic response to cortical spread depression in migraine may also lead to a migrainous infarction. However, this is a diagnosis of exclusion and further workup is required to rule out other causes of stroke.
14. Which of the following is true regarding visual seizures?
- They classically consist of multicolored, circular/spherical patterns
- They often last more than 30 minutes
- They never consist of formed objects or figures
- They are the most common type of partial seizure
14. Which of the following is true regarding visual seizures? 1. They classically consist of multicolored, circular/spherical patterns
Visual seizures are uncommon in patients with epilepsy. When they originate in the occipital lobe, they often consist of multicolored, circular and spherical patterns that last on the order of minutes. Temporal lobe seizures or those that spread secondarily to this region can produce hallucinations of formed objects and written words. Visual seizures are often confused with release hallucinations (Charles-Bonnet syndrome) or migraine visual auras and uncertainty may be resolved with seizure monitoring.
15. Palinopsia is the abnormal persistence of a visual image and can be seen in the context of migraine. What other etiologies may be responsible for this visual disturbance?
- Retinitis pigmentosa
- Parieto-occipital lesions
- Advanced glaucoma
- Pancoast tumor
15. Palinopsia is the abnormal persistence of a visual image and can be seen in the context of migraine. What other etiologies may be responsible for this visual disturbance? 2. Parieto-occipital lesions
Palinopsia may be secondary to drugs, migraine, or cerebral lesions. Drug-induced palinopsia may be permanent and has been reported in patients taking lysergic acid diethlamide (LSD) and 3,4-methylenedioxymethamphetamine (Ectasy). Cerebral lesions, particularly those in the non-dominant parieto-occipital area, should also be considered. These are almost always associated with a visual field such as a complete or incomplete homonymous hemianopia.
16. Which of the following is true regarding Charles-Bonnet syndrome?
- It is seen in patients with severe monocular vision loss
- Hallucinations may be simple (colored lines and shapes) or complex (recognizable objects and figures)
- Patients often have cognitive impairment
- It is seen almost exclusively in patients with advanced bilateral retinal pathology
16. Which of the following is true regarding Charles-Bonnet syndrome? 2. Hallucinations may be simple (colored lines and shapes) or complex (recognizable objects and figures)
Charles-Bonnet syndrome, also known as release hallucinations, refers to visual hallucinations experienced by people with bilateral blindness or severe vision loss. These patients do not have any cognitive or psychiatric impairment. Bilateral or sequential vision loss from any cause may result in the hallucinations, which may be simple or complex. Simple hallucinations consist of brief flashes of light, colored lines or shapes whereas complex hallucinations include recognizable objects and figures, which may have a dreamlike quality (fantasy figures such as dragons or miniature policemen).
Case Summary
She had stereotyped visual auras that occurred only on the right side of her vision field in both eyes. These episodes lasted only a few minutes and started to increase in frequency. A Humphrey 24-2 SITA-Fast visual field showed a right inferior homonymous quadrantanopia and MRI of the brain with contrast showed a left occipital meningioma with associated cerebral edema. She underwent resection of the meningioma and her visual symptoms resolved, but the visual field defect persisted.
Further reading:
-
Olesen J, Friberg L, Olsen TS, et al. Ischaemia-induced (symptomatic) migraine attacks may be more frequent than migraine-induced ischaemic insults. Brain 1993;116:187-202. https://www.ncbi.nlm.nih.gov/pubmed/8453456
-
Shams PN, Plant GT. Migraine-like visual aura due to focal cerebral lesions: case series and review. Surv Ophthalmol 2011;56:135-161. https://www.ncbi.nlm.nih.gov/pubmed/21335146
-
Liu GT, Schatz NJ, Galetta SL, et al. Persistent positive visual phenomena in migraine. Neurology 1995;45:664-668. https://www.ncbi.nlm.nih.gov/pubmed/7723952
-
Khoury J, Donahue SP, Lavin PJM, Tsai JC. Comparison of 24-2 and 30-2 perimetry in glaucomatous and nonglaucomatous optic neuropathies. J Neuroophthalmol 1999;19(2):100-108. https://www.ncbi.nlm.nih.gov/pubmed/10380130