5
Case
Age: 25-year-old white woman
Reason for referral to ophthalmology: Right eye painful vision loss
Past medical history: None
Past ocular history: None
Medications: Oral contraceptive pill
Habits: Non-smoker and does not drink alcohol
HPI: Three days ago, she developed pain around her right eye that worsened with eye movements. She developed blurry vision in the right eye one day later and saw an optometrist who noted a visual acuity of 20/50 in the right eye and 20/20 in the left eye, but did not detect any other abnormalities. She was referred to the emergency room and an ophthalmology consultation was requested.
Ophthalmological Examination:
Blood pressure: 118/82, heart rate 75
Visual acuity is 20/60 OD, 20/20 OS
Pupils are equal sizes and there is a right RAPD
Color vision is 2/14 OD and 14/14 OS correct Ishihara color plates
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
1. What is the most likely diagnosis?
- Functional vision loss
- Compressive optic neuropathy
- Typical optic neuritis
- Atypical optic neuritis
1. What is the most likely diagnosis? 3. Typical optic neuritis
This is a young woman who has ocular pain, pain with eye movements and reduced vision from an optic neuropathy, which is a typical presentation of optic neuritis. A relative afferent pupillary defect (RAPD) is not seen in cases of functional vision loss and compressive optic neuropathies usually cause gradual, painless vision loss.
2. What are the features of typical optic neuritis seen in this case?
- Young, white woman
- Pain with eye movements
- Absent or mild disc edema
- All of the above
2. What are the features of typical optic neuritis seen in this case? 4. All of the above
The Optic Neuritis Treatment Trial (ONTT) was a randomized controlled trial that compared treatment with intravenous methylprednisolone, oral prednisone, and placebo for patients with optic neuritis. The ONTT provided additional valuable information about the clinical profile of patients with this condition. Typical features of optic neuritis include aspects from the history, examination and response to treatment as summarized below.
Clinical Pearl
Typical features of optic neuritis include aspects from the history, examination, and response to treatment.
History:
- Young age, usually between 20 and 50 years old
- White
- Ocular pain or pain with eye movements
- Acute to subacute loss of vision
- Unilateral
Examination:
- Absent or mild optic disc edema
- Absence of intraocular inflammation
- Absence of optic disc hemorrhages, retinal hemorrhages or retinal vasculitis
Response to treatment:
- Recovery of vision with or without treatment
3. Approximately what percentage of patients with optic neuritis have pain?
- > 90%
- 70 – 75%
- 45 – 50%
- 20 – 25%
3. Approximately what percentage of patients with optic neuritis have pain? 1. > 90%
The ONTT found that 92.2% of patients had ocular pain. The pain was constant and worse with eye movements in 51.3% and present with eye movements only in 35.8%. This is a typical feature of optic neuritis. Although some patients with optic neuritis do not have pain, the absence of pain should raise concern for another diagnosis.
4. Approximately what percentage of patients with optic neuritis have optic disc edema?
- > 75%
- 60 – 70%
- 50%
- 30 – 40%
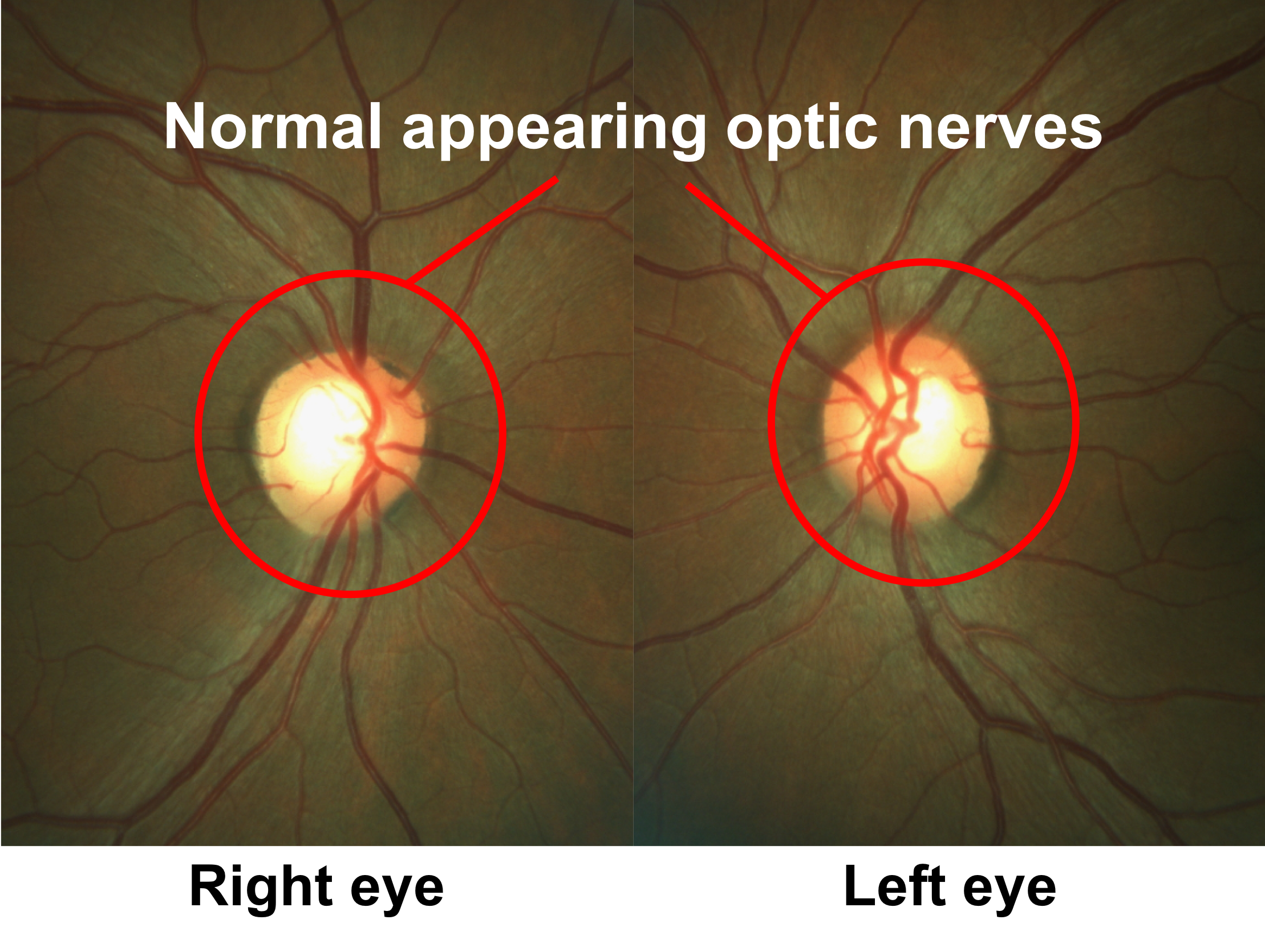
4. Approximately what percentage of patients with optic neuritis have optic disc edema? 4. 30-40%
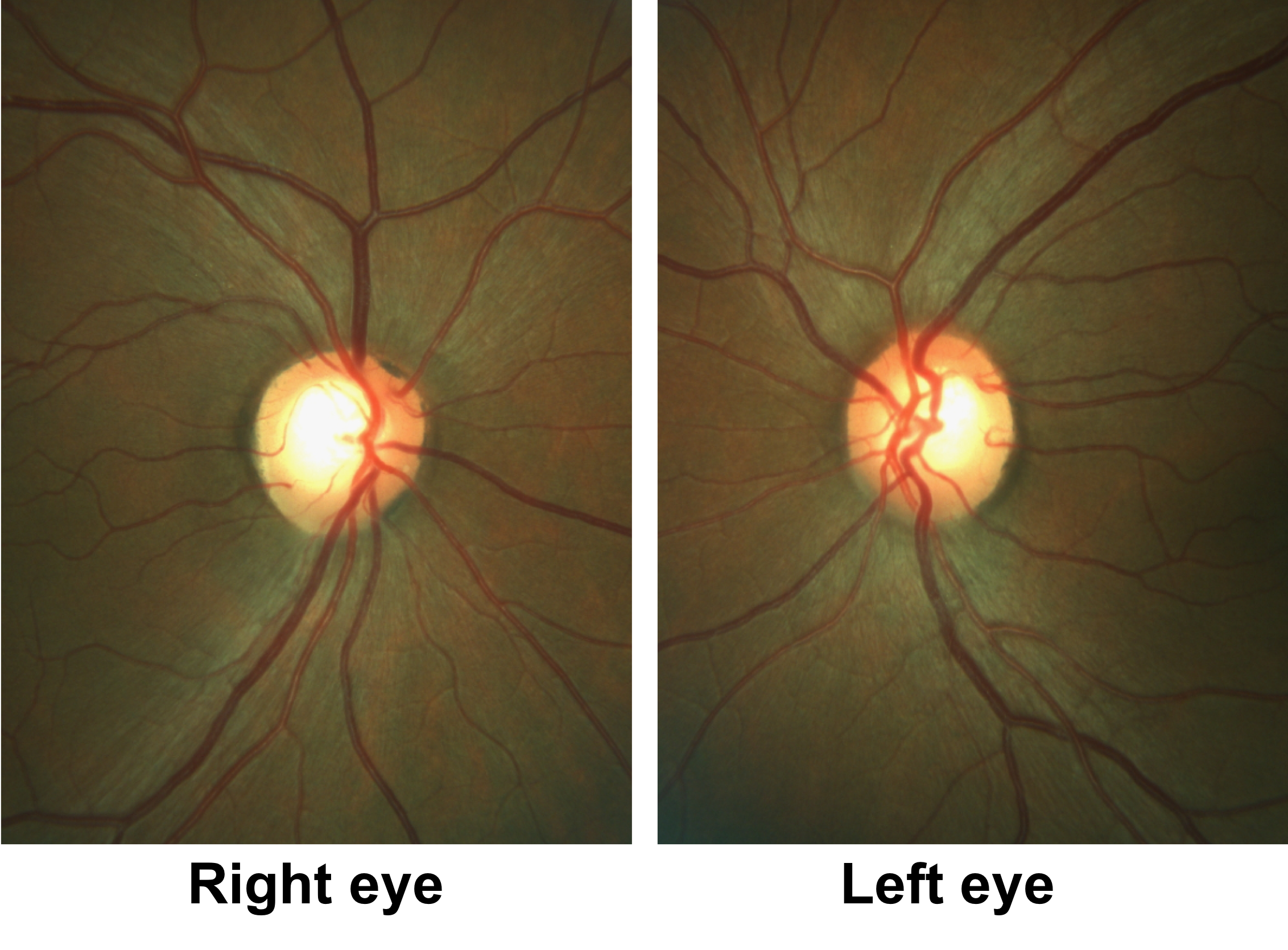
In the ONTT, 35.3% of patients had optic disc edema. In optic neuritis, the disc edema is usually mild and without disc hemorrhages. Disc or peripapillary hemorrhages were found in only 5.6% of patients in the ONTT.
Clinical Pearl
Severe optic disc edema and the presence of hemorrhages are atypical features of optic neuritis.
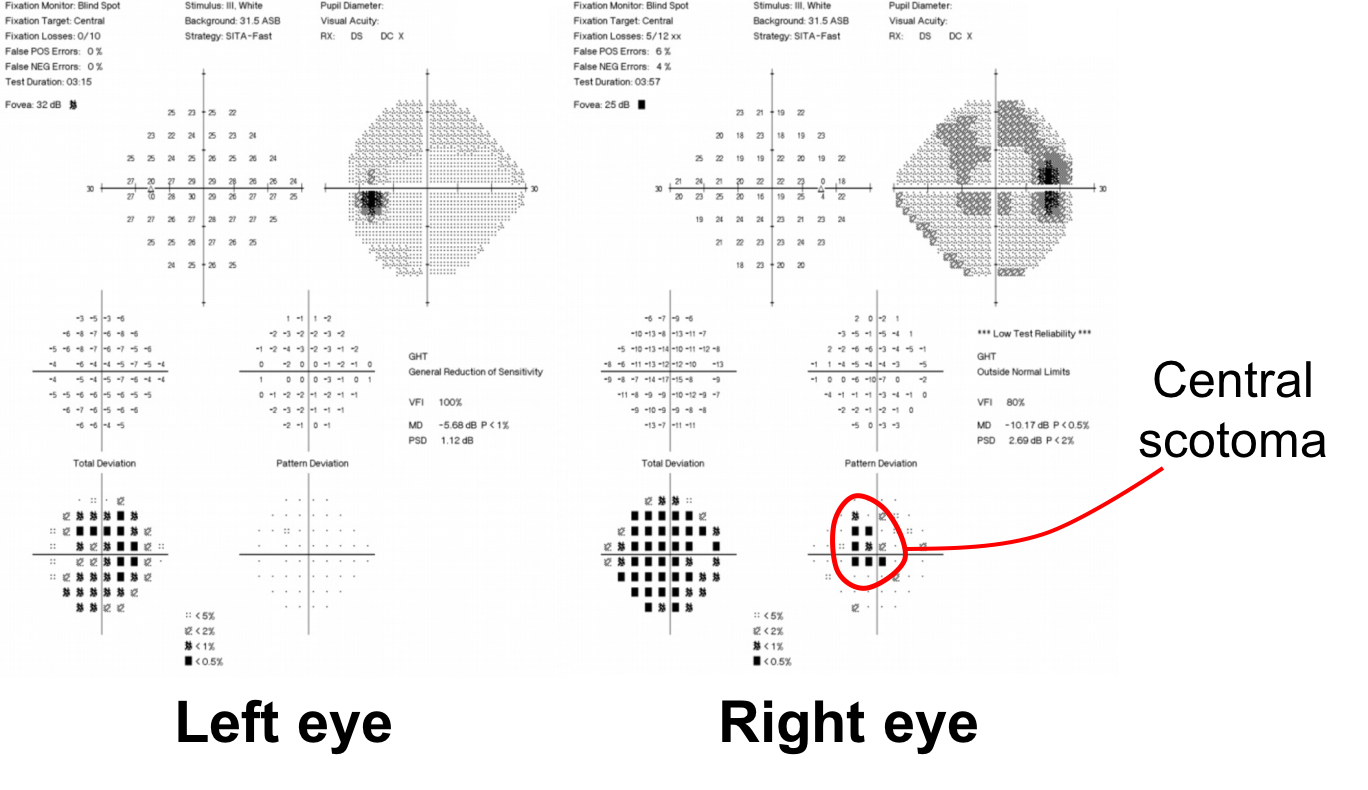
5. What visual field defects occur in optic neuritis?
- Generalized depression
- Altitudinal defect
- Central scotoma
- Hemianopic defect
- All of the above
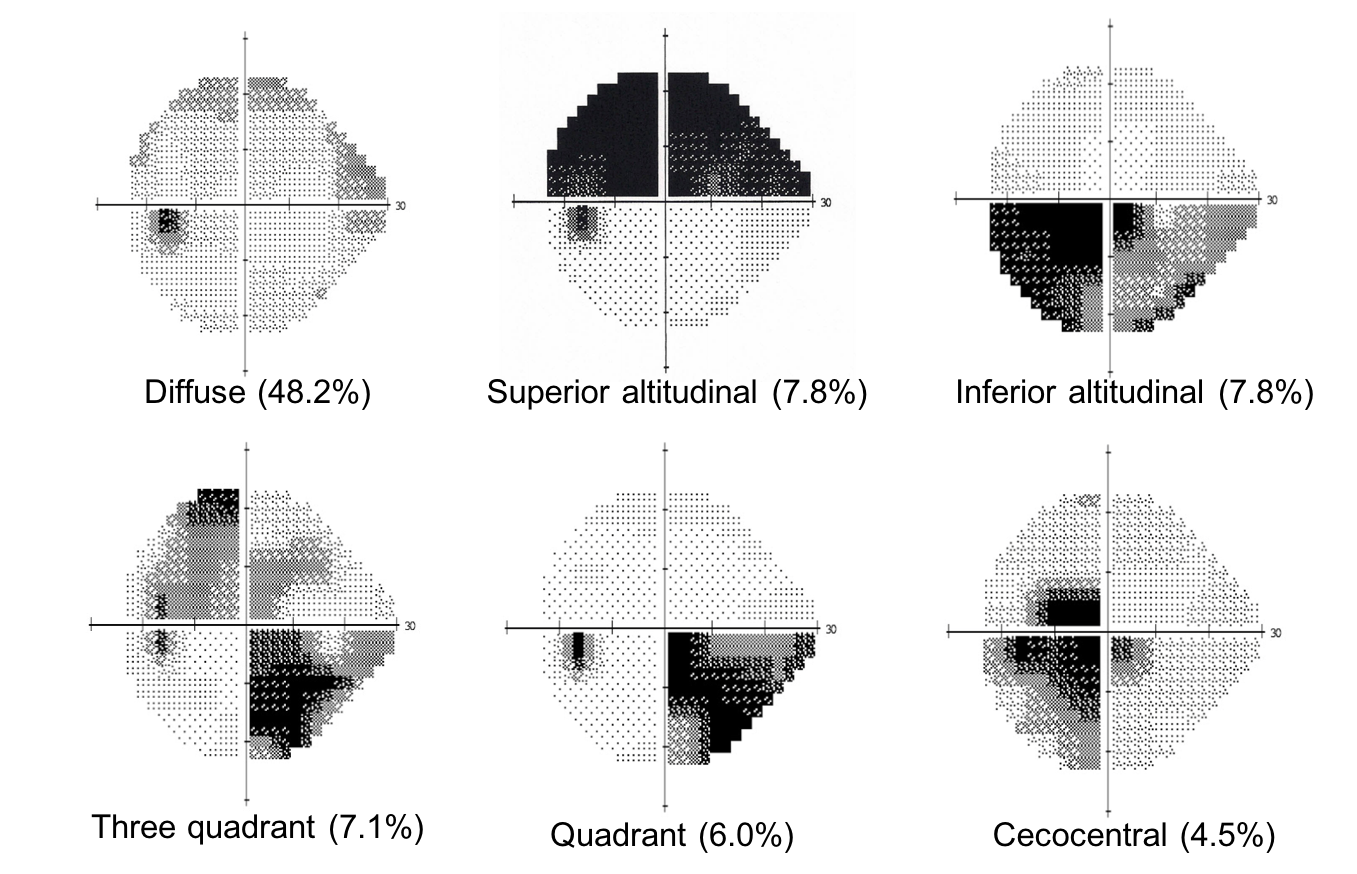
5. What visual field defects occur in optic neuritis? 5. All of the above
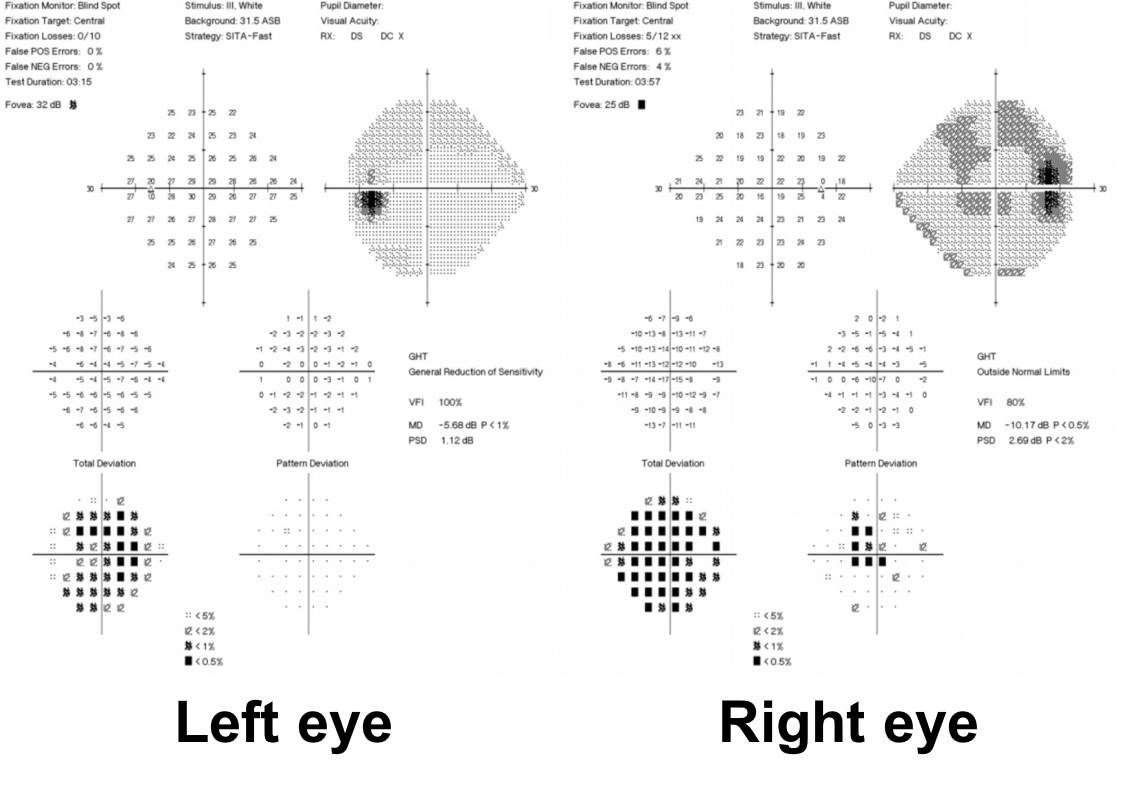
Almost every type of visual field pattern can be seen in optic neuritis. The ONTT found that the most common visual field defects were diffuse (48.2%), altitudinal (14.9%), three quadrant (7.1%), quadrant (6.0%), cecocentral (4.5%), and hemianopic (4.2%) defects.
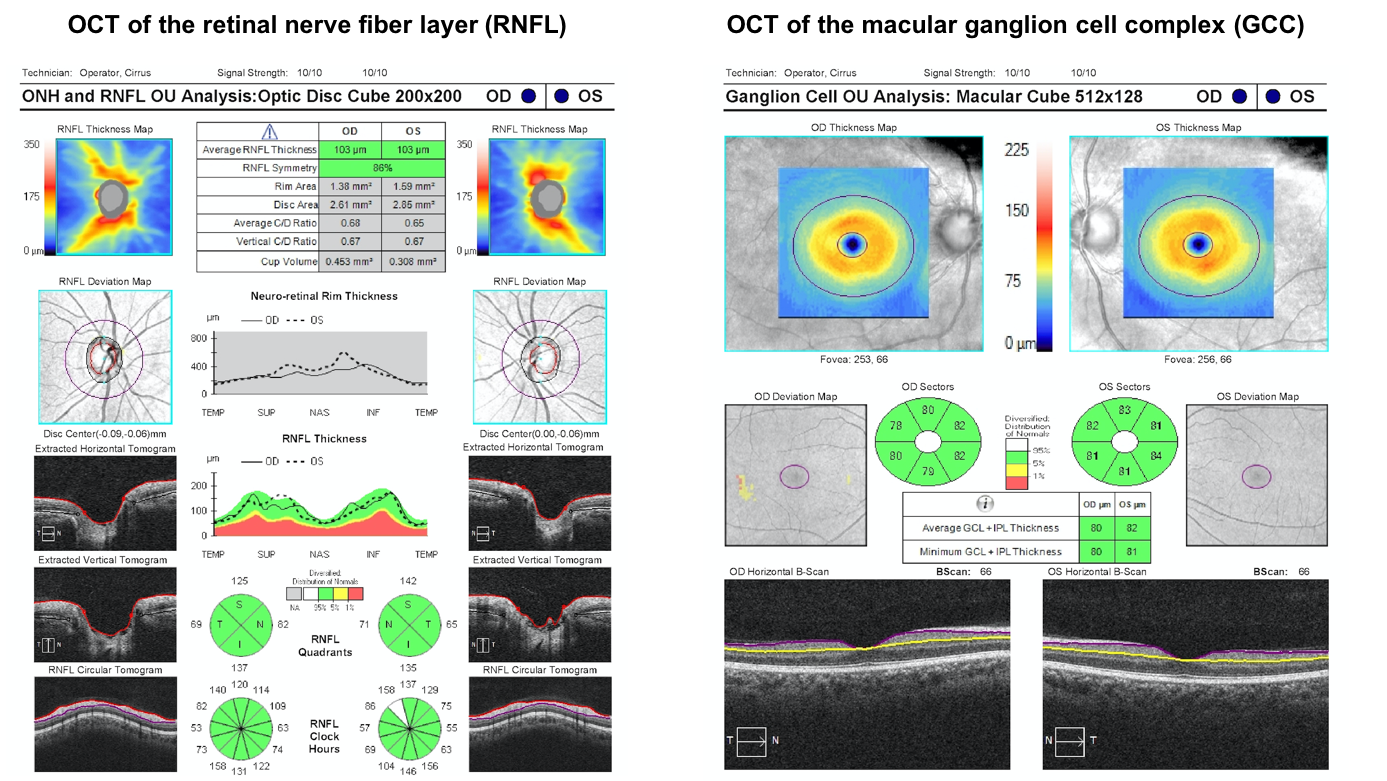
6. If Optical Coherence Tomography (OCT) of the retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) were performed at this time, what would you expect them to show? (GCC: ganglion cell layer and inner plexiform layer)
- Reduced RNFL and GCC thickness
- Reduced GCC, but normal RNFL thickness
- Reduced RNFL, but normal GCC thickness
- Normal RNFL and GCC thickness
6. If Optical Coherence Tomography (OCT) of the retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) were performed at this time, what would you expect them to show? 4. Normal RNFL and GCC thickness
OCT is a non-invasive clinical tool that can be used to measure the RNFL and GCC thickness. However, in patients with acute optic neuritis and no optic disc edema, the RNFL and GCC are approximately normal thickness assuming there is no prior history of an optic neuropathy. The RNFL and GCC will start to decrease in thickness a few weeks after the onset of vision loss. OCT of the RNFL and macular GCC from this patient with acute optic neuritis is shown below and shows an RNFL and macular GCC thickness within the normal range.
7. Which of the following tests should be considered in this patient?
- MRI of the brain
- MRI of the spine with contrast
- MRI of the orbits with contrast
- All of the above
- None of the above
7. Which of the following tests should be considered would be helpful in this patient: 4. All of the above
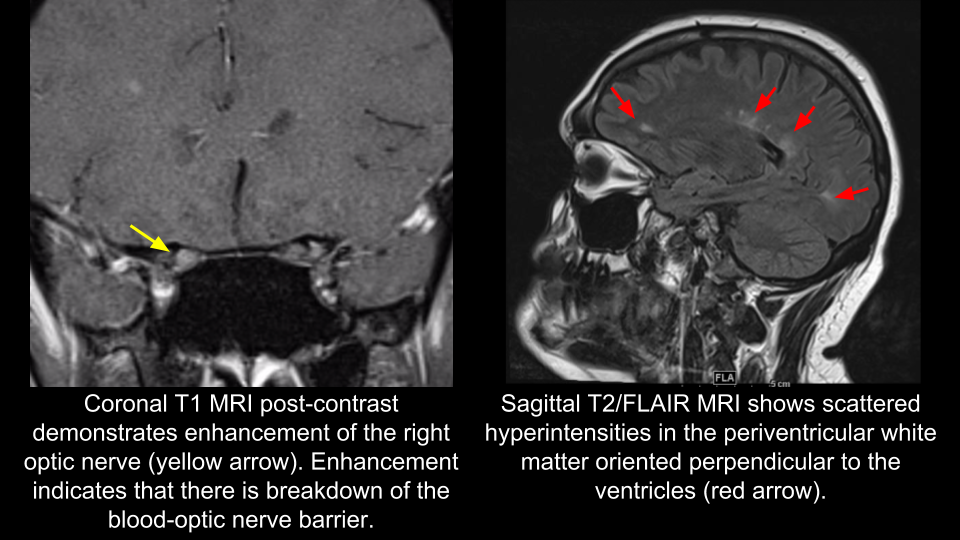
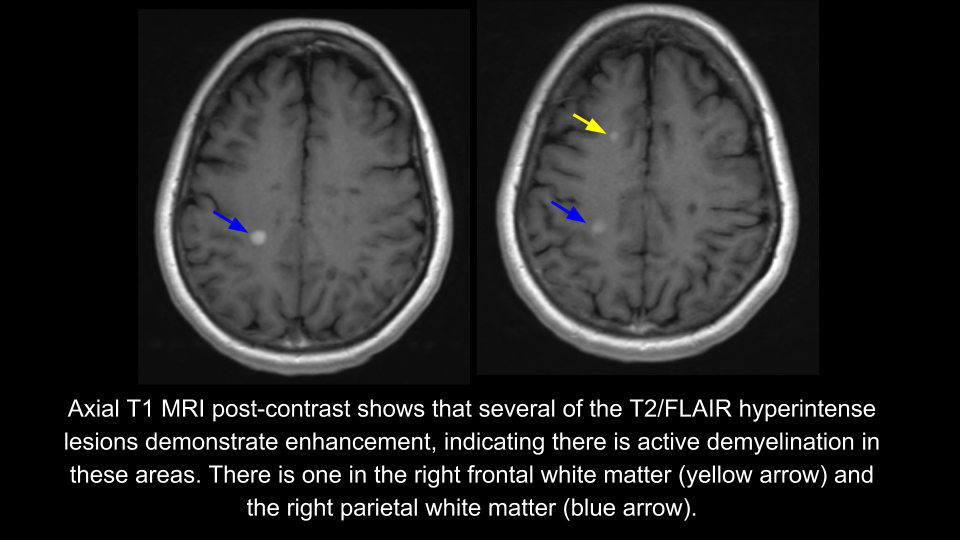
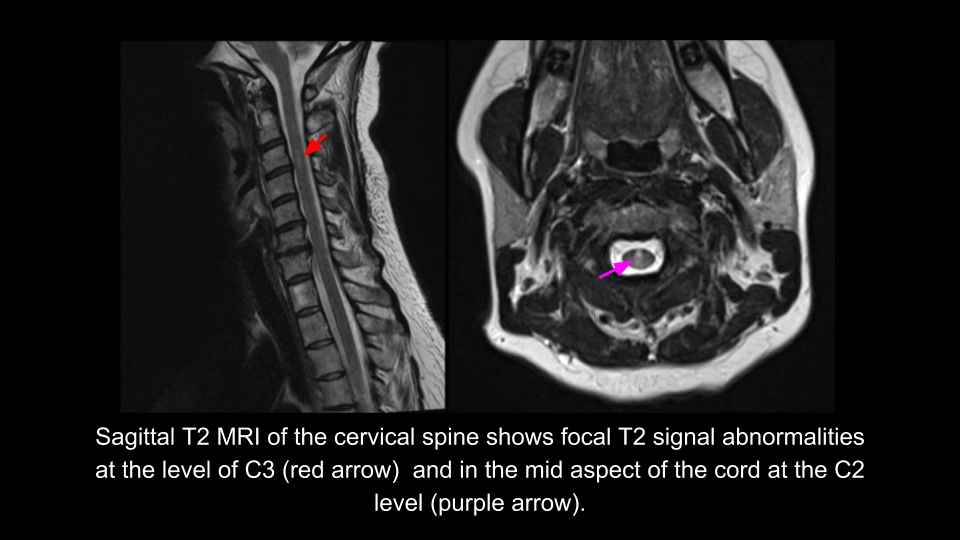
In a patient with typical optic neuritis, investigations should be directed towards assessing for any evidence of white matter lesions elsewhere in the central nervous system. This would be best evaluated with an MRI of the brain and spine with contrast. The presence of lesions disseminated in time and space would support a diagnosis of multiple sclerosis. MRI of the orbits is not strictly required for diagnosis, but may also be obtained to ensure there are no signs to suggest an alternative cause for vision loss. MRI of the orbits would be expected to show enhancement of the involved optic nerve due to breakdown of the blood-optic nerve barrier.
Many neuro-ophthalmologists recommend serologic studies to assess for neuromyelitis optica (NMO) spectrum disorders in all patients with optic neuritis. These include aquaporin-4 (AQP4) and myelin oligodendrocyte glycoprotein (MOG) antibodies, which are discussed in more detail in the next chapter. If the patient is positive for AQP4-IgG or MOG-IgG, this suggests a worse visual prognosis and a high chance of a relapsing course and intravenous methylprednisolone in combination with immunosuppressive medications are usually initiated.
In this patient AQP4-IgG and MOG-IgG were negative. MRI of the brain, orbits and spine are shown below.
8. According to the 2017 revisions of the McDonald criteria, dissemination in space is established in this patient by the presence of:
- Optic nerve and periventricular lesions
- Optic nerve and cervical spine lesions
- Periventricular and cervical spine lesions
- Multiple periventricular lesions
8. According to the 2017 revisions of the McDonald criteria, dissemination in space is established in this patient by the presence of: 4. Periventricular and cervical spine lesions
Dissemination is space refers to the development of lesions in distinct anatomical locations within the central nervous system and is essential for the diagnosis of multiple sclerosis. It can be demonstrated by the presence of one or more T2-hyperintense lesions characteristic of multiple sclerosis in two or more of four areas in the central nervous system: periventricular, cortical or juxtacortical, infratentorial brain regions or the spinal cord. The optic nerve was not included as a site to determine dissemination in space in the 2017 revision of the McDonald criteria since it was felt that there was insufficient evidence for its value in predicting a second attack. However, the optic nerve is a common anatomic site of demyelination and may be included in future revisions to the McDonald criteria.
Clinical Pearl
According to the 2017 revisions to the McDonald criteria, dissemination in space (DIS) can be shown by involvement of at least 2 of the following 4 areas:
• Periventricular
• Cortical or juxtacortical
• Infratentorial brain regions
• Spinal cord
Note: the optic nerve was not included as an anatomical location to establish DIS.
9. According to the 2017 revisions to the McDonald criteria, dissemination in time is established in this patient by the presence of:
- Symptomatic and asymptomatic lesions
- Gadolinium enhancing and non-enhancing lesions
- T2-hyperintense and T1-hypointense lesions
- Multiple periventricular lesions
9. According to the 2017 revisions to the McDonald criteria, dissemination in time is established in this patient by the presence of: 2. Gadolinium enhancing and non-enhancing lesions
Dissemination in time refers to the development or appearance of new central nervous system lesions over time. Dissemination in time is essential for the diagnosis of multiple sclerosis and can be demonstrated either by the simultaneous presence of gadolinium-enhancing and non-enhancing lesions or by the appearance of a new T2-hyperintense of gadolinium-enhancing lesion on follow-up MRI, irrespective of the timing of the baseline MRI. Gadolinium enhancement indicates an active lesion and is usually observable for the first 4-6 weeks after formation. If there are enhancing (new) and non-enhancing (older) lesions, dissemination in time can be established. Cerebrospinal fluid-specific oligoclonal bands may also be used to establish dissemination in time and were added to the 2017 revisions to the McDonald criteria.
Clinical Pearl
According to the 2017 revisions to the McDonald criteria for the diagnosis of MS, dissemination in time can be shown by:
• Simultaneous presence of gadolinium-enhancing and nonenhancing lesions at any time
• A new T2 and/or gadolinium-enhancing lesion(s) on follow-up MRI, with reference to a baseline scan, irrespective of the timing of the baseline MRI
• CSF-specific oligoclonal bands
10. Which of the following is the best choice of treatment for optic neuritis in this patient in addition to consultation with a multiple sclerosis specialist for consideration of disease modifying therapy?
- Oral prednisone (0.5 mg/kg/day) x 7 day
- Oral prednisone (1 mg/kg day) x 7 days
- Intravenous methylprednisolone 1 g daily for 3 days followed by an oral prednisone taper
- Treatment with methotrexate and rituximab
10. Which of the following is the best choice of treatment for optic neuritis in this patient in addition to consultation with a multiple sclerosis specialist for consideration of disease modifying therapy? 3. Intravenous methylprednisolone 1 g daily for 3 days followed by an oral prednisone taper
The patient has a clinical diagnosis of typical optic neuritis, which was confirmed by the enhancement seen in the right optic nerve on the MRI of the orbits with contrast. The Optic Neuritis Treatment Trial (ONTT) compared treatment with intravenous methylprednisolone to oral prednisone (1 mg/kg) and oral placebo and found that intravenous methylprednisolone hastened the recovery of vision by approximately 4-6 weeks if started within 8 days of onset. There was no difference in visual acuity at 6 months in the intravenous methylprednisolone compared to the placebo or oral prednisone group. Visual acuity improved to at least 20/40 in over 90% of patients at 6 months. Intravenous methylprednisolone also reduced the risk of developing clinically definite multiple sclerosis for two years in the intravenous methylprednisolone group. This beneficial effect appeared to lessen after the first two years of follow-up. Given the results of the ONTT, it is also reasonable to observe this patient since visual recovery is likely to occur without treatment.
11. What percentage of patients with optic neuritis will have a recurrent episode of optic neuritis within 10 years?
- 10%
- 20%
- 35%
- 50%
11. What percentage of patients with optic neuritis will have a recurrent episode of optic neuritis within 10 years? 3. 35%
The ONTT showed that the overall risk of recurrence at 10 years was 35%. The recurrence risk was higher in the oral prednisone group (44%) when compared with the intravenous methylprednisolone group (29%; p = 0.03). Oral prednisone at a dose of 1 mg/kg should not be used in the treatment of optic neuritis because of the increased risk of recurrence and lack of improved visual outcome compared to placebo.
12. According to the ONTT, what is the risk of developing clinically definite multiple sclerosis at 15 years if a patient with optic neuritis has a normal MRI of the brain?
- 72%
- 50%
- 35%
- 25%
12. According to the ONTT, what is the risk of developing clinically definite multiple sclerosis at 15 years if a patient with optic neuritis has a normal MRI of the brain? 4. 25%
The ONTT showed that for patients with a normal MRI of the brain, the risk of developing clinically definite multiple sclerosis was 25% at 15 years. If there was at least 1 white matter lesion > 3 mm in diameter, the risk of clinically definite multiple sclerosis was 72% at 15 years. The overall risk of multiple sclerosis was 50% at 15 years.
13. Which of the following features in patients with optic neuritis and a normal MRI of the brain would make the risk of multiple sclerosis essentially zero?
- No light perception vision in the affected eye
- Absence of periocular pain
- Severe optic disc edema
- Retinal exudates
- All of the above
13. Which of the following features in patients with optic neuritis and a normal MRI of the brain would make the risk of multiple sclerosis essentially zero? 5. All of the above
Atypical features of optic neuritis include severely reduced vision such as no light perception, the absence of pain, severe optic disc edema, and retinal exudates. These features were associated with a 0% risk of developing multiple sclerosis in the ONTT when the brain MRI was normal. This is because these findings suggest an alternative inflammatory etiology.
14. When the patient comes for a follow-up appointment in 1 year, what do you expect Humphrey visual field testing to show?
- The visual field should show the same visual field defect
- The visual field should be normal
- The visual field should show generalized depression
- The visual field should show an inferior altitudinal defect
14. When the patient comes for a follow-up appointment in 1 year, what do you expect Humphrey visual field testing to show? 2. The visual field should be normal
The ONTT showed that spontaneous visual recovery begins within 3 weeks and continues up to 1 year. At 1 year follow-up, at least 95% of patients had a visual acuity better than 20/40. The visual field defect is also expected to resolve. Despite this, patients will feel that the eye that had optic neuritis does not completely return back to baseline and usually notice that colors appear faded. Although intravenous methylprednisolone increased the speed of visual recovery, there was no difference in visual acuity at 6 months compared to placebo. There were slightly better visual fields, contrast sensitivity and color vision in the intravenous methylprednislone group at 6 months, but this was not seen at 1 year.
Clinical Pearl
In typical optic neuritis, visual recovery starts around 2 weeks, peaks at 1 month and continues up to 1 year without treatment.
15. A patient with typical optic neuritis has a normal MRI of the brain and spine. How might a lumbar puncture help in determining her risk of multiple sclerosis?
- The presence of nucleated cells would rule out multiple sclerosis
- The presence of elevated protein would confirm the diagnosis of neuromyelitis optica
- The presence of CSF-specific oligoclonal bands would confer an increased risk of multiple sclerosis
- The presence of CSF angiotensin converting enzyme (ACE) would confirm the diagnosis of multiple sclerosis
15. A patient with typical optic neuritis has a normal MRI of the brain and spine. How might a lumbar puncture help in determining her risk of multiple sclerosis? 3. The presence of CSF-specific oligoclonal bands would confer an increased risk of multiple sclerosis
CSF-oligoclonal bands are immunoglobulins that are a marker for inflammation in the central nervous system. A patient with optic neuritis and a normal MRI of the brain has a lower risk of multiple sclerosis, but the presence of CSF-specific oligoclonal bands suggests a higher risk compared to someone without this finding. The 2017 McDonald criteria for the diagnosis of multiple sclerosis includes the presence of CSF-oligoclonal bands in the criteria to establish dissemination in time.
16. What CSF results would you expect in a patient with optic neuritis and a diagnosis of multiple sclerosis?
- Normal leukocyte count and normal protein
- Elevated leukocyte count and elevated protein
- Normal leukocyte count and elevated protein
- Elevated leukocyte count and normal protein
16. What CSF results would you expect in a patient with optic neuritis and a diagnosis of multiple sclerosis? 1. Normal leukocyte count and normal protein
In multiple sclerosis, the CSF total leukocyte count and protein are usually normal. The leukocyte count is normal in two-thirds of patients, exceeds 15 cells/uL in less than 5% of patients and rarely exceeds 50 cells/uL. If the leukocyte cell count is very elevated, it should raise suspicion for a condition other than multiple sclerosis. If there are elevated lymphocytes, usually T-cells predominate. Cerebrospinal fluid protein is usually normal, but may sometimes be elevated.Cerebrospinal fluid albumin can also be measured since it reflects the degree of breakdown of the blood-brain barrier since it is not made in the central nervous system.
17. What additional testing is always indicated in a patient with typical optic neuritis?
- Antinuclear antibodies (ANA)
- Anti-neutrophil cytoplasmic antibodies (ANCA)
- Lyme serology
- Vitamin B12 levels
- None of the above
17. What additional testing is always indicated in a patient with optic neuritis? 5. None of the above
Ancillary testing for patients with optic neuritis depends on the clinical context. In a patient with a typical course and findings of optic neuritis, testing is directed towards determining the patients risk of multiple sclerosis and may also include assessing for serologic evidence of NMO spectrum disorder. However, if there are other factors from the history or examination that suggest a nondemyelinative cause then other testing may be helpful. For example, in a black patient with a history of uveitis and a facial nerve palsy, testing for sarcoidosis with a chest x-ray and serum angiotensin converting enzyme (ACE) are indicated. A CT scan of the chest may also be considered. In a patient with HIV and optic neuritis, more extensive investigations including a lumbar puncture and syphilis testing are indicated since there are a number of infectious causes of optic neuritis that must be considered. Routine screening for connective tissue disease was not found to be helpful in the ONTT. Lyme serology is not indicated unless there is a suggestive history or the patient is from an endemic area with Lyme disease.
18. How does optic neuritis in children classically differ from that typically seen in adults?
- It is more often anterior (present with optic disc edema)
- It is more often bilateral
- It is more often associated with a viral prodrome
- It is less often associated with multiple sclerosis
- All of the above
18. How does optic neuritis in children classically differ from that typically seen in adults? 5. All of the above
Optic neuritis in children classically has several unique characteristics that distinguish it from that seen in adults. It is more likely to present with optic disc edema, is more often bilateral, it often occurs within 1-2 weeks of a presumed viral infection, and it is less often associated with the development of multiple sclerosis. It responds well to steroids and may be steroid dependent. A large majority of patients regain normal visual acuity at 1 year regardless of their baseline clinical characteristics.
19. Why do patients with acute optic neuritis have pain with eye movements?
- There is often intraocular inflammation
- There is often significant thickening of the extraocular muscles
- The attachments of the rectus muscles are in close proximity to the inflamed optic nerve sheath
- There is sterile inflammation of the cavernous sinus
19. Why do patients with acute optic neuritis have pain with eye movements? 3. The attachments of the rectus muscles are in close proximity to the inflamed optic nerve sheath
The presence of pain and pain with eye movements are typical features of demyelinating optic neuritis. The pain is thought to be due to the close proximity of the rectus muscle insertions to the optic nerve sheath at the orbital apex. Contraction of these muscles pulls on the inflamed optic nerve and causes pain.
20. A 25-year-old woman develops pain with eye movements and vision loss and is diagnosed with optic neuritis in the right eye. Her neurological examination, MRI brain and spine are normal and she recovers vision. One year later she develops a similar episode in the left eye and she again has a normal MRI brain and spine. Does this patient meet the criteria for a diagnosis of multiple sclerosis?
- Yes, she has lesions separated in time and space
- Yes, she has 2 distinct clinical episodes consistent with demyelination
- No, she does not have separation in space
- No, she does not have any radiological signs on her MRIs
20. A 25-year-old woman develops pain with eye movements and vision loss and is diagnosed with optic neuritis in the right eye. Her neurological examination, MRI brain and spine are normal and she recovers vision. One year later she develops a similar episode in the left eye and she again has a normal MRI brain and spine. Does this patient meet the criteria for a diagnosis of multiple sclerosis? 3. No, she does not have separation in space
Since the patient only had 2 episodes of optic neuritis without any other radiological or clinical signs of other demyelination, she does not meet the criteria for a diagnosis of multiple sclerosis. She only had demyelinating lesions of the optic nerve and since this is the same location, she does not have dissemination in space. Moreover, the 2017 revisions to the McDonald criteria do not include the optic nerve as a anatomic location to establish dissemination in space.
21. A patient with optic neuritis and multiple sclerosis has transient blurring of her vision during a hot bath and when she runs outside. What is this called?
- Lhermitte’s sign
- Uhthoff phenomenon
- Pulfrich phenomenon
- Riddoch phenomenon
21. A patient with optic neuritis and multiple sclerosis has transient blurring of her vision during a hot bath and when runs outside. What is this called? 2. Uhthoff phenomenon
Uhthoff’s phenomenon is a transient worsening of symptoms during exercise, during an elevation of body temperature, or during emotional distress in patients with multiple sclerosis or other demyelinating conditions. Uhthoff’s phenomenon was reported by about 10% of patients after 6 months in the ONTT and is more common in patients that have had optic neuritis and have multiple sclerosis, although it can also be seen in otherwise healthy patients that have had demyelinating optic neuritis. This may be due to conduction block that occurs as the body temperature increases and is reached at a lower point in demyelinated nerves.
22. A small target oscillating in the frontal plane appears to be moving in an elliptical path in a patient with unilateral optic neuritis and multiple sclerosis. This is called:
- Lhermitte’s sign
- Uhthoff phenomenon
- Pulfrich phenomenon
- Riddoch phenomenon
22. A small target oscillating in the frontal plane appears to be moving in an elliptical path in a patient with unilateral optic neuritis and multiple sclerosis. This is called: 3. Pulfrich phenomenon
The Pulfrich phenomenon is when a small object oscillating in the frontal plane appears to be moving in an elliptical path in a patient with unilateral or asymmetric bilateral optic neuropathies. It is due to delayed transmission of information to the occipital cortex and can be produced in normal people by placing a neutral density filter over one eye. If the filter is placed over the right eye the object appears to be rotating counterclockwise and if placed over the left eye appears to be rotating clockwise.
23. What percentage of patients in the ONTT had no light perception vision at presentation?
- 3%
- 10%
- 20%
- 30%
23. What percentage of patients in the ONTT had no light perception vision at presentation? 1. 3%
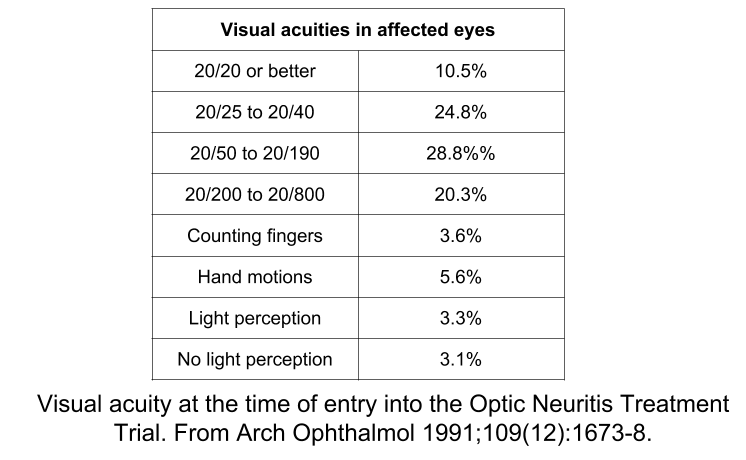
In the ONTT, approximately 35% of affected eyes had a visual acuity between 20/20 to 20/40, 30% of eyes had a visual acuity between 20/50 to 20/200 and 35% of eyes were worse than 20/200. The visual acuity at presentation in affected eyes is summarized in the table below. Patients with worse visual acuity at study entry still recovered vision. Ninety-one percent of patients in the placebo group worse than 20/200 at study entry had a visual acuity better than 20/40 one year later.
Case Summary
She had a loss of vision in the right eye with pain and pain with eye movements. Examination showed signs of a right optic neuropathy including a right RAPD, reduced color vision, and visual field defect. Her presentation was typical for optic neuritis and MRI of the brain and spine supported the diagnosis of multiple sclerosis since there were characteristic white matter lesions disseminated in time and space. She was seen by a multiple sclerosis specialist and started on disease-modifying therapy. Her vision recovered to baseline after treatment with intravenous corticosteroids and she did not develop another episode of optic neuritis.
Further reading:
Keltner JL, Johnson CA, Spurr JO, Beck RW. Baseline visual field profile of optic neuritis. The experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Arch Ophthalmol 1993;111(2):231-4. https://www.ncbi.nlm.nih.gov/pubmed/8431161
The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Optic Neuritis Study Group. Arch Ophthalmol 1991;109(12):1673-8. https://www.ncbi.nlm.nih.gov/pubmed/1841573
A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med 1992;326(9):581-8. http://www.nejm.org/doi/full/10.1056/NEJM199202273260901
Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol 1991;109(12):1673-8. https://www.ncbi.nlm.nih.gov/pubmed/1841573
Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol 2008;65(6):727-32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2440583/
Atkins EJ, Biousse V, Newman NJ. Optic neuritis. Sem Neurol 2007;27(3):211-20. https://www.ncbi.nlm.nih.gov/pubmed/17577863
Wan MJ, Adebona O, Benson LA, Gorman MP, Heidary G. Visual outcomes in pediatric optic neuritis. Am J Ophthalmol 2014;158:503-507. https://www.ncbi.nlm.nih.gov/pubmed/24907434