BUILDING AND MAINTAINING YOUR SKILLS
There are many options to consider in developing and maintaining your skills, knowledge and leadership in reproductive health, rights and justice, both during and after training. Support can be identified through help of mentors and existing national networks and organizations.
GAINING AND MAINTAINING CLINICAL COMPETENCY
As of 2020, medication abortion accounts for more than half of the abortions in the United States. As medication abortion is becoming more common, provider training should center on medication abortion as well as aspiration abortion. Many clinics are only capable of offering mifepristone and misoprostol for abortion or miscarriage management, so obtaining this training is vital to providing care. Expanding clinical care to include medication management for early pregnancy loss and abortion is an important step in familiarizing providers with these medications, normalizing their use in primary care, and expanding access to full-spectrum reproductive healthcare. As abortion in the U.S. becomes more restricted, training in medication abortion may be especially important, and new providers entering care can help increase access.
It can be advantageous to gain experience in medication and procedural abortion during professional training, as both credentialing and malpractice can be covered under interagency agreements between your training program and a high-volume clinical site. However, there are also opportunities after training, including through the following organizations:
- Midwest Access Project
- Medical Students For Choice
- TEACH Leadership Fellowship
- Clinical Abortion Training Centers
- Nurses for Sexual and Reproductive Health- Training Opportunity for RNs
- Reproductive Health Access Project (RHAP)
Each skill can be delineated into clear steps with observable competencies for learners and for trainers-in-training (Cappiello 2016). Important aspects of clinical competence in medication and aspiration abortion include patient-centered counseling and the ability to identify and triage complications as they arise (Levi 2012). The number of cases to achieve competence and confidence in medication or aspiration abortion will vary between individuals, training environment, and exposure to complications or complex cases. Your reproductive health trainers can help you estimate what it will take to achieve competency in the services you hope to provide (See Chapter 13: Core Competencies for Early Abortion Care by Primary Care Clinician).
CONSIDERATIONS FOR ADVANCED PRACTICE CLINICIAN (APC) PROVIDERS
APCs, (including NPs, CNMs, PAs) have a long history of providing primary, reproductive, and abortion care, especially in underserved areas, and are a natural fit in the role of abortion providers. APC provision of abortion-related services is safe, efficacious, and acceptable to patients (NASEM 2018). Through additional training opportunities and job support, we can expand the number of APC providers as part of the solution to increase community access to abortion, miscarriage and post-abortion contraceptive care.
Even with a changing policy landscape permitting APC abortion care, clinical training opportunities in abortion care for APCs have been rare. New state initiatives are beginning to fund and prioritize APC training, emphasizing the need to increase training capacity within APC educational programs and create training pathways for existing APC providers. Most recently, 22 states allow APCs to provide medication abortion, and 20 of these also allow APCs to provide aspiration abortion (Taylor 2023). State regulations related to physician oversight may also add burdens for APCs providing care.
Achieving competency is similar for APCs and physicians (Levi 2018; see Chapter 13: Competencies and Sign Off). Medication and procedural abortion is already within APC Professional Scope of Practice (per WHO, NASEM, NAF, ACOG, APHA, and APC professional organizations). Legal Scope of Practice differs due to Physician-Only laws which create artificial legal barriers to practice (similar to banned states where physicians also cannot provide abortion care that is within their scope of practice) (Jenkins 2023). For more information, see the AP Toolkit, the Law Atlas Policy Surveillance Project, and contact your state Board of Registered Nursing or PA licensing board.
Physicians and administrators can support APC involvement by prioritizing their training, ongoing practice volume, and professional development opportunities, as well as ensuring guidance on referrals as needed.
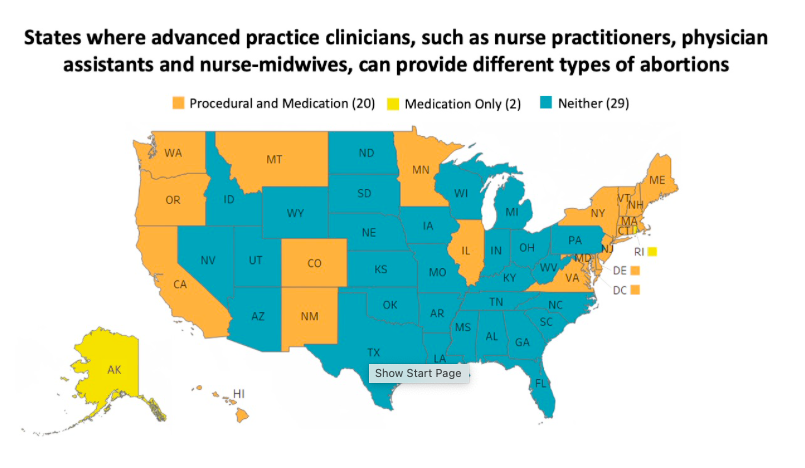
Taylor D, APC Toolkit: 2023
BUILDING A STRONG KNOWLEDGE BASE
Please consider using the following resources to develop foundational knowledge, review evidence-based practices, and expand understanding:
- Online resources
- Innovating Education: videos, materials, and resources on abortion, early pregnnacy loss, contraception, counseling, and more
- National Abortion Federation: online courses on abortion, contrapeption, ultrasound, trans-inclusive abortion care, and values clarification
- Reproductive Health Access Project Contraceptive Pearls: sign up and review previous pearls
- Reproductive Health Access Project: resources and patient information on abortion, contraception, and miscarriage management
- Nurses for Sexual and Reproductive Health (NSRH): online learning portal for members with educational modules on sexual and reproductive health
- Partners in Contraceptive Choice and Knowledge: provider and patient resources and webinars
- AbortionPillCME: See one, do one, teach one medication abortion training
- Access Listserv: National listserv to participate in ongoing discussions. Membership requires referral by a current participant for security reasons.
- TEACH Curriculum: complete supplemental readings in each chapter
- Medical journals:
- Books
- Reproductive Justice, Loretta Ross and Rickie Solinger
- Radical Reproductive Justice: Foundation, Theory, Practice, and Critique, Loretta Ross, Lynn Robers, Erika Derkas, et al.
- Killing the Black Body, Dorothy Roberts
- Sister Outsider, Audre Lorde
- You’re The Only One I’ve Told: The Stories Behind Abortion, Meera Shah
- Shout your Abortion, Amelia Bonow, Emily Nokes (Editors)
- The Turnaway Study, Diana Greene Foster
- Policing the Womb, Michele Goodwin
- Textbooks
- Management of Unintended and Abnormal Pregnancy, Maureen Paul
- Contraceptive Technology, Robert Hatcher
- Radical Reproductive Justice, Whitney Peoples and Loretta Ross
- Procedures in Primary Care, Grant Fowler
- Podcasts
- Annual reproductive health conferences:
ACHIEVING DIVERSITY, EQUITY, AND INCLUSION IN TRAINING AND PROVISION
The framework of reproductive justice should be employed in training to acheieve diversity, equity, and inclusion in both training environments and abortion care (BMMA 2020, Ross 2017). The pervasiveness of white supremacy in medicine, and reproductive health specifically, has harmed Black, Indigenous, Latinx/e/a and other communities of color for generations. This has sustained white providers in positions of power and / or providing abortions for communities with whom they may share little background. For example, recent analysis shows large differences in provider and patient ethnicities (AAMC 2019, Guttmacher 2016).
| Ethnicity | Physicians | Patients |
| White | 56% | 39% |
| Black | 5% | 28% |
| Hispanic | 5.8% | 25% |
Patients may prefer providers of the same racial and ethnic background, and although further study is needed, shared racial/ethnic backgrounds may foster better relationships, continuity, and health outcomes (Miller 2022). In order to better meet the health needs of marginalized and diverse populations, we need to increase abortion provider diversity (Ma 2019, Smedley 2001). Priority should be placed on supporting and training providers of diverse racial, ethnic, and socioeconomic backgrounds, mirroring and honoring the diversity of patients and people. Beyond training, space should also be made in leadership positions in order to effectively change the systems we operate and organize in.
Given the hierarchical natural of training environments and historical systemic discrimination in medicine, support and mentorship should also be provided around navigating power structures and discrimination. Abortion providers also experience additional layers of discrimination given the politicization and polarization of reproductive healthcare which should be acknowledged and addressed (León 2018).
MENTORSHIP
Mentorship is a powerful tool in creating a more diverse and enriched abortion provider community. As a trainee, connect with larger communities of reproductive healthcare providers (see Organizational Resources Table below), reach out to faculty who can serve as a reference or connection to other communities, attend conferences, or join the AMSA Mentorship Sprint. After training, you can mentor a student or trainee, help fill gaps in training at their school or program, or lead a project related to reproductive health and justice.
LANDSCAPE AND LIMITATIONS
There are many reasons why abortion training and provision is limited including declining number of abortion cases nationwide, limited funding for abortion provision and training, saturation of providers in urban coastal areas, government or institutional policy limiting abortion provision to OB/GYNs or fellowship-trained physicians (excluding advanced practice clinicians and primary care physicians), and the COVID-19 pandemic limiting space for trainees. The SCOTUS decision overturning Roe in June 2022 will have seismic impacts on the landscape of abortion training across all states (Center for Reproductive Rights 2022, Kurtzman 2022). We will be following these anticipated changes.
It is also important to note that clinics in provider shortage areas may be more willing to help with credentialing and malpractice, but back-up and security issues may be more challenging. For more information on training outside of your program’s standard curriculum or after graduation, see Organizational Resources Table below).